Abstract
Human immunodeficiency virus (HIV) mainly attacks lymphocytes of the human immune system. The untreated infection leads to acquired immune deficiency syndrome (AIDS). Ritonavir (RTV) belongs to protease inhibitors (PIs), the crucial contributors of the combination therapy used in the treatment of HIV that is called highly active antiretroviral therapy (HAART). Formulations targeting the lymphatic system (LS) play a key role in delivering and maintaining therapeutic drug concentrations in HIV reservoirs. In our previous study, we developed RTV-loaded nanostructured lipid carriers (NLCs), which contain the natural antioxidant alpha-tocopherol (AT). In the current study, the cytotoxicity of the formulation was studied in HepG2, MEK293, and H9C2 cell lines. The formulation efficacy to reach the LS was evaluated through a cycloheximide-injected chylomicron flow blockade model in Wistar rats. Biodistribution and toxicity studies were conducted in rodents to understand drug distribution patterns in various organs and to establish the safety profile of the optimized formulation (RTV-NLCs). From the MTT assay, it was found that the cell viability of the formulation is comparable with the pure drug (RTV-API). More than 2.5-folds difference in AUC was observed in animals treated with RTV-NLCs with and without cycloheximide injection. Biodistribution studies revealed higher drug exposure in the lymphoidal organs with the RTV-NLCs. No significant increase in serum biomarkers for hepatotoxicity was observed in rats dosed with the RTV-NLCs. The current study reveals the lymphatic uptake of the RTV-NLCs and their safety in rodents. As the tissue distribution of RTV-NLCs is high, hence re-adjusting the RTV-NLCs dose to get the response equivalent to RTV-API may be more beneficial with respect to its safety and efficacy.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
PIs are crucial in treating human immunodeficiency virus (HIV) and are one of the key components of the highly active antiretroviral therapy (HAART) used in managing acquired immune deficiency syndrome (AIDS) [1, 2]. Ritonavir (RTV) is an antiretroviral drug and belongs to the class of protease inhibitors (PIs) [3]. It belongs to BCS class II with low solubility and high permeability [3,4,5]. RTV is known to have low oral bioavailability and severe side effects when administered for a longer time. The bioavailability of RTV in preclinical subjects varies from 7 to 30%, depending upon the species. However, absolute bioavailability is not known [6]. The major side effects of RTV include hepatotoxicity and cardiovascular dysfunction [7, 8]. RTV-induced hepatotoxicity mainly depends on the dose and duration of the administration [9,10,11]. The risk associated with the full dose (saquinavir and RTV 400 mg twice daily or RTV 600 mg twice daily) is independent of chronic hepatitis B or C co-infection [12].
First-pass metabolism is one of the major problems for many drugs with low oral bioavailability. Most of the drugs administered orally enter to the systemic blood circulation through the portal vein. However, some high lipophilic drugs enter systemic circulation by avoiding first-pass metabolism facilitating transport through the intestinal LS [13]. The lymphatic route is not only involved in the absorption of lipids; however, it can also be used as an option to deliver the drugs to treat various diseases, such as HIV and cancers, which can enter the lymphatic system (LS) [14].
The LS acts as one of the major reservoirs of HIV. Viral replication is much higher in lymph nodes than in peripheral blood mononuclear cells [15, 16]. It is difficult to maintain therapeutic concentrations to suppress the viral loads in its reservoirs, such as lymphoidal organs using conventional dosage forms [16, 17]. Even though conventional treatment can reduce viral load in plasma, after a few weeks of the treatment, it is still possible to isolate the virus from lymph nodes [16]. Hence, targeting and delivering anti-HIV drugs into the LS is of utmost importance to suppress and regulate viral loads.
Drug delivery systems targeting lymphatics are one of the emerging approaches for delivering various drugs, proteins, peptides, and vaccines [18]. Novel drug delivery carriers such as lipid-based nanoformulations are one of the best approaches for the transportation of drugs into the intestinal LS [16]. Lipid-based formulations have become one of the most promising approaches in commercial and academics in developing drug carriers to overcome the bioavailability issues of especially hydrophobic drugs [19]. Nanostructured lipid carriers (NLCs) and solid lipid nanoparticles (SLNs) are commonly used lipid-based nanoformulations that consist of unique characteristics and make them the ideal choice for targeting the LS [14]. Lymphatic delivery of therapeutic agents helps to avoid the hepatic exposure, and it is advantageous in enhancing the oral bioavailability of drugs that exhibits poor oral bioavailability, because of their first-pass metabolism. In addition, drug-induced toxicity can be reduced as the dose is minimized with increased bioavailability [16]. Formulations intended to target the intestinal lymphatics can avoid drug transport to portal circulation and can be directed into systemic circulation through the thoracic duct [13].
SLNs and NLCs are the most commonly used lipid-based nanoformulations to deliver the lipophilic drugs. SLNs consist of a solid core of a lipid matrix in which the drug is entrapped. NLCs are considered the next-generation SLNs, where the drug is encapsulated inside the matrix formed by combining solid lipids and liquid lipids. NLCs offer higher drug entrapment than SLNs and less drug leaching effect. Controlled release, protection from enzymatic degradation, non-toxicity because of biocompatibility, and ease of scale up are some additional advantages of NLCs [20]. In the recent past, many researchers developed SLNs and NLCs for targeting the LS for various drugs such as mebendazole [18], praziquantel [18], nintedanib esylate [21], and atazanavir [22].
Several researchers developed various formulations to improve the oral bioavailability of RTV, such as NLCs [22, 23], SLNs [5, 24], and proliposomes [25]. In our previous study, we developed antioxidant-containing ritonavir-loaded NLCs and achieved a sevenfold higher AUC and > 10-folds higher Cmax [26]. In the present study, we assessed the potentiality of the formulation to absorb into the intestinal LS by passing the hepatic first-pass metabolism. Furthermore, to understand the distribution pattern of the formulation, tissue biodistribution studies were conducted in rodents. Finally, the safety profile of the formulation was established in rodents by conducting a repeat dose toxicity study.
Materials and methods
Chemicals and reagents
The RTV-API used in the formulation preparation was the generous gift of Dr. Reddy’s Laboratories (Hyderabad, India). The solid lipids (glyceryl monostearate, GMS and stearic acid, SA) used in the preparation of NLCs were procured from Finar Ltd., Ahmedabad, India, and Fine Organics, Mumbai, India. The liquid lipids (oleic acid and alpha-tocopherol, AT) used in the preparation of NLCs were purchased from Sigma-Aldrich, Bangalore, India. Lopinavir-API was used as the internal standard (IS) in the bioanalysis of in vivo samples, and it was obtained as a gift sample from Cipla Ltd., Mumbai, India. The surfactants/stabilizers (Tween 20 and sodium lauryl sulfate (SLS)) were procured from Loba Chemie Pvt. Ltd. and Merck, Mumbai, India. The organic solvent (methanol) used in preparing HPLC mobile phase was obtained from SD Fine Chemicals, Mumbai. Cycloheximide was procured from Sisco Research Laboratories Pvt. Ltd., Mumbai. The ortho-phosphoric acid (OPA) used in the preparation of the mobile phase was procured from Spectrochem Private Limited, Mumbai. Regents for biochemical parameters analysis were purchased from Agappe Diagnostics, Mumbai. The type-I water used in the formulation and HPLC mobile phase preparation was collected from Elix-Millipore Advantage (Millipore Corporation, Billerica, MA, United States). All the cell lines used for the cytotoxicity studies were procured from NCCS, Pune, India.
Animals
All animal studies were conducted in Wistar rats (male and female, with an approximate weight of 200–250 g). All the animals used for the in vivo studies were inbred at the Central Animal Research Facility (CARF), MAHE, Manipal. All in vivo studies were carried out at CARF following CPCSEA norms and institutional guidelines with prior approval from the Institutional Animal Ethical Committee (approval No. IAEC/KMC/51/2018 and IAEC/KMC/72/2021).
Bioanalytical method for the quantification of RTV in in vivo samples
The protein precipitation (PPT) method was followed. RTV was extracted from Wistar rat plasma/tissue homogenate, as reported earlier [26]. Briefly, 50 μL of plasma/100 μL of tissue homogenate was transferred to a pre-labeled tube, and 20/40 μL of IS (Lopinavir, 200 μg/mL) was added, respectively and vortexed to mix. Precipitation solution (150/300 μL of ice-cold methanol, respectively) was added to all the samples, vortexed, and centrifuged (3K30, Sigma Laborzentrifugen GmbH, Germany) at a speed of 15,000 rpm for a duration of 10 min at a temperature of 4 °C. Finally, the supernatant of the samples was transferred to pre-labeled fresh autosampler vials and injected to the HPLC (LC2010CHT, Shimadzu Corporation, Kyoto, Japan). The chromatographic method developed previously was used to quantify RTV in plasma and tissue homogenate samples [26]. Briefly, the stationary phase consists of a Kromacil C18 (250 × 4.6 mm, 5 μm) column and a combination of aqueous (type-I water, pH 3.0) and organic (methanol) solvents in a ratio of 15:85, % v/v was used as the mobile phase. The stationary phase (column) was maintained at a temperature of 25 °C during the analysis. The mobile phase was pumped at a flow rate of 1.200 mL/min. The total run time of the method was 12 min, and detector wavelength was set to 242 nm.
Preparation of antioxidant-containing ritonavir-loaded NLCs
RTV-NLCs were prepared using stearic acid, glyceryl monostearate (GMS), alpha-tocopherol (AT), and oleic acid as the major excipients. NLCs were prepared by the hot-emulsion—ultra-sonication method, as reported previously [26]. In brief, solid lipids were melted using a water bath, to which liquid lipids were added. The drug (50 mg) was added to the molten mixture of lipids and mixed. To this mixture, the surfactant solution (SLS and Tween 20, kept on a water bath maintaining the same temperature as that of molten lipid) was added to form the emulsion. The solution was sonicated using a probe sonicator and chilled on an ice bath.
Cell viability studies using MTT reagent
Cytotoxicity studies were performed in three different cell lines, i.e., human embryonic kidney cells (HEK293), human liver cancer cells (HepG2), and cardiomyocytes (H9C2). Cells were cultured in 96 well plates (5000/well) using DMEM containing FBS (10%) and 1% anti-streptomycin and anti-penicillin. Cytotoxicity studies were performed for RTV-API, blank NLCs, and RTV-NLCs, and the concentration of the drug was maintained at 100 μM (stock solutions were prepared in DMSO, and the final dilutions were made in DMEM). The study was done in triplicate, and incubation conditions of 37 °C and 5% carbon dioxide (CO2) supply were maintained for 24 h. Control group cells were not given any treatment. For the DMSO control group, cells were treated with DMSO (less than 1%). Post-incubation of 24 h, each well was washed with PBS after decanting the supernatant. Followed by MTT reagent, it was added to each well under dark conditions and incubated for another 4 h. Post-incubation, the solution was decanted from all the wells and sterile DMSO was added, followed by vigorous shaking to ensure solubilization of the formazan crystals. Finally, the absorbance was recorded using a microplate reader at a wavelength of 570 nm.
Evaluation of lymphatic uptake of the formulation
Male Wistar rats were used for the lymphatic uptake evaluation study where animals were divided into two groups, with six rats in each group. Group I rats were dosed orally with RTV-NLCs (50 mg/kg), whereas group II animals were given intraperitoneal injection of cycloheximide (3 mg/kg) [18], and post-1 h, cycloheximide injection animals were dosed orally with RTV-NLCs (50 mg/kg) (animals were fasted over night before dosing). At different time points, the blood was withdrawn through retro-orbital plexus technique and collected into pre-labeled tubes containing an anti-coagulant (potassium EDTA). Plasma was separated from all the samples by centrifugation at 15,000 rpm, 4 °C for 10 min. The RTV concentrations in plasma samples were determined using the HPLC bioanalytical method. Finally, Pharmacokinetic (PK) parameters were calculated using Win-Nonlin software, version 5.2.
Biodistribution studies
Female Wistar rats were for the biodistribution studies. Animals were divided into three groups; each group was having 27 rats. Group I animals were treated with single dose of RTV-API suspension (50 mg/kg, po). RTV-marketed formulation (MF) suspension (Ritomune, 50 mg/kg, po) was dosed to group II animals. Group III animals were treated with RTV-NLCs (50 mg/kg, po). Three animals from each group were sacrificed at different time points, and organs such as the brain, heart, liver, spleen, kidney, stomach, intestine, and colon were collected. All the tissues were homogenized with normal saline as the diluent. In brief, tissues were individually weighed using a weighing balance, and diluent was added in a ratio of 1:2. Finally, tissues were homogenized using a high-speed homogenizer (T 25 digital Ultra-Turrax®, IKA Dispersers, Germany) at a speed of 15,000 rpm. RTV concentration in all tissue homogenate samples was determined using the HPLC bioanalytical method. PK parameters were calculated using Win-Nonlin software, version 5.2.
Toxicity studies
The toxicity study was conducted in male Wistar rats. Animals were divided into four groups, each with six rats. Group I animals were treated with vehicle (0.25% w/v sodium CMC, po). Group II animals were treated with RTV-API suspension (50 mg/kg, po). MF suspension (Ritomune, 50 mg/kg, po) was given to group III animals, and for group IV animals, RTV-NLCs (50 mg/kg, po) was given. All the animals were given treatment daily for 28 days. The blood was withdrawn from all the animals on day 0 before starting the treatment and then on day 28. Blood parameters were evaluated using a veterinary cell counter (PCE-21OVET, ERMA Inc., Tokyo, Japan). The serum was separated and analyzed for biochemical parameters using a biochemical auto-analyzer (Mispa Nano, Agappe, Switzerland). On day 28, all the animals were sacrificed, and major organs (brain, heart, liver, spleen, stomach, intestine, colon, and kidney) were collected and fixed in 10% formalin for 48 h. Blocking or embedding the tissue was done to transfer the tissue from the final wax bath to a mold filled with molten paraffin wax. Thin sections of tissues of approximately 4 microns were cut from the blocks with the help of a microtome. The tissue sections were floated in a water bath at 50–52 °C and placed on microscopic slides. Hematoxylin and eosin staining of sections was performed, followed by histopathological examination.
Statistical analysis
All the results are expressed as mean ± SD, n ≥ 3. GraphPad Prism (version 5.03, San Diego, California, USA) was used for all the statistical calculations. One-way ANOVA with Dunnett’s post hoc test/Bonferroni post hoc test was used for the statistical analysis, and P < 0.05 was considered statistically significant.
Results
Preparation of antioxidant-containing ritonavir-loaded NLCs
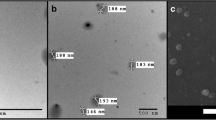
RTV-loaded NLCs were prepared following the procedure mentioned in our previous work [26], where the final excipients include stearic acid (50 mg), GMS (174.12 mg), AT (18 μL), oleic acid (24 μL), SLS (0.25%), and Tween 20 (0.93%). All the parameters of the formulation were found to be within the range of validation data (i.e., particle size, PDI, zeta potential, and entrapment efficiency were found to be 362.1 ± 27.57 nm, 0.431 ± 0.05, − 56.40 ± 10.43 mV, and 46.40 ± 4.00%) [26].
MTT assay
In vitro cytotoxicity assays on HEPG2 cells revealed the percent cell viability of RTV-NLCs was similar to the percent cell viability of RTV-API suspension. However, cell viability was significantly lower in both the treatments than control-treated cells. A similar kind of percent cell viability pattern was observed in HEK 293 and H9C2 cells, and the results are presented in Fig. 1 and it was found that there is no significant difference between the percent cell viability of RTV-API suspension and RTV-NLCs.
In vitro cytotoxicity assay of ritonavir pure suspension, blank NLCs, and drug-loaded NLCs in HEK293, HEPG2, and H9C2 cell lines. The percent cell viability of drug-loaded NLCs is comparable to the pure drug suspension in all the cell lines. The results are expressed as mean ± SD, n = 4. One-way ANOVA with Dunnett’s post hock test was used for the statistical analysis. P < 0.05 was considered statistically significant
Evaluation of lymphatic uptake of the formulation
The plasma concentration profile of group I and II is shown in Fig. 2, and PK parameters of both the groups are given in Table 1. The data showed the RTV absorption more than 2.5-folds higher in group I (without cycloheximide) animals compared to the group II (with cycloheximide). Cycloheximide blocks the lymphatic uptake of drugs; hence, the absorption noticed in group II is representing the absorption achieved only through the portal vein. In group I, extravagant amount of the drug was absorbed through the lymphatic pathway as there was free access to the NLCs for entry into LS, which is evident from the higher Cmax (maximum concentration) and AUC (area under the curve). These results are in line with the previous work [20, 27, 28] in this area for other drugs such as mebendazole [27], atazanavir [20], and darunavir [28]. The elimination rate of constant, mean residence time (MRT), and half-life (t1/2) is almost similar in both the groups.
Biodistribution studies
RTV-API suspension, MF, and RTV-NLCs tissue concentration profiles are shown in Fig. 3, and pharmacokinetic parameters are presented in Table 2. RTV-NLCs exhibited higher drug exposure in the brain, heart, liver, spleen, and kidney compared to the other organs. In contrast, lower exposure was observed in the stomach, intestine, and colon. Tmax of RTV-NLCs group was found to be less than 2 h for most of the tissues (heart, liver, spleen, kidney, intestine, and colon), except brain and stomach, which showed the highest Tmax value compared to the RTV-API suspension and MF. Animals treated with RTV-NLCs showed higher Cmax and AUC in the heart, liver, spleen, and kidney compared to the other groups. In contrast, lower Cmax and AUC values were obtained in the brain, stomach, intestine, and colon. Previously, tissue distribution studies were conducted in female rats (Norvir 50 mg/kg), and time-dependent exposure of RTV was reported in all tissues except the gastrointestinal tract and liver [6]. The mean residence time (MRT) of the RTV-NLCs group was found to be similar in all the tissue compared to the RTV-API and MF groups.
Toxicity studies
Blood parameters of different group of animals for day 0 and 28 are presented in Fig. 4, whereas the serum biomarkers estimation is presented in Figs. 5 and 6. Histopathological examination of all the groups was performed for various tissues such as brain, heart, lungs, liver, spleen, kidney, stomach, intestine, and colon. The microscopical images of tissues are presented in Fig. 7.
Hematological parameters (total WBC, RBC, hemoglobin, and platelets) in rat blood samples after treatment with different formulations. The results are expressed as mean ± SD, n = 6. One-way ANOVA with the Bonferroni post hock test was used for the statistical analysis, *P < 0.05 was considered statistically significant
Biochemical parameters (HDL high-density lipoprotein, LDL low-density lipoprotein, total protein, and LDH lactate dehydrogenase) in rat serum samples after treatment with different formulations. The results are expressed as mean ± SD, n = 6. One-way ANOVA with the Bonferroni post hock test was used for the statistical analysis, *P < 0.05 was considered statistically significant
No significant difference was found in total WBCs, RBCs, and hemoglobin between day 0 and day 28 in all the groups (Fig. 4). But, platelets decreased significantly in groups II and IV from day 0 to 28 (Fig. 4). There was no significant difference observed in serum glutamic-oxaloacetic transaminase (SGOT) levels from day 0 to day 28 in group I and group II animals. However, group III animals exhibited a significant increase in SGOT levels from day 0 to 28, indicating hepatotoxicity. In the case of group IV animals, there was no significant difference in SGOT levels was noticed from day 0 to 28. Serum glutamic pyruvic transaminase (SGPT) levels increased slightly from day 0 to 28 in groups III and IV animas. However, the difference is not significant in any of the groups. SGOT and SGPT data is depicted in Fig. 5.
Furthermore, group IV animals showed a significant increase in high-density lipoprotein (HDL) and low-density lipoprotein (LDL) levels from day 0 to 28. In contrast, group III animals exhibited only a significant increase in LDL levels. There was no significant difference noticed in LDL and HDL levels of other groups between days 0 and 28. These findings are deviating from a literature which reported increased levels of total cholesterol, LDL, triglycerides, total/HDL, and decreased HDL levels after treatment with ritonavir. However, the study was conducted in healthy volunteers and at a lower dose (100 mg bid) than the usual dose (400 mg bid) [29]. HDL, LDL, total protein, and LDH results are illustrated in Fig. 6.
No histological changes (Fig. 7) such as inflammation or necrosis in brain tissue was observed in any groups except a few degenerated neurons in the hippocampal region of group IV animals. From the biodistribution studies data, it is evident that the concentration of drug is increasing in formulation group animals (in brain mainly after 12 h) compared to the marketed and standard drug group animals. Might be this concentration is responsible for the degeneration of neurons, but not for necrosis. However, this study suggesting for further investigation to understand the degeneration of neurons and also suggesting for dose adjustment which will further reduce the side effects. In case of lung tissue, group I animals showed very few acute and chronic inflammatory cells, whereas group II animals showed inflammatory infiltration in a few areas. However, other two groups, i.e., group III and group IV, exhibited expansion of the interstitial compartment with acute inflammatory cells like neutrophils and chronic inflammatory cells like plasma cells and macrophages. Neutrophilic infiltration was observed in interstitial space, alveolar space, and blood vessels. Group IV also showed edematous areas. No histological changes like degeneration, inflammation, and necrosis were noticed in group I and group II. Group III and group IV revealed mild infiltration of chronic inflammatory cells like lymphocytes. Group III also showed hemorrhagic areas.
Liver tissue, group I, was normal without any histological changes. Group II showed infiltration of chronic inflammatory cells like lymphocytes around blood vessels, focal necrosis, chronic inflammatory infiltrate, and congested blood vessels in some areas. In group IV animals, congested blood vessels, dilated sinusoids, and inflammatory infiltrate were observed. No histological changes were noticed in the spleen of groups 1, II, and IV. Reduced white pulp area was perceived in group III animals. Few degenerated tubules with swollen cytoplasm with sloughing of cells in the lumen of kidney tissue were observed in all the groups except the group I.
Additionally, the marketed formulation (i.e., group III) showed few dilated tubules in the kidney. No significant histological changes were observed in the stomach and small intestine of all the treatment groups. Compared to the group I, groups III and IV showed infiltration of acute and chronic inflammatory cells in the mucosa, sub-mucosa, and congested blood vessels in the sub-mucosa.
Discussion
In the current study, the in vitro cytotoxicity assay of RTV-NLCs reveals the cell viability of the formulation was comparable with the RTV-API suspension, and this could be possible due to the biocompatibility of the excipients used in the preparation of the formulation. Bypassing hepatic exposure by RTV is required to reduce the drug-induced hepatotoxicity, which is the primary reason behind the limited use of RTV as a protease inhibitor. Moreover, lymph nodes, lymph, and GALT are the most important reservoirs of HIV. Mainly, lymph nodes are central to the physiology of HIV [30,31,32]. Delivery of antiviral drugs to these reservoirs and maintenance of their therapeutic concentrations plays a crucial role in suppressing the viral load. Recently, researchers developed drug delivery systems to target HIV reservoirs in LS for drugs such as lopinavir [31]. Previously, Gurumukhi and Bari developed RTV-loaded NLCs to enhance the bioavailability. The researchers evaluated permeation enhancement and pharmacokinetics of the formulation [22]. However, the ability of the formulation to enter LS was not assessed. In our previous study, antioxidant-containing RTV-loaded NLCs were developed, and the pharmacokinetic studies of optimized formulation revealed the enhanced bioavailability of this drug [26].
Lymphatic targeting of drugs enhances the oral bioavailability by evading hepatic exposure. Hence, the evaluation of the lymphatic transport of these formulations is necessary to ensure that the intended delivery system is reaching its target. The gastrointestinal tract is richly supplied with blood and lymphatic vessels. However, the fluid flow rate is much higher in portal blood than lymph flow in intestinal lymphatic vessels [18]. Xenobiotics enter the LS mainly through any of the three mechanisms, the transcellular route associated with chylomicrons, paracellular mechanisms associated with absorption enhancers, and M-cells. There are several methods to investigate xenobiotic lymphatic uptake, such as cannulation of the lymphatic duct. Animal models are the commonly used methods for evaluating the lymphatic transport system, which usually involves the cannulation of the mesenteric lymph duct that provides access to collect the lymph. The collection of lymph at various time points and quantifying the drug in the samples provides information on the extent to which the drug is entering the LS. However, cannulation of the mesenteric lymphatic duct by surgical method requires high skill to perform survival surgery on animals. Alternatively, blockage of chylomicron secretion from enterocytes can be used to assess the drug transport through LS. Chemical inhibitors such as cycloheximide and colchicine are administered to animals before actual formulation administration to block lymphatic absorption. Protein synthesis inhibitors such as cycloheximide, colchicine, and non-ionic surfactant Pluronic L-81 inhibit chylomicron secretion [33]. In previous studies, researchers have used cycloheximide for inhibition of lymphatic pathways to evaluate the intestinal lymphatic delivery of formulations such as mebendazole-loaded NLCs, praziquantel-loaded SLNs, lipid nanoparticles of darunavir, baicalein-phospholipid complex self-micro emulsifying drug delivery systems (SMEDDS), and Pueraria flavone-loaded self-emulsifying drug delivery systems (SEDDS), nintedanib esylate loaded in NLCs [18, 21, 27, 28, 34, 35].
In the current study, we used the cycloheximide-injected chylomicron flow blockade model to evaluate the lymphatic targeting of RTV-NLCs. The absorption of NLCs into the LS can be attributed to the long-chain fatty acids (GMS and stearic acid) used in the preparation of the formulation. Furthermore, liquid lipids used in the preparation of NLCs helped in the formation of the matrix that can encapsulate the drug. Lipids consisting of small-chain fatty acids (< 12C) tend to absorb into the systemic circulation, whereas medium- and long-chain fatty acids get absorbed into the LS bypassing the portal circulation [36]. These long-chain fatty acids are re-esterified and transported through intestinal lymph, which involves the acylation of absorbed 2-monoacylglycerol with fatty acids, resulting in di- and, finally, triglyceride lipids [19]. Long-chain fatty acids are good solvents for lipophilic drugs and transport them to the LS by incorporating them into chylomicrons. AT is also a good solvent for lipophilic drugs. It enters into the LS through passive diffusion by incorporating into chylomicrons and then into the systemic circulation through the lymph. The absorption of AT can be increased by the co-administration of triglycerides [37].
The biodistribution studies revealed that the AUC of the RTV-NLC group in the lymphoidal organ, i.e., the spleen, was more than two folds compared to the RTV-API suspension and MF. This can be attributed to the lymphatic targeting of the formulation and limited access to the free RTV to the LS in other treatments. A similar biodistribution pattern was reported for the antiviral drug atazanavir encapsulated in NLCs in the recent past [20]. Furthermore, the Tmax of the RTV-NLCs group in the spleen is lower than the RTV-API suspension and MF group. These results support the possible cause of the rapid absorption of RTV-NLCs into the LS as long-chain fatty acids used in the preparation of NLCs act as drug transporters [20, 38]. Moreover, lower AUC was observed in the intestine, which supports the timely absorption of the drug from the intestine into the LS. Approximately 15% of higher AUC was observed in the liver tissues of RTV-NLCs treatment animals compared to the MF. In contrast, more than 7-folds of higher plasma concentrations were observed in the formulation group in our previous study [26], which further supports bypassing the first-pass metabolism and absorption of RTV via the LS.
RTV-induced hepatotoxicity is one of the major adverse effects seen in HIV patients. The hepatotoxicity caused by RTV is concentration dependent. However, there is no clear mechanism identified for the RTV-induced hepatotoxicity. The severity of hepatotoxicity is categorized into grades by considering the elevated serum concentrations of liver enzymes SGOT and SGPT [9]. In general, the classification of hepatotoxicity from grades 1 to 4 is based on alteration in SGOT or SGPT levels compared to the upper limit of the normal reference range [39]. Even though the absorption of the drug is much higher in group IV animals than II and III, there is still no significant increase in the hepatotoxic biomarkers in serum, which supports the lower hepatotoxic nature of the formulation. The submicron particle size of NLCs and avoidance of first-pass metabolism by absorption through the LS could be the reason for the lower hepatotoxicity of the formulation.
Normal functioning of a cell requires a balance between reactive species (ROS, RNS) produced in the cell and antioxidant enzymes that include lactoperoxidase, glutathione peroxidoxin, superoxide dismutase (SOD), and catalases, and failure of the balance causes oxidative stress. Along with antioxidant enzymes, vitamins such as tocopherols (vitamin E), ascorbic acid (vitamin C), bilirubin, uric acid, and glutathione play a crucial role in maintaining this balance [40]. Alpha-tocopherol is commonly called as vitamin E, which belongs to the family of tocopherols, and it plays an important role in maintaining the immune system [41, 42]. The importance of alpha-tocopherol as an antioxidant was studied by researchers in in vivo and in vitro studies [43, 44]. Moreover, HIV infection is mainly associated with the destruction of the immune system of the body, and it also involves in lowering the levels of vitamin E [41, 45, 46]. This emphasizes vitamin E supplementation in patients suffering from HIV infection treated with Ritonavir. Hence, alpha-tocopherol was incorporated as a source of an antioxidant in the formulation. Previously, many researchers developed various formulations for RTV, such as NLCs [22, 23], SLNs [5, 24], and proliposomes [25], and mainly focused on bioavailability enhancement. However, the safety profile of these formulations and efficacy in reducing hepatotoxicity was not established. Recently, oral toxicity and histopathology studies reported anti-HIV drug atazanavir-loaded NLCs in rats [20]. But, to our knowledge, the safety profile of RTV-NLCs was not studied, and for the first time, we evaluated the safety of RTV-loaded antioxidant-containing NLCs in rats. Furthermore, we author also suggest the investigators working on RTV formulation development to re-adjust the RTV-NLCs dose to get the response equivalent to RTV-API. Even this will further completely reduce the side effects of RTV.
Conclusion
The cytotoxicity assays were performed to evaluate the toxic effect of the antioxidant-containing RTV-loaded NLCs on cell lines before proceeding with the in vivo studies. The lymphatic evaluation study was conducted to assess the formulation efficacy in entering the LS. Furthermore, biodistribution studies were conducted in Wistar rats to understand the distribution of the formulation into the various vital organs of the body. Finally, toxicity studies were carried out in rodents to establish the safety profile of the formulation. The drug-loaded NLCs showed comparable toxicity in cell line studies with pure drug. The lymphatic evaluation and biodistribution results support the uptake of the formulation by the LS. The lower SGPT levels in the RTV-NLCs and higher levels in other treatment group evidences the positive effect of the NLCs on the drug-induced hepatotoxicity. Furthermore, histopathological examination of various tissue also supports the absence of severe histological changes such as cell degeneration and necrosis. Furthermore, re-adjusting the RTV-NLCs dose to get the response equivalent to RTV-API could make this formulation better as it be safe and more effective.
Data availability
All the datasets supporting the findings of this research are available from the author's upon reasonable request.
References
Moyle GJ, Gazzard BG, Cooper DA, Gatell J. Antiretroviral therapy for HIV infection. A knowledge-based approach to drug selection and use. Drugs. 1998;55(3):383–404. https://doi.org/10.2165/00003495-199855030-00005.
Xu H, Krakow S, Shi Y, Rosenberg J, Gao P. In vitro characterization of ritonavir formulations and correlation to in vivo performance in dogs. Eur J Pharm Sci. 2018;115:286–95. https://doi.org/10.1016/j.ejps.2018.01.026.
Mehta C, Narayan R, Aithal G, Pandiyan S, Bhat P, Dengale S, et al. Molecular simulation driven experiment for formulation of fixed dose combination of Darunavir and Ritonavir as anti-HIV nanosuspension. J Mol Liq. 2019;293:111469. https://doi.org/10.1016/j.molliq.2019.111469.
De Espíndola B, Beringhs AO, Sonaglio D, Stulzer HK, Silva MAS, Ferraz HG, et al. Liquisolid pellets: a pharmaceutical technology strategy to improve the dissolution rate of Ritonavir. Saudi Pharm J. 2019;27(5):702–12. https://doi.org/10.1016/j.jsps.2019.04.005.
Kumar S, Narayan R, Ahammed V, Nayak Y, Naha A, Nayak UY. Development of ritonavir solid lipid nanoparticles by Box Behnken design for intestinal lymphatic targeting. J Drug Delivery Sci Technol. 2018;44:181–9. https://doi.org/10.1016/j.jddst.2017.12.014.
EMA. Norvir [Internet]. Eur Med Agency. 2018 [cited 2023 Jul 2]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/norvir.
Reyskens KMSE, Fisher T-L, Schisler JC, O'Connor WG, Rogers AB, Willis MS, et al. Cardio-metabolic effects of HIV Protease inhibitors (Lopinavir/Ritonavir). PLoS ONE. 2013;8(9):e73347. https://doi.org/10.1371/journal.pone.0073347.
Sulkowski MS. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA. 2000;283(1):74. https://doi.org/10.1001/jama.283.1.74.
Kuang C-C, Wang Y, Hu P-C, Gao F-F, Bu L, Wen X-M, et al. Ritonavir-induced hepatotoxicity and ultrastructural changes of hepatocytes. Ultrastruct Pathol. 2014;38(5):329–34. https://doi.org/10.3109/01913123.2014.914114.
Périard D, Telenti A, Sudre P, Cheseaux JJ, Halfon P, Reymond MJ, et al. Atherogenic dyslipidemia in HIV-infected individuals treated with protease inhibitors. The Swiss HIV Cohort Study Circulation. 1999;100(7):700–5. https://doi.org/10.1161/01.cir.100.7.700.
Purnell JQ, Zambon A, Knopp RH, Pizzuti DJ, Achari R, Leonard JM, et al. Effect of Ritonavir on lipids and post-heparin lipase activities in normal subjects. AIDS. 2000;14(1):51–7. https://doi.org/10.1097/00002030-200001070-00006.
Sulkowski MS. Drug-induced liver injury associated with antiretroviral therapy that includes HIV-1 protease inhibitors. Clin Infect Dis. 2004;38(Suppl 2):S90-97. https://doi.org/10.1086/381444.
Managuli RS, Raut SY, Reddy MS, Mutalik S. Targeting the intestinal lymphatic system: a versatile path for enhanced oral bioavailability of drugs. Expert Opin Drug Delivery. 2018;15(8):787–804. https://doi.org/10.1080/17425247.2018.1503249.
Darwis Y, Ali Khan A, Mudassir J, Mohtar N. Advanced drug delivery to the lymphatic system: lipid-based nanoformulations. IJN. 2013;2733. https://doi.org/10.2147/IJN.S41521.
Cohen OJ, Pantaleo G, Lam GK, Fauci AS. Studies on lymphoid tissue from HIV-infected individuals: implications for the design of therapeutic strategies. Springer Semin Immunopathol. 1997;18(3):305–22. https://doi.org/10.1007/BF00813500.
Singh I, Swami R, Khan W, Sistla R. Delivery systems for lymphatic targeting. Focal Contr Drug Del. 2014;429–58. https://doi.org/10.1007/978-1-4614-9434-8_20.
Désormeaux A, Bergeron MG. Lymphoid tissue targeting of anti-HIV drugs using liposomes. Methods Enzymol. 2005;391:330–51. https://doi.org/10.1016/S0076-6879(05)91019-7.
Mishra A, Vuddanda PR, Singh S. Intestinal lymphatic delivery of Praziquantel by solid lipid nanoparticles: formulation design, in vitro and in vivo studies. J Nanotechnol. 2014;2014:1–12. https://doi.org/10.1155/2014/351693.
Humberstone AJ, Charman WN. Lipid-based vehicles for the oral delivery of poorly water soluble drugs. Adv Drug Deliv Rev. 1997;25(1):103–28. https://doi.org/10.1016/S0169-409X(96)00494-2.
Gurumukhi VC, Bari SB. Quality by design (QbD)–based fabrication of atazanavir-loaded nanostructured lipid carriers for lymph targeting: bioavailability enhancement using chylomicron flow block model and toxicity studies. Drug Deliv and Transl Res. 2022;12(5):1230–52. https://doi.org/10.1007/s13346-021-01014-4.
Patel P, Patel M. Enhanced oral bioavailability of nintedanib esylate with nanostructured lipid carriers by lymphatic targeting: In vitro, cell line and in vivo evaluation. Eur J Pharm Sci. 2021;159:105715. https://doi.org/10.1016/j.ejps.2021.105715.
Gurumukhi VC, Bari SB. Development of ritonavir-loaded nanostructured lipid carriers employing quality by design (QbD) as a tool: characterizations, permeability, and bioavailability studies. Drug Deliv Transl Res. 2021. https://doi.org/10.1007/s13346-021-01083-5.
Walimbe CA, More SS, Walawalkar RU, Shah RR, Ghodke D. Optimisation of nanostructured lipid carriers of ritonavir. Inventi Rapid: NDDS. 2012;2012(4):1–8.
Javan F, Vatanara A, Azadmanesh K, Nabi-Meibodi M, Shakouri M. Encapsulation of Ritonavir in solid lipid nanoparticles: in-vitro anti-HIV-1 activity using lentiviral particles. J Pharm Pharmacol. 2017;69(8):1002–9. https://doi.org/10.1111/jphp.12737.
Ahammed V, Narayan R, Paul J, Nayak Y, Roy B, Shavi GV, et al. Development and in vivo evaluation of functionalized ritonavir proliposomes for lymphatic targeting. Life Sci. 2017;183:11–20. https://doi.org/10.1016/j.lfs.2017.06.022.
Jitta SR, Bhaskaran NA, Salwa, Kumar L. Anti-oxidant containing nanostructured lipid carriers of Ritonavir: development, optimization, and in vitro and in vivo evaluations. AAPS PharmSciTech. 2022;23(4):88. https://doi.org/10.1208/s12249-022-02240-w.
Shrivastava S, Gidwani B, Kaur CD. Development of mebendazole loaded nanostructured lipid carriers for lymphatic targeting: optimization, characterization, in-vitro and in-vivo evaluation. Parti Sci Technol. 2021;39(3):380–90. https://doi.org/10.1080/02726351.2020.1750515.
Bhalekar MR, Upadhaya PG, Madgulkar AR, Kshirsagar SJ, Dube A, Bartakke US. In-vivo bioavailability and lymphatic uptake evaluation of lipid nanoparticulates of Darunavir. Drug Delivery. 2016;23(7):2581–6. https://doi.org/10.3109/10717544.2015.1037969.
Shafran SD, Mashinter LD, Roberts SE. The effect of low-dose ritonavir monotherapy on fasting serum lipid concentrations. HIV Med. 2005;6(6):421–5. https://doi.org/10.1111/j.1468-1293.2005.00328.x.
Onabajo OO, Lewis MG, Mattapallil JJ. GALT CD4+PD-1hi T follicular helper (Tfh) cells repopulate after antiretroviral therapy. Cell Immunolo. 2021;366:104396. https://doi.org/10.1016/j.cellimm.2021.104396.
Qin C, Chu Y, Feng W, Fromont C, He S, Ali J, et al. Targeted delivery of lopinavir to HIV reservoirs in the mesenteric lymphatic system by lipophilic ester prodrug approach. J Controlled Release. 2021;329:1077–89. https://doi.org/10.1016/j.jconrel.2020.10.036.
Scholz EMB, Kashuba ADM. The lymph node reservoir: physiology, HIV infection, and Antiretroviral therapy. Clin Pharmacol Ther. 2021;109(4):918–27. https://doi.org/10.1002/cpt.2186.
Dahan A, Hoffman A. Evaluation of a chylomicron flow blocking approach to investigate the intestinal lymphatic transport of lipophilic drugs. Eur J Pharm Sci. 2005;24(4):381–8. https://doi.org/10.1016/j.ejps.2004.12.006.
Liao H, Gao Y, Lian C, Zhang Y, Wang B, Yang Y, et al. Oral absorption and lymphatic transport of baicalein following drug–phospholipid complex incorporation in self-microemulsifying drug delivery systems. IJN. 2019;14:7291–306. https://doi.org/10.2147/IJN.S214883.
Qiao J, Ji D, Sun S, Zhang G, Liu X, Sun B, et al. Oral bioavailability and lymphatic transport of pueraria flavone-loaded self-emulsifying drug-delivery systems containing sodium taurocholate in rats. Pharmaceutics. 2018;10(3):147. https://doi.org/10.3390/pharmaceutics10030147.
Desai J, Thakkar H. Enhanced oral bioavailability and brain uptake of Darunavir using lipid nanoemulsion formulation. Colloids Surf B Biointerfaces. 2019;175:143–9. https://doi.org/10.1016/j.colsurfb.2018.11.057.
Nielsen PB, Müllertz A, Norling T, Kristensen HG. Comparison of the lymphatic transport of a lipophilic drug from vehicles containing α-tocopherol and/or triglycerides in rats. J Pharm Pharmacol. 2010;53(11):1439–45. https://doi.org/10.1211/0022357011777972.
Shete H, Chatterjee S, De A, Patravale V. Long chain lipid based tamoxifen NLC. Part II: pharmacokinetic, biodistribution and in vitro anticancer efficacy studies. Int J Pharm. 2013;454(1):584–92. https://doi.org/10.1016/j.ijpharm.2013.03.036.
Sulkowski MS. Hepatotoxicity associated with antiretroviral therapy containing HIV-1 protease inhibitors. Semin Liver Dis. 2003;23(2):183–94. https://doi.org/10.1055/s-2003-39949.
Anghel L, Baroiu L, Beznea A, Grigore G. The therapeutic relevance of vitamin E. Revista de Chimie. 2019;70:3711–3. https://doi.org/10.37358/RC.19.10.7630.
Graham SM, Baeten JM, Richardson BA, Bankson DD, Lavreys L, Ndinya-Achola JO, et al. Higher pre-infection vitamin E levels are associated with higher mortality in HIV-1-infected Kenyan women: a prospective study. BMC Infec Dis. 2007;7(1):63. https://doi.org/10.1186/1471-2334-7-63.
Ijaz M, Akhtar N. Fatty acids based α-Tocopherol loaded nanostructured lipid carrier gel: in vitro and in vivo evaluation for moisturizing and anti-aging effects. J Cosmet Dermatol. 2020;19(11):3067–76. https://doi.org/10.1111/jocd.13346.
Caddeo C, Manca ML, Peris JE, Usach I, Diez-Sales O, Matos M, et al. Tocopherol-loaded transfersomes: in vitro antioxidant activity and efficacy in skin regeneration. Int J Pharm. 2018;551(1–2):34–41. https://doi.org/10.1016/j.ijpharm.2018.09.009.
Palipoch S, Punsawad C, Koomhin P, Suwannalert P. Hepatoprotective effect of curcumin and alpha-tocopherol against cisplatin-induced oxidative stress. BMC Complement Altern Med. 2014;14:111. https://doi.org/10.1186/1472-6882-14-111.
Beach RS, Mantero-Atienza E, Shor-Posner G, Javier JJ, Szapocznik J, Morgan R, et al. Specific nutrient abnormalities in asymptomatic HIV-1 infection. AIDS. 1992;6(7):701–8. https://doi.org/10.1097/00002030-199207000-00013.
Tang AM, Graham NM, Semba RD, Saah AJ. Association between serum vitamin A and E levels and HIV-1 disease progression. AIDS. 1997;11(5):613–20. https://doi.org/10.1097/00002030-199705000-00009.
Acknowledgements
The authors thank the Department of Pharmaceutics and Pharmacology of MCOPS, MAHE, Manipal, Karnataka, India, for providing facilities to conduct the study.
Funding
The ICMR, New Delhi, India, provided a Senior Research Fellowship (SRF) to authors Mr. Srinivas Reddy Jitta, Ms. Navya Ajitkumar Bhaskaran, and Ms. Sri Pragnya Cheruku, and the AICTE, New Delhi, India, provided National Doctoral Fellowship (NDF) to Ms. Salwa.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Srinivas Reddy Jitta, Salwa, Navya Ajitkumar Bhaskaran, Shirleen Miriam Marques, Lalit Kumar, SriPragnya Cheruku, Vanishree Rao, Pravesh Sharma, Onkar Kulkarni. The first draft of the manuscript was written by Srinivas Reddy Jitta and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Srinivas Reddy Jitta: methodology; formal analysis; data acquisition; original draft. Salwa: methodology; formal analysis; data acquisition. Navya Ajitkumar Bhaskaran: methodology; formal analysis; data acquisition. Shirleen Miriam Marques: formal analysis; data acquisition. Dr Lalit Kumar: conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; supervision; validation; visualization; roles/writing-original draft; writing—review and editing. Sri Pragnya Cheruku: formal analysis; data acquisition. Vanishree Rao: formal analysis; data acquisition. Pravesh Sharma: formal analysis; data acquisition. Onkar Prakash Kulkarni: formal analysis; data acquisition.
Corresponding author
Ethics declarations
Ethics approval
All animal studies were conducted with prior approval from the Institutional animal ethical committee (approval No. IAEC/KMC/51/2018 and IAEC/KMC/72/2021).
Animal studies
All institutional and national guidelines for the care and use of laboratory animals were followed.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jitta, S.R., Salwa, Bhaskaran, N.A. et al. Enhanced tissue distribution of ritonavir-loaded nanostructured lipid carriers—recommending its dose reduction. Drug Deliv. and Transl. Res. 14, 116–130 (2024). https://doi.org/10.1007/s13346-023-01386-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-023-01386-9