Abstract
Background
Epidermal growth factor receptor (EGFR) gene mutations are recurrently observed in non-small cell lung carcinomas (NSCLCs), and it has been found that they may serve as specific therapeutic targets. The aim of the present study was to determine the prevalence of EGFR gene mutations in NSCLCs in an East European (Bulgarian) population in different histological subtypes, in cytological versus histological samples and in primary versus metastatic lesions.
Methods
In this study 1427 NSCLC samples were included. DNA was extracted from either formalin-fixed paraffin embedded (FFPE) tissues or cytology specimens and analyzed for the presence of 29 recurrent EGFR gene mutations using SARMS PCR.
Results
EGFR gene mutations were found to occur significantly more often in female than in male patients (19.4 % vs. 5.4 %; p < 0.001), in adenocarcinomas than in squamous cell carcinomas or other histological subtypes (12.5 % vs. 6.2 %, and 7.6 %, respectively; p = 0.009), and in never smokers than in ex-smokers and current smokers (22.9 % vs. 8.5 % and 4.9 %, respectively; p < 0.001). No significant differences were observed in the occurrence of EGFR gene mutations in primary tumors compared to metastases (7.9 % vs. 11.2 %; p = 0.092), or in FFPE samples compared to cytological samples (8.9 % vs. 8.1 %; p = 0.813).
Conclusions
Our data show that the overall frequency of EGFR gene mutations in lung adenocarcinomas in the East European cohort studied is within the range of that observed in North American and West European populations, but that its frequency in squamous cell carcinomas is higher than that in any population reported to date. All specimens appeared to be suitable for EGFR gene mutation analysis, irrespective nature or origin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Lung cancer is the leading cause of cancer mortality worldwide and is responsible for ∼1.3 million deaths per year [1, 2]. The lung cancer survival rates vary widely, mainly depending on histological subtype and stage. The overall prognosis is better when diagnosed at earlier stages but, as yet, there are no effective methods for the early detection of lung cancer. The treatment in advanced stages is often unsuccessful [3, 4]. Despite the progress that has been made in treatment options and the research efforts that have been made to reach this goal, the prognosis for lung cancer still remains poor. Thus, there is a continuing need for the development of more effective diagnostic and therapeutic strategies [5–7]. Non-small cell lung carcinomas (NSCLCs) comprise approximately 85 % of all lung cancer cases [4]. According to the WHO classification the most frequent NSCLCs are adenocarcinoma (ADC), squamous cell carcinoma (SCC) and large cell carcinoma (LCC) [8]. In Bulgaria, lung cancer is the number one killer and annually ∼4000 new cases are registered, representing 13 % of the total cancer incidence. Only 75 % of the cases are morphologically confirmed, mainly SCC and ADC and, unfortunately, 76 % of the patients are already in stage III or IV at the time of diagnosis [9].
According to previous reports, activating mutations in exons 18–21 of the epidermal growth factor receptor gene (EGFR), encoding its tyrosine kinase domain, correlate with positive responses to treatment with tyrosine kinase inhibitors (TKIs) such as gefitinib and erlotinib, the first EGFR targeted therapy approved by the FDA for the treatment of NSCLCs [10–14]. To date, EGFR gene mutation profiles have been reported for several Asian and Caucasian populations [11, 15], predominantly from East Asia and North America, showing large differences between these populations. As yet, however, no such profiles have been reported for East European populations. Previous studies have shown that EGFR gene mutations that are predictive for responses to TKI inhibitors occur more frequently in female patients, in never smokers and in patients with ADCs [16–18]. Usually the tissues studied were derived from primary locations, implying that associations between EGFR gene mutations and different metastatic sites have so far not been studied very well. Recently, Smits et al. [19] failed to observe any significant difference in the frequency of EGFR gene mutations in primary lung ADCs (n = 360) versus different metastatic lesions (n = 261). They did, however, find that patients with malignant effusions and those with brain metastases exhibited an increased frequency (trend) in EGFR gene mutations. Another under-explored issue is sample suitability, i.e., the question whether cytology samples are equally well-suited as formalin-fixed paraffin embedded (FFPE) tissue samples for EGFR mutation analysis.
The aim of the present study was to determine the prevalence of the most recurrent EGFR gene mutations (29 selected mutations) in NSCLCs in an East European (Bulgarian) population in different histological subtypes, in cytological versus histological samples and in primary versus metastatic lesions.
2 Materials and methods
2.1 Patients and samples
We had included 1427 consecutive patients in our study for a period of 3 years starting from February 2010 to May 2013. The study was cross-sectional and the analyses were performed at the time of diagnosis of the patients (stage III or IV) or when metastases or relapses were detected when monitoring the patients in stage I or II. All studied materials were taken as part of routine diagnostic procedures before starting treatment of the patient. Samples from patients from all over the country were included. The participating hospitals were: University hospital for lung diseases “St. Sofia” - Sofia, Military medical academy - Sofia, National oncology hospital - Sofia, University hospital “Tsaritsa Yoanna - ISUL” - Sofia, “Serdika” hospital - Sofia, “Pirogov” hospital - Sofia, Tokuda university hospital - Sofia, Lozenets university hospital - Sofia; Complex Oncology Center - Vratsa, Complex Oncology Center - Pleven, University hospital “Georgi Stranski” - Pleven, “Avis medica” hospital - Pleven, Complex Oncology Center - Plovdiv, University hospital “St. George” - Plovdiv, University hospital “Prof. St. Kirkovich” - Stara Zagora, Complex Oncology Center - Stara Zagora, University hospital “St. Marina” - Varna, Complex Oncology Center - Burgas, Multiprofile Hospital for Active Treatment - Haskovo, Multiprofile Hospital for Active Treatment - Blagoevgrad, Multiprofile Hospital for Active Treatment - Ruse. The study has been approved by the appropriate institutional ethical committee and informed consent was obtained from all patients.
The criteria for inclusion were: NSCLC histology, stage III or IV, and operated at stage I or II but later found to be metastatic. According to the EGFR gene mutation status, decisions were made about the future therapy of the patients. The criteria for exclusion were: non-NSCLC histology and operated at stage I or II at the time of diagnosis. An exception was made in 5 cases (2 carcinoid tumors and 3 small-cell lung carcinomas combined with large cell carcinoma) based on the insistence of the referring oncologist.
The histological diagnoses were made according to the WHO criteria for lung tumors, i.e., IVth edition of the WHO classification of lung tumors [5]. The diagnosis squamous cell carcinoma (SCC) was made when the tumor showed keratinization and/or intercellular bridges, and was positive for p63. The diagnosis adenocarcinoma (ADC) was made when the tumor showed glandular differentiation or mucin production, was showing acinar, papillary, lepidic or solid with mucin growth patterns or a mixture of these patterns, and was positive for TTF-1 and cytokeratin 7. Immunohistochemistry was performed in difficult cases (i.e., poorly differentiated NSCLCs) using TTF-1, p63, cytokeratin AE1/AE3, cytokeratin 7, synaptophisin, chromogranin A and Ki-67. The specimens were evaluated by two independent pathologists, the first from the hospital of origin of the tissue and the second from the University hospital for lung diseases “St. Sofia”. In some cases a third pathologist evaluated the specimens.
The total cohort consisted of 576 ADC cases, 676 SCC cases and 118 other tumors (i.e., 37 adenosquamous carcinomas, 18 large cell carcinomas (LCC), 18 non-small cell carcinomas not otherwise specified (NSCLC-NOS), 14 pleomorphic carcinomas, 10 combined carcinomas (ADC + SCC), 9 mucoepidermoid carcinomas, 8 adenoid cystic carcinomas, 3 small cell carcinomas combined with LCC and 2 carcinoid tumors). The samples for DNA extraction were obtained from either formalin-fixed paraffin embedded (FFPE) tissues or cytology slides, Hematoxilin and Eosin (H&E) stained. The FFPE samples were taken from lung resections, lymph node extirpations, bronchoscopic biopsies, transthoracic biopsies or biopsies from metastatic locations, i.e., bone, brain, etc. The cytology samples were taken from pleural fluids, aspiration biopsies, brush biopsies or bronchoalveolar lavages. The tumor cell populations varied from 1 to 90 %, depending on the sample. The patients’ clinicopathological details are listed in Table 1. In some of the cases no information was available for (i) histology subtype, i.e., 56 cases with unspecified NSCLC histology (further sub-classification was not possible due to lack of material), (ii) TNM stage, in 179 cases, (iii) smoking history, in 139 cases and (iv) location, in 75 cases. All these cases were excluded from further analyses. Information on number of pack-years was available for 779 of 1096 former/current smokers.
2.2 DNA extraction
DNA extraction and mutation analyses were performed in the National Genetic Laboratory, Sofia. In case of FFPE samples, 4 or 6 10 μm sections were taken according to the percentage of tumor cells present in the samples, i.e., above 50 % or below 50 %, respectively. Macro-dissections were performed on surgical samples only. For the cytological samples only H&E stained slides were available. In the cytological samples the percentages of tumor cells varied from 1 to 25 %. For the DNA extractions we used the slides with the highest percentages of tumor cells. In all cases, DNA was extracted using the QIAamp DNA FFPE Tissue Kit® (Qiagen), which is specifically designed for the isolation and purification of high quality DNA from FFPE tissues (methodology according to the manufacturer’s instructions). For the cytological samples the deparaffinization step was omitted.
2.3 EGFR gene mutation analysis
For the EGFR gene mutation analyses we used the Scorpions Amplification Refractory Mutation System (SARMS) technology (Qiagen). The ARMS PCR technology combined with the Scorpions detection technology provides a better sensitivity and specificity for the detection of specific mutations than pyrosequencing and dideoxy sequencing technologies, respectively [20]. The specifically designed EGFR RGQ PCR Kit allows the detection of 29 known recurrent mutations (including the inhibitory mutation T790M) in exons 18–21 of the EGFR gene, 19 deletions in exon 19 (does not distinguish between them), T790M in exon 20, L858R in exon 21, L861Q in exon 21, G719X in exon 18 (G719S, G719A or G719C, but does not distinguish between them), S768I in exon 20 and 3 insertions in exon 20 (does not distinguish between them). See Table 2 for detailed information. The various reactions were performed according to the manufacturer’s instructions and the analyses were carried out for all the samples as described in the kit procedure. A Rotor-Gene Q MDx machine was used for performing the PCR reactions. Patients were considered to be positive if 1 of the 28 activating EGFR mutations was detected. A separate analysis was performed for patients with the TKI inhibitory mutation T790M.
2.4 Statistical analysis
The data were analyzed using SPSS software, version 13.0 for Windows. Associations between EGFR gene mutation status and patient and tumor characteristics were analyzed using a χ2 test. Binary logistic regression analysis (univariate) was used to compare the EGFR gene mutation frequencies of metastases and primary tumors. Odds ratios (OR) and 95 % confidence intervals (CI) were calculated. A multivariate logistic regression analysis was performed to test the influence of all main variables (gender, age, smoking history, TNM stage, sample type, location) on the EGFR gene mutation status (tumors positive for activating mutations, excluding the inhibitory T790M mutation) of the ADC and SCC samples (separately). In all tests, two-sided p-values less than 0.05 were considered statistically significant.
3 Results
3.1 EGFR gene mutations occur frequently in NSCLC
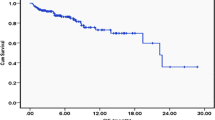
The EGFR gene mutation status was determined in 1427 samples, all derived from individual non-small cell lung cancer (NSCLC) patients. From these samples, 127 (8.9 %) were found to be positive for activating mutations in the EGFR gene: 66/127 (52 %) exhibited deletions in exon 19, 54/127 (42.5 %) exhibited a L858R point mutation in exon 21, 3/127 (2.4 %) exhibited a L861Q point mutation in exon 21, 3/127 (2.4 %) exhibited a S768I point mutation in exon 20, and 1/127 (0.8 %) exhibited a G719X point mutation in exon 18. Also, in 26/1427 (1.8 %) samples a T790M point mutation in exon 20 (associated with tyrosine kinase inhibition resistance) was detected, in none of the cases in combination with other (activating) EGFR gene mutations. The overall EGFR gene mutation frequency (including T790M) was 10.7 % (153/1427). In Fig. 1a the frequencies of the different EGFR gene mutations in the positive group, including the inhibitory T790M mutation, are summarized.
3.2 EGFR gene mutations occur predominantly in adenocarcinomas
In 1371 of the 1427 (96 %) cases included in this study the exact histological classification was established. 72 of the cases positive for activating EGFR gene mutations were diagnosed as ADC (12.5 %) and 42 were diagnosed as SCC (6.2 %). Additional activating EGFR gene mutations (n = 9) were found in 2/18 (11 %) large cell carcinomas (LCC), in 3/37 (8 %) adenosquamous (ADS) carcinomas, and in 4/18 (22 %) NSCLC-NOS. The EGFR gene mutations identified were twice as frequent in ADC than in SCC and 1.6 times as frequent in ADC than in the other histological subtypes (p = 0.009) (Table 1). The most frequently detected activating EGFR gene mutations in ADC were deletions in exon 19 (43/72 cases; 59.7 %), followed by the L858R point mutation in exon 21 (27/72 cases; 37.5 %) and the L861Q point mutation in exon 21 (2/72 cases; 2.7 %). The T790M mutation was found in 13/576 (2.3 %) of the ADC cases (Table 4; Fig. 1b). In the ADC cases, statistically significant variables affecting the mutation status in a multivariate logistic regression analysis were found to be gender (2.64 times higher in females than males; OR 2.64; CI 95 % 1.33–5.23; p = 0.005) and smoking status (3.1 times higher in non-smokers than in smokers; OR 3.10; CI 95 % 1.59–6.05; p = 0.001). In the SCCs the L858R point mutation in exon 21 was found to be most frequent (21/42 cases; 50 %), followed by deletions in exon 19 (17/42 cases; 40.5 %), the L861Q point mutation in exon 21 (1/42 cases; 2.4 %), the S768I point mutation in exon 20 (2/42 cases; 4.7 %) and the G719X point mutation in exon 18 (1/42 cases; 2.4 %). The T790M mutation was found in 13/676 (1.9 %) SCC cases (Table 4; Fig. 1c). With respect to the T790M mutation, no significant differences were found between ADC (13/563; 2.3 %) and SCC (13/673; 1.9 %) cases (p = 0.265). In the SCC cases the variables affecting the mutation status in a multivariate logistic regression analysis were gender (3.9 times higher in females than males; OR 3.91; CI 95 % 1.55–9.90; p = 0.004) and the site of biopsy (2.6 times higher in metastases than in primary carcinomas (OR 2.63, CI 95 % 1.12–6.19; p = 0.027).
3.3 EGFR gene mutations occur frequently in females and older patients
We found that the EGFR gene mutations occurred 3.6 times more frequent in female (69/355; 19.4 %) than in male (58/1072; 5.4 %) patients (p < 0.001) (Table 1), irrespective the histological subtype (Table 3). In female patients mutations in exon 19 (42/355; 11.8 %) were more frequent than mutations in exon 21 (27/355; 7.6 %) (p = 0.048). In male patients the two most frequent mutations were equally represented, i.e., exon 19 mutations (24/1072; 2.2 %) and exon 21 mutations (30/1072; 2.8 %) (p = 0.401) (Table 4). In case of the T790M mutation no gender differences were found, i.e., present in 7/355 females (2 %) and in 19/1072 males (1.8 %) (p = 0.479). The median age of the patients was 62 years. Based on this notion, we divided the patients into two groups: younger than or 62 years (n = 774) and older than 62 years (n = 653). By doing so, we found that the EGFR gene was significantly more frequently mutated in the older than 62 years group (70/653; 10.7 %) than in the younger than 62 years group (57/774; 7.4 %) (p = 0.032; Fisher’s exact test).
3.4 No association between EGFR gene mutation status and TNM stage
In 1248 cases (88 %) information regarding TNM stage was available. We found that there was no statistically significant difference between the presence of activating EGFR gene mutations or a wild type EGFR gene status and different TNM stages (p = 0.163, χ2 test). We did find, however, that EGFR gene mutations occurred more frequently (trend) in more advanced stages, i.e., in TNM stages I/II in 6/117 cases (5.1 %), in TNM stage III in 35/453 cases (7.7 %) and in TNM stage IV in 67/678 cases (9.9 %) (Table 1).
3.5 EGFR gene mutations occur frequently in never smokers
For 1288 patients (90 %) the smoking history was available. We found that the EGFR gene mutation frequency was significantly higher in never smokers (44/192; 22.9 %) than in ex-smokers (37/434; 8.5 %) and current smokers (28/662; 4.2 %) (p < 0.001). Within the group of ex-smokers and current smokers, the average number of pack-years (when available) was significantly lower in the EGFR gene mutation-positive (28.4 ± 18) than the EGFR gene mutation-negative (36.5 ± 17.7) patients (p = 0.002) (Table 1). In the non-smokers the mutations in exon 19 (25/192; 13 %) were more frequent than the mutations in exon 21 (18/192; 9.4 %) (p = 0.085), whereas in the ex-/current smokers the exon 19 mutations (31/1096; 2.8 %) were almost equal to the exon 21 mutations (33/1096; 3 %) (p = 0.320) (Table 4). For the T790M mutation no differences were found, i.e., present in 3/192 non-smokers (1.6 %) and in 21/1096 ex-/current smokers (1.9 %) (p = 0.509).
3.6 No associations between EGFR gene mutation frequencies and sample types
No significant differences were observed between the frequencies of EGFR gene mutations in formalin-fixed paraffin embedded (FFPE) histological samples (122/1365, 8.9 %) and cytological samples (5/62, 8.1 %) (p = 0.813) (Table 1).
3.7 EGFR gene mutation frequencies are similar in primary tumors and metastases
In 1352 cases (95 %) information on the site of biopsy was available. In 75 cases the origin of the biopsy (primary or metastatic) was not specified by the referring oncologist and these cases were excluded from further analysis. The EGFR gene mutation status was determined in 1083 primary tumors and 269 independent metastases. No paired primary tumor-metastasis samples were available. We divided the metastatic lesions in different categories (more than 10 cases in each category) and, by doing so, found the following rates of EGFR gene mutations: lymph node metastases in 8/104 (7.7 %) cases (OR 0.967; CI95% 0.455–2.05; p = 0.931), brain metastases in 2/42 (4.8 %) cases (OR 0.58; CI95% 0.14–2.44; p = 0.458), pleural metastases in 13/80 (16.3 %) cases (OR 2.25; CI95% 1.19–4.24; p = 0.012), pleural and pericardial effusions in 1/10 (10 %) cases (OR 1.29, CI95% 0.16–10.29, p = 0.811), bone metastasis in 3/17 (17.6 %) cases (OR 2.49; CI95% 0.70–8.82; p = 0.159) and others in 3/15 (20 %) cases (OR 2.90; CI95% 0.80–10.48; p = 0.104). The metastatic lesions showed an increase in EGFR gene mutation frequency (30/269; 11.2 %) compared to the primary tumors (86/1083; 7.9 %), but without reaching statistical significance (p = 0.092). Binary logistic regression analysis confirmed the lack of a significant difference between the primary lung tumor and metastasis groups (OR 0.684; CI95% 0.441–1.061; p = 0.090). Only pleura-derived metastases showed a statistically significant increase in EGFR gene mutations compared to primary tumors (OR 2.25; CI95% 1.19–4.24; p = 0.012). In the ADCs the metastatic lesions (19/155, 12.3 %) showed no differences in EGFR gene mutation frequencies when compared to the primary tumors (45/383, 11.7 %) (p = 0.353), but in the SCCs the metastatic lesions showed an increase in EGFR gene mutation frequency (9/79; 11.4 %) when compared to the primary tumors (32/586; 5.5 %) (p = 0.022). Logistic regression analysis of the SCCs showed a statistically significant difference only for bone metastases, i.e., 8.65 times more frequent than primary tumors (OR 8.656; CI95% 1.528–49.04; p = 0.015). In the ADCs none of the metastatic lesions showed a statistically significant EGFR gene mutation rate compared to the primary tumors.
4 Discussion
As of yet, the frequency of EGFR gene mutations in non-small cell lung carcinomas (NSCLC) has mainly been studied in East Asian, North American and in West European populations, showing large differences between these populations. To the best of our knowledge, this is the first study assessing the prevalence of EGFR gene mutations in NSCLCs in a large East European cohort. In conformity with previous studies in East Asian, North American and West European populations [16, 17, 21, 22], we found that the EGFR gene mutation rates were higher in female patients compared to male patients (19.4 % vs. 5.4 %; p < 0.001). Again, in concordance with previous studies [16, 17, 21–23], we found that gender (p < 0.001), smoking status (p < 0.001) and histological subtype (p = 0.009) are main factors affecting the EGFR gene mutation status. In the East Asian population the frequency of EGFR gene mutations varies from 36.4 to 66.3 % in ADCs, the most frequently occurring lung cancer type in this population [16, 21] and, therefore, the most studied subtype. In Bulgarian patients the most frequently occurring lung cancer type is SCC, i.e., 54 % of the morphologically confirmed cases [9]. In the North American and West European populations the EGFR gene mutation frequencies are lower, ranging from 6.0 to 14.0 % [24, 25]. In the Dutch population EGFR gene mutations were detected in 9.1 % of the samples tested, in 10.6 % of the ADC samples tested and in none of the SCC samples tested, and more frequently in female than in male patients (13.4 % vs. 5.5 %) [19]. In the Spanish population EGFR gene mutations were detected in 12 % of the samples tested, but only in ADC samples and not in SCC samples [26]. In our study, activating mutations were found in 8.9 % of the samples tested, which is in concordance with previous reports on the Caucasian population. According to a recent meta-analysis (59 studies) EGFR gene mutations occur more frequently in ADCs than in SCCs in both West European (19.2 % vs. 3.3 %) and East Asian populations (47.9 % vs. 4.6 %) [23]. Our study confirms that EGFR gene mutations occur more frequently in ADCs than in SCCs (12.5 % vs. 6.2 %, p < 0.001).
So far, most reported studies have primarily focussed on ADCs, and only a few studies have evaluated the frequency of EGFR gene mutations in non-adenocarcinoma NSCLCs, such as SCCs. In these latter studies, EGFR gene mutations were observed in 0 % to 3 % of the SCCs studied [17, 27–31]. Miyamae et al. [5] found that 3/87 SCCs tested (3.4 %) carried EGFR gene mutations. In Bulgaria, SCC is the predominant histological NSCLC subtype [9]. We evaluated one of the largest SSC cohorts reported to date, encompassing 676 patients. In a recent meta-analysis 334 SCCs from a Western European population (3.3 % with an EGFR gene mutation) and 474 SCCs from an East Asian population (4.6 % with EGFR gene mutation) were included [23]. We found that 6.2 % of our SCC patients exhibited activating EGFR gene mutations, which is almost twice that observed in other studies. This difference may be due to differences in environmental factors, smoking habits and/or cohort sizes. In our current study, no differences in the prevalence of EGFR gene mutation-positive lung cancers and TNM stages were observed (p = 0.163).
The frequency of EGFR gene mutations was found to be four times higher in never smokers than in former and current smokers (22.9 % vs. 5.9 %, p < 0.001), which is in concordance with previous reports on the East Asian, North American and West European populations [16, 17, 21–23, 32]. Within the group of former and current smokers, however, the average number of pack-years was significantly lower in the EGFR gene mutation-positive patients compared to the EGFR gene mutation-negative patients (p = 0.002).
We have also compared the frequencies of EGFR gene mutations in histological (FFPE) and cytological samples, and found no difference (p = 0.813). This observation supports the notion that the SARMS method [20] is sufficiently sensitive to detect mutations in even small samples such as cytological samples.
Our assessment of metastatic lesions showed an increase in EGFR gene mutation frequencies compared to the primary tumors, without reaching statistical significance (p = 0.092). These results are in agreement with those of Smits et al. [19] who found no differences in EGFR gene mutation frequencies between primary lung ADCs and different metastatic lesions, although patients with malignant effusions and brain metastases exhibited (a trend in) increased EGFR gene mutation frequencies [19]. Again, in agreement with the results of Smits et al. [19] we observed a higher EGFR gene mutation frequency in metastases derived from the pleura (p = 0.012). In the ADCs the metastatic lesions showed no differences in EGFR gene mutation frequencies compared to the primary tumors (p = 0.353). Unlike Smith et al. [19], we also studied a group of SCCs. In these cases a multivariate logistic regression analysis revealed that the metastases exhibited a 2.6 times higher mutation rate compared to the primary tumors (p = 0.027). In particular, bone metastases exhibited a 8.65 times more frequent EGFR gene mutation rate than primary SCCs (p = 0.015). Additionally, we conclude from our results that tissue samples derived from both sites, i.e., primary or metastatic, are suitable for mutation analysis. Additional studies should be aimed at comparing paired primary-metastasis cases.
We found that in Bulgarian NSCLC patients the most frequent EGFR gene mutations were deletions in exon 19 and the L858R mutation in exon 21, which is in concordance with previous studies [25, 33]. Besides three cases with a L861Q point mutation in exon 21, known to be TKI-sensitive [25], we detected two other rare point mutations: S768I in exon 20 (thrice) and G719X in exon 18 (once). In 26/1427 (1.8 %) cases a T790M point mutation (exon 20), known to cause resistance to TKI treatment [34] was detected, but never in combination with an activating EGFR gene mutation. The T790M point mutation is the most common known cause of acquired TKI resistance and is found in approximately 50 % of TKI-resistant patients [35]. When this mutation occurs after TKI treatment, combinations with other EGFR gene mutations are commonly seen [34]. In our study, all T790M mutations were found in untreated patients. Our data are also in agreement with other reports on the occurrence of this mutation in untreated patients, which range from 1 % to 80 % (based on different methods used). The baseline mutation levels are in concordance with the known sensitivities of the methods used [23, 33, 36].
Taken together, we conclude that the overall frequency of EGFR gene mutations in lung ADCs in the East European (Bulgarian) population is within the range of that observed in North American and West European populations, but that the EGFR gene mutation frequency in SCCs is higher than that in any population described to date. All patient samples were found to be suitable for EGFR gene mutation detection, regardless origin (primary or metastatic).
References
GLOBOCAN 2008 (IARC) Section of Cancer Information, http://globocan.iarc.fr/. Accessed 21 Sep 2013
A. Koren, H. Motaln, T. Cufer, Lung cancer stem cells: a biological and clinical perspective. Cell. Oncol. 36, 265 (2013)
P. Boyle, B. Levin, WHO/IARC World Cancer Report 2008 (International Agency for Cancer Research Press, Lyon, 2008)
J.R. Molina, P. Yang, S.D. Cassivi, S.E. Schild, A.A. Adjei, Non–small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin. Proc. 83, 584 (2008)
Y. Miyamae, K. Shimizu, J. Hirato, T. Araki, K. Tanaka, H. Ogawa, S. Kakegawa, M. Sugano, T. Nakano, Y. Mitani, K. Kaira, I. Takeyoshi, Significance of epidermal growth factor receptor gene mutations in squamous cell lung carcinoma. Oncol Rep. 25, 921 (2011)
N. Peled, M.W. Wynes, N. Ikeda, T. Ohira, K. Yoshida, J. Qian, M. Ilouze, R. Brenner, Y. Kato, C. Mascaux, F.R. Hirsch, Insulin-like growth factor-1 receptor (IGF-1R) as a biomarker for resistance to the tyrosine kinase inhibitor gefitinib in non-small cell lung cancer. Cell. Oncol. 36, 277 (2013)
S.H. Ahn, E.H. Jeong, T.G. Lee, S.Y. Kim, H.R. Kim, C.H. Kim, Gefitinib induces cytoplasmic translocation of the CDK inhibitor p27 and its binding to a cleaved intermediate of caspase 8 in non-small cell lung cancer cells. Cell. Oncol. 37, 377 (2014)
W.D. Travis, E. Brambilla, H.K. Muller-Hemerlink, C.C. Harris, World Health Organization classification of tumors. Pathology and genetics of tumours of the lung, pleura, thymus and heart (IARC Press, Lyon, 2004)
N. Dimitrova, M. Vukov, Z. Valerianova, Cancer Incidence in Bulgaria 2009 (AVIS-24 Ltd, Sofia, 2011)
T.S. Mok, Y.L. Wu, S. Thongprasert, C.H. Yang, D.T. Chu, N. Saijo, P. Sunpaweravong, B. Han, B. Margono, Y. Ichinose, Y. Nishiwaki, Y. Ohe, J.J. Yang, B. Chewaskulyong, H. Jiang, E.L. Duffield, C.L. Watkins, A.A. Armour, M. Fukuoka, Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. New Engl. J. Med. 361, 947 (2009)
C. Willmore-Payne, J.A. Holden, C.T. Wittwer, L.J. Layfield, The use of EGFR exon 19 and 21 unlabeled DNA probes to screen for activating mutations in non–small cell lung. J. Biomol. Tech. 19, 217 (2008)
T.J. Lynch, D.W. Bell, R. Sordella, S. Gurubhagavatula, R.A. Okimoto, B.W. Brannigan, P.L. Harris, S.M. Haserlat, J.G. Supko, F.G. Haluska, D.N. Louis, D.C. Christiani, J. Settleman, D.A. Haber, Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. New Engl. J. Med. 350, 2129 (2004)
J.G. Paez, P.A. Jänne, J.C. Lee, S. Tracy, H. Greulich, S. Gabriel, P. Herman, F.J. Kaye, N. Lindeman, T.J. Boggon, K. Naoki, H. Sasaki, Y. Fujii, M.J. Eck, W.R. Sellers, B.E. Johnson, M. Meyerson, EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 304, 1497 (2004)
W. Pao, V. Miller, M. Zakowski, J. Doherty, K. Politi, I. Sarkaria, B. Singh, R. Heelan, V. Rusch, L. Fulton, E. Mardis, D. Kupfer, R. Wilson, M. Kris, H. Varmus, EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc. Natl. Acad. Sci. 101, 13306 (2004)
T. Takano, Y. Ohe, H. Sakamoto, K. Tsuta, Y. Matsuno, U. Tateishi, S. Yamamoto, H. Nokihara, N. Yamamoto, I. Sekine, H. Kunitoh, T. Shibata, T. Sakiyama, T. Yoshida, T. Tamura, EGFR mutations and gene amplification in NSCLC: molecular analysis of the IDEAL/INTACT Gefitinib trials. J. Clin. Oncol. 23, 6829 (2005)
B. Gao, Y. Sun, J. Zhang, Y. Ren, R. Fang, X. Han, L. Shen, X.Y. Liu, W. Pao, H. Chen, H. Ji, Spectrum of LKB1, EGFR, and KRAS mutations in Chinese lung adenocarcinomas. J. Thorac. Oncol. 5, 1130 (2010)
A. Marchetti, C. Martella, L. Felicioni, F. Barassi, S. Salvatore, A. Chella, P.P. Camplese, T. Iarussi, F. Mucilli, A. Mezzetti, F. Cuccurullo, R. Sacco, F. Buttitta, EGFR mutations in non-small-cell lung cancer: analysis of a large series of cases and development of a rapid and sensitive method for diagnostic screening with potential implications on pharmacologic treatment. J. Clin. Oncol. 23, 857 (2005)
R.K. Hsieh, K.H. Lim, H.T. Kuo, C.Y. Tzen, M.J. Huang, Female sex and bronchioloalveolar pathologic subtype predict EGFR mutations in non-small cell lung cancer. Chest. 128, 317 (2005)
A.J. Smits, J.A. Kummer, J.W. Hinrichs, G.J. Herder, K.C. Scheidel-Jacobse, N.M. Jiwa, P.T. Nooijen, M.G. Looijen-Salamon, M.J. Ligtenberg, F.B. Thunnissen, D.A. Heideman, R.A. de Weger, A. Vink, EGFR and KRAS mutations in lung carcinomas in the Dutch population: increased EGFR mutation frequency in malignant pleural effusion of lung adenocarcinoma. Cell. Oncol. 35, 189 (2012)
A.M. Cushman-Vokoun, A.M. Crowley, S.A. Rapp, T.C. Greiner, Comparison study of the performance of the QIAGEN EGFR RGQ and EGFR Pyro assays for mutation analysis in non-small cell lung cancer. Am. J. Clin. Pathol. 140, 7 (2013)
N.C. Bae, M.H. Chae, M.H. Lee, K.M. Kim, E.B. Lee, C.H. Kim, T.I. Park, S.B. Han, S. Jheon, T.H. Jung, J.Y. Park, EGFR, ERBB2, and KRAS mutations in Korean non-small cell lung cancer patients. Cancer Genet. Cytogenet. 173, 107 (2007)
R. Rosell, T. Moran, C. Queralt, R. Porta, F. Cardenal, C. Camps, M. Majem, G. Lopez-Vivanco, D. Isla, M. Provencio, A. Insa, B. Massuti, J.L. Gonzalez-Larriba, L. Paz-Ares, I. Bover, R. Garcia-Campelo, M.A. Moreno, S. Catot, C. Rolfo, N. Reguart, R. Palmero, J.M. Sánchez, R. Bastus, C. Mayo, J. Bertran-Alamillo, M.A. Molina, J.J. Sanchez, M. Taron, Spanish Lung Cancer Group, Screening for epidermal growth factor receptor mutations in lung cancer. N. Engl. J. Med. 361, 958 (2009)
S. Dearden, J. Stevens, Y.-L. Wu, D. Blowers, Mutation incidence and coincidence in non small-cell lung cancer: meta-analyses by ethnicity and histology (mutMap). Ann. Oncol. 24, 2371 (2013)
J.L. Marks, M.D. McLellan, M.F. Zakowski, A.E. Lash, Y. Kasai, S. Broderick, I.S. Sarkaria, D. Pham, B. Singh, T.L. Miner, G.A. Fewell, L.L. Fulton, E.R. Mardis, R.K. Wilson, M.G. Kris, V.W. Rusch, H. Varmus, W. Pao, Mutational analysis of EGFR and related signaling pathway genes in lung adenocarcinomas identifies a novel somatic kinase domain mutation in FGFR4. PLoS One. 2, e426 (2007)
G.J. Riely, K.A. Politi, V.A. Miller, W. Pao, Update on epidermal growth factor receptor mutations in non-small cell lung cancer. Clin. Cancer Res. 12, 7232 (2006)
H. Cortes-Funes, C. Gomez, R. Rosell, P. Valero, C. Garcia-Giron, A. Velasco, A. Izquierdo, P. Diz, C. Camps, D. Castellanos, V. Alberola, F. Cardenal, J.L. Gonzalez-Larriba, J.M. Vieitez, I. Maeztu, J.J. Sanchez, C. Queralt, C. Mayo, P. Mendez, T. Moran, M. Taron, Epidermal growth factor receptor activating mutations in Spanish gefitinib-treated non-small-cell lung cancer patients. Annals of Oncology. 16, 1081 (2005)
T. Kosaka, Y. Yatabe, H. Endoh, H. Kuwano, T. Takahashi, T. Mitsudomi, Mutations of the epidermal growth factor receptor gene in lung cancer: biological and clinical implications. Cancer Res. 64, 8919 (2004)
Y.H. Soung, J.W. Lee, S.Y. Kim, S.H. Seo, W.S. Park, S.W. Nam, S.Y. Song, J.H. Han, C.K. Park, J.Y. Lee, N.J. Yoo, S.H. Lee, Mutational analysis of EGFR and K-RAS genes in lung adenocarcinomas. Virchows Arch. 446, 483 (2005)
K. Sugio, H. Uramoto, K. Ono, T. Oyama, T. Hanagiri, M. Sugaya, Y. Ichiki, T. So, S. Nakata, M. Morita, K. Yasumoto, Mutations within the tyrosine kinase domain of EGFR gene specifically occur in lung adenocarcinoma patients with a low exposure of tobacco smoking. Br. J. Cancer. 94, 896 (2006)
Y. Tomizawa, H. Iijima, N. Sunaga, K. Sato, A. Takise, Y. Otani, S. Tanaka, T. Suga, R. Saito, T. Ishizuka, K. Dobashi, J.D. Minna, T. Nakajima, M. Mori, Clinicopathologic significance of the mutations of the epidermal growth factor receptor gene in patients with non-small cell lung cancer. Clin. Cancer Res. 11, 6816 (2005)
S.F. Huang, H.P. Liu, L.H. Li, Y.C. Ku, Y.N. Fu, H.Y. Tsai, Y.T. Chen, Y.F. Lin, W.C. Chang, H.P. Kuo, Y.C. Wu, Y.R. Chen, S.F. Tsai, High frequency of epidermal growth factor receptor mutations with complex patterns in nonsmall cell lung cancers related to gefitinib responsiveness in Taiwan. Clin. Cancer Res. 10, 8195 (2004)
G.J. Riely, W. Pao, D. Pham, A.R. Li, N. Rizvi, E.S. Venkatraman, M.F. Zakowski, M.G. Kris, M. Ladanyi, V.A. Miller, Clinical course of patients with non-small cell lung cancer and epidermal growth factor receptor exon 19 and exon 21 mutations treated with gefitinib or erlotinib. Clin. Cancer Res. 12, 839 (2006)
M. Majem, J. Remon, Tumor heterogeneity: evolution through space and time in EGFR mutant non small cell lung cancer patients. Transl. Lung Cancer Res. 2, 226 (2013)
S. Toyooka, K. Kiura, T. Mitsudomi, EGFR mutation and response of lung cancer to gefitinib. N. Engl. J. Med. 352, 2136 (2005)
S. Kobayashi, T.J. Boggon, T. Dayaram, P.A. Janne, O. Kocher, M. Meyerson, B.E. Johnson, M.J. Eck, D.G. Tenen, B. Halmos, EGFR mutation and resistance of non-small cell lung cancer to gefitinib. N. Engl. J. Med. 352, 786 (2005)
L. Cheng, R. Alexander, G. MacLennan, O. Cummings, R. Montironi, A. Lopez-Beltran, H. Cramer, D. Davidson, S. Zhang, Molecular pathology of lung cancer: key to personalized medicine. Mod. Pathol. 25, 347 (2012)
Acknowledgments
The authors wish to thank Radka Budinova for technical assistance with some of the samples. The authors express special thanks to all the referring physicians. Astra Zeneca has provided the kits for EGFR gene mutation testing.
Conflict of interests
DM and AS do not have any conflicts of interest. SB and YS have received honoraria from Astra Zeneca for consultancies regarding EGFR testing in Bulgaria.
Ethical standards
The authors declare that the experiments comply with the current laws of the country (Bulgaria) in which they were performed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bichev, S.N., Marinova, D.M., Slavova, Y.G. et al. Epidermal growth factor receptor mutations in East European non-small cell lung cancer patients. Cell Oncol. 38, 145–153 (2015). https://doi.org/10.1007/s13402-014-0211-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-014-0211-7