Abstract
Numerous studies observed a link between the herpes smplex virus-1 (HSV-1) and Alzheimer’s disease. However, the exact viral and cellular dynamics that lead from an HSV-1 infection to Alzheimer’s disease are unknown. In this paper, we use the microcompetition model to formulate these dynamics by connecting seemingly unconnected observations reported in the literature. We concentrate on four pathologies characteristic of Alzheimer’s disease. First, we explain how an increase in the copy number of HSV-1 during latency can decrease the expression of BECN1/Beclin1, the degradative trafficking protein, which, in turn, can cause a dysregulation of autophagy and Alzheimer’s disease. Second, we show how an increase in the copy number of the latent HSV-1 can decrease the expression of many genes important for mitochondrial genome metabolism, respiratory chain, and homeostasis, which can lead to oxidative stress and neuronal damage, resulting in Alzheimer’s disease. Third, we describe how an increase in this copy number can reduce the concentration of the NMDA receptor subunits NR1 and NR2b (Grin1 and Grin2b genes), and brain derived neurotrophic factor (BDNF), which can cause an impaired synaptic plasticity, Aβ accumulation and eventually Alzheimer’s disease. Finally, we show how an increase in the copy number of HSV-1 in neural stem/progenitor cells in the hippocampus during the latent phase can lead to an abnormal quantity and quality of neurogenesis, and the clinical presentation of Alzheimer’s disease. Since the current understanding of the dynamics and homeostasis of the HSV-1 reservoir during latency is limited, the proposed model represents only a first step towards a complete understanding of the relationship between the copy number of HSV-1 during latency and Alzheimer’s disease.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is characterized by formation of senile plaques in the hippocampus and cortex, cognitive decline, and dementia. The plaques are mostly made of amyloid β (Aβ) and neurofibrillary tangles (NFTs) composed of tau protein. The metabolism of Aβ is dependent on autophagy, a process that leads to degradation of proteins and organelles. This process is disrupted in AD, leading to the main pathology, accumulation of Aβ, and NFTs in brain cells. The reason for the disruption in AD is unknown. However, studies observed a link to abnormal expression of the degradative trafficking protein BECN1/Beclin1, a key autophagy regulator. In addition, AD patients present reduced mitochondrial activity, enzymes, and biosynthesis in neurons. This results in axonal and neuronal damage. A third pathology is dysregulations of the synaptic transmission via NDMA receptors and brain-derived neurotrophic factor (BDNF) activity in the hippocampus. Studies have shown that these dysregulations result in impaired synaptic plasticity, and increased pathology of extracellular Aβ accumulation. A fourth pathology is impaired neurogenesis in AD brains, and interrupted ability to repair hippocampal damage.
Numerous studies observed a link between the herpes simplex virus-1 (HSV-1) and Alzheimer’s disease (Harris and Harris 2018). In this paper, we use the microcompetition model to explain how a latent HSV-1 can cause the above four pathologies observed in AD. Finally, we theorize what is the deciding factor that makes an HSV-1 positive individual develop AD.
HSV-1 and Alzheimer’s disease
Several animal studies showed that HSV-1 enters the brain via the olfactory bulb, and then modifies the structures of the limbic system, such as the entorhinal cortex and the hippocampus, known to be greatly affected in AD (McLean et al. 1993; Mori et al. 2005). A recent study on human brains showed an increase in gene expression of the host cell viral entry receptor proteins of HSV-1 in the hippocampus, indicating that this area is particularly susceptible to HSV-1 infection (Lathe and Haas 2017). Using polymerase chain reaction (PCR) analysis, another study detected the latent HSV-1 in the hippocampus, temporal and frontal lobes of 70–100% of sporadic AD and normal elderly brains (Jamieson et al. 1991). Wozniak et al. found HSV-1 DNA in the amyloid plaques in 72% of AD patients, compared to 24% of age equivalent healthy controls (Wozniak et al. 2009). Postmortem analysis of elderly brains showed that the combination of an HSV-1 infection and the APOE-ε4 allele increased the risk of AD by a factor of 12 (Itzhaki et al. 1997; Lin et al. 1998; Itabashi et al. 1997). A longitudinal study of 512 elderly people showed a strong association between AD and HSV-1 infection and reactivation (Letenneur et al. 2008). Postmortem analysis of 147 autopsies also uncovered HSV-1 DNA in 90% of AD patients (Hill et al. 2008). Specific AD pathologies were also associated with HSV-1 infection. A study observed an increase in accumulation of Aβ and decreased Amyloid β Precursor Protein (APP) levels both in vivo and in vitro after infection with HSV-1 (Itzhaki et al. 2016).
Tzeng et al. (2018) preformed a population-based study in Taiwan with over 33,000 participants aged 50 and older and associated symptomatic HSV-1 with dementia. The study included 8362 patients clinically diagnosed with HSV (HSV-1 and HSV-2) and have made at least three outpatient visits to the clinic within a one-year study period regarding symptoms of HSV-1 or HSV-2. For each HSV diagnosed patient, the study enrolled three controls without a clinical history of HSV infection. The seropositivity of HSV-1 in the adult population in Taiwan in over 90% (Shen et al. 2015); hence, it is reasonable to assume that a large portion of the asymptomatic controls were also seropositive. Therefore, it is more accurate to consider study group as infected/symptomatic, and the control group as infected/asymptomatic. Tzeng et al. observed a 2.8-fold increase in the hazard ratio of developing dementia of Alzheimer type in the infected/symptomatic compared to the infected/asymptomatic individuals. The study also followed the infected/symptomatic HSV-1 subjects who used anti-herpetic agents over a period of 10 years. These subjects had a 5 times lower risk of developing dementia in comparison to infected/asymptomatic participants. Considering that during the 10 years, the virus remains mostly in the latent phase, this suggests a possible association between the latent HSV-1 and AD. We propose that the difference between the two groups is a higher copy number of the virus during latency in the infected/symptomatic compared to the infected/asymptomatic individuals. See more on copy number below.
In this paper, we use the microcompetition model to describe the viral and cellular dynamics that may lead from the copy number of HSV-1 during the latent phase to the four pathologies commonly observed in AD patients: reduced autophagy activity, mitochondrial dysfunction, NMDA receptor and BDNF dysregulation, and unbalanced neurogenesis.
We use the literature regarding the life cycle of HSV-1, latency programs, gene expression, and latent copy number to map the sequence of events that lead from the copy number of the latent virus to the development of AD. However, it is important to state that latency is only partially understood. We do not aim to add observations about latency, but to connect seemingly unconnected observations reported in the literature to build the molecular dynamics that lead from the copy number of HSV-1 in the hippocampus during latency to AD.
The GABP transcription factor
The GA binding protein (GABP), also called the nuclear respiratory factor 2 (NRF2), is a ubiquitous transcription factor operating from embryonic development until death. GABP is a heterotetramer that consists of a pair of two subunits, GA binding protein alpha (GABPα) and GA binding protein beta (GABPβ). The β subunit has three isoforms, including two splice variants. GABP is a member of the ETS-domain transcription factor family (ETS-TF) (Sharrocks 2001). It binds genes through an ETS-binding site called the N box.
GABP has a variety of functions, one of which is to promote cell cycle progression through the S-phase by allowing the transcription of DNA synthesis genes (Rosmarin et al. 2004). It cooperates with the two related histone acetyltransferases co-activators p300 and CBP (CREB binding protein), together denoted p300/CBP, which levels are limiting in the cell (Lee et al. 2010; Bhattacharyya et al. 2010; Polansky and Schwab 2018a, b; Zhou et al. 2015) to form the limiting GABP•p300/CBP complex.
AD pathology number 1: impaired autophagy in neurons
Neurons of AD patients have reduced autophagy, mainly through the BECN1-dependent degradative pathways.
BECN1 and AD
BECN1 is a key regulator of degradative trafficking pathways, including the endosomal pathway and autophagy. In their study, Swaminathan et al. (2016) explored the role of BECN1 in amyloid-β precursor protein (APP) trafficking from the cell surface/plasma membrane. Using co-immunoprecipitation (co-IP) on whole-cell extracts (WCE) and rat cortical neurons, they demonstrated that APP is a novel BECN1-interacting protein. Then, using a BECN1 deletion mutant, they discovered that the evolutionary conserved domain (ECD) is indispensable for APP-BECN1 association.
Next, they tested the effect of BECN1 endocytosis of the surface receptor APP and the sorting for lysosomal degradation. To measure the effect of BECN1 on APP internalization, they labeled the N-terminal FLAG-APP695 on the surface of HeLa cells with a FLAG antibody. They observed that BECN1 depletion decreased the surface APP internalization and that ectopic BECN-1 expressing cells had higher internalization of APP.
Then, they assessed the effect of BECN-1 on the postendocytic traffic of the internalized APP to the endolysosomal and autolysosomal compartments. They overexpressed BECN1, and observed an increase in colocalization of the internalized APP with GFP-LC3-positive autophagosomes. This indicates that BECN1 assists APP sorting to endosomes. Swaminathan et al. concluded that the BECN1 ECD interacts with APP and promotes APP internalization and degradation via endosomes and autophagosomes.
The observations in Swaminathan et al. suggest that a BECN1 deficiency can cause impaired degradative sorting of PM-APP, which is the precursor of the toxic amyloid-β (Aβ).
Other studies also noticed the relation between BECN-1 and AD pathology. For instance, Pickford et al. (2008) observed a decrease in BECN-1 levels in the brains of eight AD patients compared to healthy controls. They also found that a BECN-1 deficiency in APP transgenic mice decreased neuronal autophagy, disrupted lysosomes, increased the accumulation of Aβ intracellularly and extracellularly, and ultimately caused neurodegeneration. Furthermore, an increase in BECN-1 expression decreased the amyloid pathology in the APP transgenic mice. Several more studies have shown, both in vitro and in vivo, the importance of BECN-1 dependent autophagy in neurodegenerative diseases. By overexpressing BECN1, neuronal cytotoxicity and death were prevented (Hung et al. 2009; Wang et al. 2009).
As the previous studies have shown, a decrease in BECN1 reduces autophagy and contributes to proteinopathies, such as Aβ pathology, a characteristic of Alzheimer’s disease.
In the next sections, we will answer the question, what causes the BECN1 deficiency in AD, and how is it related to HSV-1?
BECN1 and GABP
Although the cause of the decrease in BECN1 expression in AD is unknown, a study by Salminem et al. (2013) proposed a link with certain neurovirulent proteins, such as those expressed by HSV-1. In this paper, we propose a different link, using GABP.
Zhu et al. sought to discover the role of GABP in regulating autophagy (Zhu et al. 2014). Using bioinformatics analysis, Zhu et al. observed that genes encoding the BECN1-PIK3C3 complexes contain ETS-TF core sequences, the binding site for GABP, in their promoter regions. This led them to believe that GABP might be regulating the transcription of the BECN1-PIK3C3 complex. To test this hypothesis, Zhu et al. used clones with sequences from the promoter regions of BECN1, PIK3C3, UVRAG, and ATG14 in luciferase reporter constructs, and compared the luciferase activities of each promoter-luciferase construct with constructs that had mutations in their GABP binding sites. They discovered that mutations in the GABP sites on the BECN1 and PIK3C3 promoter fragments reduced the luciferase activity by 90%. This indicates that GABP is responsible for most of the transcriptional activities of these two promoter fragments.
Next, Zhu et al. tested the binding of GABP to the promoter regions of these autophagy regulatory genes, and the effect of such binding on transcription. They performed chromatin immunoprecipitation (ChIP) assays using an antibody to GABPα and discovered that GABPα binds to the promoter regions of BECN1, PIK3CS, PIK3R4, ATG14, and UVRAG. Then, they knocked down GABPα using siRNA oligonucleotides and examined the transcripts of the autophagy genes using real-time quantitative PCR (qPCR). The results showed that a 70% decrease in GABPα mRNA levels caused a significant decrease in all of the autophagy gene transcripts mentioned previously. From these results, Zhu et al. concluded that GABP binds to the promoter regions of autophagy regulatory genes and transactivates them. Using western blots, Zhu et al. observed that a 75% decrease in GABPα decreased BECN1-PIK3C3 complex protein levels and autophagy. The decrease in GABPα also caused a significant decrease in BECN1, PIK3C3, and UVRAG. This indicates that GABP is important for maintaining the levels of the BECN1-PIK3C3 complex protein, and the cellular process of autophagy. Then, Zhu et al. tested the effect of an increase in GABP on cellular autophagy. Zhu et al. transfected GABP expression constructs into HeLa cells, and measured some cellular autophagy markers. As expected, the increase in GABP expression increased the autophagosomal marker LC3-II and the levels of PIK3C3, BECN1, and UVRAG. Using fluorescent microscopy and western blot analysis, they observed that an increase in GABPα or GABPβ1 expression increased GFP-LC3. Using transmission electron micrographs of HeLa cells, Zhu et al. also observed an increase in cytoplasmic autolysosomes in cells cotransfected with GABPα or GABPβ1 expression constructs. From these observations they concluded that GABP increases the expression of genes encoding BECN1-PIK3c3 complexes, which increases autophagy.
We conclude that GABP has a key role in BECN1 expression, and therefore, may have a role in autophagy abnormalities associated with AD.
AD pathology number 2: mitochondrial dysfunction
Mitochondria in neurons, mainly in the hippocampus, have reduced activity and biogenesis in AD.
Mitochondrial dysfunction in AD
Many studies demonstrated a reduced mitochondrial function in AD patients, mostly in neurons located in the hippocampus, see Wang et al. (2020). Using fluoro-2-deoxyglucose positron-emission tomography (FDG-PET), a decline in glucose metabolism was noticed early in AD (Arbizu et al. 2018; Sörensen et al. 2019). Oxygen metabolism rate, measured by oxygen-15 PET, was greatly decreased in AD brains, with a correlation to the severity of dementia (Tohgi et al. 1998; Lajoie et al. 2017; Ishii et al. 1996), indicating a dysfunction in the oxidative phosphorylation (OXPHOS) machinery in AD. Furthermore, using immunofluorescence analysis, studies observed elevated levels of 8-hydroxyguanosine (8-OHG), a marker for oxidative damage, in both DNA (including mitochondrial DNA) and RNA, in AD brain specimen, suggesting excessive production of reactive oxygen species (ROS) (Manczak et al. 2004; Nunomura et al. 2012). With an increased oxidative stress, energy metabolism is impaired, eventually leading to neuronal damage, neurodegeneration pathologies, and AD (Keller et al. 1997; Manczak et al. 2006).
In the process of OXPHOS, five reciprocal enzymatic complexes reduce oxygen molecules to initiate ATP production. Several studies noticed a decrease in the enzymatic activity in the hippocampus of all OXPHOS complexes, especially cytochrome C oxidase (COX) (Parker and Parks 1995; Maurer et al. 2000; Bosetti et al. 2002). Some suggested that the reason is reduced expression of the subunits composing the functional OXPHOS complexes.
Eighty nuclear genes encode the OXPHOS complexes subunits. Using postmortem analysis of AD hippocampus tissue, Liang et al. (2008) found a decrease in 58% of the nuclear-encoded genes for subunits composing OXPHOS complexes and mitochondrial translocases. Particularly, they observed a twofold decrease in the mRNA levels of 49 out of the 80 (61%) nuclear-encoded genes for subunits composing complexes I–V. Protein levels of these genes were also reduced. Similarly, a recent microarray study by Mastroeni et al. (2017) found a decrease in hippocampal OXPHOS gene expression in AD in comparison to age equivalent healthy controls. All nuclear-encoded genes for complex I subunits and complex II subunits SDHA/B/C/D were reduced by up to 25% and 15%, respectively. With the exception of one gene, all other COX nuclear coding genes were differentially reduced in AD brains. For instance, COX5A, COX6C, and COX7B genes were all decreased by more than 25%. The expression of complex V (ATP synthase) F1 beta subunit gene, ATP5B, was reduced by 25%, along with a decrease in all other nuclear-encoded complex V genes. The data, summarized in, suggest that there is a decrease in the expression of many OXPHOS nuclear genes, causing the oxidative stress seen in AD.
The mitochondrial genome codes for 13 core OXPHOS proteins that depend on nuclear encoded mitochondrial transcription factors. The expression of some of these genes, especially complex I, are reduced in AD brain tissues (Manczak et al. 2004), suggesting that mtDNA metabolism in the mitochondrial genome may be disrupted. As expected, studies observed a decrease in mtDNA copy number both in AD postmortem hippocampus tissue (Rice et al. 2014), and in M17 cells transfected with a mutant APP gene (Sheng et al. 2012). Another study (Coskun et al. 2004) also observed a 63% average increase in mtDNA mutation rate and lower mtDNA copy number in AD brains. It is also interesting that patients carrying mtDNA mutations present cognitive deficits similar to AD patients (Inczedy-Farkas et al. 2014).
Various factors, such as mitochondrial transcription factor A (TFAM), mitochondrial polymerase, TWINKLE mtDNA helicase, participate in mtDNA metabolism. Some are underexpressed in AD. For instance, TFAM, which has a key role in mtDNA transcription, copy number, and stabilizing the mtDNA (Campbell et al. 2012), was found to be depleted in the course of AD. Sheng et al. reported a 50% decrease in the protein levels of TFAM in AD hippocampus autopsy tissue, and in a cell model of AD. A postmortem study observed a decrease in mRNA levels of both TFAM and mitochondrial polymerase subunit γ (POLG) (Young-Collier et al. 2012). Studies also observed lower TFAM protein levels in mice models of AD carrying PS1 and ADswe mutations (Pedrós et al. 2014; Petrov et al. 2016). Moreover, overexpression of TFAM in a mouse model of AD resulted in improved cognitive function, a reversal in mitochondrial dysfunction, lower levels of the 8-OXG oxidative stress marker, and less intracellular Aβ accumulation (Oka et al. 2016). Similarly, overexpression of TFAM in in vitro models of AD neurons resulted in lower ROS formation, better OXPHOS function, and higher mtDNA copy number (Xu et al. 2009).
Another mitochondrial dysfunction is protein transport. Since 99% of the mitochondrial proteins are of nuclear origin, mitochondrial function depends on mitochondrial transport (Wiedemann and Pfanner 2017; Harbauer et al. 2014; Chai et al. 2018). This process is performed by translocase of the inner membrane (TIM), and translocase of the outer membrane (TOM) complexes. Interestingly, a study observed a decrease in TOM20 and TOM70 subunits levels in AD hippocampus. This decrease was correlated with the decrease in complexes III, IV (COX), and V proteins levels (Chai et al. 2018). Liang et al. observed a 2.7-fold and 2.6-fold reduction in the mRNA of 3 out of 11 subunits for TIM, and in 4 out of 6 subunits for TOM complexes, respectively (the exact genes found to be reduced are not mentioned).
Hence, it is well documented that AD neurons in the hippocampus suffer from mitochondrial dysfunction that seem to start from underexpression of nuclear genes crucial for mitochondrial function and homeostasis. Some of these genes include many OXPHOS genes, as observed by Liang et al. and Mastroeni et al. (see Table 1). Others include genes that are necessary for mtDNA metabolism and protein transportation into the mitochondria.
Table 1 lists genes found to be reduced in AD postmortem hippocampus tissue. Data collected from the studies by Liang et al. and Mastroeni et al. Liang et al. does not specify the exact genes: only the ratio of subunits’ genes found to be significantly reduced (p < 0.01) in the category was reported and is mentioned above. Mastroeni et al. collected microarray data of OXPHOS genes. In the table, each category lists only the top four genes with the greatest decrease in expression, along the minimal reduction in expression. More genes found to be downregulated in AD are not listed, such as TFAM and POLG were reduced in AD brains (see Young-Collier et al. and Sheng et al.). *Only the reduction in SDHA subunit mRNA stands out. The other three subunits were reduced by less than 5%, and therefore not listed.
GABP and mitochondrial damage
It is well established that GABP is a regulator of nuclear mitochondrial genes (Gugneja et al. 1996). GABP binding sites were found in several human genes involved in mitochondrial homeostasis (Chen et al. 2009; Kelly and Scarpulla 2004), including those that regulate OXPHOS, mtDNA metabolism and transport into the mitochondria, functions that are impaired in AD (see "Mitochondrial Dysfunction in AD"). To further examine the effect of GABP on the mitochondria, Yang et al. used mouse embryonic fibroblasts (MEFs) wild type (WT) and with floxed GABP (Yang et al. 2014). They observed a decrease in mitochondrial mass, count, and mtDNA copy number in the floxed GABP group. ATP production and oxygen consumption were also noticeably lower, indicating that OXPHOS activity is strongly dependent on GABP.
An in vitro study by Ongwijitwat et al. examined the effect of GABP on mitochondrial proteins and activity (Ongwijitwat et al. 2006). Using RNAi, GABP was decreased by more than 50%. As a result, the transcripts of all ten nuclear encoded COX genes in F2 cells were also decreased. Over 50% decrease was seen in the mRNA levels of COX4I1, COX5A, COX6B, COX6C, COX7A, COX7B, COX7C, and COX8. The group later found that COX enzymatic activity was lower by 20%. Next, using tetrodotoxin (TTX), a chemical known to induce transcriptional downregulation and inhibition of COX activity, the group observed a 60% decrease in the COX4I1 promoter activity. Overexpression of GABP reversed the effect of TTX.
As noted, Yang et al. observed a decrease in mtDNA copy number in floxed GABP cells. To further examine the relationship between GABP and mtDNA metabolism, Bruni et al. measured seven proteins involved in mtDNA transcription and replication (Bruni et al. 2010). Using ChIP analysis on human HeLa cells, they observed enrichments in the promoters of five genes: mitochondrial termination factor (mTERF), RNA polymerase POLRMT, TWINKLE, mtSSB, and POLG-b genes. Later, GABP silencing using RNAi resulted in up to 50% reduction the mRNA levels of all five genes. Overexpression of GABP resulted in 2–2.6-fold increase in the transcripts levels of these genes.
Besides COX subunits, Ongwijitwat et al. observed a decrease in the mRNA levels of many other genes following GABP knock down: TFAM, mitochondrial transcription factor B isoform 1 (TFB1M), surfeit 1 (SURF1), voltage-dependent anion channel (VDAC1), and TOM20 genes.
Put together, these results are consistent with the observations reported by Yang et al. regarding the effect of GABP on mitochondrial biogenesis, mtDNA metabolism, and OXPHOS function. Following a decline in the availability of GABP, many mitochondria related genes show underexpression (see), and a mitochondrial dysfunction typical of AD. The low OXPHOS activity, ATP production, accumulation of ROS, and inappropriate mitochondrial gene expression profiles, are similar in both cases, suggesting a possible link. In a study mentioned above, Sheng et al. examined overexpression of PGC-1α in the M17 cells, a model of AD, attempting to find out whether it resolves the mitochondrial abnormalities found in these cells. PGC-1α is known to upregulate GABP downstream. As expected, GABP levels increased, which improved the deficient mitochondrial function. This study provides additional support to a possible role of a GABP deficiency in the mitochondrial abnormalities observed in AD. However, Table 2 includes only human genes.
AD pathology number 3: impaired long-term synaptic plasticity and neuronal survival
AD patients carry cognitive disabilities, which are explained by impaired neuroplasticity and function. Interestingly, the expression of three genes responsible for neuroplasticity is decreased in AD brains: NMDA glutamate receptor subunits NR1 and NR2b and BDNF.
NMDA receptor dysregulation in AD
The NMDA (N-methyl-D-aspartate) glutamate receptors are widely spread in the CNS. In adults, they are composed of a combination of two NR1 subunits and two NR2A-D subunits (McBain and Mayer 1994). Synapses containing NMDA receptors (NMDAR), particularly those composed of NR1 and NR2b subunits, are involved in memory, learning and long-term potentiation (LTP) (El Gaamouch et al. 2012; Tang et al. 1999). Abnormal regulation of the NMDAR subunits is implicated in the pathophysiology of neurological diseases, such as bipolar disorder (Fountoulakis 2012), schizophrenia (Balu 2016), depression, Huntington’s disease (Lakhan et al. 2013), and Parkinson disease (Loopuijt and Schmidt 1998). A similar dysregulation of NMDAR was found in AD.
In AD, brain cells die, and synapses are lost. Brain regions in healthy individuals have high levels of NMDARs, especially in those severely affected in AD, such as the hippocampus, entorhinal, and peripheral cortices (Hyman et al. 1989; Suzuki et al. 1993; Ułas and Cotman 1997). The following three studies measured the concentration of NMDAR in AD brains.
Ułas et al. (Ułas and Cotman 1997) showed a decrease of up to 45% in the expression of the NR1 subunit gene Grin1 in AD postmortem brains. Hynd et al. (2004) reports similar observations with the NR2b subunit. The study found a threefold and fivefold decrease in the mRNA and protein levels of NR2b (Grin2b gene), respectively. The decrease was observed in AD pathologically susceptible regions only.
Sze et al. (2001), who examined the levels of several NMDAR subunits in postmortem early and definite AD patients, found a 53% decrease of NR1 protein levels in AD hippocampus tissue. In addition, the study found a 40% and 31% decrease in NR2b subunit levels in the hippocampus and entorhinal cortex, respectively. However, the study emphasizes that these changes were observed only with definite AD, but not with early AD, that is, patients lacking the clinical manifestation of dementia.
Another study examined the concentration of NMDAR throughout AD clinical progression. Mishizen-Eberz et al. (2004) examined postmortem hippocampus tissues of mild, moderate, and severe AD patients. The results showed an association between the disease stage and the decrease in mRNA and protein levels of both NR1 and NR2b subunits. In comparison to mild patients, moderate and severe patients showed a 16% decrease in NR1 mRNA. The levels of NR1 protein were also reduced by 14% and 33% in moderate and severe AD brain, respectively. A similar decrease was observed with the NR2b subunit. The study observed a 16% average decrease in mRNA levels in moderate and severe AD patients, in comparison to mild cases. The study does not report a comparison to healthy individuals. The results in Mishizen-Eberz et al. implicate NMDARs, and especially the NR1 and NR2b subunits, in the clinical progression of AD.
As these studies showed, the levels of the NR1 and NR2b subunits of the NMDAR are reduced in the course of AD. One interesting question is: why are these subunits reduced? Numerous studies showed that Aβ induces synaptic NMDAR internalization via endocytosis, both in vivo and in vitro (Kurup et al. 2010; Dewachter et al. 2009; Lacor et al. 2007). Surface levels of NR2b and NR1 were also reduced in ADswe mice overexpressing the human familiar Swedish mutation (Snyder et al. 2005). Two studies have shown that knocking down a protein involved in the internalization process resulted in greater surface NMDAR levels, a reversal of cognitive deficits, and improved hippocampal memory and LTP (Zhang et al. 2010; Venkitaramani et al. 2011). However, this explanation does not address the observed decrease in levels of the NMDAR subunits mRNA.
Another interesting question is: how do low NMDAR levels contribute to AD pathology?
Using different animal models, Vergas et al. (2011) showed that low NMDARs activation leads to an increase in the extracellular Aβ levels, whereas high NMDAR activity results in up to a 50% decrease of the extracellular Aβ. The study suggested a mechanism involving the recruitment of ERK (extracellular regulated kinase). Activation of NMDAR, activates the ERK signaling cascade, which eventually reduces the formation of Aβ via shifting to the non-amyloidogenic α-secretase pathway (Marcello et al. 2007). However, under normal conditions, the basal NMDAR activity was sufficient in suppressing APP processing to Aβ. This suggests that healthy brains, which have basal NMDAR activity, should normally suppress Aβ levels, whereas downregulation of NMDAR activity may lead to Aβ accumulation and AD.
These studies showed that NMDARs, and particularly NR1 and NR2b, are important in the etiology of AD. Low NMDAR levels, as seen in AD brains, leads to impaired synaptic plasticity and LTP, and greater accumulation of Aβ. This, eventually, results in AD and its clinical manifestation, mainly dementia.
NMDA receptors and GABP
As shown above, the expression of NR1 and NR2b subunits is reduced in AD. Priya et al. tested the effect of GABP on NMDAR subunits genes (Priya et al. 2013). To measure the effect, the study performed several experiments.
ChIP
Using murine N2a cells, ChIP showed GABP positive bands for Grin1 (NR1 subunit) and Grin2b (NR2b subunit) genes only. Same results were found in an in vivo ChIP assay over murine visual cortex extract, binding to the genes promoters both in vivo and in vitro.
Promoter mutants
Next, Priya et al. used N2a cells mutants in their GABP binding sites. The cells showed reduced Grin1/Grin2b promoter activity by 26% and 41%, respectively.
Promoter mutants + KCl
Priya et al. checked whether adding KCl, known to stimulate NR1 and NR2b transcription, restores the mutant promoters' expression. With the wild-type (WT) group, addition of KCl enhanced Grin1 and Grin2b expression by 50%. In contrast, the mutants group still presented reduced expression by 20–30%.
GABP knockdown
Knocking down GABPα using RNAi led to an average of 55% decrease in GABPα mRNA and protein levels. The decrease in GABPα reduced the mRNA levels of both Grin1 and Grin2b subunits by more than 38%.
GABP knockdown + KCl
Next, Priya et al. repeated the procedure adding KCl to GABP knockdown cells. The WT group showed a greater than twofold increase in the subunits’ expression. In contrast, the knockdown group did not show any increase with KCl addition. It showed an about 30% decrease in the genes’ expression. These results highlight the effect of GABP on the Grin1 and Grin2b genes.
Over expression of GABP
In N2a cells, an overexpression of GABP (over 3.5-fold increase in GABP subunits levels) led to a large increase in the subunits’ levels. The mRNA levels of Grin1 and Grin2b increased by 158.6% and 221.7%, respectively, and the protein levels by 422% and 376%, respectively.
Over expression of GABP + TTX
Tetrodotoxin (TTX) is known to decrease the expression of the subunits (Dhar and Wong-Riley 2009). The study examined the effect of an over expression of GABP on the downregulation effect of TTX. As expected, the addition of TTX decreased the expression of Grin1 and Grin2b by 79% and 48%, respectively. An over expression of GABP reversed the effect of TTX.
The results reported in Priya et al. show that GABP increases the expression of the NMDAR subunits.
BDNF and AD
Trophic factors are important for neuronal homeostasis and function. Some, especially brain-derived neurotrophic factor, were implicated early in AD. BDNF is an important player in neuronal function. It contributes to stimulating acetylcholine release, sustaining neuronal survival and neuroplasticity (Acheson et al. 1995). Similar to NMDARs, BDNF-mutant or knockout mice have significantly reduced LTP (Olofsdotter et al. 2000; Korte et al. 1995). Correspondently, administration of exogenous BDNF restored cognitive function (Patterson et al. 1996).
A study showed that abnormal expression of BDNF may cause cognitive decline typical of AD, and therefore, should be considered as a therapeutic target (Fumagalli et al. 2006). Interestingly, BDNF was also proven to take part in neurogenesis. It regulates the proliferation/differentiation balance of neural stem cells (NSC) and progenitor cells (PC), and controls the increase in the number of new adult-born neurons (Park and Poo 2013). In a study by Blurton-Jones et al. BDNF induced a cognitive recovery of AD mice models upon NSC transplant to the hippocampus (Blurton-Jones et al. 2009). BDNF is highly expressed in NSC/PC compared to mature neurons (Kamei et al. 2007). Using tests that measure gain and loss of function, Blurton-Jones et al. determined the basal expression of BDNF in NSC/PC, which is necessary for their effects on cognition and synaptic density.
It is well established that both the protein and mRNA levels of BDNF are reduced in AD brains. Hock et al. found a decrease in BDNF protein levels in four AD brain regions (Hock et al. 2000). The decrease was especially pronounced in the hippocampus, with an up to twofold decrease. Connor et al. (1997) also noticed a decrease. They observed a 70% decrease in BDNF immunoreactivity in the dentate gyrus of AD patients. The BDNF-immunopositive neurons count was also strongly reduced in the CA1 region.
The reason for the decrease might be a transcriptional downregulation. Several studies noticed a decrease in BDNF mRNA levels in postmortem. Hybridization and RNase assay revealed a fourfold and twofold decrease in BDNF expression in the hippocampus, respectively (Phillips et al. 1991). Another study noticed a 20–70% decrease in the mRNA levels of BDNF in the hippocampus (Murray et al. 1994).
It is therefore clear that BDNF expression is downregulated in the course of AD. The mechanism suggested includes downregulation of Aβ over the cAMP response element (CRE) binding protein (CREB), a transcription factor that regulates the BDNF gene. Phosphorylation by Akt and Erk turns CREB into an active phosphorylated CREB (pCREB), the form that recruits cellular coactivators to facilitate the transcription of the BDNF gene (Shieh et al. 1998). Aβ was found to inhibit CREB phosphorylation, and therefore BDNF expression in vivo (Tong et al. 2001) and in vitro (Garzon and Fahnestock 2007). Hence, through CREB, Aβ can induce transcriptional downregulation of BDNF and contribute to cognitive deficits in AD. In this paper, we show how a latent HSV-1 may also lead to a similar downregulation of BDNF in both NSC/PC and mature neurons.
BDNF-IX, GABP
As reviewed by Zheng et al. the BDNF gene is composed of nine exons in rodents and human (Zheng et al. 2012). Exons I-VIII are noncoding exons, while exon IX is the coding exon. Each exon has a promoter, referred to as “promoter I-IX,” regulating transcription. Exons I–VIII carry a regulatory role, while the end product is an identical mature BDNF protein. Interestingly, as all AD pathological genes reviewed in this paper, BDNF exon IX (BDNF-IX) is also transregulated by GABP.
Nair and Wong-Riley showed that GABP upregulates transcription from the coding exon IX (Nair and Wong-Riley 2016). First, in silico analysis revealed four N-box sequences in the IX promoter. EMSA and ChIP assays showed that two out of the four binding sites interacted with GABP. Mutating each of these sites decreased luciferase activity by up to 62%. Next, Nair and Wong-Riley knocked down GABPα using RNAi in visual cortical rat neuronal cultures. The 50% decrease of GABPα protein levels caused a 43% and 53% decrease in BDNF-IX mRNA and BDNF protein levels, respectively. Addition of KCl, known to stimulate the transcription, did not reverse the effect. Finally, overexpression of GABPα and GABPβ increased the proteins’ levels by more than 1.8-fold. This increased the BDNF-IX mRNA and BDNF protein levels by 249% and 167%, respectively. Using TTX did not reverse the effect. Finally, the study states that the two active GABP biding sites are conserved between mice and rats, and partially conserved in humans. Hence, Nair and Wong-Riley concluded that GABP is a transcriptional regulator of BDNF-IX exon, and decreasing its availability may lower BDNF levels, causing cognitive deficits observed in AD.
AD pathology number 4: unbalanced neurogenesis
Hippocampal neurogenesis is impaired in AD.
Neurogenesis and AD: the abortive birth of new neurons
Neurogenesis is under intensive research, and not yet fully understood. In the adult brain, neurogenesis is restricted to two zones: the subventricular zone (SVZ), and the hippocampus dentate gyrus (DG) in the sub region called the sub granular layer (SGL). Neurogenesis originates in neural stem cells (NSC), which proliferate to generate more NSC. With a specific stimulus, NSC give rise to progenitor cells (PC), which can proliferate a few more times, and then differentiate (Zhao et al. 2008). Differentiated PC can divide into neuroblasts (Nb) and glial cells, later migrating and forming mature neurons and glia. Neurogenesis was previously associated exclusively with developmental stages and youth. However, recent studies in animals and postmortem tissues showed that although moderately decreased with age, neurogenesis continues to the 10th decade of life (Moreno-Jiménez et al. 2019; Tobin et al. 2019).
Dentate gyrus (DG) neurogenesis is associated with improved memory, learning, and cognitive ability during aging (Richards and Frankland 2017; Lazarov and Hollands 2016). Neurogenesis abnormalities are linked with neurocognitive disease, including Alzheimer’s disease.
An in vivo study by Demars et al. showed a decrease of up to 36% in proliferating and differentiating cells in transgenic mice expressing the APPswe mutation (Demars et al. 2010). The reduction was observed early, before the onset of AD symptoms. More studies observed similar results in PS1 (presenilin-1) knockdown mice (Lalonde et al. 2005; Wang et al. 2004; Feng et al. 2001; Jankowsky et al. 2005).
Similar observations are reported in postmortem studies. For instance, Moreno-Jiménez et al. observed a decline in neurogenesis very early in AD, even before the pathological presence of NFT and amyloid plaques (1995). In 45 individuals, with Braak I to VI scores, they observed a decline in neurogenesis with the progression of the disease. Specifically, they observed an over 30% and 65% decrease in differentiating PC and Nb counts in individuals with Braak I and VI scores, respectively, showing an inverse relationship between neurogenesis and clinical progression in AD. Another study observed a direct relationship between reduced neurogenesis and worsening cognitive scores and clinical symptoms in Mild Cognitive Impairment (MCI) and AD patients (Patterson et al. 1996).
Briley et al. (2016) preformed a postmortem analysis on the brains of healthy, AD, MCI, and nondemented with Alzheimer’s disease neuropathology (NDAN) patients. NDAN patients showed the full neuropathological features of AD; however, they remained cognitively intact. Both AD and MCI patients demonstrated a decrease in total proliferating, differentiating cells, and immature neurons cell counts. For instance, AD patients showed up to twofold decrease in proliferation cell markers. Interestingly, NDAN patients showed increased counts of both proliferating and immature cells. NDAN patients also showed a decrease in the transcripts of miRNAs that downregulate neurogenesis, in contrast to AD and MCI patients. Notably, higher ratios of undifferentiated NSC and newly formed neurons were associated with higher cognitive MMSE scores. This cannot be explained by a reduced number of mature neurons, because the overall counts of mature neurons were not significantly different among the groups. Actually, a negative correlation was found between mature neurons counts and MMSE scores, suggesting that those neurons represent an older population of neurons, associated with poor cognitive scores.
Briely et al. suggested that, occasionally, diseased brains enhance the already impaired proliferation in an attempt to fix the defects, an attempt that fails in AD brains. This explains the controversial and inconclusive results found in postmortem studies, regarding the up- or downregulation of NSC/PC proliferation in AD brains (Gatt et al. 2019).
These studies suggest the existence of an association between impaired neurogenesis and AD. By increasing NSC proliferation, successful differentiation, and survival of the newborn neurons, the brain tries to stop the progression of the disease, and prevent the cognitive decline, as observed in NDAN patients. In support of this conclusion, several in vivo and in vitro studies showed a trend towards recovery from neurodegenerative diseases after restoring neurogenesis (Cosacak et al. 2019; Diaz Brinton and Ming Wang 2006; Papadimitriou et al. 2018). In a study by Blurton-Jones et al. mentioned above, NSC transplant to the hippocampus in AD transgenic mice was beneficial in improving cognitive function, without altering Aβ pathology. The study credited the improvement to BDNF activity, implying BDNF has a role in the quality of neurogenesis.
Whether neurogenesis is successful (healthy/NDAN) or unsuccessful (AD) depends on the balance between proliferation, differentiation, and survival of the immature neuron.
In the upcoming sections, we will explain how HSV-1 decreases NSC/PC proliferation, reducing the neurogenic available pool, leading to the cognitive decline in AD.
Neurogenesis and GABP
It is well established that GABP is involved in embryonic stem cells’ proliferation and survival. In GABP-null embryonic stem cells, proliferation was strongly repressed, and the cells died within 2 days (Ueda et al. 2017). However, until recently, GABP was not examined in relation to neural stem/progenitor cells (NSC/PC). A study by Liu et al. examined this relationship in vitro and in vivo (Liu et al. 2019).
First, the study showed that GABP is functional in NSC/PC both in vitro and in vivo. In fact, its expression levels were twofold higher in NSC/PC than in mature neurons. Next, the study knocked out certain splice variant of the GABPβ subunit. The result was a decrease in the number and size of the neurospheres. Next, they used in vivo models of adult mice. They injected RNAi targeting GABPβ into the right dentate gyrus (DG), and a control vector into the left DG of the same mouse. The result was a 40% decrease in proliferation markers. In addition, GABPβ knock down resulted in cell cycle arrest from G1 to S phase, followed by quick differentiation. Based on these results, Liu et al. concluded that GABP might alter the expression of cell cycle/apoptosis/DNA replication genes. Quantitate PCR (q-PCR) analysis revealed that GABPβ knock down downregulates most genes participating in cell cycle and DNA replication, and upregulates those participating in the PI3K/Akt, p53, and tissue necrosis alpha (TNF) signaling pathways, and apoptosis. Overall, a total of 810 genes were differentially expressed, of which 510 were upregulated and 300 downregulated. See Table 3 for a list of 15 genes strongly downregulated and 15 genes strongly upregulated following GABPβ knock down in NSC/PC.
The results in Liu et al. showed the effect of GABP on NSC/PC life cycle, suggesting that GABPβ is crucial for upregulating NSC/PC proliferation.
Another study examined hematopoietic stem/progenitor cells. They observed that the GABPα subunit was crucial for their differentiation and survival (Yu et al. 2011). GABPα null mice bone marrow LSK cells and myeloid progenitors demonstrated increased proliferation, whereas GABPβ knock out in NSC/PC results in rapid differentiations and decrease in proliferation (according to Liu et al.). This indicates that the different GABP subunits are involved in different stem cells stages. By regulating the expression of cell cycle/apoptosis/DNA replication genes, GABP affects the proliferation/differentiation balance in NSC/PC.
These results suggest that GABP is regulating the neurogenic pool balance by affecting NSC/PC proliferation and differentiation.
GABP transcription factor and the AD pathologies
As described in the previous sections, the GABP transcription factor regulates many genes associated with AD. Also, GABP forms the GABP•p300/CBP transcription complex, which is limiting.
-
i.
GABP upregulates the expression of BECN1, which, in turn, regulates cellular degradative traffic including autophagy. A decrease in the availability of the limiting GABP•p300/CBP decreases the expression of BECN1, and impairs autophagy in neurons. This may lead Aβ accumulation and AD.
-
ii.
GABP dominates the regulation of many genes involved in mitochondrial biogenesis and function (see). A decrease in the availability of the limiting GABP•p300/CBP complex can cause oxidative stress, which may disrupt synaptic transmission and neuronal function in hippocampus neurons, and may, eventually, lead to the development of AD.
-
iii.
GABP also upregulates the two NMDA receptor subunits NR1 and NR2b genes Grin1 and Grin2b. A decrease in the availability of the limiting GABP•p300/CBP complex decreases the expression of these two NMDAR. The decrease may disrupt synaptic plasticity, causing accumulation of Aβ plaques, and AD.
-
iv.
GABP, and p300/CBP dominate the expression of BDNF gene exons IX in mature neurons and in NSC/PC. A decrease in the availability of p300/CBP in neurons may lead to memory impairment, neuronal death and cognitive deficits, and hence eventually AD. In addition, reducing BDNF in NSC/PC will impair the potential neurogenesis has with preventing AD.
-
v.
GABP subunits have a key role in neural stem/progenitor cells proliferation and differentiation, which determines the overall neurogenic pool. A decrease in the availability of the limiting GABP•p300/CBP complex impairs the hippocampus ability to counteract neuronal damage via neurogenesis. Therefore, depleting GABP•p300/CBP in NSC/PC may impair the quantity and quality of neurogenesis (see list item iv above). This may lead to cognitive defects and dementia.
As these points suggest, a decrease in the availability of the limiting GABP•p300/CBP seems to be the link between all four pathologies characteristic of AD.
Latent HSV-1 and AD: the microcompetition model
HSV-1 latency
The HSV-1 life cycle consists of three main phases:
-
i.
Acute: HSV-1 is mostly acquired through the epithelium, usually oral. After the initial infection, viral components, proteins, and replicated genomes are packed in capsids ready for to be released towards the CNS. By 14 to 21 days pi, lytic genes levels are almost undetectable.
-
ii.
Latency: After being released from the epithelium, viral capsids enter the nervous system via sensory neuron axons terminals, and move retrograde to the soma. This step takes about a week to complete. In mouse models, the virus was observed in the trigeminal ganglia as early as 12 h post infection (pi) (Miller et al. 1998). At this point, 28 days pi, HSV-1 is present only in the latent state (Perng et al. 1996). During latency, the HSV-1 virus expresses the latency-associated transcripts (LATs) (Held and Derfuss 2011). The viral strategy during latency is to favor survival. First, staying quiescent helps the virus evade intrinsic and outer immune systems. Second, it inhibits host’s apoptosis using the LATs (Carpenter et al. 2007). In addition, HSV-1 sets a latent infection in neurons. It should be noted, that the current understanding of the molecular dynamics during latency is limited, and research in this topic is ongoing.
-
iii.
Reactivation/lytic: Given a specific stimulus, such as UV, fever, menstruation etc. (You et al. 2017), HSV-1 can reactivate from latency and become lytic. It has to overcome the repression mechanisms set during latency over lytic genes. The virus replicates its genome, synthesizes virulence factors and viral proteins. Eventually, the capsid moves anterograde, and leaves the host. The target tissue is usually the epithelium. In many cases, reactivation results in neuronal destruction by apoptosis/phagocytosis (Doll et al. 2020; Olney et al. 2002; Henken et al. 1993).
Latency is the longest phase. It extends over 95% of the time of the infection. The virus reactivates for short periods of time only (matter of hours/days) (Mark et al. 2008). In addition, not all neurons are capable of reactivating the latent HSV-1 (Singh and Tscharke 2020).
Also, during latency, the virus interacts with host signaling proteins, modifying transcription, and the balance between apoptosis and survival. For instance, studies observed that LATs and viral glycoproteins inhibit the apoptosis cascade via interacting with cellular factors (Henderson et al. 2002; Jin et al. 2003; Nguyen and Blaho 2006; Peng et al. 2004; Jerome et al. 2001; Aubert et al. 2008).
In addition, the host has its own special signaling programs to maintain latency and cellular survival. HSV-1 uses NFG (neuronal growth factor), mTORC1, Akt, and PI3-K to maintain latency. Eliminating both NFG and mTORC1 quickly resulted in reactivations (Kobayashi et al. 2012; Camarena et al. 2010; Hill et al. 1997). Along with LAT, these signaling programs take part in sequestration of transcriptional activators, epigenetic modifications, and recruitment of cellular repressors needed for maintaining latency.
Lastly, extraneuronal factors also play a part in maintaining HSV-1 latency. Glia and CD8 + T cells have an active role in maintaining latency. CD8 + T cells prevent reactivation and maintain latency with secreting interferon-γ and granzyme B (Knipe and Cliffe 2008; Deshmane and Fraser 1989; Leger and Hendricks 2011; Knickelbein et al. 2008).
ICP4 expression during latency
In this paper, we focus on the effect of HSV-1 on the host during the latent period. Therefore, we concentrate on the viral genes expressed during latency. Although ICP4 (infected cell polypeptide 4) is a member of the HSV-1 IE genes, which are considered by many to be epigenetically silenced during latency, studies showed that ICP4 is expressed during that time. For instance, Feldman et al. reported expression of ICP4 in neuronal and non-neuronal cells of latently infected trigeminal ganglia (TG) (Feldman et al. 2002). Kwiatkowsky et al. reported that ICP4 had more molecules per genome than tk and gC during HSV-1 latency (Kwiatkowsky et al. 2009). Taus and Mitchell reported that the ICP4 promoter was activated in a large number of Schwann cells in the trigeminal ganglia during latent HSV-1 infection (Taus and Mitchell 2001). Furthermore, Kramer and Coen reported an ICP4-specific RNA signal in latently infected trigeminal ganglia at a level of 1.6 × 102 to 2.5 × 104 molecules per ganglion (Kramer and Coen 1995). Studies in the mouse detected ICP4 transcripts in ganglia during latency (Preston et al. 2007). Also, consider the heterogeneity of genes expression levels and timing during HSV-1 latency observed in Yang et al. (2000) and Sawtell (1997). To summarize, studies reported that the ICP4 promoter is transactive during latency.
HSV-1 and GABP
The promoter of the ICP4 gene contains the cis-regulatory element CGGAAR as a tandem repeat (LaMarco and McKnight 1989). Binding of cellular transcription factors to the CGGAAR site in the ICP4 promoter transactivates the viral gene (Bzik and Preston 1986; Triezenberg et al. 1988). One of these factors is GABP (LaMarco et al. 1991; Douville et al. 1995; Hagmann et al. 1995). Hagmann et al. analyzed GABPα/β expression in mammalian cell lines and neural tissues. They observed a ternary complex consisting of a single GABPα/β heterodimer on a single CGGAAR site in the ICP4 promoter (Hagmann et al. 1995). Another study observed that GABP cooperatively interacts with the Oct-1/VP16 transcription factor complex to facilitate transcription controlled by the ICP4 HSV-1 promoter through synergistic activation (Douville et al. 1995). Furthermore, the immediate early (IE) enhancer core of HSV-1 was found to have a neighboring binding site for GABP in several studies (Vogel and Kristie 2000; Narayanan et al. 2005; Nogueira et al. 2004). Gel shift analysis, showed that GABP interacts with the C1 factor, a vital coordinator of the HSV-1 enhancer complex assembly. Although the study of latency is poor and inconclusive, these studies indicate that GABP binds to the HSV-1 promoter, and interacts with specific transcription factors to enhance transcription of HSV-1 IE genes.
It should be noted that the sequestering effect occurs every time there is an expression of viral genes that bind GABP, such as ICP4. Of course, this can happen both during the latent and the lytic phases. We concentrate on the latent phase since it is the longest period of the viral life cycle and fits the slow development of AD. Also, during the lytic phase, the cell most often dies, and therefore does not exhibit the long term abnormal behavior typical of AD.
The microcompetition model
The microcompetition model was first described in Polansky (2003). According to the model, the genome of certain viruses includes a cis regulatory sequence called the N-box as part of the viral promoter/enhancer sequence. This sequence binds the cellular GABP•p300/CBP transcription complex, which is limiting. Therefore, the viral regulatory element competes with the cellular genes over the p300/CBP•GABP transcription complex. The competition causes the cellular genes that are transactivated by the p300/CBP•GABP complex to express fewer proteins, and the genes that are transsuppressed by the complex to express more proteins. This abnormal expression may lead to the development of a chronic disease. The microcompetition model was previously used to map out the viral and cellular dynamics of diseases such as breast cancer (Polansky and Schwab 2019), classic Hodgkin lymphoma (Polansky and Javaherian 2015a), and B-cell acute lymphoblastic leukemia (B-ALL) (Polansky and Javaherian 2015b).
The cause of AD according to the microcompetition model
During latency, the HSV-1 virus expresses the ICP4 gene. The viral promoter binds to the limiting GABP•p300/CBP transcription complex (Bannert et al. 1999; Bush et al. 2003). This sequesters the complex, which decreases its availability to cellular genes, including the BECN1 gene, over a dozen genes critical to mitochondrial function, homeostasis and biogenesis (see Table 2), the NMDA receptor subunits NR1 and NR2b, and gene groups regulating neurogenesis (see Table 3). The abnormal expression of these genes may cause the development of AD. See Table 4.
First note: It is possible that other HSV-1 genes also bind and sequester the limiting GABP•p300/CBP transcription complex during latency. This will enhance the effect of the ICP4 gene on the host.
Second note: The HSV-1 proteins VP16 and ICP0 also sequester the limiting p300/CBP independently of GABP (Du et al. 2013; Herrera and Triezenberg 2004; Melroe et al. 2007). However, VP16 and ICP0 are mostly expressed during reactivation.
The microcompetition mechanism leading to AD. The HSV-1 ICP4 gene sequesters the limiting GABP•p300/CBP transcription complex. This alters the expression of certain cellular genes, resulting in Aβ accumulation, mitochondrial dysfunction, impaired synaptic transmission via NMDAR and via BDNF signaling, and unbalanced NSC/PC proliferation/differentiation quantity as well and quality.
-
i.
HSV1, GABP, and BECN1
Many in vivo and in vitro studies observed extra- and intracellular Aβ accumulation following HSV-1 infection (Piacentini et al. 2011, 2015; De Chiara et al. 2010). Consider the following viral and cellular dynamics.
The competition between the N-box in the ICP4 IE HSV-1 gene and the BECN1 promoter for the limiting GABP•p300/CBP transcription complex decreases the expression of BECN1, which decreases the level of the BECN1-PIK3C3 complex. As reported in Swaminathan et al. BECN1 modifies the internalization and degradation of APP via endosomes and autophagosomes. The decrease in BECN1-PIK3C3 causes a decrease in the breakdown of APP, the toxic precursor to Aβ, leading to Alzheimer’s disease.
-
ii.
HSV1, GABP, and mitochondrial genes
ICP4 promoter competes with many promoters of crucial mitochondrial genes over the limiting GABP•p300/CBP transcription complex, decreasing its availability to the mitochondrial genes, including genes composing OXPHOS subunits, genes involved in mtDNA metabolism, and genes participate in mitochondrial homeostasis (see). The competition leads to a decrease in their expression, resulting in mitochondrial dysfunction, oxidative stress, and mitochondrial damage in neurons, causing flaws in synaptic communication, and eventually neuronal damage. These abnormal changes may lead to neurodegeneration and AD.
-
iii.
HSV1, GABP, and NMDA receptor subunits NR1/NR2b genes
Both the promoters of HSV-1 ICP4 gene and the NR1 (Grin1) and NR2b (Grin2b) NMDA receptor subunits genes compete for binding the limiting GABP•p300/CBP transcription complex. The competition results in lower expression of the cellular Grin1 and Grin2b genes. As shown by Priya et al. a 50% decrease in GABP levels resulted in an over 80% decrease in NR1 and NR2b levels. The decrease in NMDARs levels interrupts the synaptic plasticity, enhances Aβ amyloidogenic pathway, leading to dementia and AD.
-
iv.
HSV1, GABP, and BDNF
BDNF is an important neuronal factor active in neurons and highly expressed in NSC/PC. The sequestration effect by ICP4 reduces the allocation of GABP•p300/CBP to the promoters of BDNF exon IX. This leads to lower BDNF protein levels. Low BDNF levels are responsible for many cognitive defects, including impaired memory, LTP and low quality neurogenesis.
-
v.
HSV1, GABP, and neurogenesis
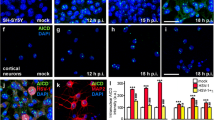
Does HSV-1 establish a latent infection in neural stem/progenitor cells? Li Puma et al. (2019) reports that 71.5% of the cells in a cell culture of proliferating NSC showed an HSV-1 infection, a sixfold higher percentage compared to cultured hippocampal mature neurons.
As we explained above, the ICP4 sequesters the limiting GABP•p300/CBP transcription complex decreasing its availability to genes regulating cell cycle/apoptosis/replication/cell signaling pathways (see), and to BDNF gene, hence altering the neural stem/progenitor cells’ ability to successfully proliferate, and differentiate. This leads to impaired neuronal regeneration in response to damage, and cognitive defects typical of AD. Li Puma et al. also found an association between HSV-1 and neurogenesis. HSV-1 infection increased Aβ levels in NSC, and inhibited NSC/PC proliferation and differentiation, both in vivo and in vitro. The group concluded that the inhibition of neurogenesis is associated with Aβ accumulation, which was shown before to decrease proliferation (Demars et al. 2013). Also, when the group used APP-null mice, HSV-1 infection had no effect on neurogenesis. It should be noted that these results are not consisted with the observations collected in postmortem and other in vivo studies described above that showed reduced neurogenesis prior to the appearance of Aβ. It is possible that the mice did not sustain a long enough latent infection (the group used an infection protocol of around 10 weeks, including a couple of thermal shocks during that period). Also, the viral copy number was possibly too low (see next section on copy number for details).
To summarize, according to the microcompetition model, the initial event is a latent infection with HSV-1. The final outcome is the development of Alzheimer’s disease.
HSV-1 and AD: why only a portion of the population develop AD?
The HSV-1 virus is highly prevalent. An estimated 3.7 billion people worldwide are infected, that is, around 67% of the global population (World Health Organization 2018). Since the virus is highly prevalent, why only a fraction of the infected people develop AD?
A recent paper by Pandey et al. offers an explanation (Pandey et al. 2020). They showed that homozygous individuals that carry the GM17 genetic variant of IgG1 gene have a fourfold higher risk for developing AD, regardless of the ApoE4 allele status. The GM17 variant allows HSV-1 to evade the host immune response by having lower levels of IgG1, thus, making it easier for the virus to infect the CNS and establish latency in the hippocampus. The study explains, at least in part, why some HSV-1 positive individuals will be more likely to develop AD. In this paper, we propose another answer that centers on the viral copy number during latency. Only a high enough copy number produces a strong enough sequestering effect that causes AD. See Fig. 1.
How the latent HSV-1 causes Alzheimer’s disease according to the microcompetition model. (A) Initial event, i.e., stress, surgery, aging, etc. occurs. (→ B) As a result, there is an increase in the copy number of the latent HSV-1 in neurons and neural stem/progenitor cells in the hippocampus. (→ C) The HSV-1 ICP4 gene promoter sequesters larger amounts of GABP•p300/CBP, reducing its availability to cellular genes. (→ D) The expression of cellular genes decreases: these genes include the BECN1, Grin1 (NR1), Grin2b (NR2b), and BDNF exon IX, also genes that regulate mitochondrial function, and genes responsible of proliferation (in neural stem/progenitor cells). (→ E) As a result, neurons malfunction and neurodegeneration occurs. (→ F) Clinical aspects of Alzheimer’s disease are manifested
Recently, a paper by Zuo et al. (2015) showed that the copy number of latent EBV, another virus that binds GABP•p300/CBP during latency, is strongly associated with oncogenicity (Lu et al. 2016; Polansky and Schwab 2018a). What determines the copy number of the latent HSV-1?
An in vivo study showed that, during latency, the HSV-1 copy number can range from less than 10 to over 1000 copies per cell in mice (Thompson and Sawtell 1997). Sawtell et al. also showed that the viral copy number depends on the viral strain and dose (Sawtell et al. 1998). They showed that the copy number of a latent HSV-1 in a single neuron can range from 1 to 910 copies, depending on the viral strain. In addition, frequent reactivations, starting with an acute replication, and during the latent stages of the infection might be contributing to the reservoir of viral genomes during latency.
Our understanding of latency is limited and inconclusive. Specifically, little is known about the dynamics and homeostasis of the viral reservoir during latency. However, some studies has shown that the steady state viral copy number is strongly dependent on the immune response. Many events can damage the immune system, including aging (Castelo-Branco and Soveral 2014), certain medications (Beghi and Shorvon 2011; Røge et al. 2012), surgery (Decker et al. 2005; Brøchner et al. 2016; Angka et al. 2017), chemotherapy, radiation (Ghiringhelli and Apetoh 2014), and stress (Vitlic et al. 2014). Those immune-damaging events may increase the HSV-1 copy number during latency. Perhaps, individuals that carry the GM17 variant of IgG1 have an inadequate immune response against HSV-1, resulting in higher replication, higher copy number, and eventually, AD. Zou et al. study showed that the EBV load in blood and tumor tissues, and hence the copy number, is strongly associated with the clinical course of lymphoma and NPC, and its prognosis. The microcompetition model based explanation is consistent with this observation.
As recalled, in the population based study in Taiwan mention above, HSV-1 infected/symptomatic patients were more likely to develop AD in comparison to the infected/asymptomatic individuals (Tzeng et al. 2018). Presumably, the patients with the higher odds for AD had a weaker immune system, resulting in a more severe viral disease. At the cellular level, the weaker immune system might have led to a higher viral copy number during the latent phase, and therefore increased odds of AD.
We conclude that the difference in copy number of HSV-1 during latency may distinguish between those who develop AD from those who do not. Interestingly, AD patients were found to have a weaker anti HSV-1 response. In a study by La Rosa et al. (2019), the inner immune interferon lambda (IFN-λ) anti-viral pathway was ineffective in AD. IFN-λ was not successful in controlling HSV-1. It is therefore suggested that an inefficient anti HSV-1 response may lead to a larger viral copy number, and a higher probability of developing AD.
What is next?
We highly recommend considering using anti-viral agents that target the latent HSV-1 as a preventive treatment. In the Taiwan population wide study by Tzeng et al. (2018), anti-herpetic agents significantly lowered the risk of developing dementia, including of Alzheimer type. Sawtell found that treatment with acyclovir reduced the number of latently infected neurons by a 20-fold, and equally, lowered the viral latent copy number of under 10 copies per cell in 100% of the examined pool (Sawtell 1997). Therefore, existing anti-viral agents may lower the viral copy number, and prevent the establishment of a latent infection in the first place. However, the literature is insufficient, and we encourage further research on the topic.
Another study by La Rosa et al. emphasized the importance of effective anti-viral response in stopping the progression to AD in Mild Cognitive Impairment (MCI) patients over a 24 months follow-up (La Rosa et al. 2016; 2017). During the two-year period, HSV-1 was mostly latent (Ariotti et al. 2014). This study suggests that that an effective anti-viral response, which targets both latent and lytic viruses, may be effective in stopping the progression of AD.
Along with anti-viral treatments, we recommend to assay viral gene expression and copy number during latency as a diagnostic, rather than settling for the common “HSV-1 positive” or “HSV-1 negative” tests. We believe that the results of the new assays may useful in predicting the future progression of the disease.
Our interpretation of the microcompetition model agrees with Zuo et al. According to the model, the copy number of HSV-1, and other viruses that sequester the limiting GABP•p300/CBP transcription complex, determines the faith of the infected individual. Therefore, we believe that the viral copy number and/or gene expression during latency should be measured in clinical practice with at risk patients. The greater the copy number, the more the virus sequesters GABP•p300/CBP transcription complex from cellular genes, including BECN1 gene, many mitochondrial genes, the NR1 and NR2b subunits, and genes promoting balanced neurogenesis, which together increase the risk of developing AD.
The sections above show how an increase in the copy number of the latent HSV-1 can cause AD. However, since the current understanding of the dynamics and homeostasis of the viral reservoir during latency is limited, the proposed model represents only a first step towards a complete understanding of the relationship between the copy number of the latent HSV-1 and Alzheimer’s disease.
Conclusion
-
In this paper, we use the microcompetition model to map out the viral and cellular dynamics of a latent HSV-1 infection in the brain. These dynamics explain the observed connection reported in many studies between the virus and Alzheimer’s disease, and provide a framework for further investigations.
-
According to the model, an increase in the copy number of the latent HSV-1 increases the sequestering of the limiting p300/CBP•GABP transcription complex. This disrupts the allocation of the transcription complex to cellular genes, specifically to BECN1, many important mitochondrial genes, two NMDA receptor subunits genes, BDNF gene, and genes promoting neurogenesis. When this disruption is large enough, the host develops AD.
-
This paper presents a model that connects seemingly unconnected observations on the copy number of the latent HSV-1 and AD. However, current research on viral latency and copy number homeostasis is limited, incomplete, sometimes contradictory, and therefore confusing. We believe that future research will clear up some of this confusion, and add important details to the proposed model.
-
How significant are models and theories in science? To answer this question, we would like to quote Albert Einstein (Calaprice 2000).
“The truly great advances in our understanding of nature originated in a way almost diametrically opposed to induction. The intuitive grasp of essentials of a large complex of facts leads the scientist to the postulation of a hypothetical basic law, or several such laws. From these laws, he derives his conclusions, … which can then be compared to experience. Basic laws (axioms) and conclusions together form what is called a “theory.” Every expert knows that the greatest advances in natural science … originated in this manner.”
Abbreviations
- HSV-1:
-
Herpes simplex virus-1
- AD:
-
Alzheimer’s disease
- PCR:
-
Polymerase chain reaction
- APP:
-
Amyloid β precursor protein
- co-IP:
-
Co-immunoprecipitation
- WCE:
-
Whole-cell extracts
- ECD:
-
Evolutionary conserved domain
- Aβ:
-
Amyloid-β
- GABP:
-
GA binding protein
- NRF2:
-
Nuclear respiratory factor 2
- GABPα:
-
GA binding protein alpha
- GABPβ:
-
GA binding protein beta
- ETS-TF:
-
ETS-domain transcription factor family
- ChIP:
-
Chromatin immunoprecipitation
- RT-PCR:
-
Reverse transcriptase PCR
- qPCR:
-
Quantitative PCR
- IE:
-
Immediate early
- LATs:
-
Latency-associated transcripts
- OXPHOS:
-
Oxidative phosphorylation
- COX:
-
Cytochrome C oxidase
- mtDNA:
-
Mitochondrial DNA
- NMDA:
-
N-methyl-D-aspartate glutamate
- NMDAR:
-
N-methyl-D-aspartate glutamate receptors
- WT:
-
Wild type
- NSC:
-
Neural stem cells
- PC:
-
Progenitor cells
- MCI:
-
Mild cognitive impairment
- Nb:
-
Neuroblasts
- NFT:
-
Neurofibrillary tangles
- BDNF:
-
Brain-derived neurotrophic factor
References
Acheson A, Conover JC, Fandl JP, DeChiara TM, Russell M, Thadani A, Lindsay RM (1995) A BDNF autocrine loop in adult sensory neurons prevents cell death. Nature 374(6521):450–453
Angka L, Khan ST, Kilgour MK, Xu R, Kennedy MA, Auer RC (2017) Dysfunctional natural killer cells in the aftermath of cancer surgery. Int J Mol Sci 18(8):1787
Arbizu J, Festari C, Altomare D, Walker Z, Bouwman F, Rivolta J, Nestor P (2018) Clinical utility of FDG-PET for the clinical diagnosis in MCI. Eur J Nucl Med Mol Imaging 45(9):1497–1508
Ariotti S, Hogenbirk MA, Dijkgraaf FE, Visser LL, Hoekstra ME, Song JY, Schumacher TN (2014) Skin-resident memory CD8+ T cells trigger a state of tissue-wide pathogen alert. Science 346(6205):101–105
Aubert M, Chen Z, Lang R, Dang CH, Fowler C, Sloan DD, Jerome KR (2008) The antiapoptotic herpes simplex virus glycoprotein J localizes to multiple cellular organelles and induces reactive oxygen species formation. J Virol 82(2):617–629
Balu DT (2016) The NMDA receptor and schizophrenia: from pathophysiology to treatment. In Advances in Pharmacology Vol 76, pp 351–382 Academic Press
Bannert N, Avots A, Baier M, Serfling E, Kurth R (1999) GA-binding protein factors, in concert with the coactivator CREB binding protein/p300, control the induction of the interleukin 16 promoter in T lymphocytes. Proc Natl Acad Sci 96(4):1541–1546
Bzik DJ, Preston CM (1986) Analysis of DNA sequences which regulate the transcription of herpes simplex virus immediate early gene 3: DNA sequences required for enhancer-like activity and response to trans-activation by a virion polypeptide. Nucleic Acids Res 14(2):929–943
Beghi E, Shorvon S (2011) Antiepileptic drugs and the immune system. Epilepsia 52:40–44
Bhattacharyya A, Chattopadhyay R, Hall EH, Mebrahtu ST, Ernst PB, Crowe SE (2010) Mechanism of hypoxia-inducible factor 1α-mediated Mcl1 regulation in Helicobacter pylori-infected human gastric epithelium. Am J Physiol Gastrointest Liver Physiol 299(5):G1177-G1186
Blurton-Jones M, Kitazawa M, Martinez-Coria H, Castello NA, Müller FJ, Loring JF, LaFerla FM (2009) Neural stem cells improve cognition via BDNF in a transgenic model of Alzheimer disease. Proc Natl Acad Sci 106(32):13594–13599
Bosetti F, Brizzi F, Barogi S, Mancuso M, Siciliano G, Tendi EA, Solaini G (2002) Cytochrome c oxidase and mitochondrial F1F0-ATPase (ATP synthase) activities in platelets and brain from patients with Alzheimer’s disease. Neurobiol Aging 23(3):371–376
Briley D, Ghirardi V, Woltjer R, Renck A, Zolochevska O, Taglialatela G, Micci MA (2016) Preserved neurogenesis in non-demented individuals with AD neuropathology. Sci Rep 6(1):1–10
Brøchner AC, Mikkelsen S, Hegelund I, Hokland M, Mogensen O, Toft P (2016) The immune response is affected for at least three weeks after extensive surgery for ovarian cancer. Dan Med J 63(6):A5243
Bruni F, Polosa PL, Gadaleta MN, Cantatore P, Roberti M (2010) Nuclear respiratory factor 2 induces the expression of many but not all human proteins acting in mitochondrial DNA transcription and replication. J Biol Chem 285(6):3939–3948
Bush TS, St. Coeur M, Resendes KK, Rosmarin AG (2003) GA-binding protein (GABP) and Sp1 are required, along with retinoid receptors, to mediate retinoic acid responsiveness of CD18 (β2 leukocyte integrin): a novel mechanism of transcriptional regulation in myeloid cells. Blood, The Journal of the American Society of Hematology 101(1):311–317
Calaprice A (2000) The expanded quotable Einstein. Princeton University Press P 237
Camarena V, Kobayashi M, Kim JY, Roehm P, Perez R, Gardner J, Chao MV (2010) Nature and duration of growth factor signaling through receptor tyrosine kinases regulates HSV-1 latency in neurons. Cell Host Microbe 8(4):320–330
Campbell CT, Kolesar JE, Kaufman BA (2012) Mitochondrial transcription factor A regulates mitochondrial transcription initiation, DNA packaging, and genome copy number. Biochimica et Biophysica Acta (BBA)-Gene Regulatory Mechanisms 1819(9–10):921–929
Carpenter D, Hsiang C, Brown DJ, Jin L, Osorio N, BenMohamed L, Wechsler SL (2007) Stable cell lines expressing high levels of the herpes simplex virus type 1 LAT are refractory to caspase 3 activation and DNA laddering following cold shock induced apoptosis. Virology 369(1):12–18
Castelo-Branco C, Soveral I (2014) The immune system and aging: a review. Gynecol Endocrinol 30(1):16–22
Chai YL, Xing H, Chong JR, Francis PT, Ballard CG, Chen CP, Lai MK (2018) Mitochondrial translocase of the outer membrane alterations may underlie dysfunctional oxidative phosphorylation in Alzheimer’s disease. J Alzheimers Dis 61(2):793–801
Chen JQ, Cammarata PR, Baines CP, Yager JD (2009) Regulation of mitochondrial respiratory chain biogenesis by estrogens/estrogen receptors and physiological, pathological and pharmacological implications. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research 1793(10):1540–1570
Connor B, Young D, Yan Q, Faull RLM, Synek B, Dragunow M (1997) Brain-derived neurotrophic factor is reduced in Alzheimer’s disease. Mol Brain Res 49(1–2):71–81
Cosacak MI, Bhattarai P, Reinhardt S, Petzold A, Dahl A, Zhang Y, Kizil C (2019) Single-cell transcriptomics analyses of neural stem cell heterogeneity and contextual plasticity in a zebrafish brain model of amyloid toxicity. Cell Rep 27(4):1307–1318
Coskun PE, Beal MF, Wallace DC (2004) Alzheimer’s brains harbor somatic mtDNA control-region mutations that suppress mitochondrial transcription and replication. Proc Natl Acad Sci 101(29):10726–10731
De Chiara G, Marcocci ME, Civitelli L, Argnani R, Piacentini R, Ripoli C, Palamara AT (2010) APP processing induced by herpes simplex virus type 1 (HSV-1) yields several APP fragments in human and rat neuronal cells. PLoS One 5(11):e13989
Decker D, Tolba R, Springer W, Lauschke H, Hirner A, von Ruecker A (2005) Abdominal Surgical Interventions: Local and Systemic Consequences for the Immune System—a Prospective Study on Elective Gastrointestinal Surgery1. J Surg Res 126(1):12–18
Demars M, Hu YS, Gadadhar A, Lazarov O (2010) Impaired neurogenesis is an early event in the etiology of familial Alzheimer’s disease in transgenic mice. J Neurosci Res 88(10):2103–2117
Demars MP, Hollands C, Zhao KDT, Lazarov O (2013) Soluble amyloid precursor protein-α rescues age-linked decline in neural progenitor cell proliferation. Neurobiol Aging 34(10):2431–2440
Deshmane SL, Fraser NW (1989) During latency, herpes simplex virus type 1 DNA is associated with nucleosomes in a chromatin structure. J Virol 63(2):943–947
Dewachter I, Filipkowski RK, Priller C, Ris L, Neyton J, Croes S, Godaux E (2009) Deregulation of NMDA-receptor function and down-stream signaling in APP [V717I] transgenic mice. Neurobiol Aging 30(2):241–256
Dhar SS, Wong-Riley MT (2009) Coupling of energy metabolism and synaptic transmission at the transcriptional level: role of nuclear respiratory factor 1 in regulating both cytochrome c oxidase and NMDA glutamate receptor subunit genes. J Neurosci 29(2):483–492
Diaz Brinton R, Ming Wang J (2006) Therapeutic potential of neurogenesis for prevention and recovery from Alzheimer’s disease: allopregnanolone as a proof of concept neurogenic agent. Curr Alzheimer Res 3(3):185–190
Doll JR, Hoebe K, Thompson RL, Sawtell NM (2020) Resolution of herpes simplex virus reactivation in vivo results in neuronal destruction. PLoS Pathogens 16(3):e1008296
Douville P, Hagmann M, Georgiev O, Schaffner W (1995) Positive and negative regulation at the herpes simplex virus ICP4 and ICPO TAATGARAT motifs. Virology 207(1):107–116
Du T, Zhou G, Roizman B (2013) Modulation of reactivation of latent herpes simplex virus 1 in ganglionic organ cultures by p300/CBP and STAT3. Proc Natl Acad Sci 110(28):E2621–E2628
El Gaamouch F, Buisson A, Moustié O, Lemieux M, Labrecque S, Bontempi B, Nicole O (2012) Interaction between αCaMKII and GluN2B controls ERK-dependent plasticity. J Neurosci 32(31):10767–10779
Feldman LT, Ellison AR, Voytek CC, Yang L, Krause P, Margolis TP (2002) Spontaneous molecular reactivation of herpes simplex virus type 1 latency in mice. Proc Natl Acad Sci U S A 99(2):978–983
Feng R, Rampon C, Tang YP, Shrom D, Jin J, Kyin M, Sisodia SS (2001) Deficient neurogenesis in forebrain-specific presenilin-1 knockout mice is associated with reduced clearance of hippocampal memory traces. Neuron 32(5):911–926
Fountoulakis NK (2012) The possible involvement of NMDA glutamate receptor in the etiopathogenesis of bipolar disorder. Curr Pharm Des 18(12):1605–1608
Fumagalli F, Racagni G, Riva MA (2006) The expanding role of BDNF: a therapeutic target for Alzheimer’s disease?. Pharmacogenomics J 6(1):8–15
Gatt A, Lee H, Williams G, Thuret S, Ballard C (2019) Expression of neurogenic markers in Alzheimer’s disease: a systematic review and metatranscriptional analysis. Neurobiol Aging 76:166–180
Garzon DJ, Fahnestock M (2007) Oligomeric amyloid decreases basal levels of brain-derived neurotrophic factor (BDNF) mRNA via specific downregulation of BDNF transcripts IV and V in differentiated human neuroblastoma cells. J Neurosci 27(10):2628–2635
Ghiringhelli F, Apetoh L (2014) The interplay between the immune system and chemotherapy: emerging methods for optimizing therapy. Expert Rev Clin Immunol 10(1):19–30
Gugneja S, Virbasius CM, Scarpulla RC (1996) Nuclear respiratory factors 1 and 2 utilize similar glutamine-containing clusters of hydrophobic residues to activate transcription. Mol Cell Biol 16(10):5708–5716
Hagmann M, Georgiev O, Schaffner W, Douville P (1995) Transcription factors interacting with herpes simplex virus α gene promoters in sensory neurons. Nucleic Acids Res 23(24):4978–4985
Harbauer AB, Zahedi RP, Sickmann A, Pfanner N, Meisinger C (2014) The protein import machinery of mitochondria—a regulatory hub in metabolism, stress, and disease. Cell Metab 19(3):357–372
Harris SA, Harris EA (2018) Molecular mechanisms for herpes simplex virus type 1 pathogenesis in Alzheimer’s disease. Front Aging Neurosci 10:48
Held K, Derfuss T (2011) Control of HSV-1 latency in human trigeminal ganglia—current overview. J Neurovirol 17(6):518–527
Henderson G, Peng W, Jin L, Perng GC, Nesburn AB, Wechsler SL, Jones C (2002) Regulation of caspase 8–and caspase 9–induced apoptosis by the herpes simplex virus type 1 latency-associated transcript. Neurovirol 8
Henken DB, Goldstein ME, Martin JR (1993) Herpes simplex virus type-2 infection by a footpad route results in neuronal death in mouse spinal ganglia. J Neurol Sci 115(2):177–183
Herrera FJ, Triezenberg SJ (2004) VP16-dependent association of chromatin-modifying coactivators and underrepresentation of histones at immediate-early gene promoters during herpes simplex virus infection. J Virol 78(18):9689–9696
Hill JM, Ball MJ, Neumann DM, Azcuy AM, Bhattacharjee PS, Bouhanik S, Kaufman HE (2008) The high prevalence of herpes simplex virus type 1 DNA in human trigeminal ganglia is not a function of age or gender. J Virol 82(16):8230–8234
Hill JM, Garza H, Helmy MF, Cook SD, Osborne PA, Johnson M, Gebhardt BM (1997) Nerve growth factor antibody stimulates reactivation of ocular herpes simplex virus type 1 in latently infected rabbits. J Neurovirol 3(3):206–211
Hock C, Heese K, Hulette C, Rosenberg C, Otten U (2000) Region-specific neurotrophin imbalances in Alzheimer disease: decreased levels of brain-derived neurotrophic factor and increased levels of nerve growth factor in hippocampus and cortical areas. Arch Neurol 57(6):846–851
Hung SY, Huang WP, Liou HC, Fu WM (2009) Autophagy protects neuron from Aβ-induced cytotoxicity. Autophagy 5(4):502–510
Hyman BT, Damasio H, Damasio AR, Van Hoesen GW (1989) Alzheimer’s disease. Annu Rev Public Health 10(115–140)
Hynd MR, Scott HL, Dodd PR (2004) Differential expression of N-methyl-D-aspartate receptor NR2 isoforms in Alzheimer’s disease. J Neurochem 90(4):913–919
Inczedy-Farkas G, Trampush JW, Perczel Forintos D, Beech D, Andrejkovics M, Varga Z, Molnar MJ (2014) Mitochondrial DNA mutations and cognition: a case-series report. Arch Clin Neuropsychol 29(4):315–321
Ishii K, Kitagaki H, Kono M, Mori E (1996) Decreased medial temporal oxygen metabolism in Alzheimer’s disease shown by PET. J Nucl Med 37(7):1159
Itabashi S, Arai H, Matsui T, Higuchi S, Sasaki H (1997) Herpes simplex virus and risk of Alzheimer’s disease. The Lancet 349(9058):1102
Itzhaki RF, Lathe R, Balin BJ, Ball MJ, Bearer EL, Braak H, Del Tredici K (2016) Microbes and Alzheimer’s disease. Journal of Alzheimer’s Disease: JAD 51(4):979
Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA (1997) Herpes simplex virus type 1 in brain and risk of Alzheimer’s disease. The Lancet 349(9047):241–244
Jamieson GA, Maitland NJ, Wilcock GK, Craske J, Itzhaki RF (1991) Latent herpes simplex virus type 1 in normal and Alzheimer’s disease brains. J Med Virol 33(4):224–227
Jankowsky JL, Melnikova T, Fadale DJ, Xu GM, Slunt HH, Gonzales V, Savonenko AV (2005) Environmental enrichment mitigates cognitive deficits in a mouse model of Alzheimer’s disease. J Neurosci 25(21):5217–5224
Jerome KR, Chen Z, Lang R, Torres MR, Hofmeister J, Smith S, Corey L (2001) HSV and glycoprotein J inhibit caspase activation and apoptosis induced by granzyme B or Fas. J Immunol 167(7):3928–3935
Jin L, Peng W, Perng GC, Brick DJ, Nesburn AB, Jones C, Wechsler SL (2003) Identification of herpes simplex virus type 1 latency-associated transcript sequences that both inhibit apoptosis and enhance the spontaneous reactivation phenotype. J Virol 77(11):6556–6561
Kamei N, Tanaka N, Oishi Y, Hamasaki T, Nakanishi K, Sakai N, Ochi M (2007) BDNF, NT-3, and NGF released from transplanted neural progenitor cells promote corticospinal axon growth in organotypic cocultures. Spine 32(12):1272–1278
Keller JN, Pang Z, Geddes JW, Begley JG, Germeyer A, Waeg G, Mattson MP (1997) Impairment of glucose and glutamate transport and induction of mitochondrial oxidative stress and dysfunction in synaptosomes by amyloid β-peptide: role of the lipid peroxidation product 4-hydroxynonenal. J Neurochem 69(1):273–284
Kelly DP, Scarpulla RC (2004) Transcriptional regulatory circuits controlling mitochondrial biogenesis and function. Genes Dev 18(4):357–368
Knickelbein JE, Khanna KM, Yee MB, Baty CJ, Kinchington PR, Hendricks RL (2008) Noncytotoxic lytic granule–mediated CD8+ T cell inhibition of HSV-1 reactivation from neuronal latency. Science 322(5899):268–271
Knipe DM, Cliffe A (2008) Chromatin control of herpes simplex virus lytic and latent infection. Nat Rev Microbiol 6(3):211–221
Kobayashi M, Wilson AC, Chao MV, Mohr I (2012) Control of viral latency in neurons by axonal mTOR signaling and the 4E-BP translation repressor. Genes Dev 26(14):1527–1532
Korte M, Carroll P, Wolf E, Brem G, Thoenen H, Bonhoeffer T (1995) Hippocampal long-term potentiation is impaired in mice lacking brain-derived neurotrophic factor. Proc Natl Acad Sci 92(19):8856–8860
Kramer MF, Coen DM (1995) Quantification of transcripts from the ICP4 and thymidine kinase genes in mouse ganglia latently infected with herpes simplex virus. J Virol 69(3):1389–1399
Kurup P, Zhang Y, Xu J, Venkitaramani DV, Haroutunian V, Greengard P, Lombroso PJ (2010) Aβ-mediated NMDA receptor endocytosis in Alzheimer’s disease involves ubiquitination of the tyrosine phosphatase STEP61. J Neurosci 30(17):5948–5957
Kwiatkowski DL, Thompson HW, Bloom DC (2009) The polycomb group protein Bmi1 binds to the herpes simplex virus 1 latent genome and maintains repressive histone marks during latency. J Virol 83(16):8173–8181
Lacor PN, Buniel MC, Furlow PW, Clemente AS, Velasco PT, Wood M, Klein WL (2007) Aβ oligomer-induced aberrations in synapse composition, shape, and density provide a molecular basis for loss of connectivity in Alzheimer’s disease. J Neurosci 27(4):796–807
Lajoie I, Nugent S, Debacker C, Dyson K, Tancredi FB, Badhwar A, Bocti C (2017) Application of calibrated fMRI in Alzheimer's disease. NeuroImage: Clinical 15:348–358
Lakhan SE, Caro M, Hadzimichalis N (2013) NMDA receptor activity in neuropsychiatric disorders. Front Psych 4:52
LaMarco K, Thompson CC, Byers BP, Walton EM, McKnight SL (1991) Identification of Ets-and notch-related subunits in GA binding protein. Science 253(5021):789–792
LaMarco KL, McKnight SL (1989) Purification of a set of cellular polypeptides that bind to the purine-rich cis-regulatory element of herpes simplex virus immediate early genes. Genes Dev 3(9):1372–1383
Lalonde R, Kim HD, Maxwell JA, Fukuchi K (2005) Exploratory activity and spatial learning in 12-month-old APP695SWE/co+ PS1/ΔE9 mice with amyloid plaques. Neurosci Lett 390(2):87–92
La Rosa F, Agostini S, Bianchi A, Nemni R, Piancone F, Marventano I, Clerici M (2019) Herpes simplex virus-1 (HSV-1) infection induces a potent but ineffective IFN-λ production in immune cells of AD and PD patients. J Transl Med 17(1):286
La Rosa F, Saresella M, Baglio F, Piancone F, Marventano I, Calabrese E, Clerici M (2017) Immune and imaging correlates of mild cognitive impairment conversion to Alzheimer’s disease. Sci Rep 7(1):1–10
La Rosa F, Saresella M, Piancone F, Marventano I, Calabrese E, Nemni R, Clerici M (2016) P1–157: Increased TLR8 and 9 expression correlates with preserved hyppocampal volumes and lack of progression to Alzheimer’s disease in individuals with a diagnosis of mild cognitive impairment. Alzheimers Dement 12:P463–P463
Lathe R, Haas JG (2017) Distribution of cellular HSV-1 receptor expression in human brain. J Neurovirol 23(3):376–384
Lazarov O, Hollands C (2016) Hippocampal neurogenesis: learning to remember. Prog Neurobiol 138:1–18
Lee CW, Ferreon JC, Ferreon ACM, Arai M, Wright PE (2010) Graded enhancement of p53 binding to CREB-binding protein (CBP) by multisite phosphorylation. Proc Natl Acad Sci 107(45):19290–19295
Leger AJS, Hendricks RL (2011) CD8+ T cells patrol HSV-1-infected trigeminal ganglia and prevent viral reactivation. J Neurovirol 17(6):528–534
Letenneur L, Pérès K, Fleury H, Garrigue I, Barberger-Gateau P, Helmer C, Dartigues JF (2008) Seropositivity to herpes simplex virus antibodies and risk of Alzheimer’s disease: a population-based cohort study. PLoS One 3(11):e3637
Li Puma DD, Piacentini R, Leone L, Gironi K, Marcocci ME, De Chiara G, Grassi C (2019) Herpes simplex virus type-1 infection impairs adult hippocampal neurogenesis via amyloid-β protein accumulation. Stem Cells 37(11):1467–1480
Liang WS, Reiman EM, Valla J, Dunckley T, Beach TG, Grover A, Kukull W (2008) Alzheimer’s disease is associated with reduced expression of energy metabolism genes in posterior cingulate neurons. Proc Natl Acad Sci 105(11):4441–4446
Lin WR, Graham J, MacGowan SM, Wilcock GK, Itzhaki RF (1998) Alzheimer's disease, herpes virus in brain, apolipoprotein E4 and herpes labialis. Alzheimers Reports 1(3)
Liu C, Dai SK, Sun Z, Wang Z, Liu PP, Du HZ, Teng ZQ (2019) GA-binding protein GABPβ1 is required for the proliferation of neural stem/progenitor cells. Stem Cell Res 39:101501
Loopuijt LD, Schmidt WJ (1998) The role of NMDA receptors in the slow neuronal degeneration of Parkinson’s disease. Amino Acids 14(1–3):17–23
Lu J, Zuo L, Du S, Liu L (2016) The oncogenicity of Epstein-Barr virus: being more or less is to be concerned. Cancer Cell & Microenvironment 3
Manczak M, Anekonda TS, Henson E, Park BS, Quinn J, Reddy PH (2006) Mitochondria are a direct site of Aβ accumulation in Alzheimer’s disease neurons: implications for free radical generation and oxidative damage in disease progression. Hum Mol Genet 15(9):1437–1449
Manczak M, Park BS, Jung Y, Reddy PH (2004) Differential expression of oxidative phosphorylation genes in patients with Alzheimer’s disease. NeuroMol Med 5(2):147–162
Marcello E, Gardoni F, Mauceri D, Romorini S, Jeromin A, Epis R, Di Luca M (2007) Synapse-associated protein-97 mediates α-secretase ADAM10 trafficking and promotes its activity. J Neurosci 27(7):1682–1691
Mark KE, Wald A, Magaret AS, Selke S, Olin L, Huang ML, Corey L (2008) Rapidly cleared episodes of herpes simplex virus reactivation in immunocompetent adults. J Infect Dis 198(8):1141–1149
Mastroeni D, Khdour OM, Delvaux E, Nolz J, Olsen G, Berchtold N, Coleman PD (2017) Nuclear but not mitochondrial-encoded oxidative phosphorylation genes are altered in aging, mild cognitive impairment, and Alzheimer’s disease. Alzheimers Dement 13(5):510–519
Maurer I, Zierz S, Möller HJ (2000) A selective defect of cytochrome c oxidase is present in brain of Alzheimer disease patients. Neurobiol Aging 21(3):455–462
McBain CJ, Mayer ML (1994) N-methyl-D-aspartic acid receptor structure and function. Physiol Rev 74(3):723–760
McLean JH, Shipley MT, Bernstein DI, Corbett D (1993) Selective lesions of neural pathways following viral inoculation of the olfactory bulb. Exp Neurol 122(2):209–222
Melroe GT, Silva L, Schaffer PA, Knipe DM (2007) Recruitment of activated IRF-3 and CBP/p300 to herpes simplex virus ICP0 nuclear foci: potential role in blocking IFN-β induction. Virology 360(2):305–321
Miller CS, Danaher RJ, Jacob RJ (1998) Molecular aspects of herpes simplex virus I latency, reactivation, and recurrence. Crit Rev Oral Biol Med 9(4):541–562
Mishizen-Eberz AJ, Rissman RA, Carter TL, Ikonomovic MD, Wolfe BB, Armstrong DM (2004) Biochemical and molecular studies of NMDA receptor subunits NR1/2A/2B in hippocampal subregions throughout progression of Alzheimer’s disease pathology. Neurobiol Dis 15(1):80–92
Moreno-Jiménez EP, Flor-García M, Terreros-Roncal J, Rábano A, Cafini F, Pallas-Bazarra N, Llorens-Martín M (2019) Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease. Nat Med 25(4):554–560
Mori I, Nishiyama Y, Yokochi T, Kimura Y (2005) Olfactory transmission of neurotropic viruses. J Neurovirol 11(2):129–137
Murray KD, Gall CM, Jones EG, Isackson PJ (1994) Differential regulation of brain-derived neurotrophic factor and type II calcium/calmodulin-dependent protein kinase messenger RNA expression in Alzheimer’s disease. Neuroscience 60(1):37–48
Nair B, Wong-Riley MT (2016) Transcriptional regulation of brain-derived neurotrophic factor coding exon ix role of nuclear respiratory factor 2. J Biol Chem 291(43):22583–22593
Narayanan A, Nogueira ML, Ruyechan WT, Kristie TM (2005) Combinatorial transcription of herpes simplex virus and varicella zoster virus immediate early genes is strictly determined by the cellular coactivator HCF-1. J Biol Chem 280(2):1369–1375
Nguyen ML, Blaho JA (2006) Apoptosis during herpes simplex virus infection. Adv Virus Res 69:67–97
Nogueira ML, Wang VE, Tantin D, Sharp PA, Kristie TM (2004) Herpes simplex virus infections are arrested in Oct-1-deficient cells. Proc Natl Acad Sci 101(6):1473–1478
Nunomura A, Tamaoki T, Motohashi N, Nakamura M, McKeel DW Jr, Tabaton M, Zhu X (2012) The earliest stage of cognitive impairment in transition from normal aging to Alzheimer disease is marked by prominent RNA oxidation in vulnerable neurons. J Neuropathol Exp Neurol 71(3):233–241
Oka S, Leon J, Sakumi K, Ide T, Kang D, LaFerla FM, Nakabeppu Y (2016) Human mitochondrial transcriptional factor A breaks the mitochondria-mediated vicious cycle in Alzheimer’s disease. Sci Rep 6:37889
Olney JW, Tenkova T, Dikranian K, Muglia LJ, Jermakowicz WJ, D’Sa C, Roth KA (2002) Ethanol-induced caspase-3 activation in the in vivo developing mouse brain. Neurobiol Dis 9(2):205–219
Olofsdotter K, Lindvall O, Asztely F (2000) Increased synaptic inhibition in dentate gyrus of mice with reduced levels of end
Ongwijitwat S, Liang HL, Graboyes EM, Wong-Riley MT (2006) Nuclear respiratory factor 2 senses changing cellular energy demands and its silencing down-regulates cytochrome oxidase and other target gene mRNAs. Gene 374:39–49
Pandey JP, Olsson J, Weidung B, Kothera RT, Johansson A, Eriksson S, Lövheim H (2020) An Ig γ Marker Genotype Is a Strong Risk Factor for Alzheimer Disease, Independent of Apolipoprotein E ε4 Genotype. J Immunol 205(5):1318–1322
Papadimitriou C, Celikkaya H, Cosacak MI, Mashkaryan V, Bray L, Bhattarai P, Antos CL (2018) 3D culture method for Alzheimer’s disease modeling reveals interleukin-4 rescues Aβ42-induced loss of human neural stem cell plasticity. Dev Cell 46(1):85–101
Park H, Poo MM (2013) Neurotrophin regulation of neural circuit development and function. Nat Rev Neurosci 14(1):7–23
Parker WD, Parks JK (1995) Cytochrome c oxidase in Alzheimer’s disease brain: purification and characterization. Neurology 45(3):482–486
Patterson SL, Abel T, Deuel TA, Martin KC, Rose JC, Kandel ER (1996) Recombinant BDNF rescues deficits in basal synaptic transmission and hippocampal LTP in BDNF knockout mice. Neuron 16(6):1137–1145
Pedrós I, Petrov D, Allgaier M, Sureda F, Barroso E, Beas-Zarate C, Folch J (2014) Early alterations in energy metabolism in the hippocampus of APPswe/PS1dE9 mouse model of Alzheimer's disease. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease 1842(9):1556–1566
Peng W, Jin L, Henderson G, Perng GC, Brick DJ, Nesburn AB, Jones C (2004) Mapping herpes simplex virus type 1 latency-associated transcript sequences that protect from apoptosis mediated by a plasmid expressing caspase-8. J Neurovirol 10(4):260–265
Perng GC, Ghiasi H, Slanina SM, Nesburn AB, Wechsler SL (1996) The spontaneous reactivation function of the herpes simplex virus type 1 LAT gene resides completely within the first 1.5 kilobases of the 8.3-kilobase primary transcript. J Virol 70(2):976–984
Petrov D, Luque M, Pedrós I, Ettcheto M, Abad S, Pallàs M, Camins A (2016) Evaluation of the role of JNK1 in the hippocampus in an experimental model of familial Alzheimer’s disease. Mol Neurobiol 53(9):6183–6193
Pickford F, Masliah E, Britschgi M, Lucin K, Narasimhan R, Jaeger PA, Wyss-Coray T (2008) The autophagy-related protein beclin 1 shows reduced expression in early Alzheimer disease and regulates amyloid β accumulation in mice. J Clin Investig 118(6):2190–2199
Phillips HS, Hains JM, Armanini M, Laramee GR, Johnson SA, Winslow JW (1991) BDNF mRNA is decreased in the hippocampus of individuals with Alzheimer’s disease. Neuron 7(5):695–702
Polansky H (2003) Microcompetition with foreign DNA and the origin of chronic disease. Center for the Biology of Chronic.
Polansky H, Schwab H (2018a) Copy number of latent viruses, oncogenicity, and the microcompetition model. Oncotarget 9(60):31568
Polansky H, Schwab H (2018b) How a disruption of the competition between HIF-1 and p53 for limiting p300/CBP by latent viruses can cause disease. Genes Cancer 9(5–6):153
Polansky H, Schwab H (2019) How latent viruses cause breast cancer: an explanation based on the microcompetition model. Bosn J Basic Med Sci 19(3):221
Preston CM, Efstathiou S (2007) Molecular basis of HSV latency and reactivation. In: Arvin A, Campadelli-Fiume G, Mocarski E, Moore PS, Roizman B, Whitley R, Yamanishi K, editors. Human herpesviruses: biology, therapy, and immunoprophylaxis. United Kingdom: Cambridge University Press Chapter 33
Priya A, Johar K, Wong-Riley MT (2013) Nuclear respiratory factor 2 regulates the expression of the same NMDA receptor subunit genes as NRF-1: both factors act by a concurrent and parallel mechanism to couple energy metabolism and synaptic transmission. Biochimica et Biophysica Acta (BBA)-Molecular Cell Research 1833(1):48–58
Polansky H, Javaherian A (2015a) Microcompetition with latent Epstein-Barr virus causes a transcription factor deficiency, under-expression of retinoblastoma, and classic Hodgkin lymphoma. Int J Res Med Sci 3(6):1562
Polansky H, Javaherian A (2015b) Latent viruses, microcompetition, transcription factor deficiency and the cause of acute lymphoblastic leukemia. J Adv Med 541–543
Piacentini R, Civitelli L, Ripoli C, Marcocci ME, De Chiara G, Garaci E, Grassi C (2011) HSV-1 promotes Ca2+-mediated APP phosphorylation and Aβ accumulation in rat cortical neurons. Neurobiol Aging 32(12):2323-e13
Piacentini R, Puma DDL, Ripoli C, Marcocci ME, De Chiara G, Garaci E, Grassi C (2015) Herpes Simplex Virus type-1 infection induces synaptic dysfunction in cultured cortical neurons via GSK-3 activation and intraneuronal amyloid-β protein accumulation. Sci Rep 5(1):1–14
Rice AC, Keeney PM, Algarzae NK, Ladd AC, Thomas RR, Bennett JP Jr (2014) Mitochondrial DNA copy numbers in pyramidal neurons are decreased and mitochondrial biogenesis transcriptome signaling is disrupted in Alzheimer’s disease hippocampi. J Alzheimers Dis 40(2):319–330
Richards BA, Frankland PW (2017) The persistence and transience of memory. Neuron 94(6):1071–1084
Røge R, Møller BK, Andersen CR, Correll CU, Nielsen J (2012) Immunomodulatory effects of clozapine and their clinical implications: what have we learned so far?. Schizophr Res 140(1–3):204–213
Rosmarin AG, Resendes KK, Yang Z, McMillan JN, Fleming SL (2004) GA-binding protein transcription factor: a review of GABP as an integrator of intracellular signaling and protein–protein interactions. Blood Cells Mol Dis 32(1):143–154
Salminen A, Kaarniranta K, Kauppinen A, Ojala J, Haapasalo A, Soininen H, Hiltunen M (2013) Impaired autophagy and APP processing in Alzheimer’s disease: the potential role of Beclin 1 interactome. Prog Neurobiol 106:33–54
Sawtell NM (1997) Comprehensive quantification of herpes simplex virus latency at the single-cell level. J Virol 71(7):5423–5431
Sawtell NM, Poon DK, Tansky CS, Thompson RL (1998) The latent herpes simplex virus type 1 genome copy number in individual neurons is virus strain specific and correlates with reactivation. J Virol 72(7):5343–5350
Sharrocks AD (2001) The ETS-domain transcription factor family. Nat Rev Mol Cell Biol 2(11):827–837
Shen JH, Huang KYA, Chao-Yu C, Chen CJ, Lin TY, Huang YC (2015) Seroprevalence of herpes simplex virus type 1 and 2 in Taiwan and risk factor analysis, 2007. PLoS One 10(8):e0134178
Sheng B, Wang X, Su B, Lee HG, Casadesus G, Perry G, Zhu X (2012) Impaired mitochondrial biogenesis contributes to mitochondrial dysfunction in Alzheimer’s disease. J Neurochem 120(3):419–429
Shieh PB, Hu SC, Bobb K, Timmusk T, Ghosh A (1998) Identification of a signaling pathway involved in calcium regulation of BDNF expression. Neuron 20(4):727–740
Singh N, Tscharke DC (2020) Herpes simplex virus latency is noisier the closer we look. J Virol 94(4)
Snyder EM, Nong Y, Almeida CG, Paul S, Moran T, Choi EY, Greengard P (2005) Regulation of NMDA receptor trafficking by amyloid-β. Nat Neurosci 8(8):1051–1058
Sörensen A, Blazhenets G, Rücker G, Schiller F, Meyer PT, Frings L, Alzheimer's Disease Neuroimaging Initiative (2019) Prognosis of conversion of mild cognitive impairment to Alzheimer's dementia by voxel-wise Cox regression based on FDG PET data. NeuroImage: Clinical 21:101637
Suzuki WA, Zola-Morgan S, Squire LR, Amaral DG (1993) Lesions of the perirhinal and parahippocampal cortices in the monkey produce long-lasting memory impairment in the visual and tactual modalities. J Neurosci 13(6):2430–2451
Swaminathan G, Zhu W, Plowey ED (2016) BECN1/Beclin 1 sorts cell-surface APP/amyloid β precursor protein for lysosomal degradation. Autophagy 12(12):2404–2419
Sze CI, Bi H, Kleinschmidt-DeMasters BK, Filley CM, Martin LJ (2001) N-Methyl-D-aspartate receptor subunit proteins and their phosphorylation status are altered selectively in Alzheimer’s disease. J Neurol Sci 182(2):151–159
Tang YP, Shimizu E, Dube GR, Rampon C, Kerchner GA, Zhuo M, Tsien JZ (1999) Genetic enhancement of learning and memory in mice. Nature 401(6748):63–69
Taus NS, Mitchell WJ (2001) The transgenic ICP4 promoter is activated in Schwann cells in trigeminal ganglia of mice latently infected with herpes simplex virus type 1. J Virol 75(21):10401–10408
Thompson RL, Sawtell NM (1997) The herpes simplex virus type 1 latency-associated transcript gene regulates the establishment of latency. J Virol 71(7):5432–5440
Tobin MK, Musaraca K, Disouky A, Shetti A, Bheri A, Honer WG, Lazarov O (2019) Human hippocampal neurogenesis persists in aged adults and Alzheimer’s disease patients. Cell Stem Cell 24(6):974–982
Tohgi H, Yonezawa H, Takahashi S, Sato N, Kato E, Kudo M, Sasaki T (1998) Cerebral blood flow and oxygen metabolism in senile dementia of Alzheimer’s type and vascular dementia with deep white matter changes. Neuroradiology 40(3):131–137
Tong L, Thornton PL, Balazs R, Cotman CW (2001) β-amyloid-(1–42) impairs activity-dependent cAMP-response element-binding protein signaling in neurons at concentrations in which cell survival is not compromised. J Biol Chem 276(20):17301–17306
Triezenberg SJ, LaMarco KL, McKnight SL (1988) Evidence of DNA: protein interactions that mediate HSV-1 immediate early gene activation by VP16. Genes Dev 2(6):730–742
Tzeng NS, Chung CH, Lin FH, Chiang CP, Yeh CB, Huang SY, Chiang WS (2018) Anti-herpetic medications and reduced risk of dementia in patients with herpes simplex virus infections—a nationwide, population-based cohort study in Taiwan. Neurotherapeutics 15(2):417–429
Ueda A, Akagi T, Yokota T (2017) GA-binding protein alpha is involved in the survival of mouse embryonic stem cells. Stem Cells 35(11):2229–2238
Ułas J, Cotman CW (1997) Decreased expression of N-methyl-D-aspartate receptor 1 messenger RNA in select regions of Alzheimer brain. Neuroscience 79(4):973–982
Venkitaramani DV, Moura PJ, Picciotto MR, Lombroso PJ (2011) Striatal-enriched protein tyrosine phosphatase (STEP) knockout mice have enhanced hippocampal memory. Eur J Neurosci 33(12):2288–2298
Verges DK, Restivo JL, Goebel WD, Holtzman DM, Cirrito JR (2011) Opposing synaptic regulation of amyloid-β metabolism by NMDA receptors in vivo. J Neurosci 31(31):11328–11337
Vitlic A, Lord JM, Phillips AC (2014) Stress, ageing and their influence on functional, cellular and molecular aspects of the immune system. Age 36(3):9631
Vogel JL, Kristie TM (2000) The novel coactivator C1 (HCF) coordinates multiprotein enhancer formation and mediates transcription activation by GABP. EMBO J 19(4):683–690
Wang R, Dineley KT, Sweatt JD, Zheng H (2004) Presenilin 1 familial Alzheimer’s disease mutation leads to defective associative learning and impaired adult neurogenesis. Neuroscience 126(2):305–312
Wang T, Lao U, Edgar BA (2009) TOR-mediated autophagy regulates cell death in Drosophila neurodegenerative disease. J Cell Biol 186(5):703–711
Wang W, Zhao F, Ma X, Perry G, Zhu X (2020) Mitochondria dysfunction in the pathogenesis of Alzheimer’s disease: recent advances. Mol Neurodegener 15:1–22
Wiedemann N, Pfanner N (2017) Mitochondrial machineries for protein import and assembly. Annu Rev Biochem 86:685–714
World Health Organization (2018) Herpes simplex virus. http://www.who.int/en/news-room/fact-sheets/detail/herpes-simplex-virus. Published 2018. Accessed 27 Aug 2018
Wozniak MA, Mee AP, Itzhaki RF (2009) Herpes simplex virus type 1 DNA is located within Alzheimer’s disease amyloid plaques. The Journal of Pathology: A Journal of the Pathological Society of Great Britain and Ireland 217(1):131–138
Xu S, Zhong M, Zhang L, Wang Y, Zhou Z, Hao Y, Yu Z (2009) Overexpression of Tfam protects mitochondria against β-amyloid-induced oxidative damage in SH-SY5Y cells. FEBS J 276(14):3800–3809
Yang L, Voytek CC, Margolis TP (2000) Immunohistochemical analysis of primary sensory neurons latently infected with herpes simplex virus type 1. J Virol 74(1):209–217
Yang ZF, Drumea K, Mott S, Wang J, Rosmarin AG (2014) GABP transcription factor (nuclear respiratory factor 2) is required for mitochondrial biogenesis. Mol Cell Biol 34(17):3194–3201
You Y, Cheng AC, Wang MS, Jia RY, Sun KF, Yang Q, Zhao XX (2017) The suppression of apoptosis by α-herpesvirus. Cell Death Dis 8(4):e2749–e2749
Young-Collier KJ, McArdle M, Bennett JP (2012) The dying of the light: mitochondrial failure in Alzheimer’s disease. J Alzheimers Dis 28(4):771–781
Yu S, Cui K, Jothi R, Zhao DM, Jing X, Zhao K, Xue HH (2011) GABP controls a critical transcription regulatory module that is essential for maintenance and differentiation of hematopoietic stem/progenitor cells. Blood, The Journal of the American Society of Hematology 117(7):2166–2178
Zhang Y, Kurup P, Xu J, Carty N, Fernandez SM, Nygaard HB, Lombroso PJ (2010) Genetic reduction of striatal-enriched tyrosine phosphatase (STEP) reverses cognitive and cellular deficits in an Alzheimer’s disease mouse model. Proc Natl Acad Sci 107(44):19014–19019
Zhao C, Deng W, Gage FH (2008) Mechanisms and functional implications of adult neurogenesis. Cell 132(4):645–660
Zheng F, Zhou X, Moon C, Wang H (2012) Regulation of brain-derived neurotrophic factor expression in neurons. International Journal of Physiology, Pathophysiology and Pharmacology 4(4):188
Zhou CH, Zhang XP, Liu F, Wang W (2015) Modeling the interplay between the HIF-1 and p53 pathways in hypoxia. Sci Rep 5:13834
Zhu W, Swaminathan G, Plowey ED (2014) GA binding protein augments autophagy via transcriptional activation of BECN1-PIK3C3 complex genes. Autophagy 10(9):1622–1636
Zuo L, Yu H, Liu L, Tang Y, Wu H, Yang J, Li G (2015) The copy number of Epstein-Barr virus latent genome correlates with the oncogenicity by the activation level of LMP1 and NF-κB. Oncotarget 6(38):41033
Author information
Authors and Affiliations
Contributions
Hanan Polansky initiated and supervised the research. Benjamin Goral collected and summarized the literature.
The study includes no participants. All authors express consent for publication. There is no additional data and material.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Polansky, H., Goral, B. How an increase in the copy number of HSV-1 during latency can cause Alzheimer’s disease: the viral and cellular dynamics according to the microcompetition model. J. Neurovirol. 27, 895–916 (2021). https://doi.org/10.1007/s13365-021-01012-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-021-01012-9