Abstract
This study was to describe and compare the expenditures per hospital admission between urban and rural patients with a primary diagnosis of type 2 diabetes with and without complications in an urban tertiary hospital in Jinan, China. This study comprised 880 inpatients hospitalized from 1 January 2006 to 31 August 2008. Inpatient costs were directly collected from hospital accounting system, which comprised the costs of all prescribed drugs, medical procedures, laboratory tests, hotel service, and nursing care during the hospital stay. Generalized linear model (GLM) with log-link and gamma variance functions was used to identify the differences in the total inpatient costs between urban and rural patients after controlling for the potential cost predictors. The adjusted individual inpatient costs per hospitalization were $1680 for urban patients and $1437 for rural patients who had no complications; $1973 and $1687 for those with microvascular diseases; $2045 and $1750 for those with macrovascular diseases; $2208 and $1889 for those with both microvascular and macrovascular diseases (p < 0.05 between urban and rural patients for all the categories). The costs of prescribed drugs accounted for more than two thirds of the total costs in both groups. Urban residence was positively associated with inpatient costs in addition to diabetic complications, insurance, days in the hospital, male gender, and insulin treatment. In conclusion, within the same disease category, rural patients always spent less than the urban patients’ per hospital admission. Large out-of-pocket financing burden, low medical insurance coverage and reimbursement rate, and low income of rural patients can partly attribute to the urban–rural gap in healthcare expenditures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In China, the prevalence of type 2 diabetes mellitus is increasing. The China National Diabetes and Metabolic Disorder Study, conducted from 2007 to 2008, showed that China has passed India in having the largest diabetic population worldwide, amounting to 92.4 million adults [1]. Diabetes and its complications reduce the quality of life [2–4] and raise premature mortality [5]. This disease also imposes a heavy economic burden on the patients’ family, healthcare system, and society [6, 7]. In 2013, the global health expenditure on diabetes is estimated to at least USD 548 billion, accounting for 11 % of world’s total healthcare expenditures and USD 627 billion by 2035 [8]. In China, about 6 % of total health expenditure and USD 115 per person spent on diabetes in 2010 [9].
A large healthcare disparity between urban and rural patients exists in China. Since a wide inequality in medical resources allocation [10, 11] and medical insurance system [12], high-quality medical resources tend to be concentrated in large-capacity hospitals in urban areas. High levels of out-of-pocket expenditure and long distances to the hospital compromised many rural people access to healthcare [13]. Whether inpatient treatment costs are higher in urban patients than in rural patients due to type 2 diabetes and its complications, however, is less well known. The aim of this study was to describe and compare the expenditures per hospital admission between urban and rural patients with a primary diagnosis of type 2 diabetes with and without complications in an urban tertiary hospital, Jinan, China.
Methods
Study populations
This observational study was carried out in a provincial public hospital (tertiary level) in Jinan, the capital city of Shandong Province, China. This study comprised 880 patients, with a primary diagnosis of type 2 diabetes and receiving medical treatment in hospital from 1 January 2006 to 31 August 2008. Demographic and clinical characteristics came from the patients’ clinical records and included age, gender, date of admission and discharge, residence locations, insurance types, occupations, family history of diabetes, duration of diabetes, insulin treatment, hypertension, body mass index (BMI), blood glucose, hemoglobin A1c levels (HbA1c), and the presence of complications. Hypertension was defined as with hypertension history or receiving antihypertensive drug treatments in hospital, or both. Patient was broadly categorized as a “rural” or “urban” patient based on their information in the family register system. Insurance included the medical insurance scheme of an urban employee, a free medical care scheme, the basic medical insurance scheme of urban residents, and a new rural cooperative medical scheme introduced since the February in 2003.
Inpatient costs of patients with type 2 diabetes were directly collected from hospital accounting system, which comprised the costs of all prescribed drugs, medical procedures, laboratory tests, hotel service, and nursing care during the hospital stay. All costs were collected in Chinese Yuan (¥), by using the exchange rate of 1 USD($) ≈ 6.9 CNY(¥), representing the level for the year 2008.
Diagnoses of type 2 diabetes and diabetic complications were identified from hospital discharge records filled in by a doctor in charge according the international and national standard diagnostic procedures and criteria [14]. The following complications were taken into account: microvascular diseases constituting neuropathy, nephropathy, retinopathy, and diabetic foot ulcers; macrovascular diseases constituting peripheral vascular disease, stroke, coronary heart disease, myocardial infarction, and coronary artery disease. For economic analysis, patients with type 2 diabetes were classified into four categories: (I) without complication, (II) with one or more microvascular diseases only, (III) with one or more macrovascular diseases only, (IV) with both microvascular and macrovascular diseases.
Statistical analysis
Differences in means between two groups were compared using independent sample students’ T test; in proportions were tested with the Pearson Chi-square test. Given the right-skewed distribution of the cost data, the generalized linear model (GLM) with log-link and gamma variance functions was used to identify the differences in inpatient costs between urban and rural patients with type 2 diabetes after controlling for the potential cost predictors.
All statistical analyses were performed with Predictive Analytics SoftWare (PASW) 18.0 (Statistical Package for the Social Sciences, Chicago, IL, USA), with statistical significance defined as a two-tailed p < 0.05.
Results
During January 1, 2006 to August 31, 2008, a total of 880 patients with a primary diagnosis of type 2 diabetes were admitted in hospital and all included in the current study. The urban patients had longer stays in hospital, higher medical insurance coverage rate and were more obese than those in rural patients (p < 0.05 between urban and rural). HbA1c was significantly higher in the rural patients, compared with urban patients (p < 0.001). A high proportion of patients received insulin treatment in both groups (88.5 % in urban and 91.9 % in rural patients, p > 0.05), and there were no differences in 2 h postload glucose levels when discharged from the hospital (Table 1).
The multivariate adjusted mean of total individual inpatient costs per hospitalization were $2045 for urban patients and $1759 for rural patients (p < 0.05) (Table 2). The costs of prescribed drugs were significantly higher in urban patients than in rural patients ($1423 vs. $1197, p < 0.05), accounting for more than two thirds of the total costs for both groups. The hotel service and nursing care costs altogether accounted for less than 6 % of total costs for both groups.
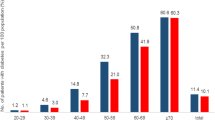
In our study, 10.7 % of urban and 17.7 % of rural patients did not experience complications; 38.0 % and 45.2 % had microvascular complications only; 6.0 % and 5.6 % had macrovascular complications only; and 45.3 % and 31.5 % suffered from both micro- and macrovascular complications. Compared with the patients without complications, the adjusted total inpatient costs for patients with microvascular diseases, macrovascular diseases, and both were 1.2, 1.2, and 1.3 times higher for both urban and rural inpatients, but within the same disease category, the costs were significantly lower in rural patients than in urban patients (Table 3).
Multivariate regression analysis revealed that urban residence was positively associated with the inpatient costs in addition to diabetic complications, length of hospitalization, male gender, and insulin treatment (Table 4). Compared with those who did not receive insulin treatment, insulin receivers added 22 % more money on the top of drug costs in both urban ($1449 in receivers vs. $1126 in non-receivers) and rural patients ($1218 in receivers and $947 in non-receivers) (p < 0.001 for both groups). The insurance types appeared to be a significant predictor when the variable for the location of residence and occupations were removed from the multivariate model.
Discussion
The per hospital admission inpatient costs in this urban tertiary hospital were significantly different between urban and rural diabetic patients. The findings are consistent with previous studies in China and India. A Chinese study showed that the age-adjusted diabetes inpatient expenses were 6199 CNY for urban patients and 3649 CNY for rural patients (p < 0.05) in three tertiary and three secondary urban hospitals of Xuzhou [15]. In India, total annual medical expenditures on healthcare were significantly higher for urban patients than for rural patients with type 2 diabetes (227 USD vs. 142 USD, p < 0.001) [16]. A previous urban study in China has shown that in patients with diabetes, a major driver of healthcare costs is complications [17]. Our study further confirmed these findings, suggesting a need to prevent the onset and development of diabetic complications in order to save medical resources and expenditures.
Urban–rural gap was mainly due to the insurance system and social-economic status. Our results demonstrated that insurance coverage rates were significantly different between urban and rural patients. A study investigated the expenditures on hospital admission for inpatients with type 2 diabetes in Asia found that uninsured patients had significantly shorter length of stay and lower spending than insured patients, especially in the countries with large out-of-pocket financing burdens such as India and China [18]. In China, dominate forms of medical insurance in urban areas are the Urban Employee’s Basic Medical Insurance System for all the employees in both public and private companies and the Urban Residents Basic Medical Insurance since 2007, which cover all urban registered residents. In 2003, a new rural health insurance program, the New Cooperative Medical Scheme (NCMS), was introduced in the Shandong province [13]. Since it operated on a voluntary basis, a minority of the rural patients in our study was enrolled in. Most of the rural patients were uninsured and pay out-of-pocket for hospital care. For the people who had NCMS membership, the monetary reimbursements were also insufficient.
Limited ability to pay for the increasing cost of medical services among rural patients would also contribute to this disparity. The household income was lower in rural than in urban patients. Based on the national statistical report in 2008, the per capita annual net income of rural households in Shandong provinces was 722 USD, compared with the 2067 USD disposable income for urban households [19]. In urban areas, the elderly are more likely to receive retirement pensions ranging from 60 to 100 % of their last wage. For the majority of rural elderly who have neither medical insurance nor retirement pensions, the family is their predominant mode of support [20].
The cost of prescribed drugs was the largest contributor to the overall expenditures, accounting for almost 70 % of the total inpatient costs, whereas the overall costs of drug therapy represented only 27 % of total healthcare costs in the Cost of Diabetes in Europe-Type 2 (CODE-2) study [21] in Europe. The drug prices relative to the gross domestic product (GDP) were higher in China than in Europe. For example, the retail price of a 10-ml vial of soluble human insulin 100 IU/ml manufactured by Eli Lilly was 9.4 USD (62.10 CNY) in our study hospital, 22.5 USD (150 Swedish Kroner) in Sweden [22] and 27.5 USD (20.33 EUR) in Finland [23], while the GDP per capita based on purchasing power parity (PPP) in 2008 was 6188 International dollars (ID) in China, 36205 ID in Sweden, and 35951 ID in Finland [24]. The drug price in China was one third of that in Finland, but the GDP per capita was one sixth of the Finnish GDP per capita.
Finally, it should be kept in mind that these findings from the study hospital may not be applicable to other hospitals. Our study hospital is a tertiary-level provincial hospital located in the economically well-developed urban capital city and share common features with other hospitals in the same level. But to what extent the estimated costs differ from the costs incurred in a secondary hospital is unknown and needs good further investigation.
In conclusion, the costs of per hospital admission were lower for the rural type 2 diabetes patients than for their urban counterparts given the same disease severity. Large out-of-pocket financing burden, low medical insurance coverage and reimbursement rate, and low income of rural patients can partly attribute to the urban–rural gap in healthcare expenditures. The living and medical care conditions in the rural population need to be further improved.
References
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, et al. China national diabetes and metabolic disorders study group. Prevalence of diabetes among men and women in china. N Engl J Med. 2010;362(12):1090–101.
Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ. 2005;14(3):217–30.
Solli O, Stavem K, Kristiansen IS. Health-related quality of life in diabetes: the associations of complications with EQ-5D scores. Health Qual Life Outcomes. 2010;8:18.
Zhang Y, Sun J, Pang Z, Wang X, Gao W, Ning F, et al. The impact of new screen-detected and previously known type 2 diabetes on health-related quality of life: a population-based study in Qingdao, China. Qual Life Res. 2014;23(8):2319–26.
Roglic G, Unwin N, Bennett PH, Mathers C, Tuomilehto J, Nag S, et al. The burden of mortality attributable to diabetes: realistic estimates for the year 2000. Diabetes Care. 2005;28(9):2130–5.
American Diabetes Association. Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31(3):596–615.
Schmitt-Koopmann I, Schwenkglenks M, Spinas GA, Szucs TD. Direct medical costs of type 2 diabetes and its complications in Switzerland. Eur J Public Health. 2004;14(1):3–9.
International Diabetes Federation. IDF DIABETES ATLAS sixth edition. 2013. Available at: https://www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdf. Accessed 11 Nov 2014.
Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(3):293–301.
Liu M, Zhang Q, Lu M, Kwon CS, Quan H. Rural and urban disparity in health services utilization in China. Med Care. 2007;45(8):767–74.
Wang H, Xu T, Xu J. Factors contributing to high costs and inequality in China’s health care system. JAMA. 2007;298(16):1928–30.
Ling RE, Liu F, Lu XQ, Wang W. Emerging issues in public health: a perspective on China’s healthcare system. Public Health. 2011;125(1):9–14.
Mahmood MA, Raulli A, Yan W, Dong H, Aiguo Z, Ping D. Cooperative medical insurance and the cost of care in Shandong, PR China: perspectives of patients and community members. Asia Pac J Public Health. 2015;27(2):NP897–902.
WHO/IDF Consultation. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/International Diabetes Federation Consultation; 2006.
Lin JD, Zhang L, Xu ZZ, Xu LC. Research on burden of chronic diseases among rural–urban residents in Xuzhou. Public Health. 2010;124(6):345–9.
Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V, et al. Increasing expenditure on health care incurred by diabetic subjects in a developing country: a study from India. Diabetes Care. 2007;30(2):252–6.
Wang W, Fu CW, Pan CY, Chen W, Zhan S, Luan R, et al. How do type 2 diabetes mellitus-related chronic complications impact direct medical cost in four major cities of urban China? Value Health. 2009;12(6):923–9.
Goldhaber-Fiebert JD, Li H, Ratanawijitrasin S, Vidyasagar S, Wang XY, Aljunid S, et al. Inpatient treatment of diabetic patients in Asia: evidence from India, China, Thailand and Malaysia. Diabet Med. 2010;27(1):101–8.
National Bureau of Statistics China, 2008. Available from http://www.stats.gov.cn/ . Accessed 21/12 2010.
Shi L. Health care in China: a rural–urban comparison after the socioeconomic reforms. Bull World Health Organ. 1993;71(6):723–36.
Jonsson B. CODE-2 Advisory Board. Revealing the cost of type II diabetes in Europe. Diabetologia. 2002;45(7):S5–S12.
TLV (the dental and pharmaceutical benefits agency) 2010; Available at: http://www.tlv.se/beslut/sok/lakemedel/. Accessed 21/12, 2010.
The common European Drug database(CEDD) [article online], 2010. Available from http://cedd.oep.hu/. Accessed 21/12 2010.
The World Bank, 2010; Available at: http://data.worldbank.org/indicator/NY.GDP.PCAP.CD. Accessed 21/12, 2010.
Acknowledgments
The data analysis and manuscript draft were supported by a grant from Academy of Finland (129197).
Conflict of interest
The authors declare that there are no conflicts of interest.
Authors’ contributions
Y.L Zhang designed the concept, analyzed data, and drafted the manuscript. Q Qing designed the concept, provided financial support to the work, and reviewed the manuscript. X.Y Wang, J Wang, and Y.W Li contributed to data collection. H Sintonen provided supervision, technical support, reviewed and edited the manuscript. All authors have seen and approved the final version.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Y., Wang, X., Sintonen, H. et al. Imbalance in inpatient costs between urban and rural diabetes patients in Jinan, China. Int J Diabetes Dev Ctries 35 (Suppl 2), 248–252 (2015). https://doi.org/10.1007/s13410-015-0371-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-015-0371-7