Abstract
Aims
To examine and compare health-related quality of life (HRQoL) in people with previously known diabetes, new screen-detected asymptomatic diabetes and people without diabetes.
Methods
HRQoL of 4,613 individuals who participated in a population-based cross-sectional diabetes survey in Qingdao, China, in 2009, was assessed using the 15D instrument. A Tobit regression model to estimate the effects of diabetes on HRQoL separate from effects of other health determinants was constructed.
Results
Among the surveyed population, 220 (4.8 %) individuals had previously known diabetes and 531 (11.5 %) individuals had new screen-detected diabetes, defined by fasting plasma glucose ≥7.0 mmol/l and/or 2-h plasma glucose ≥11.1 mmol/l. The age-, gender-, and BMI-adjusted mean 15D score of people without diabetes, with new screen-detected diabetes, and previously known diabetes was 0.975, 0.975, and 0.964, respectively, for urban and 0.971, 0.972, and 0.960, respectively, for rural participants. HRQoL overall and on all the dimensions (p < 0.05) except for hearing, eating, and speech was worse in the people with previously known diabetes compared to those with new screen-detected diabetes and those without diabetes. Compared to people without diabetes, people with new screen-detected diabetes were worse off on the dimension of usual activities (p < 0.05). After adjusting for comorbid diseases and other confounders, the impact of diabetes on reduced HRQoL was diminished.
Conclusion
Health-related quality of life was impaired in people with previously known diabetes who had co-morbid conditions, but was largely unaltered in people with newly detected asymptomatic diabetes as compared to people without diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Health-related quality of life (HRQoL) is a multidimensional concept, which measures the individual’s “total welfare” including physical, mental, and social functionality. It measures the burden of disease from the patients’ functionality perspective including the subjective experience, instead of the traditional concept based on clinical outcomes of morbidity or mortality. Several generic multiattribute utility systems, i.e., EQ-5D, SF-6D, HUI, and 15D, have been developed to assess HRQoL, which enable comparison across different diseases and help develop cost-utility analysis of interventions. The 15D instrument was developed in Finland and is the most frequently used instrument by researchers there [1, 2]. It is also considered a reasonable choice for economic analyses involving type 2 diabetes patients [3].
Prevalence of type 2 diabetes is increasing rapidly in China, and the proportion of undiagnosed diabetes is high (50–80 % of the diabetes population) [4, 5]. Care of diabetes and its complications impose a heavy economic burden on patients’ families, health care systems, and national economies. Type 2 diabetes is associated with high rates of mortality from co-morbid cardiovascular disease and is the leading cause of blindness and renal failure among adults [6]. Many studies have shown that people with clinically diagnosed type 2 diabetes have worse HRQoL than people without diabetes [7, 8], but whether HRQoL is impaired in new screen-detected asymptomatic diabetes has not been studied. The purpose of this study was to examine the HRQoL in people with previously known diabetes and new screen-detected asymptomatic diabetes as compared to people without diabetes in a population-based study in Qingdao, China.
Participants and methods
Study population
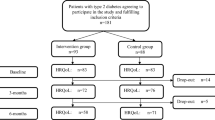
Between April 2009 and December 2011, a cross-sectional population-based diabetes survey was conducted in three urban districts (Shinan, Shibei, Sifang) and three rural districts (Jiaonan, Huangdao, Jimo) in Qingdao, China. Five communities (or villages) from each districts and 200–250 residents aged 35–74 years living in the targeted communities for at least 5 years were selected through random stratification proportional to the age and gender distribution of the population. About 5,110 of the 7,612 randomly selected individuals invited for the study participated in the survey, giving a response rate of 67.1 %. For inclusion in the current data analysis, the following criteria had to be satisfied: (1) previously confirmed known diagnosis of diabetes in spite of current blood glucose levels; (2) availability of valid blood glucose values based on the standard 2-h 75-g oral glucose tolerance test (OGTT) performed during the survey; (3) valid and completed 15D questionnaire; and (4) no data missing for the variables of interest. A total of 4,613 individuals met the inclusion criteria further reducing the sample size by 9.7 % (497 of 5,110).
All participants were interviewed by a trained survey team consisting of doctors and nurses at the local survey sites. Height and weight were measured with the participants wearing only light clothes and without shoes. In surveys carried out in winter time, the weight of clothes was reduced by around 1 or 2 kg from the measured weight of individuals depending on the woolens they wore. The body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared (kg/m2). Family history of diabetes was defined as at least one first degree relative having diabetes. Education was classified as ≥9 or <9 school years. Personal monthly income was classified as income ≥¥1,000/month or <¥999/month (¥: Chinese Yuan, 1€ ≈ 8.5¥). In our original questionnaire of survey, there were six categories for personal monthly income: (1) <¥300, (2) ¥300–¥599, (3) ¥600–¥999, (4) ¥1,000–¥1,999), (5) ¥2,000–¥2,999, and (6) ≥¥3,000. ¥1,000–¥1,999 per month is a median income category and arbitrarily chosen as a cutoff value to dichotomies study. Smoking status was classified as current smokers (smoking everyday) or non-smokers (including ex-smokers and occasional smokers). Alcohol consumption status was defined as regular drinkers or non-drinkers (including ex-drinkers and occasional drinkers). All information was recorded on standard paper-based questionnaires during the interview.
After an overnight fast, all participants except those with known diagnosis of diabetes underwent a standard 75-g oral glucose tolerance test (OGTT). Plasma glucose was determined by the glucose oxidase method, and fasting plasma triglycerides, total, and high-density lipoprotein cholesterol (HDL-C) were determined using the enzymatic method.
Previously known diabetes was confirmed by an examiner at the survey site based on the prior history of a diagnosis of diabetes or receiving anti-diabetic treatment. New screen-detected diabetes was defined as fasting plasma glucose (FPG) ≥7.0 mmol/l and/or 2-h plasma glucose (2hPG) ≥11.1 mmol/l among participants without a prior history of diabetes. Non-diabetes was defined as FPG < 7.0 mmol/l and 2hPG < 11.1 mmol/l. Newly detected hypertension was defined as blood pressure ≥140/90 mmHg, excluding individuals with a prior history of a diagnosis of hypertension or receiving antihypertensive treatment. Based on the criteria for dyslipidemia by the European guidelines on cardiovascular disease prevention (Version 2012) [9], elevated triglycerides (TG) were defined as TG ≥ 1.7 mmol/l. Reduced high-density lipoprotein cholesterol (HDL-C) was defined as HDL-C < 1.0 mmol/l for men and <1.2 mmol/l for women. Newly detected dyslipidemia was defined as elevated TG and/or reduced HDL-C excluding individuals with a prior history of dyslipidemia or lipid-lowering treatment. Impaired renal function was defined as a glomerular filtration rate (GFR) <60 ml/min/1.73 m2. GFR was calculated using the formula:
Self-reported history of diseases including hypertension, dyslipidemia, kidney disease, eye disease, and cardiovascular disease were recorded separately to differentiate from the same conditions identified through survey examination, with the assumption that the impact of a self-reported condition on HRQoL might be stronger than that of an asymptomatic morbid condition of the same diagnosis.
HRQoL measurement
Health-related quality of life was measured using the 15D—a generic, multidimensional, self-assessment tool, which can also be used in an interview—and proxy administration setting [10]. It can be used both as a profile and single index score measure. The 15D utility system consists of 15 dimensions: mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality, and sexual activity. Each dimension is divided into five ordinal levels, by which more or less the attribute is distinguished. The single index score (15D score), representing the overall HRQoL on a 0–1 scale (1 = full health, 0 = being dead), is calculated from the health state descriptive system using a set of population-based preference or utility weights. Weight for each level of each dimension is obtained by multiplying the level value by the importance weight of the dimension at that level. The level values on a 0–1 scale reflect the goodness of the levels relative to no problems on the dimension and to being dead. The importance weights summing up to unity have been elicited earlier from representative population samples.
The 15D questionnaire usually takes 5–10 min to complete. A Chinese version of 15D questionnaire was developed in consultation with the 15D developer (Harri Sintonen) and validated among Chinese individuals with a range of glucose tolerance status before it was administrated to the survey participants.
The 15D questionnaire was interviewer-administrated to all participants, and 78 % of participants (3,582/4,613) completed the questionnaire without any missing answers. Deriving the 15D score with the valuation algorithm requires a response to each question (dimension). We used the data imputation procedure to replace the missing data in the remaining questionnaires, as recommended by the 15D instrument developer; with this procedure, the probability of getting the level of the dependent variable right is 70–80 % [11]. After replacing missing answers, all the participants had completed 15D scores in the current analysis.
Statistical and sensitivity analyses
A Tobit (censored regression) model [12] was constructed to assess the effect of new screen-detected diabetes and previously known diabetes, controlling for confounding effects of age, gender, BMI, urban/rural residence, income, education, smoking and drinking habit, and comorbid conditions. The Tobit regression model is suitable for the current analysis because of two reasons. First, the distribution of the dependent variable (15D score) is skewed and censored at 0 and 1. Second, 54.3 % of observations in our study were at the upper limit of 1. The Tobit regression model has superior performance in the analysis of continuous measures of health status with a ceiling effect [12]. Modeling was performed with LIMDEP 8.0 econometric software.
The mean 15D score between the two groups was compared using independent samples T-test. Differences between the groups in other categorical variables were tested with the Pearson Chi-square test, and continuous variable was tested with one-way analysis of variance (ANOVA) and post hoc multiple comparisons based on the least significant difference (L-S-D), with statistical significance defined as a two-tailed p value <0.05. All statistics were performed using PASW statistics (version 18.0.2, Chicago: SPSS Inc.; April 2, 2010).
To ascertain that the results were not biased because of the 15D data imputation in some cases with incomplete questionnaires, a sensitivity analysis was performed to evaluate the HRQoL of individuals who had fully completed the 15D questionnaire. We also compared the characteristics of excluded and included participants to check whether the inclusion criteria had introduced any selection bias.
Results
Among 4,613 participants, 220 (4.8 %) individuals had previously known diabetes and 531 (11.5 %) individuals had new screen-detected diabetes. Participants with diabetes were older and more frequently had a positive family history of diabetes and related comorbidities than people without diabetes. Hypertension and dyslipidemia were the most common comorbid conditions. The socio-economic status was better among urban participants than rural participants. After adjusting for age, gender, and BMI using the Tobit model, the mean 15D score of people without diabetes, with new screen-detected diabetes, and previously known diabetes was 0.975, 0.975, and 0.964, respectively, for urban and 0.971, 0.972, and 0.960, respectively, for rural participants (Table 1). There was no statistically significant difference in HRQoL between urban and rural participants (p > 0.05).
As expected, the 15D score declined with age. The mean 15D score was significantly lower for people with previously known diabetes than for people without diabetes in the age group of 66–75 years in urban and in the age ≥56 years in rural (p < 0.05) (Table 2). People with previously known diabetes had a relatively lower HRQoL compared to those with new screen-detected diabetes and without diabetes on all the dimensions (p < 0.05) except for hearing, eating, and speech (Fig. 1). There was no significant difference in the mean 15D score between people without diabetes and with new screen-detected diabetes (p > 0.05) in all age groups, except that people with new screen-detected diabetes had lower scores on the dimension of usual activities (p < 0.05) (Fig. 1).
The 15D profiles of participants stratified by diabetes status, estimated mean using Tobit model adjusted for age, gender, and BMI. *p > 0.05 between people with previously known diabetes and new screen-detected diabetes/without diabetes. + p < 0.05 between people with new screen-detected diabetes and without diabetes
In univariate Tobit analysis, the mean 15D score of people with diabetes was impaired, but the impact was diminished after adjustment for comorbid diseases and other confounders (Table 3). Gender, urban/rural residence, BMI, drinking habit, hypertension, and dyslipidemia identified through survey examination were not significantly associated with HRQoL in this population and were not entered into the final multivariate model. Self-reported history of dyslipidemia (β coefficient −0.009), kidney disease (−0.020), eye disease (−0.011), and cardiovascular disease (−0.010) remained in the final model and were negatively associated with the HRQoL score (p < 0.01, all). Aging, low education, and low income also reduced the HRQoL (Table 3).
Sensitivity analysis
The completion rate of 15D questionnaire ranged from 98.8 % in age group of 34–45 years to 42.6 % in age group of 66–75 years. Younger people tended to answer the 15D questionnaire more completely than older people. As expected, people with complete initial answers had lower prevalence of previously known diabetes (3.8 vs. 8.2 %, p < 0.001), new screen-detected diabetes (9.7 vs. 17.7 %, p < 0.001), and other co-morbidities than those who had missing answers, but did not differ in gender distribution, mean BMI, smoking, and drinking status. Before data imputation, the age-, gender-, and BMI-adjusted mean of 15D score in people without diabetes, with new screen-detected diabetes, and with previously known diabetes was 0.969, 0.969, and 0.955, respectively, for the urban participants and 0.970, 0.969, and 0.956, respectively, for the rural participants. The mean of 15D score with and without imputation was quite similar.
To ascertain if the inclusion criteria had introduced selection bias, we compared the baseline characteristics of individuals excluded and included from the final data analysis. The individuals who met the strict inclusion criteria were not different from those who did not meet the criteria with regard to mean age, gender, BMI, fasting capillary blood glucose, and prevalence of all the other comorbidities, so the results were unlikely to be biased by the inclusion criteria applied in the study.
Discussion
To our knowledge, this is the first large population study using preference-based instrument to investigate differences in HRQoL in people without diabetes, with new screen-detected, and previously known diabetes in China. Little was known from previous studies whether the HRQoL begins to diminish among asymptomatic people with undetected diabetes.
Although there are no comparable studies in China, our findings are consistent with previous studies describing the burden of previously known diabetes on HRQoL and newly diagnosed diabetes in some dimensions. A study using the Nottingham Health Profile instrument to evaluate HRQoL among 259 Finns aged 73 or older found that people with previously known diabetes had worse HRQoL than subjects with undiagnosed diabetes or prediabetes. The HRQoL was similar in undiagnosed diabetes, prediabetes, and normal glucose tolerance groups [13]. Another population-based cross-sectional study in Western Finland conducted among the healthy individuals aged 45–70 found that newly diagnosed diabetes impaired HRQoL on three of eight dimensions (general health, physical functioning, and emotional role limitation) of SF-36 compared to subjects with normal glucose tolerance [14]. Two studies from Australia (AusDiab) have shown that previously diagnosed diabetes is associated with a reduced HRQoL on each dimension of the SF-36, but the association is attenuated after adjustment for age, gender, BMI, and treatment for hypertension and lipid abnormalities. Among those with newly diagnosed diabetes detected by OGTT, HRQoL was also reduced on some dimensions of the SF-36 [15, 16].
People with long-standing type 2 diabetes are more likely to have history of comorbid diseases compared to people with screen-detected diabetes and those without diabetes. Our study found that self-reported symptomatic comorbid conditions such as cardiovascular disease, kidney disease, and eye disease had a strong negative impact on HRQoL. Hypertension and dyslipidemia were very common in the citizen of Qingdao as shown in this study and in our previous studies [17, 18]. Most of the people with hypertension and/or dyslipidemia were asymptomatic and unaware of their conditions before the survey. These people’s daily life and activities were not affected by these hitherto undiagnosed comorbid conditions. They considered themselves as healthy as the others without these conditions. These findings are also consistent with previous studies which show that the presence of comorbid conditions such as heart disease or stroke leads to lower HRQoL scores compared to type 2 diabetes alone [19], and people suffering from diabetes and hypertension had similar HRQoL as people with diabetes without comorbidities [20]. Self-reported symptomatic comorbid conditions were more strongly associated with lower quality of life than asymptomatic conditions [21]. Chronic long-term drug consumption, frequent visits to doctor, and dietary restrictions may affect these people’s quality of life as much as the consequence of the disease itself. The overall mean of HRQoL score was not different between people without diabetes and people with new screen-detected asymptomatic diabetes; however, the mean usual activity score was lower in the latter, probably due to the clustering and prior presence of obesity, hypertension, dyslipidemia, etc., with asymptomatic and as yet undetected hyperglycemia.
Numerous social-demographic factors and culture/ethnicity differences influence the HRQoL. Education and income were associated with HRQoL in our study. Poor quality of life is likely to be associated with low education or low income, and it may also increase the likelihood of developing type 2 diabetes [22]. Type 2 diabetes may cause poor quality of life and may impose a heavy economic burden leading to poverty. Many studies have suggested that Chinese individuals consider their health quality subjectively better [23, 24]. In our study population with a mean age of 52 years, the mean 15D score was 0.969 and 54.3 % of population reported full health. In a representative Finnish population sample, whose mean age was 53 years, the mean 15D score was 0.910 with only 15 % respondents reporting full health [25]. The difference does not necessarily mean that the general health of Chinese people is objectively much better than that of Finns. The differences in culture, expectations, interpretation of life and happiness, living standard and environment, access to medical care and other social circumstances influence the perceptions of health.
Strengths and weaknesses of various statistical approaches used to model censored HRQoL score have been evaluated and discussed over recent years [13, 26, 27]. The Tobit regression model is a frequently used tool for modeling censored variables. The censored least absolute deviations (CLAD) regression has been proposed as a robust alternative. In our study, both approaches were compared and the results showed they have a good agreement. Another study used both Tobit and CLAD regression to investigate the impact of 29 chronic conditions on HRQoL measured by the 15D instrument. The estimates of regression coefficient of the two models were similar, and the differences did not exceed the minimal clinically important change of 0.03 [25].
The response rate of our survey was 67.1 %; non-participants were slightly younger (50 vs. 52 years old) and more men (52 vs. 40 %) than the participants. There was no large difference in urban/rural distribution between participants and non-participants (72 % of participants vs. 73 % of non-participants from rural areas). Given the large sample size, and a random cluster sampling approach including both rural and urban areas, our study population is fairly representative of the population of Qingdao, China, and the results may be applicable to other parts of China with similar socio-economic status. In the 15D questionnaire, we considered answers “do not know” as missing. Most missing data occurred on the dimension of sexual activity, and discussing sexual activity is cultural taboo in China. In addition, a relatively high proportion of the elderly people could not complete the 15D questionnaire due to lower education and poor understanding of the questions.
Our study was cross-sectional in design. Whether a new diagnosis of diabetes can have a negative impact on individuals’ perception of their well-being over the years after screening is still unknown in China. Whether screen diagnosis and early detection and better care will prevent inevitable deterioration in HRQoL can only be answered through a longitudinal study, which evaluates the changes in HRQoL over time among the people with new screen diagnosed diabetes compared to people without diabetes.
Conclusion
HRQoL was impaired in people with previously known diabetes who had co-morbid conditions, but was largely unaltered in people with newly detected asymptomatic diabetes as compared to people without diabetes.
References
Hahl, J., Hamalainen, H., Sintonen, H., Simell, T., Arinen, S., & Simell, O. (2002). Health-related quality of life in type 1 diabetes without or with symptoms of long-term complications. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 11(5), 427–436.
Ahola, A. J., Saraheimo, M., Forsblom, C., Hietala, K., Sintonen, H., Groop, P. H., et al. (2010). Health-related quality of life in patients with type 1 diabetes—association with diabetic complications (the FinnDiane Study). Nephrology, Dialysis, Transplantation: Official Publication of the European Dialysis and Transplant Association—European Renal Association, 25(6), 1903–1908.
Kontodimopoulos, N., Pappa, E., Chadjiapostolou, Z., Arvanitaki, E., Papadopoulos, A. A., & Niakas, D. (2012). Comparing the sensitivity of EQ-5D, SF-6D and 15D utilities to the specific effect of diabetic complications. The European Journal of Health Economics: HEPAC: Health Economics in Prevention and Care, 13(1), 111–120.
Yang, W., Lu, J., Weng, J., Jia, W., Ji, L., Xiao, J., et al. (2010). Prevalence of diabetes among men and women in China. The New England journal of medicine, 362(12), 1090–1101.
Dong, Y., Gao, W., Nan, H., Yu, H., Li, F., Duan, W., et al. (2005). Prevalence of Type 2 diabetes in urban and rural Chinese populations in Qingdao, China. Diabetic Medicine: A Journal of the British Diabetic Association, 22(10), 1427–1433.
Fradkin, E. J. (2012). Confronting the urgent challenge of diabetes: An overview. Health Affairs, 31(1), 12.
Alonso, J., Ferrer, M., Gandek, B., Ware, J. E, Jr, Aaronson, N. K., Mosconi, P., et al. (2004). Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 13(2), 283–298.
Choi, Y. J., Lee, M. S., An, S. Y., Kim, T. H., Han, S. J., Kim, H. J., et al. (2011). The relationship between diabetes mellitus and health-related quality of life in Korean adults: The Fourth Korea National Health and Nutrition Examination Survey (2007–2009). Diabetes & Metabolism Journal, 35(6), 587–594.
Perk, J., De Backer, G., Gohlke, H., Graham, I., Reiner, Z., Verschuren, W. M., et al. (2012). European guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). International Journal of Behavioral Medicine, 19(4), 403–488.
Sintonen, H. (2001). The 15D instrument of health-related quality of life: Properties and applications. Annals of Medicine, 33(5), 328–336.
Sintonen, H. (1994). The 15D-measure of health-related quality of life. I. Reliability, validity and sensitivity of its health state descriptive system. National Centre for Health Program Evaluation, working paper 41, Melbourne. http://www.buseco.monash.edu.au/centres/che/pubs/wp41.pdf.
Austin, P. C., Escobar, M., & Kopec, J. A. (2000). The use of the Tobit model for analyzing measures of health status. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 9(8), 901–910.
Hiltunen, L., & Keinanen-Kiukaanniemi, S. (1999). Does glucose tolerance affect quality of life in an elderly population? Diabetes Research and Clinical Practice, 46(2), 161–167.
Seppala, T., Saxen, U., Kautiainen, H., Jarvenpaa, S., & Korhonen, P. E. (2013). Impaired glucose metabolism and health related quality of life. Primary Care Diabetes, 7(3), 223–227.
Tapp, R. J., Dunstan, D. W., Phillips, P., Tonkin, A., Zimmet, P. Z., Shaw, J. E., et al. (2006). Association between impaired glucose metabolism and quality of life: Results from the Australian diabetes obesity and lifestyle study. Diabetes Research and Clinical Practice, 74(2), 154–161.
Tapp, R. J., O’Neil, A., Shaw, J. E., Zimmet, P. Z., Oldenburg, B. F., & AusDiab Study Group. (2010). Is there a link between components of health-related functioning and incident impaired glucose metabolism and type 2 diabetes? The Australian Diabetes Obesity and Lifestyle (AusDiab) study. Diabetes Care, 33(4), 757–762.
Zhou, X., Pang, Z., Gao, W., Wang, S., Zhang, L., Ning, F., et al. (2010). Performance of an A1C and fasting capillary blood glucose test for screening newly diagnosed diabetes and pre-diabetes defined by an oral glucose tolerance test in Qingdao, China. Diabetes Care, 33(3), 545–550.
Ning, F., Pang, Z. C., Dong, Y. H., Gao, W. G., Nan, H. R., Wang, S. J., et al. (2009). Risk factors associated with the dramatic increase in the prevalence of diabetes in the adult Chinese population in Qingdao, China. Diabetic Medicine: A Journal of the British Diabetic Association, 26(9), 855–863.
Maddigan, S. L., Feeny, D. H., & Johnson, J. A. (2005). Health-related quality of life deficits associated with diabetes and comorbidities in a Canadian National Population Health Survey. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 14(5), 1311–1320.
Miksch, A., Hermann, K., Rolz, A., Joos, S., Szecsenyi, J., Ose, D., et al. (2009). Additional impact of concomitant hypertension and osteoarthritis on quality of life among patients with type 2 diabetes in primary care in Germany—A cross-sectional survey. Health and Quality of Life Outcomes, 7, 19.
Wexler, D. J., Grant, R. W., Wittenberg, E., Bosch, J. L., Cagliero, E., Delahanty, L., et al. (2006). Correlates of health-related quality of life in type 2 diabetes. Diabetologia, 49(7), 1489–1497.
Kazemi-Galougahi, M. H., Ghaziani, H. N., Ardebili, H. E., & Mahmoudi, M. (2012). Quality of life in type 2 diabetic patients and related effective factors. Indian Journal of Medical Sciences, 66(9–10), 230–237.
Avis, N. E., Ory, M., Matthews, K. A., Schocken, M., Bromberger, J., & Colvin, A. (2003). Health-related quality of life in a multiethnic sample of middle-aged women: Study of Women’s Health Across the Nation (SWAN). Medical Care, 41(11), 1262–1276.
Wang, H., Kindig, D. A., & Mullahy, J. (2005). Variation in Chinese population health related quality of life: Results from a EuroQol study in Beijing, China. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 14(1), 119–132.
Saarni, S. I., Harkanen, T., Sintonen, H., Suvisaari, J., Koskinen, S., Aromaa, A., et al. (2006). The impact of 29 chronic conditions on health-related quality of life: A general population survey in Finland using 15D and EQ-5D. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 15(8), 1403–1414.
Austin, P. C. (2002). A comparison of methods for analyzing health-related quality-of-life measures. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 5(4), 329–337.
Sullivan, P. W., Lawrence, W. F., & Ghushchyan, V. (2005). A national catalog of preference-based scores for chronic conditions in the United States. Medical Care, 43(7), 736–749.
Acknowledgments
The studies were designed and organized by researchers from the University of Helsinki, Helsinki, Finland; Qingdao Municipal Centers for Disease Control and Prevention (CDC), and the Qingdao Endocrinology and Diabetes Hospital and Institute, Qingdao, China. The field investigation of the surveys was supported by the Qingdao Municipal Health Bureau, the Qingdao Municipal Centers for Disease Control and Prevention, and local Health Bureau and CDC in Huangdao, Jiaonan, Shinan, Shibei, Jimo and Sifang districts.
Conflict of interest
Harri Sintonen is the developer of the 15D. The others have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yanlei Zhang and Jianping Sun have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, Y., Sun, J., Pang, Z. et al. The impact of new screen-detected and previously known type 2 diabetes on health-related quality of life: a population-based study in Qingdao, China. Qual Life Res 23, 2319–2326 (2014). https://doi.org/10.1007/s11136-014-0674-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-014-0674-z