Abstract
Both epidermal growth factor receptor (EGFR) and RAS gene mutations contribute to the development of non-small cell lung cancer (NSCLC). Because RAS is one of the downstream molecules in the EGFR signal transduction, the association between the somatic mutations of EGFR and RAS may be important in the pathogenesis of NSCLC . However, to date, such data are lacking. In this study, we analyzed the hotspot regions of K-RAS gene (codons 12, 13, 59 and 61) and EGFR gene (exons 18, 19 and 21) in 153 NSCLC tissue samples including 69 adenocarcinomas. Overall, we detected 30 EGFR mutations (19.6%) and 6 K-RAS mutations (3.9%) in the 153 NSCLCs. In the 69 adenocarcinomas, 26 EGFR mutations (37.7%) and six K-RAS mutations (8.7%) were detected. Of note, the 26 tumors with EGFR mutations did not harbor any K-RAS mutations, and the six tumors with K-RAS mutations did not harbor any EGFR mutations. Inverse relationship between K-RAS and EGFR mutations in the lung adenocarcinoma was statistically significant (P=0.046, χ2 test). As regards smoking history, EGFR mutation was significantly associated with never-smoking history, whereas K-RAS mutation was significantly associated with smoking history. Our data suggest that mutations of EGFR and K-RAS genes might separately, but not cooperatively, contribute to lung adenocarcinoma pathogenesis, and that EGFR and K-RAS mutants could separately be anti-neoplastic targets in lung adenocarcinomas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer is the most common cause of cancer deaths in both men and women worldwide, with non-small cell lung cancer (NSCLC) accounting for approximately 80% of these cases [8]. Despite advances in surgical and chemotherapeutic intervention, survival has improved very little over the past few decades, with an overall cure rate of <15% [19].
The epidermal growth factor receptor (EGFR), a receptor protein tyrosine kinase, contributes to a number of processes in tumor survival and growth activity, thus making it a promising molecular target for cancer therapy [9]. One of the agents that target the EGFR is the orally active EGFR tyrosine kinase inhibitor gefitinib (Iressa), which has given significant clinical benefit to NSCLC patients [6, 11, 21]. However, since not all NSCLC patients exhibit the same response, there is considerable interest in prognostic indicators that might predict the response to gefitinib. Recently, three research groups discovered that somatic mutations of EGFR gene in the NSCLC could predict significant clinical responses to gefitinib [13–15]. Most of the EGFR somatic mutations were exclusively detected in the adenocarcinomas (including bronchioloalveolar carcinomas). The mutations were detected in the exons 18, 19 and 21 that encode the intracellular kinase domain. The mutations detected in the exon 18 would substitute the amino acid G719 in the P-loop, while those detected in the exon 21 would substitute amino acids in the activation domain (L858 and L861). The mutations in the exon 19 were in-frame deletions that may alter the structure of αC helix. All of the EGFR mutations affect amino acids near the ATP-binding pocket that is targeted by gefitinib. Functional assays revealed that the hotspot mutants of EGFR had a higher EGF-dependent activation than the wild-type EGFR had [13–15, 18].
Activation of the RAS pathway also plays a critical role in cell proliferation, and is frequently activated in cancer cells by the somatic mutation [4]. In NSCLC, the K-RAS mutations are more common in adenocarcinoma than those in the other histologic types and have been detected in approximately 7–40% of lung adenocarcinomas [7]. Of note, RAS pathway is one of the major signaling pathways that mediate the downstream effects of EGFR activation. Although genetic alterations of both EGFR and K-RAS genes are important in the pathogenesis of NSCLC, to date the data that analyzed the relationship between the incidences of EGFR and K-RAS mutations in NSCLC is lacking. In this study, we analyzed 153 NSCLCs, including 69 adenocarcinomas, for the detection of both EGFR and K-RAS gene mutations, and found the inverse relationship between EGFR and K-RAS mutations in lung adenocarcinomas.
Materials and methods
Methacarn-fixed tissues of 153 human NSCLC tissue samples were randomly obtained from surgically treated patients. These samples consisted of 69 adenocarcinomas (including 20 adenocarcinomas with bronchioloalveolar carcinoma features and three pure bronchioloalveolar carcinomas), 70 squamous cell carcinomas, three adenosquamous carcinomas and 11 large cell carcinomas. We analyzed the primary tumors, but not the metastatic lesions of the NSCLC. The male to female ratio was 111:42. Ages of the patients ranged from 36 to 79 years, with an average of 59.6 years. The patients consisted of 91 current smokers, eight former smokers and 54 non-smokers (Tables 1 and 2). Approval was obtained from the Catholic University of Korea, College of Medicine’s institutional review board for this study. Informed consent was provided according to the Declaration of Helsinki.
Through the microdissection, tumor cells and normal cells were selectively procured from hematoxylin and eosin-stained slides of the same patients using a 30G1/2 hypodermic needle (Becton Dickinson, Franklin Lakes, N.J., USA) affixed to a micromanipulator, as described previously [12]. DNA extraction was performed by a modified single-step DNA extraction method [12]. Because all of the EGFR mutations in the NSCLC have been detected within exons 18, 19 and 21 in the previous studies [13–15], we analyzed the mutations in these three exons by polymerase chain reaction (PCR)-single strand conformation polymorphism (SSCP) analysis. Radioisotope ([32P] dCTP) was incorporated into the PCR products for detection by autoradiogram. After SSCP, bands showing mobility shifts were cut out from the dried gel, re-amplified for 30 cycles, and sequenced using the cyclic sequencing kit (Perkin-Elmer, Foster City, Calif., USA). The procedures of PCR and SSCP analysis were performed as described previously [12]. We analyzed K-RAS mutations at codons 12, 13, 59 and 61 by both PCR-SSCP and direct DNA sequencing.
Results
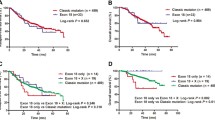
PCR and subsequent SSCP analysis of the EGFR gene identified aberrantly migrating bands compared with the wild-type bands (Fig. 1). None of the corresponding normal samples from the same patients showed evidence of mutations by SSCP (Fig. 1), indicating that the mutations had risen somatically. Enrichment and DNA sequence analysis of the aberrantly migrating bands led us to identify that 30 out of the 153 samples harbored EGFR mutations (19.6%) (Table 1). The EGFR mutations were detected in the exon 19 (12 mutations) and exon 21 (18 mutations), but not detected in the exon 18. Of the EGFR mutations detected in the exon 21, all of the mutations were the known hotspot mutation at the nucleotide 2573 (2573T→G) that would result in an amino acid change (L858R). In exon 19, we found five types of in-frame EGFR mutations and the most common one was 2235_2249delGGAATTAAGAGAAGC, which would result in in-frame deletion of five amino acids (E746_A750del).
PCR-SSCP of EGFR gene in the NSCLC. Representative data of SSCP (A) and DNA sequencing analysis (B) of EGFR DNA from tumors (lane T) and normal tissues (lane N). a: SSCPs of DNA in exons 19 and 21 from the tumors (T) show wild type bands and additional aberrant bands (arrows) as compared with SSCP from corresponding normal cells of the same patients (N). B: Sequencing analysis from the aberrant bands in (A). Numbering of cDNA of EGFR was carried out with respect to the ATG start codon (GenBank)
According to the histologic types, the EGFR mutations were identified in 26 of the 69 adenocarcinomas (38%), two of the 70 squamous cell carcinomas (3%), two of the three adenosquamous carcinomas (67%) and none of 11 large cell carcinomas (0%). The incidence of the EGFR mutation in the adenocarcinomas was significantly higher than that of the squamous cell carcinomas (Fisher’s exact test, P<0.01). Furthermore, the incidence of the EGFR mutations was significantly associated with being female (Fisher’s exact test, P<0.01) and never-smoking history (Fisher’s exact test, P<0.01) (Table 2).
We also analyzed K-RAS mutations in the same 153 NSCLC tissue samples. In agreement with the previous reports that K-RAS mutations have been detected mainly in adenocarcinoma type of NSCLC [7, 17], we detected six K-RAS mutations (8.7%) of the 69 adenocarcinomas, but not in other types of NSCLC (Fig. 2, Table 1). The mutations consist of three 34G→T (G12C), two 35 G→T (G12V) and one 35G→A (G12D). Interestingly, the 26 tumors with EGFR mutations did not harbor any K-RAS mutations, and the six tumors with K-RAS mutations did not harbor any EGFR mutations. The inverse relationship between K-RAS and EGFR mutations was statistically significant (Table 3; P=0.046, χ2 test). The incidence of K-RAS mutation was significantly associated with smoking history (Fisher’s exact test, P<0.05). There was no association of either EGFR and K-RAS mutations with patient’s age, size of the tumor and number of lymph nodes with tumor metastasis.
PCR-SSCP of K-RAS gene in the NSCLC. Representative data of SSCP (A) and DNA sequencing analysis (B) of K-RAS DNA from tumors (lane T) and normal tissues (lane N). A: SSCPs of DNA in the exon 1 from the tumors (T) show wild type bands and additional aberrant bands (arrows) as compared to SSCP from corresponding normal cells of the same patients (N). B: Sequencing analysis from the aberrant bands in (A). Numbering of cDNA of K-RAS was done in respect to the ATG start codon (GenBank)
Discussion
The previous observations that signaling pathways of EGFR and K-RAS are overlapped [4] led us to analyze the relationship between the incidences of mutations of these two genes in NSCLC. We observed that most of the EGFR mutations (26 of the total 30 mutations) and all of the K-RAS mutations were detected in the adenocarcinoma type. Furthermore, there was an inverse relationship between the occurrences of EGFR and K-RAS mutations in the adenocarcinomas. As regards the inverse relationship between EGFR and K-RAS mutations, there have been genetic epidemiology data that support that. For the smoking history, K-RAS mutation was strongly associated with cigarette smoking in lung adenocarcinomas [2], whereas EGFR mutation was commonly found in NSCLCs from never smokers as apposed to former or current smokers [13–15]. In the current study, we also observed that K-RAS mutation was associated with cigarette smoking and that EGFR mutation was associated with non-smoking status (Table 2). These data suggested the possibility that EGFR and K-RAS mutations target different subsets of lung adenocarcinomas.
So far, more than ten types of EGFR mutations in the exon 19 have been reported [13–15]. Of the five types of the exon 19 mutations detected in the present study, three (2236_2250delGAATTAAGAGAAGCA, 2235_2249delGGAATTAAGAGAAGC and 2240_2257delTAAGAGAAGCAACATCTC) were the previously reported mutations, while the remaining two (2245_2253delGAAGCAACA, and 2254_2276delTCTCCGAAAGCCAACAAGGAAAT with 2252delC) were novel mutations that would also result in the in-frame deletion of the amino acids near the ATP-binding pocket. The EGFR mutations in the kinase domain were reported in 3–32% of the adenocarcinomas, and the mutations were more frequent in patients from Japan than in those from the United States [13–15]. The incidence of the EGFR mutation in our study (37.7% of the Korean patients with lung adenocarcinoma) is similar to that of the Japanese patients [14], confirming the racial difference of the EGFR mutation in lung cancers. Regarding K-RAS gene, the incidence of the mutation in the lung adenocarcinomas in this study was 8.7%, which was at the low part of the 7–40% reported in the previous studies [2, 7, 17]. The lower incidence of K-RAS mutation is unlikely to be a result of low sensitivity of the detection methods, because we used both direct sequencing and SSCP, which have been used to detect K-RAS mutations in the previous studies [2, 7, 17].
What would be the difference in the oncogenic effects between the EGFR-mutated and the K-RAS-mutated lung adenocarcinomas? The major downstream pathways mediating oncogenic effects of EGFR are activation of ERKs via RAS, and AKT via PI3K [10]. Given the observation that EGFR mutants in the kinase domain selectively activated AKT pathway with no effects on the ERK pathway via RAS [18], the EGFR mutation would result in the increased survival of the affected cancer cells by AKT. Although RAS mutants mainly activate the ERK pathway [20], they also activate AKT via PI3K [16]. Therefore, the K-RAS mutants would result in both increased survival and proliferation of the affected cancer cells. However, the exact consequences of the K-RAS and EGFR mutations in the complicated cellular contexts should be further analyzed in future studies.
Findings of EGFR mutations in NSCLC raised several critical questions. One of them was as to whether other components of the EGFR signaling could be drug targets. In the current study, our data suggested that the lung adenocarcinomas with the EGFR mutations might comprise an adenocarcinoma group that is distinct from those with K-RAS mutations. Therefore, the EGFR mutants as well as the RAS mutants could separately be anti-neoplastic targets in the different sets of lung adenocarcinomas. The most impressive examples of recent cancer therapies used the small-molecule inhibitors for tyrosine kinases such as imanitib, trastzumab and gefitinib [3, 5, 21]. In addition, several inhibitors of the RAS mutants and downstream molecules of RAS are now in clinical trials for cancer therapy [1]. In this respect, the present study may provide the basic information of lung adenocarcinomas for future therapies targeting EGFR and RAS mutations.
Abbreviations
- PCR:
-
polymerase chain reaction
- SSCP:
-
single strand conformation polymorphism
- EGFR:
-
epidermal growth factor receptor
- NSCLC:
-
non-small cell lung cancer
- BAC:
-
bronchioloalveolar carcinoma
References
Adjei AA (2001) Blocking oncogenic Ras signaling for cancer therapy. J Natl Cancer Inst 93:1062–1074
Ahrendt SA, Decker PA, Alawi EA, Zhu YYR, Sanchez-Cespedes M, Yang SC, Haasler GB, Kajdacsy-Balla A, Demeure MJ, Sidransky D (2001) Cigarette smoking is strongly associated with mutation of the K-ras gene in patients with primary adenocarcinoma of the lung. Cancer 92:1525–1530
Arteaga CL, Moulder SL, Yakes FM (2002) HER (erbB) tyrosine kinase inhibitors in the treatment of breast cancer. Semin Oncol 29:4–10
Downward J (2003) Targeting RAS signalling pathways in cancer therapy. Nat Rev Cancer 3:11–22
Druker BJ, Sawyers CL, Kantarjian H, Resta DJ, Reese SF, Ford JM, Capdeville R, Talpaz M (2001) Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N Engl J Med 344:1038–1042
Fukuoka M, Yano S, Giaccone G, Tamura T, Nakagawa K, Douillard JY, Nishiwaki Y, Vansteenkiste J, Kudoh S, Rischin D, Eek R, Horai T, Noda K, Takata I, Smit E, Averbuch S, Macleod A, Feyereislova A, Dong RP, Baselga J (2003) Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer. J Clin Oncol 21:2237–2246
Graziano SL, Gamble GP, Newman NB, Abbott LZ, Rooney M, Mookherjee S, Lamb ML, Kohman LJ, Poiesz BJ (1999) Prognostic significance of K-ras codon 12 mutations in patients with resected stage I and II non-small-cell lung cancer. J Clin Oncol 17:668–675
Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, Feuer EJ, Thun MJ, American Cancer Society (2004) Cancer statistics, 2004. Cancer J Clin 54:8–29
Jorissen RN, Walker F, Pouliot N, Garrett TP, Ward CW, Burgess AW (2003) Epidermal growth factor receptor: mechanisms of activation and signalling. Exp Cell Res 284:31–53
Kamata T, Feramisco JR (1984) Epidermal growth factor stimulates guanine nucleotide binding activity and phosphorylation of ras oncogene proteins. Nature 310:147–150
Kris MG, Natale RB, Herbst RS, Lynch TJ Jr, Prager D, Belani CP, Schiller JH, Kelly K, Spiridonidis H, Sandler A, Albain KS, Cella D, Wolf MK, Averbuch SD, Ochs JJ, Kay AC (2003) Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 290:2149–2158
Lee JY, Dong SM, Kim SY, Yoo NJ, Lee SH, Park WS (1998) A simple, precise and economical microdissection technique for analysis of genomic DNA from archival tissue sections. Virchows Arch 433:305–309
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG, Louis DN, Christiani DC, Settleman J, Haber DA (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350:2129–2139
Paez JG, Janne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304:1497–1500
Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, Mardis E, Kupfer D, Wilson R, Kris M, Varmus H (2004) EGF receptor gene mutations are common in lung cancers from “never smokers” and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci USA 101:13306–13311
Rodriguez-Viciana P, Warne PH, Dhand R, Vanhaesebroeck B, Gout I, Fry MJ, Waterfield MD, Downward J (1994) Phosphatidylinositol-3-OH kinase as a direct target of Ras. Nature 370:527–532
Slebos RJ, Hruban RH, Dalesio O, Mooi WJ, Offerhaus GJ, Rodenhuis S (1991) Relationship between K-ras oncogene activation and smoking in adenocarcinoma of the human lung. J Natl Cancer Inst 83:1024–1027
Sordella R, Bell DW, Haber DA, Settleman J (2004) Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science 305:1163–1167
Sridhar SS, Seymour L, Shepherd FA (2003) Inhibitors of epidermal-growth-factor receptors: a review of clinical research with a focus on non-small-cell lung cancer. Lancet Oncol 4:397–406
Vojtek AB, Hollenberg SM, Cooper JA (1993) Mammalian Ras interacts directly with the serine/threonine kinase Raf. Cell 74:205–214
Wakeling AE, Guy SP, Woodburn JR, Ashton SE, Curry BJ, Barker AJ, Gibson KH (2002) ZD1839 (Iressa): an orally active inhibitor of epidermal growth factor signaling with potential for cancer therapy. Cancer Res 62:5749–5754
Acknowledgements
This work was supported by the Korea Science & Engineering Foundation (KOSEF) through the Cell Death Disease Research Center at The Catholic University of Korea (R13-2002-005-01004-0).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soung, Y.H., Lee, J.W., Kim, S.Y. et al. Mutational analysis of EGFR and K-RAS genes in lung adenocarcinomas. Virchows Arch 446, 483–488 (2005). https://doi.org/10.1007/s00428-005-1254-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-005-1254-y