Abstract
Sensory peripheral neuropathy (PN) remains a common complication in HIV-positive patients despite effective combination anti-retroviral therapy (ART). Data on PN on second-line ART is scarce. We assessed PN using a standard tool in patients failing first-line ART and for 96 weeks following a switch to PI-based second-line ART in a large Randomised Clinical Trial in Sub-Saharan Africa. Factors associated with PN were investigated using logistic regression. Symptomatic PN (SPN) prevalence was 22 % at entry (N = 1,251) and was associated (p < 0.05) with older age (OR = 1.04 per year), female gender (OR = 1.64), Tuberculosis (TB; OR = 1.86), smoking (OR = 1.60), higher plasma creatinine (OR = 1.09 per 0.1 mg/dl increase), CD4 count (OR = 0.83 per doubling) and not consuming alcohol (OR = 0.55). SPN prevalence decreased to 17 % by week 96 (p = 0.0002) following similar trends in all study groups (p = 0.30). Asymptomatic PN (APN) increased over the same period from 21 to 29 % (p = 0.0002). Signs suggestive of PN (regardless of symptoms) returned to baseline levels by week 96. At weeks 48 and 96, after adjusting for time-updated associations above and baseline CD4 count and viral load, SPN was strongly associated with TB (p < 0.0001). In summary, SPN prevalence was significantly reduced with PI-based second-line therapy across all treatment groups, but we did not find any advantage to the NRTI-free regimens. The increase of APN and stability of PN-signs regardless of symptoms suggest an underlying trend of neuropathy progression that may be masked by reduction of symptoms accompanying general health improvement induced by second-line ART. SPN was strongly associated with isoniazid given for TB treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sensory peripheral neuropathy (PN) remains one of the most common complications in HIV-positive patients despite the use of effective combination anti-retroviral therapy (cART) (Ellis et al. 2010; Kamerman et al. 2012). Prevalence of symptomatic PN in HIV-positive individuals has been reported to range between 20 and 60 % in cross-sectional studies and has been associated with several factors. PN is a complication of HIV disease progression in ART-naïve patients but can also be aggravated by ART-induced immune restoration, where greater CD4 cell count recovery has been associated with an increased risk of developing PN (Childs et al. 1999; Ellis et al. 2010; Maritz et al. 2010). However, more often it has been reported as adverse reaction to dideoxynucleosides or “d-drugs”, particularly stavudine (d4T) and didanosine (ddI) (van Oosterhout et al. 2012; Wadley et al. 2011; Wright et al. 2008) which until relatively recently were frequently used in Sub-Saharan African countries. Other drugs frequently used in HIV-positive individuals such as isoniazid can also cause similar neuropathic symptoms(van der Watt et al. 2011). Clinical presentation of HIV-induced and toxicity-associated PN are often indistinguishable and regardless of its cause PN has a significant negative impact on the quality of life of HIV-positive adults (Biraguma and Rhoda 2012; Ellis et al. 2010).
In ART-naïve patients, signs of PN appear to persist after initiation of effective cART and increase over-time (Evans et al. 2012; Evans et al. 2011). Incidence of new PN while on first-line cART has been estimated to range between 12 to 21 cases per 100 person-years but association between “d-drug” exposure and persistent or incident PN during first-line therapy has been inconsistently reported(S. R. Evans et al. 2011; Mehta et al. 2011; Nakamoto et al. 2010). In ART-experienced patients PN appears to remain a major problem despite effective virological control (Chen et al. 2013). Little is known about prevalence of and risk factors for PN in ART-experienced patients failing first-line ART or how PN changes on protease inhibitor (PI)-based second-line ART in resource-limited settings. We therefore conducted an analysis to investigate this in a large clinical trial in sub-Saharan Africa.
Methods
Participants and setting
The EARNEST trial was a large, open-label, randomised clinical trial (ISRCTN-37737787), performed in 14 centres in sub-Saharan Africa where HIV-positive adult and adolescent patients with virological, immunological or clinical first-line cART failure were randomised to lopinavir/ritonavir 400 mg/100 mg twice daily with either (1) two to three new or recycled NRTIs chosen by the treating physician (“PI/NRTI”); (2) raltegravir 400 mg twice daily (“PI/RAL”); or (3) raltegravir induction for the first 12 weeks only (“PImono”). The main analysis of the trial has been reported elsewhere(Paton et al. 2014). In summary, the PI/NRTI arm and PI/RAL arm were indistinguishable on the primary composite endpoint (clinical, immunological and virological components) and produced identical rates of VL suppression at 96 weeks (86 % <400 copies/ml). The PI-mono arm was similar to PI/NRTI on clinical and CD4 components of the composite endpoint, but VL suppression was substantially worse (61 % <400 copies at 96 weeks). The study (which included neuropathy assessments as part of the main protocol in all patients) was approved by all relevant ethics committees and regulatory agencies in participating countries and in the UK. All participants or caregivers provided written informed consent.
Participants were assessed for PN using the AIDS Clinical Trials Group (ACTG) Brief Peripheral Neuropathy Screen tool (BPNS) (Cettomai et al. 2010; Marra et al. 1998) at baseline, week 48 and week 96. Symptomatic PN (SPN) was defined as presence of bilateral neuropathic symptoms (at least one of pain, aching or burning, pins and needles, or numbness) and abnormal signs (either reduced or absent ankle reflex or reduced vibration sense at the great toe (vibration of a 128-Hz tuning fork felt for 10 seconds or less)) (Ellis et al. 2005; S. R. Evans et al. 2011). Asymptomatic PN (APN) was defined as reduced or absent ankle reflex or reduced vibration sense at the great toe without symptoms. Site investigators were trained on the BPNS tool at site initiation visits.
In addition, medical assessment at these study visits included symptom review, physical examination, full blood count, serum creatinine levels and CD4 counts. HIV-RNA was measured centrally (Joint Clinical Research Centre, Kampala, Uganda) on stored plasma samples.
Statistical analysis
All statistical tests presented are two-sided. All analyses were carried out in Stata version 13.1. Association between PN and patient characteristics at switch to second-line, including demographics, study site, anthropometric measures, CD4 cell count, HIV-RNA level, WHO HIV disease stage, ART exposure, co-morbidities (such as TB, diabetes mellitus and cardiovascular disease(CVD)), concomitant medication in the last 10 weeks, alcohol consumption, smoking status and socio-economic variables including household income and employment status were modelled using complete case univariable logistic regression with fractional polynomials to allow for non-linear relationships between continuous factors and PN. Years on first-line ART and creatinine were censored at approximate 99th percentiles to reduce the impact of outliers. Centre effects were estimated pooling sites with similar overall prevalence (Table 1) to prevent perfect prediction in low prevalence sites. Primary analyses excluded 19 participants from the smallest centre that reported very high and potentially implausible rates of PN on symptom report (12/19 63 %) and abnormal signs (17/17 with completed PN signs, 100 %).
Factors associated with PN status univariably with p < 0.2 were included in a multivariable logistic regression. Backward selection (exit criteria p > 0.1) was used to select independent risk factors using fractional polynomials to allow for non-linear relationships (Stata mfpmi command). Multiple imputation using chained estimating equations (Stata ice command) was used to impute a small amount of missing data in risk factors and components of PN (if at least one component was complete) (van Buuren et al. 1999).
Sensitivity analyses were performed (1) on complete cases, (2) using multiple imputation including the site excluded from the primary analysis, and (3) abnormal signs (regardless of the presence of symptoms), (4) symptoms (regardless of the presence of abnormal signs) and (5) bilateral symptoms plus either reduced vibration sense or absent ankle reflex. A repeated measures model (generalized estimating equations, independent correlation structure, binomial distribution) looked at the effect of time updated factors selected in the baseline model as well as baseline CD4 and viral load on PN at weeks 48 and 96 in complete cases.
Prevalence of SPN, APN, abnormal signs (regardless of the presence of symptoms) and symptoms (regardless of the presence of abnormal signs) were calculated at baseline, weeks 48 and 96 by study treatment arm in those with complete PN assessment and was compared between the arms at each time point using risk differences and chi squared tests. Generalised estimating equations (independent correlation structure, binomial distribution) were used to test for a difference between the arms across all time points.
Results
Of the 1,277 patients randomised in the EARNEST trial, 19 were from the excluded site, 1 had completely absent baseline PN assessment and 1 was an amputee so could not be assessed leaving 1,256 (98 %) eligible patients. 1251 had a complete PN assessment at baseline. Of these, 726 (58 %) were female and the median age at switch to second-line was 37 years (inter-quartile range (IQR) 31–44). At second-line switch, patients had been on first-line cART for a median of 4 years (IQR 2.8–5.4); most had been exposed to zidovudine (AZT; 68 %) or d4T (60 %) during first-line, with fewer already exposed to tenofovir disoproxil fumarate (TDF; 14 %). At switch, median CD4 count was 71 cell/mm3 (IQR 30–147), median plasma HIV viral load (VL) was 67,500 copies/ml (IQR 22,818–193,000) and 80 % of participants with medical history available had been reported to have at least one WHO stage 3/4 condition (Table 1). In EARNEST 420 participants were randomised to PI/NRTI (TDF in 79 %, abacavir (ABC) in 16 %, ddI in 13 %, d4T in <1 %, lamivudine/emtricitabine (3TC/FTC) in 87 %), 422 to PI/RAL and 409 PImono second-line ART.
PN at first-line failure
At switch, 279 of the 1,251 (22 %) patients with a complete PN assessment met the study definition for SPN and the prevalence of APN was similar at 21 %. Overall, 44 % of patients had abnormal signs at examination. SPN prevalence differed significantly between study sites ranging from 0 to 44 % (p < 0.0001). However, prevalence of SPN in the three Kampala sites was remarkably similar (25–28 %) whereas the other six Ugandan sites, located elsewhere in the country, showed also similar but much lower prevalence (0–9 %).
The characteristics of the patients at first-line failure and the univariable associations with SPN are shown in Table 1. In the multivariable model, independent associations were found with age, female gender, history of TB and higher levels of plasma creatinine. The odds of having PN at first-line failure were lower with higher CD4 counts and alcohol consumption, whereas smokers were more likely to have SPN at entry (Table 2). Weak evidence (0.05 < p < 0.1) of associations with increasing risk of SPN were found with viral load, increasing glucose, family history of CVD, TDF or nevirapine (NVP) during first line and employment status.
An exploratory analysis considered additional impact on SPN of exposure to d4T and time on d4T. After adjusting for the factors above, d4T at any time on first-line (ignoring duration) was not independently associated with SPN (p = 0.44), however adjusting for duration of exposure suggested SPN risk was higher in those with a short exposure, with the risk decreasing with increasing time on d4T (p = 0.007; electronic supplementary material, (ESM) Table 3). When isoniazid use in the last 10 weeks was included in the model as well as TB these were not independently associated with SPN, and TB was the better predictor of SPN. When substituting TB with isoniazid, the effect of isoniazid was comparable to TB (Supplementary Material Table 4).
Sensitivity analyses that included complete cases, the excluded site, bilateral symptoms and reduced vibration sense or absent ankle reflex, and presence of symptoms gave results similar to those above. There was no evidence of an association between abnormal signs (regardless of symptoms) and sex, TDF exposure or alcohol. Effects were attenuated compared to the SPN model for VL, CD4, NVP exposure, smoking, family history of CVD and glucose. The effect of age, TB, creatinine and employment status remained unchanged and additional associations were identified with d4T (OR = 1.44; 95 % CI 1.02–2.05; p = 0.04), and height (OR = 1.03; 95 % CI 1.01–1.05; p = 0.001). (ESM Table 5).
PN on second-line therapy
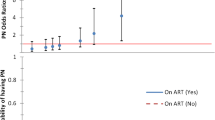
Overall, 135 out of 1,176 (11 %) patients assessed at week 48 had SPN (p < 0.0001 vs baseline) whereas the prevalence at week 96 was 17 % (p < 0.0001 vs week 48, p = 0.0002 vs baseline; Fig. 1a). In contrast, the prevalence of APN showed a steady increase over time (21, 24 and 29 % at weeks 0, 48, 96, respectively; trend p = 0.0002; Fig. 1b). Abnormal signs suggestive of PN had a smaller decline in prevalence at week 48 than SPN (44 and 36 % at weeks 0 and 48, respectively) but returned to baseline levels by week 96 (46 %; Fig. 1c).
As expected, the prevalence of SPN was similar between study groups at entry (23, 23 and 22 % in PI/NRTI, PI/RAL and PImono, respectively). There was no difference in SPN prevalence between randomisation arms at week 96 (global p = 0.11; Table 3). Overall, there was no evidence for differences between study group in the trends over time of any PN outcome measure (p > 0.1, Fig. 1). At weeks 48 and 96 there was no effect of baseline or current VL, current CD4, smoking, alcohol consumption or creatinine. The effect of family history of CVD, glucose at failure, sex, NVP and TDF exposure was attenuated, and baseline CD4, age, TB and job status remained unchanged (Supplementary Table 10). Similarly to baseline, isoniazid and TB were not independently associated with PN and isoniazid remained strongly associated with SPN (p < 0.0001) after adjusting for the factors above.
Considering the 1,132 participants with PN status assessed at all time-points, the rate of incident SPN was 4 % (38/882 patients with no SPN at baseline) by week 48 and 9 % (75/844 patients without SPN at week 48) by week 96 (Fig. 2). Resolution of SPN was observed in 64 % (159/250) of patients with SPN at baseline by week 48 and 31 % (28/91) of patients with persistent SPN at week 48 by week 96. Overall, 58 % (145/250) of the participants with SPN at first-line failure had SPN resolution at week 96. Isoniazid-based TB treatment was prescribed during study period to 18 % of patients who developed incident SPN, but only to 6 % of those patients who never developed SPN (p < 0.001). However, we found no evidence of pyridoxine reducing the chance of developing SPN since 7/18 (39 %) of those given pyridoxine and 13/48 (27 %) not given it developed SPN (p = 0.35).
Discussion
In this large, well-characterised cohort of patients taking part in a randomised controlled trial on PI-based second-line ART that were systematically assessed using a well-validated and objective tool, we observed a prevalence of SPN of 22 % at second-line switch, similar to levels reported in ART-experienced patients in Sub-Saharan Africa (21 %) (Luma et al. 2012; van Oosterhout et al. 2012) but lower than the prevalence reported at virological failure in the ALLRT study in the USA (33.7 %) (Chen et al. 2013). ALLRT study participants were assessed using the same tool but were slightly older and had been exposed to ART for longer than those recruited in EARNEST (median (IQR) age at entry 43 (37–48) and 37 (31–44) years and median (IQR) exposure to ART prior entry 6.0 (3.0, 9.3) and 4.0 (2.8–5.4) years, respectively) which at least partially explains the differences in SPN prevalence given the consistent associations between these factors and increased risk of SPN(Cherry et al. 2009; Ellis et al. 2010; Evans et al. 2011).
We found low CD4 count, but not HIV-VL associated with SPN suggesting that immuno-suppression or the incident opportunistic conditions associated with it, and the drugs required for the treatment of these conditions is a key predictor(Ellis et al. 2010; Luma et al. 2012). In particular, we found that history of TB was independently associated with SPN at the time of first-line failure probably reflecting associations between SPN and exposure to anti-TB treatment (Luma et al. 2012; Maritz et al. 2010; van der Watt et al. 2011). Neuropathy is a well-known adverse effect attributable to isoniazid, although rare when used as preventive therapy (Grant et al. 2010). Pyridoxine co-administration effectively reduces the risk of developing isoniazid-induced PN but it is inconsistently prescribed as part of TB treatment in Sub-Saharan Africa (Grant et al. 2010; van der Watt et al. 2011). In EARNEST, only 26 % of patients were prescribed pyridoxine when treated for incident TB. The risk of developing drug-induced PN is independently and significantly higher in patients simultaneously exposed to isoniazid and d-drugs(Breen et al. 2006; Dean et al. 2002), but appears to peak after the first few months of exposure to these antiretrovirals, and decline thereafter(Arenas-Pinto et al. 2008; Dean et al. 2002; Westreich et al. 2009). In our study, adding d4T and duration of exposure to d4T to our final multivariable model similarly found that the risk of presenting SPN decreased with duration of exposure to d4T in first-line, possibly due to only those not affected by SPN remaining on this NRTI for long periods of time (i.e. channelling bias) or due to special susceptibility, probably genetically mediated, to toxic effects induced by d-drugs (Arenas-Pinto et al. 2008; Kampira et al. 2013).
Our data do not support associations previously reported between PN and alcohol consumption or anthropometric measures(Cherry et al. 2009; Grant et al. 2010; Luma et al. 2012). In our cohort, only 10 % of participants reported drinking alcohol ever and patients with SPN reported it less often than patients without neuropathy (7 vs. 12 %; p = 0.02). This apparently protective effect of alcohol has been previously described in observational studies(Pettersen et al. 2006) and in vitro data suggest that cerebral neurons pre-treated with ethanol were resistant to the neurodegenerative effect of HIV protein gp120 (Collins et al. 2000). Alternatively, although the effect of alcohol is adjusted for job status, it may be possible that alcohol consumption was associated with other socio-economic variables we did not measure.
After starting second-line therapy, we observed a significant reduction in the prevalence of SPN by week 96. However, the prevalence of signs suggestive of PN regardless of symptoms showed a smaller (though still significant) decline in response to second-line treatment whereas APN actually increased progressively during follow up consistent with previous observations (Ellis et al. 2010; Evans et al. 2011). There is likely a complex interplay of factors explaining these changes in second-line therapy. Firstly, re-establishing VL control, treatment of opportunistic infections and general recovery of health might contribute to the initial reduction in symptoms. This decrease in SPN prevalence may perhaps be augmented by the confusion of non-neuropathy symptoms with neuropathy symptoms due to discrepancies between terms used to describe neuropathic pain in local African languages and English (Shaikh et al. 2013). The cessation of d4T used in first-line may also have contributed to some of the symptomatic improvement (Evans et al. 2011) although we did not find any advantage to NRTI-free regimens tested in EARNEST (PI/RAL or PImono). Most patients in the PI/NRTI group were treated with TDF, which is unlikely to cause PN, but some (14 %) were exposed to ddI in this group.
Symptom decrease with recovery of health on second line may be masking an underlying trend of neuropathy progression. One additional possibility to consider is that the PI contributed to some of the neuropathy progression in second line (Chen et al. 2013; Pettersen et al. 2006). Although the exact mechanism for the association between PI and PN is not known (Ellis et al. 2008; Lichtenstein et al. 2005), in vitro data suggest that exposure to indinavir can induce neuronal degeneration in dorsal root ganglion cultures(Pettersen et al. 2006). Furthermore, PI exposure has been associated with insulin resistance and development of diabetes mellitus (DM) (Paik and Kotler 2011) which may also lead to PN in both general and HIV-infected populations. However, we did not see any association between PN and DM.
Limitations of this study include the limited information available on past medical history and the use of non-ART medication prior to study entry (only medications in the last 10 weeks were collected). Clinical assessments in our study were performed by non-neurologists but medically qualified investigators using a rigorous case definition based on a tool previously validated in African settings (Luma et al. 2012; Maritz et al. 2010; Wadley et al. 2011). There were large differences between the sites in prevalence (after adjusting for other associations) that might suggest the possibility of systematic differences in the way the tests were applied. However, the fact that the prevalence of neuropathy in the three sites in Kampala was remarkably similar (25–28 %) whereas the other six Ugandan sites, located elsewhere in the country and with differing ethnic groups, also showed similar but much lower prevalence (0–9 %) provides some support for the belief that these differences reflect true population differences rather than erratic application of the tool.
In conclusion, our study provides evidence of high prevalence of SPN in HIV-positive patients from Sub-Saharan African countries at the time of first-line failure and during PI-based second-line therapy. In addition to well-recognised risk factors such as age, female gender and low CD4 count, SPN appeared to be strongly associated with toxic effects of isoniazid used to treat TB episodes, highlighting the importance of ensuring that pyridoxine is prescribed with TB treatment. The potential contribution to PIs to maintaining the high rate of neuropathy during second-line therapy and management strategies to treat neuropathy deserves further investigation.
References
Arenas-Pinto A, Bhaskaran K, Dunn D, Weller IV (2008) The risk of developing peripheral neuropathy induced by nucleoside reverse transcriptase inhibitors decreases over time: evidence from the Delta trial. Antivir Ther 13(2):289–295
Biraguma J, Rhoda A (2012) Peripheral neuropathy and quality of life of adults living with HIV/AIDS in the Rulindo district of Rwanda. SAHARA J 9(2):88–94
Breen RA, Miller RF, Gorsuch T, Smith CJ, Schwenk A, Holmes W et al (2006) Adverse events and treatment interruption in tuberculosis patients with and without HIV co-infection. Thorax 61(9):791–794
Cettomai D, Kwasa J, Kendi C, Birbeck GL, Price RW, Bukusi EA et al (2010) Utility of quantitative sensory testing and screening tools in identifying HIV-associated peripheral neuropathy in Western Kenya: pilot testing. PLoS One 5(12):e14256
Chen H, Clifford DB, Deng L, Wu K, Lee AJ, Bosch RJ et al (2013) Peripheral neuropathy in ART-experienced patients: prevalence and risk factors. J Neurovirol 19(6):557–564
Cherry CL, Affandi JS, Imran D, Yunihastuti E, Smyth K, Vanar S et al (2009) Age and height predict neuropathy risk in patients with HIV prescribed stavudine. Neurology 73(4):315–320
Childs EA, Lyles RH, Selnes OA, Chen B, Miller EN, Cohen BA et al (1999) Plasma viral load and CD4 lymphocytes predict HIV-associated dementia and sensory neuropathy. Neurology 52(3):607–613
Collins MA, Neafsey EJ, Zou JY (2000) HIV-I gpI20 neurotoxicity in brain cultures is prevented by moderate ethanol pretreatment. Neuroreport 11(6):1219–1222
Dean GL, Edwards SG, Ives NJ, Matthews G, Fox EF, Navaratne L et al (2002) Treatment of tuberculosis in HIV-infected persons in the era of highly active antiretroviral therapy. AIDS 16(1):75–83
Ellis RJ, Evans SR, Clifford DB, Moo LR, McArthur JC, Collier AC et al (2005) Clinical validation of the NeuroScreen. J Neurovirol 11(6):503–511
Ellis RJ, Marquie-Beck J, Delaney P, Alexander T, Clifford DB, McArthur JC et al (2008) Human immunodeficiency virus protease inhibitors and risk for peripheral neuropathy. Ann Neurol 64(5):566–572
Ellis RJ, Rosario D, Clifford DB, McArthur JC, Simpson D, Alexander T et al (2010) Continued high prevalence and adverse clinical impact of human immunodeficiency virus-associated sensory neuropathy in the era of combination antiretroviral therapy: the CHARTER Study. Arch Neurol 67(5):552–558
Evans SR, Ellis RJ, Chen H, Yeh TM, Lee AJ, Schifitto G et al (2011) Peripheral neuropathy in HIV: prevalence and risk factors. AIDS 25(7):919–928
Evans D, Takuva S, Rassool M, Firnhaber C, Maskew M (2012) Prevalence of peripheral neuropathy in antiretroviral therapy naive HIV-positive patients and the impact on treatment outcomes—a retrospective study from a large urban cohort in Johannesburg, South Africa. J Neurovirol 18(3):162–171
Grant AD, Mngadi KT, van Halsema CL, Luttig MM, Fielding KL, Churchyard GJ (2010) Adverse events with isoniazid preventive therapy: experience from a large trial. AIDS 24(Suppl 5):S29–36
Kamerman PR, Wadley AL, Cherry CL (2012) HIV-associated sensory neuropathy: risk factors and genetics. Curr Pain Headache Rep 16(3):226–236
Kampira E, Kumwenda J, van Oosterhout JJ, Dandara C (2013) Mitochondrial DNA subhaplogroups L0a2 and L2a modify susceptibility to peripheral neuropathy in malawian adults on stavudine containing highly active antiretroviral therapy. J Acquir Immune Defic Syndr 63(5):647–652
Lichtenstein KA, Armon C, Baron A, Moorman AC, Wood KC, Holmberg SD (2005) Modification of the incidence of drug-associated symmetrical peripheral neuropathy by host and disease factors in the HIV outpatient study cohort. Clin Infect Dis 40(1):148–157
Luma HN, Tchaleu BC, Doualla MS, Temfack E, Sopouassi VN, Mapoure YN et al (2012) HIV-associated sensory neuropathy in HIV-1 infected patients at the Douala General Hospital in Cameroon: a cross-sectional study. AIDS Res Ther 9(1):35
Maritz J, Benatar M, Dave JA, Harrison TB, Badri M, Levitt NS et al (2010) HIV neuropathy in South Africans: frequency, characteristics, and risk factors. Muscle Nerve 41(5):599–606
Marra CM, Boutin P, Collier AC (1998) Screening for distal sensory peripheral neuropathy in HIV-infected persons in research and clinical settings. Neurology 51(6):1678–1681
Mehta SA, Ahmed A, Laverty M, Holzman RS, Valentine F, Sivapalasingam S (2011) Sex differences in the incidence of peripheral neuropathy among Kenyans initiating antiretroviral therapy. Clin Infect Dis 53(5):490–496
Nakamoto BK, McMurtray A, Davis J, Valcour V, Watters MR, Shiramizu B et al (2010) Incident neuropathy in HIV-infected patients on HAART. AIDS Res Hum Retrovir 26(7):759–765
Paik IJ, Kotler DP (2011) The prevalence and pathogenesis of diabetes mellitus in treated HIV-infection. Best Pract Res Clin Endocrinol Metab 25(3):469–478
Paton NI, Kityo C, Hoppe A, Reid A, Kambugu A, Lugemwa A et al (2014) Assessment of second-line antiretroviral regimens for HIV therapy in Africa. N Engl J Med 371(3):234–247
Pettersen JA, Jones G, Worthington C, Krentz HB, Keppler OT, Hoke A et al (2006) Sensory neuropathy in human immunodeficiency virus/acquired immunodeficiency syndrome patients: protease inhibitor-mediated neurotoxicity. Ann Neurol 59(5):816–824
Shaikh A, Bentley A, Kamerman PR (2013) Symptomatology of peripheral neuropathy in an African language. PLoS One 8(5):e63986
van Buuren S, Boshuizen HC, Knook DL (1999) Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 18(6):681–694
van der Watt JJ, Harrison TB, Benatar M, Heckmann JM (2011) Polyneuropathy, anti-tuberculosis treatment and the role of pyridoxine in the HIV/AIDS era: a systematic review. Int J Tuberc Lung Dis 15(6):722–728
van Oosterhout JJ, Mallewa J, Kaunda S, Chagoma N, Njalale Y, Kampira E et al (2012) Stavudine toxicity in adult longer-term ART patients in Blantyre, Malawi. PLoS One 7(7):e42029
Wadley AL, Cherry CL, Price P, Kamerman PR (2011) HIV neuropathy risk factors and symptom characterization in stavudine-exposed South Africans. J Pain Symptom Manag 41(4):700–706
Westreich DJ, Sanne I, Maskew M, Malope-Kgokong B, Conradie F, Majuba P et al (2009) Tuberculosis treatment and risk of stavudine substitution in first-line antiretroviral therapy. Clin Infect Dis 48(11):1617–1623
Wright E, Brew B, Arayawichanont A, Robertson K, Samintharapanya K, Kongsaengdao S et al (2008) Neurologic disorders are prevalent in HIV-positive outpatients in the Asia-Pacific region. Neurology 71(1):50–56
Acknowledgments
We thank all the patients and staff from all the centres participating in the EARNEST trial. The EARNEST trial was funded by the European and Developing Countries Clinical Trials Partnership (EDCTP) with contributions from the Medical Research Council, UK, Institito de Salud Carlos III, Spain, Irish Aid, Ireland, Swedish International Development Cooperation Agency (SIDA), Sweden, Instituto Superiore di Sanita (ISS), Italy and Merck, USA. Substantive in-kind contributions were made by the Medical Research Council Clinical Trials Unit, UK, CINECA, Bologna, Italy, Janssen Diagnostics, Mechelen, Belgium; GSK, UK; Abbott Laboratories, USA. Trial medication was donated by AbbVie, Merck, Pfizer, GSK and Gilead
Conflict of interest
NIP was the EDCTP grant recipient for this trial. NIP, ASW, MT, JT and AAP are employed by the MRC-UK. NIP, ASW and AAP have received funding support for other studies from GSK or Janssen. AM, GM and HM have received support from the Research Councils-UK for research projects. NIP has received payments for lectures from Merck, Janssen and AbbVie. AAP has received payments for lectures from Janssen. Institutional payment has been received from Gilead Sciences because of a lecture given by ASW. ASW has been DSMB member—for studies sponsored by Tibotec.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Members of the Europe Africa Research Network for Evaluation of Second-line Therapy (EARNEST) Trial Team are listed in the Appendix
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 85 kb)
The EARNEST Trial Team are:
The EARNEST Trial Team are:
Participating Sites
Uganda:
JCRC Kampala (African trial co-ordinating centre; 231) E Agweng, P Awio, G Bakeinyaga, C Isabirye, U Kabuga, S Kasuswa, M Katuramu, C Kityo, F Kiweewa, H Kyomugisha, E Lutalo, P Mugyenyi, D Mulima, H Musana, G Musitwa, V Musiime, M Ndigendawan, H Namata, J Nkalubo, P Ocitti Labejja, P Okello, P Olal, G Pimundu, P Segonga, F Ssali, Z Tamale, D Tumukunde, W Namala, R Byaruhanga, J Kayiwa, J Tukamushaba.
IDI, Kampala (216): G Bihabwa, E Buluma, P Easterbrook, A Elbireer, A Kambugu, D Kamya, M Katwere, R Kiggundu, C Komujuni, E Laker, E Lubwama, I Mambule, J Matovu, A Nakajubi, J Nakku, R Nalumenya, L Namuyimbwa, F Semitala, B Wandera, J Wanyama
JCRC, Mbarara (97): H Mugerwa, A Lugemwa, E Ninsiima, T Ssenkindu, S Mwebe, L Atwine, H William, C Katemba, S Abunyang, M Acaku, P Ssebutinde, H Kitizo, J Kukundakwe, M Naluguza, K Ssegawa, Namayanja, F Nsibuka, P Tuhirirwe, M Fortunate
JCRC Fort Portal (66): J Acen, J Achidri, A Amone, M. Chamai, J Ditai, M Kemigisa, M Kiconco, C Matama, D Mbanza, F Nambaziira, M Owor Odoi, A Rweyora, G. Tumwebaze
San Raphael of St Francis Hospital, Nsambya (48): H Kalanzi, J Katabaazi , A Kiyingi, M Mbidde, M. Mugenyi, R Mwebaze, P Okong, I Senoga
JCRC Mbale (47): M Abwola, D Baliruno, J Bwomezi, A Kasede, M Mudoola, R Namisi, F Ssennono, S Tuhirwe
JCRC Gulu (43): G Abongomera, G Amone, J Abach, I Aciro, B Arach, P Kidega, J Omongin, E Ocung, W Odong, A Philliam
JCRC Kabale (33): H Alima, B Ahimbisibwe, E Atuhaire, F Atukunda, G Bekusike, A Bulegyeya, D. Kahatano, S Kamukama, J Kyoshabire, A Nassali, A Mbonye, T M Naturinda, Ndukukire, A Nshabohurira, H. Ntawiha, A Rogers, M Tibyasa;
JCRC Kakira (31): S. Kiirya, D. Atwongeire, A. Nankya, C. Draleku, D. Nakiboneka, D. Odoch, L. Lakidi, R. Ruganda, R. Abiriga, M. Mulindwa, F. Balmoi, S. Kafuma, E. Moriku
Zimbabwe
University of Zimbabwe Clinical Research Centre, Harare (265): J Hakim, A Reid, E Chidziva, GMusoro,
C Warambwa, G Tinago, S Mutsai, M Phiri, S Mudzingwa, T Bafana, V Masore, C Moyo, R Nhema, S Chitongo.
Malawi
College of Medicine, University of Malawi, Blanytre (92): Rob Heyderman, Lucky Kabanga, Symon Kaunda, Aubrey Kudzala, Linly Lifa, Jane Mallewa, Mike Moore, Chrissie Mtali, George Musowa, Grace Mwimaniwa, Rosemary Sikwese, Joep van Oosterhout, Milton Ziwoya
Mzuzu Central Hospital, Mzuzu (19): H Chimbaka. B Chitete, S Kamanga, T Kayinga E Makwakwa, R Mbiya, M Mlenga, T Mphande, C Mtika, G Mushani, O Ndhlovu, M Ngonga, I Nkhana, R Nyirenda
Kenya
Moi Teaching and Referral Hospital (52): P Cheruiyot, C Kwobah, W Lokitala Ekiru, M Mokaya, A Mudogo, A Nzioka, A Siika, M Tanui, S Wachira, K Wools-Kaloustian
Zambia
University Teaching Hospital (37): P Alipalli, E Chikatula, J Kipaila, I Kunda, S Lakhi, J Malama, W Mufwambi, L Mulenga, P Mwaba, E Mwamba, A Mweemba, M Namfukwe
The Aids Support Organisation (TASO), Uganda: E Kerukadho, B Ngwatu, J Birungi
MRC Clinical Trials Unit: N Paton, J Boles, A Burke, L Castle, S Ghuman, L Kendall, A Hoppe, S Tebbs, M Thomason, J Thompson, S Walker, J Whittle, H Wilkes, N Young
Monitors: C Kapuya, F Kyomuhendo, D Kyakundi, N Mkandawire, S Mulambo, S Senyonjo
Clinical Expert Review Committee: B Angus, A Arenas-Pinto, A Palfreeman, F Post, D Ishola
European Collaborators: J Arribas, B Colebunders, M Floridia, M Giuliano, P Mallon, P Walsh, M De Rosa, E Rinaldi
Trial Steering Committee: I Weller (Chair), C Gilks, J Hakim, A Kangewende, S Lakhi, E Luyirika, F Miiro, P Mwamba, P Mugyenyi, S Ojoo, N Paton, S Phiri, J van Oosterhout, A Siika, S Walker, A Wapakabulo,
Data Monitoring Committee: T Peto (Chair), N French, J Matenga
Pharmaceutical companies: G Cloherty, J van Wyk, M Norton, S Lehrman, P Lamba, K Malik, J Rooney, W Snowden, J Villacian
Rights and permissions
About this article
Cite this article
Arenas-Pinto, A., Thompson, J., Musoro, G. et al. Peripheral neuropathy in HIV patients in sub-Saharan Africa failing first-line therapy and the response to second-line ART in the EARNEST trial. J. Neurovirol. 22, 104–113 (2016). https://doi.org/10.1007/s13365-015-0374-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-015-0374-7