Abstract
Background
Multiple magnet ingestion is increasingly reported in paediatrics and can cause significant morbidity. Various surgical approaches exist, though minimal literature compares outcomes between techniques. This review evaluates laparoscopic, laparoscopic-assisted, and open surgery with regard to outcomes.
Method
Systematic review across MEDLINE, Embase, Scopus, and Web of Science identified reports of paediatric multiple magnet ingestion managed surgically between 2002 and 2022.
Results
Ninety-nine studies were included, reporting data from 136 cases. Of these, 82 (60%) underwent laparotomy, 43 (32%) laparoscopic surgery, and 11 (8%) laparoscopic-assisted procedures. Sixteen laparoscopic cases were converted to open, often due to intraoperative findings including necrosis/perforation, or grossly dilated bowel. Bowel perforation occurred in 108 (79%); 47 (35%) required bowel resection, and 3 had temporary stoma formation. Postoperative recovery was uneventful in 118 (86%). Complications were reported following 15 (18%) open and 3 (7%) laparoscopic surgeries. No complications occurred following laparoscopic-assisted surgery. All post-laparoscopic complications were Clavien-Dindo (CD) Grade I. Following open surgery, 5 complications were CD grade I, 6 were CD grade II, and 4 were CD grade IIIb, requiring re-laparotomy. Median length of stay for open and laparoscopic-assisted procedures was 7 days, and for laparoscopic was 5 days (p < 0.001).
Conclusion
Surgical management of multiple magnet ingestion often achieved uncomplicated recovery and no long-term sequelae. Whilst open laparotomy was the more common approach, laparoscopic surgery was associated with reduced length of stay and postoperative complications. Therefore, in experienced hands, laparoscopic surgery should be considered first-line, with the possibility of conversion to open if required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Incidence of multiple magnet ingestion in the paediatric population has increased drastically over the past few decades and is associated with high morbidity and potentially fatal outcomes [1,2,3]. While ingestion of a single magnet is unlikely to cause significant harm, attractive forces between multiple magnets within the digestive tract can result in necrosis, perforations, fistulas and bowel obstruction [1].
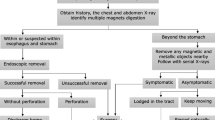
A number of algorithms have been developed to determine the optimal approach to diagnosis and management of multiple magnet ingestion. In 2012, following a survey that highlighted a more prevalent and hazardous problem than previously appreciated, the North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) developed a comprehensive algorithm that aimed to more clearly define the roles of paediatric gastroenterologists and endoscopy [2]. While more detailed than previous algorithms, the role of surgical management, and optimal surgical approach, remained somewhat unclear.
Laparoscopic and open surgical approaches have been extensively compared and evaluated outside of the context of multiple magnet ingestion with key advantages of laparoscopic procedures reported as reduced blood loss, postoperative pain, wound infections, length of stay, and recovery time [4,5,6].
There is, however, minimal literature comparing outcomes between these surgical approaches in the management of multiple magnet ingestion in the paediatric population. The aim of this study was to analyse and compare outcomes for laparoscopic, laparoscopic-assisted, and open-surgical approaches in multiple magnet ingestion with a focus on morbidity, perforation, and postoperative outcomes to determine the optimal approach to operative management.
Methods
Systematic search across MEDLINE, EMBASE, Scopus, and Web of Science was conducted in September 2023 using the search terms ‘multiple magnet’, ‘ingestion’, and ‘surgical’. Truncation and wildcards were applied to synonyms to include all relevant papers; synonyms were pooled with ‘OR’; ‘AND’ was used to combine search terms. An abstract screen was conducted, followed by a full-text screen.
Inclusion criteria were: (a) reports of cases of multiple magnet ingestion managed surgically in patients under 18 years of age, (b) published between the years 2002 and 2022, and (c) published in English. Exclusion criteria were: (a) unclear or incomplete case/cohort documentation such that either the operative approach or the number, age, and sex of patients could not be defined and (b) unavailability of full text.
Data was collected for age, sex, comorbidities, magnet type/size/location, preoperative management/imaging, length of time from ingestion to surgery, surgical approach, conversions, sepsis, perforation, follow-up, morbidity and mortality. The study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement 2020 (Fig. 1). The systematic review protocol was registered at the International Prospective Register of Systematic Reviews (PROSPERO) registration number CRD42023461706.
Results
The literature search revealed 410 articles, of which 174 reported surgical management of multiple magnet ingestion in paediatric patients, and 99 met the inclusion criteria.
A total of 136 children were analysed, of which 91 (67%) were male. Age ranged from 9 months to 17 years with a median age of 4 years (IQR 2–8 years). There were 14 children with relevant physical or psychiatric comorbidities including autism spectrum disorder (ASD) (n = 4), attention deficit hyperactivity disorder (ADHD) (n = 3), pica (n = 2), developmental delay (n = 4), adjustment disorder (n = 1), and Fragile X (n = 1).
The most frequently reported symptoms included abdominal pain (n = 98, 72%), vomiting (n = 83, 61%), constipation (n = 14, 10%), fever (n = 14, 10%), abdominal distension (n = 13, 10%), and diarrhoea (n = 7, 5%). Bowel obstruction was reported in 27 (20%), peritonitis was reported in 22 (16%), and 1 child was septic on admission. Asymptomatic presentation was reported in 19 (14%).
The most common type of magnets ingested included balls/beads (n = 76, 56%), rods (n = 18, 13%), discs (n = 18, 13%), and ‘rattle’/’singing’ magnets (n = 9, 7%). Magnet type was unspecified in 22 (16%). Median number of magnets ingested was 5 (IQR 2–12). The maximum number of magnets ingested was 70. The number of magnets ingested was not specified for 9 cases (7%). Most ingestions were unwitnessed (n = 102, 75%).
Surgical management was entirely open in 82 (60%) (laparotomy n = 81 [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69], mini-laparotomy n = 1 [70]). In 43 (32%) the procedures began laparoscopically, of which 27 were entirely laparoscopic [7, 8, 66, 67, 69, 71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87] and 16 (37%) were converted to open (laparotomy n = 12 [68, 88,89,90,91,92,93,94,95,96,97], mini-laparotomy n = 4 [66, 98]). Reasons for conversion to open were: (a) to achieve removal of all magnets (n = 5) [66, 96,97,98]; (b) concern of free perforation through multiple loops of bowel (n = 1) [90]; (c) magnets sticking to the camera rod and obstructing vision (n = 1) [68]; (d) unclear aetiology of small bowel obstruction (n = 1) [92]; (e) intraoperative findings including necrosis and/or perforations (n = 4) [89, 93, 94, 98], grossly dilated small bowel (n = 2) [68, 88], impending gastroceacal fistula (n = 1) [95], and dense matted small bowel (n = 1) [91]. Laparoscopic-assisted surgery was performed in 11 (8%) [82, 83, 93, 98,99,100,101,102,103], with removal achieved most often through extension of the umbilical port site incision.
Table 1 describes a breakdown of case characteristics by surgical approach. Sex, age, number of magnets, witnessed ingestions, and time from ingestion to surgical intervention (reported in 60 cases) were similar across groups.
Figure 2 depicts the increase in case reports of multiple magnet ingestion requiring surgical management over the past two decades broken down by surgical approach.
Magnets were located in the small bowel in 115 (85%), large bowel in 44 (32%), and stomach in 27 (20%). The most common intestinal sites specified included the ileum (n = 56, 41%), jejunum (n = 32, 24%), and cecum (n = 21, 15%). Magnets were either partially or completely extraluminal in 9 (7%) and were removed from the appendix via appendectomy in 4 (3%) (magnets located in appendix n = 2; magnets milked to the appendix for removal n = 2).
Table 2 describes patient outcomes broken down by surgical approach.
Bowel perforations and/or fistulas were reported in 108 (79%) (69/82 open procedures (84%), 30/43 laparoscopic procedures (70%) (17/27 entirely laparoscopic (63%), 13/16 laparoscopic converted to open (81%)), and 9/11 laparoscopic assisted procedures (82%). Multiple perforations were reported in 96 (71%). Perforation of the small bowel was reported in 94 (69%), large bowel in 36 (26%) and stomach in 19 (14%). The most common sites of perforation specified included the ileum (n = 52, 38%), jejunum (n = 32, 24%), and cecum (n = 20, 15%). Bowel necrosis without perforation was reported in 10 (7%) and volvulus occurred in 6 (4%).
Bowel resection was required in 47 (35%) (34/82 open procedures (41%), 10/43 laparoscopic procedures (23%) (6/27 entirely laparoscopic (22%), 4/16 laparoscopic converted to open (25%)), and 3/11 laparoscopic-assisted procedures (27%). 3 patients (2%) required temporary stoma formation (all of whom underwent entirely open procedures) of which one was reversed at postoperative day 21, one planned for reversal at 6 months, and one planned for reversal at an unspecified timepoint.
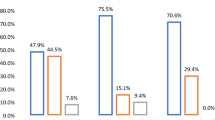
Postoperative recovery was uncomplicated in 118 cases (86%): 67/82 open procedures (82%), 40/43 laparoscopic procedures (93%) (24/27 entirely laparoscopic (89%), 16/16 laparoscopic converted to open (100%)), and 11/11 laparoscopic-assisted procedures (100%).
Complications occurred in 18 cases. Of these, 8 (44%) were Clavien Dindo classification (CD) grade I including: ileus (n = 5), bowel obstruction (n = 1), wound infection (n = 1), wound infection and bowel obstruction (n = 1). Complications were CD grade II in 6 cases including: abdominal abscesses requiring interventional radiology (IR) drainage (n = 2), wound infection with dehiscence requiring vacuum dressing (n = 1), prolonged ileus requiring total parenteral nutrition (TPN) (n = 1), high output jejunostomy requiring TPN (n = 1), and prolonged antibiotic treatment for peritonitis (n = 1). Complications were CD grade IIIb in 4 cases including wound infection requiring re-laparotomy (n = 2), bowel obstruction requiring resection and adhesiolysis (n = 1), and missed fistula causing bowel obstruction requiring re-laparotomy (n = 1). No lethal outcomes were reported following surgical management.
Of the 27 laparoscopic cases, 3 (11%) had postoperative complications (all CD grade I). Of the 82 open cases, 15 (18%) had postoperative complications (CD grade I: n = 5, CD grade 2: n = 6, CD grade 3b: n = 4). No complications were reported following procedures that began laparoscopically and were converted to open or following laparoscopic-assisted procedures.
Postoperative length of stay (LOS) was reported in 99 cases. Median LOS was 7 days (IQR 5–8). For entirely open procedures, median LOS was 7 days (IQR 5.75–9.25), for laparoscopic procedures median LOS was 5 days (IQR 3–7) (p < 0.001). For laparoscopic-assisted procedures, median LOS was 7 days (IQR 4–8).
Discussion
The results of this study demonstrate favourable outcomes following surgical management of multiple magnet ingestion in the paediatric population with a majority of patients reported to have uncomplicated postoperative recovery with no long-term sequelae. In line with previous reviews [2, 104, 105], the incidence of multiple magnet ingestion increased over time and the majority of patients (60%) underwent open surgery while laparoscopic procedures accounted for 32%, and laparoscopic-assisted 8%.
The majority of patients (79%) suffered perforation as a result of multiple magnet ingestion and 35% required bowel resection. Only 3 patients required stoma formation, all of which were planned for reversal.
The results of this analysis demonstrate an entirely laparoscopic approach to be favourable in this patient population, as it is associated with a shorter length of stay and reduced incidence and severity of postoperative complications when compared to open procedures. All complications that occurred following laparoscopic procedures were CD grade I, while following open procedures, 40% of complications were CD grade II and 27% were CD grade IIIb requiring re-laparotomy.
A previous case series of eight children who ingested powerful rare-earth magnets reported the successful use of endoscopy (n = 3), colonoscopy (n = 1), and laparoscopy (n = 4) with no requirement for open procedures [85]. Likewise, Wooten et al. reported a case where laparoscopy proved both diagnostic and therapeutic for malrotation with associated fistula and volvulus following ingestion of multiple magnets [95].
Opposing literature has recommended an open approach, proposing laparoscopic removal to be more challenging in cases of magnet ingestion owing to the magnets adhering to the instruments [106, 107]. The results of this study however demonstrate the majority of laparoscopic procedures to be successful, with only one occasion in which the magnets stuck to the camera rod and obstructed vision [68]. In this case, conversion to open surgery was successful in retrieving the magnets and the patient was discharged after seven days with no complications noted over four months of outpatient follow-up. These conclusions are in line with previous studies that lend favour to laparoscopic procedures as a first-line surgical treatment for magnetic foreign body ingestion [108,109,110].
Laparoscopic procedures however are not without limitation, and laparoscopic-assisted surgery has been proposed to offer a potential balance between the improved postoperative outcomes associated with minimally invasive techniques and the longer operating times, steep learning curve, and high costs that present barriers to the implementation of such techniques in clinical practice [111]. The earliest report of laparoscopic assisted management included in this review was published in 2012 and the low number of cases available for analysis limits the ability to draw definitive conclusions as to its associated outcomes. Despite this, it can be noted that of the 11 patients who underwent laparoscopic-assisted procedures, none suffered postoperative complications and no conversions to open laparotomy were reported, lending support to this approach as a potentially favourable surgical option, though further analysis of larger cohorts is undoubtedly required.
When determining the optimal surgical approach, it is well recognised that consideration should be given, not only to previously associated outcomes and individual patient factors, but also to the operating surgeon’s preferred technique and relevant expertise, which play vital roles in such matters [112].
Conclusion
The incidence of multiple magnet ingestion requiring surgical intervention has increased over the past two decades, though consensus on the optimal approach is yet to be reached and requires ongoing review of associated outcomes. Whilst the majority of cases thus far have been managed through open laparotomy, this review demonstrates a laparoscopic approach to be both feasible and potentially advantageous, associated with shorter length of stay and reduced postoperative complications. Therefore, in experienced hands, laparoscopic surgery should be considered as first-line management in this population, with the possibility of conversion to open surgery if required.
Data availability
All data underlying the results are included in this article as references to published articles, or are available from the corresponding authors on reasonable request.
References
Hodges NL, Denny SA, Smith GA (2017) Rare-Earth Magnet Ingestion-Related Injuries in the Pediatric Population: A Review. Am J Lifestyle Med 11(3):259. https://doi.org/10.1177/1559827615594336
Hussain SZ, Bousvaros A, Gilger M, et al (2012) Management of ingested magnets in children. J Pediatr Gastroenterol Nutr 55(3):239–242. https://doi.org/10.1097/MPG.0B013E3182687BE0
Strickland M, Rosenfield D, Fecteau A (2014) Magnetic foreign body injuries: a large pediatric hospital experience. J Pediatr 165(2):332–335. https://doi.org/10.1016/J.JPEDS.2014.04.002
Jaschinski T, Mosch CG, Eikermann M, Neugebauer EAM, Sauerland S (2018) Laparoscopic versus open surgery for suspected appendicitis’. Cochr Database Syst Rev. https://doi.org/10.1002/14651858.CD001546.PUB4/MEDIA/CDSR/CD001546/IMAGE_N/NCD001546-CMP-004-04.PNG
Laudicella M, Walsh B, Munasinghe A, Faiz O (2016) Impact of laparoscopic versus open surgery on hospital costs for colon cancer: a population-based retrospective cohort study. BMJ Open 6(11):e012977. https://doi.org/10.1136/BMJOPEN-2016-012977
Velanovich V (2000) Laparoscopic vs open surgery: a preliminary comparison of quality-of-life outcomes. Surg Endosc 14(1):16–21. https://doi.org/10.1007/S004649900003
Lin A, Chan LCN, Hon KLE, et al (2019) Magnetic Foreign Body Ingestion in Children: The Attractive Hazards. Case Rep Pediatr 2019:1–4. https://doi.org/10.1155/2019/3549242
Tavarez MM, Saladino RA, Gaines BA, Manole MD (2013) Prevalence, clinical features and management of pediatric magnetic foreign body ingestions. J Emerg Med 44(1):261–268. https://doi.org/10.1016/J.JEMERMED.2012.03.025
Abuzneid YS, Alzeerelhouseini HIA, Rabee A, et al (2022) Double Magnet Ingestion Causing Intestinal Perforation with Peritonitis: Case Report and Review of the Literature. Case Rep Surg 2022:1–4. https://doi.org/10.1155/2022/4348787
Adu-Frimpong J, Sorrell J (2009) Magnetic toys: the emerging problem in pediatric ingestions. Pediatr Emerg Care 25(1):42–43. https://doi.org/10.1097/PEC.0B013E318191DBB1
Ahmed AM, Hassab MH, Al-Hussaini AA, Al-Tokhais TI (2010) Magnetic toy ingestion leading to jejunocecal fistula in a child. Saudi Med J 31(4):442–444
Alkhamisy A (2021) Gastrojejunal fistula caused by magnet beads ingestion in a 2 -year-old boy. J Pediatr Surg Case Rep. https://doi.org/10.1016/J.EPSC.2021.101809
Alzahem AM, Soundappan SSV, Jefferies H, Cass DT (2007) Ingested magnets and gastrointestinal complications. J Paediatr Child Health 43(6):497–498. https://doi.org/10.1111/J.1440-1754.2007.01121.X
Hernández Anselmi E, Gutiérrez San Román C, Barrios Fontoba JE, et al (2007) Intestinal perforation caused by magnetic toys. J Pediatr Surg 42(3):e13–e16. https://doi.org/10.1016/J.JPEDSURG.2006.12.066
Arslan S, Basuguy E, Zeytun H, Okur MH, Aydogdu B, Arslan MS (2015) Jejunoileal perforation and volvulus caused by multiple magnet ingestion. Acta Clin Croat 54(1):96–98
Baines H, Saenz NC, Dory C, Marchese SM, Bernard-Stover L (2012) Magnet-associated intestinal perforation results in a new institutional policy of ferromagnetic screening prior to MRI. Pediatr Radiol 42(12):1506–1509. https://doi.org/10.1007/S00247-012-2441-Z
Blevrakis E, Raissaki M, Xenaki S, Astyrakaki E, Kholcheva N, Chrysos E (2018) Multiple magnet ingestion causing instestinal obstruction and entero-enteric fistula: Which imaging modality besides radiographs? A case report. Ann Med Surg 31:29. https://doi.org/10.1016/J.AMSU.2018.04.033
Butterworth J, Feltis B (2007) Toy magnet ingestion in children: revising the algorithm’. J Pediatr Surg. https://doi.org/10.1016/J.JPEDSURG.2007.09.001
Cauchi JA, Shawis RN (2002) Multiple magnet ingestion and gastrointestinal morbidity. Arch Dis Child 87(6):539–540. https://doi.org/10.1136/ADC.87.6.539
Cherchi V, Adani GL, Righi E, et al (2018) Ileocecal Fistula Caused by Multiple Foreign Magnetic Bodies Ingestion. Case Rep Surg 2018:1–3. https://doi.org/10.1155/2018/7291539
Cho J, Sung K, Lee D (2017) Magnetic foreign body ingestion in pediatric patients: Report of three cases. BMC Surg 17(1):1–6. https://doi.org/10.1186/S12893-017-0269-Z/FIGURES/8
Clarke R, Everett T, Watts A, Qureshi T (2010) Reminder of important clinical lesson: The magnetism of surgery: small bowel obstruction in an 8-year-old boy’. BMJ Case Rep. https://doi.org/10.1136/BCR.01.2010.2667
Corduk N, Odabas S, Sarioglu-Buke A (2014) Intestinal perforation caused by multiple magnet ingestion. Afr J Paediatr Surg 11(1):84–86. https://doi.org/10.4103/0189-6725.129249
Zubarew T, Jama S, Gutiérrez J (2017) Abdominal pain secondary to ileocecal fistulae by ingestion of multiple magnetic bodies: Clinical Case. Rev Chil Pediatr 88(3):553–560. https://doi.org/10.4067/S0370-41062017000300018
Fenton SJ, Torgenson M, Holsti M, Black RE (2007) Magnetic attraction leading to a small bowel obstruction in a child. Pediatr Surg Int 23(12):1245–1247. https://doi.org/10.1007/S00383-007-1997-4
Gün F, Günendi T, Kiliç B, Çelik A (2013) Multiple magnet ingestion resulting in small bowel perforation: a case report. Ulus Travma Acil Cerrahi Derg 19(2):177–179. https://doi.org/10.5505/TJTES.2013.26779
Holtz TK, Greisen PW, Qvist N, Bjørn N (2020) Unexpected finding of ingested magnetic toys in a child undergoing cerebral MRI. J Pediatr Surg Case Rep 61:101579. https://doi.org/10.1016/J.EPSC.2020.101579
Ilçe Z, Samsum H, Mammadov E, Celayir S (2007) Intestinal volvulus and perforation caused by multiple magnet ingestion: report of a case. Surg Today 37(1):50–52. https://doi.org/10.1007/S00595-006-3330-6
Jain N, Mitra A, Ratan SK, Panda SS (2022) “Necklace of magnets” in the abdomen: an unusual case with “multiple” bowel perforations. Med J Armed Forces India. https://doi.org/10.1016/J.MJAFI.2022.09.015
Kathayat LB, Chalise A, Maharjan JS, Bajracharya J, Shrestha R (2022) Intestinal Perforation with Ingestion of Blunt Foreign Bodies: A Case Report. JNMA J Nepal Med Assoc 60(253):817. https://doi.org/10.31729/JNMA.7650
Kim Y, Hong J, Moon SB (2014) Ingestion of multiple magnets: The count does matter. J Pediatr Surg Case Rep 2(3):130–132. https://doi.org/10.1016/J.EPSC.2014.02.013
Kircher MF, Milla S, Callahan MJ (2007) Ingestion of magnetic foreign bodies causing multiple bowel perforations. Pediatr Radiol 37(9):933–936. https://doi.org/10.1007/S00247-007-0542-X
Lee BK, Ryu HH, Moon JM, Jeung KW (2010) Bowel perforations induced by multiple magnet ingestion. Emerg Med Australas 22(2):189–191. https://doi.org/10.1111/J.1742-6723.2010.01276.X
Lindley S, Pathak S, Mulchandani M, Dalton S, Sutton R (2012) Magnetic Meckel’s: an unusual case report of foreign body ingestion. J Surg Case Rep 2012(3):7. https://doi.org/10.1093/JSCR/2012.3.7
Mirza MB, Bux N, Talat N, Saleem M (2015) Multiple singing magnet ingestion leading to pressure necrosis of the small bowel. J Indian Assoc Pediatr Surg 20(2):90. https://doi.org/10.4103/0971-9261.151557
Miyamoto R, Okuda M, Kaneko K, Numoto S, Okumura A (2019) Multiple Magnets Ingestion Followed by Intestinal Fistula With Mild Symptoms. Glob Pediatr Health 6:1–4. https://doi.org/10.1177/2333794X19855805
Munghate GS, Reddy AS, Bodhanwala M (2020) Multiple magnetic foreign bodies causing complex intestinal fistula. J Pediatr Surg Case Rep. https://doi.org/10.1016/J.EPSC.2020.101661
Nagaraj HS, Sunil I (2005) Multiple foreign body ingestion and ileal perforation. Pediatr Surg Int 21(9):718–720. https://doi.org/10.1007/S00383-005-1422-9
Nui A, Hirama T, Katsuramaki T, et al (2005) An intestinal volvulus caused by multiple magnet ingestion: an unexpected risk in children. J Pediatr Surg 40(9):e9–11. https://doi.org/10.1016/j.jpedsurg.2005.05.065
Pogorelić Z, Borić M, Markić J, Jukić M, Grandić L (2016) A Case of 2-Year-Old Child with Entero-Enteric Fistula Following Ingestion of 25 Magnets. Acta Medica (Hradec Kralove) 59(4):140–142. https://doi.org/10.14712/18059694.2017.42
Robinson AJ, Bingham J, Thompson RLE (2009) Magnet induced perforated appendicitis and ileo-caecal fistula formation’. Ulster Med J 78:1–4
Saeed A, Johal NS, Aslam A, Brain J, Fitzgerald RJ (2009) Attraction Problems Following Magnet Ingestion. Ann R Coll Surg Engl 91(5):W10. https://doi.org/10.1308/147870809X450566
Sahin C, Alver D, Gulcin N, Kurt G, Celayir AC (2010) A rare cause of intestinal perforation: ingestion of magnet. World J Pediatr 6(4):369–371. https://doi.org/10.1007/S12519-010-0237-5
Salimi A, Kooraki S, Esfahani SA, Mehdizadeh M (2012) Multiple magnet ingestion: Is there a role for early surgical intervention? Ann Saudi Med 32(1):93. https://doi.org/10.5144/0256-4947.2012.93
Sekmenli T, Ciftci I (2016) Multiple Intestinal Perforation and Necrosis due to Magnet Ingestion. Eurasian J Med 48(3):225. https://doi.org/10.5152/EURASIANJMED.2015.0080
Shalaby MS (2015) How dangerous a toy can be? The magnetic effect. Arch Dis Child 100(11):1049–1050. https://doi.org/10.1136/ARCHDISCHILD-2014-307756
Si X, Du B, Huang L (2016) Multiple Magnetic Foreign Bodies Causing Severe Digestive Tract Injuries in a Child. Case Rep Gastroenterol 10(3):720. https://doi.org/10.1159/000450538
Soomro S, Mughal SA (2014) Singing magnets ingestion: a rare cause of intestinal obstruction in children. J Coll Physicians Surg Pak 24(9):688–689
Stephenson SG, Knight CT, Rana HN, Standley T, Figarola S (2022) An Unfortunate Union: A Case of Multiple Magnet Ingestion in a Pediatric Patient’. Cureus. https://doi.org/10.7759/CUREUS.21490
Surd A, Aldea C, Mironescu A, Gocan H (2018) Transmesocolic double gastro-enteric fistulas due to ingestion of 28 magnets. J Pediatr Surg Case Rep 32:85–86. https://doi.org/10.1016/J.EPSC.2018.02.007
Taher H, Azzam A, Khowailed O, Elseoudi M, Shaban M, Eltagy G (2019) A case report of an asymptomatic male child with multiple entero-enteric fistulae post multiple magnet ingestion. Int J Surg Case Rep 58:50. https://doi.org/10.1016/J.IJSCR.2019.03.043
Teague WJ, Vaughan EM, McHoney M, McCabe AJ (2013) Case Report: Swallowed magnets and batteries: a dangerous but not unexpected attraction’. BMJ Case Rep. https://doi.org/10.1136/BCR-2013-009073
Uchida K, Otake K, Iwata T, et al (2006) Ingestion of multiple magnets: hazardous foreign bodies for children. Pediatr Radiol 36(3):263–264. https://doi.org/10.1007/S00247-005-0056-3
Van Biervliet S, Van de Putte D, De Jaegher A, et al (2012) Multiple magnet ingestion: a real challenge for the paediatric surgeon. Acta Clin Belg 67(4):298–300. https://doi.org/10.2143/ACB.67.4.2062677
Verma S, Shinde SR, Gupta C (2013) Multiple magnet ingestion: An uncommon cause of peritonitis. J Indian Assoc Pediatr Surg 18(4):160. https://doi.org/10.4103/0971-9261.121126
Wildhaber BE, Le Coultre C, Genin B (2005) Ingestion of magnets: innocent in solitude, harmful in groups’. J Pediatr Surg. https://doi.org/10.1016/J.JPEDSURG.2005.06.022
Zachos K, Panagidis A, Georgiou G, Alexopoulos V, Sinopidis X (2019) Double Jejunoileal Fistula after Ingestion of Magnets. J Indian Assoc Pediatr Surg 24(1):63. https://doi.org/10.4103/JIAPS.JIAPS_92_18
Zgraj O, Awadalla S (2015) Accidental ingestion of magnetic spheres in children. Ir Med J 108(5):149–150
Bin Zhang Y, Gao ZG, Xiong QX, Zhang LF, Te Cai D, Bin Cai J (2017) Clinical experience in the treatment of children who swallowed multiple magnetic foreign bodies: A report of five cases’. World J Pediatr. https://doi.org/10.1007/S12519-016-0083-1
Ali A, Alhindi S (2020) A Child With a Gastrocolic Fistula After Ingesting Magnets: An Unusual Complication’. Cureus. https://doi.org/10.7759/CUREUS.9336
Brown JC, Murray KF, Javid PJ (2012) Hidden attraction: a menacing meal of magnets and batteries. J Emerg Med 43(2):266–269. https://doi.org/10.1016/J.JEMERMED.2011.09.003
Karjoo M, Dragnich A, Karjoo S, Warsi QA (2017) Save the Children from Gastric and Intestinal Perforation Secondary to Small Magnet Ingestion by Educating Families with the Help of Pediatricians. Int J Pediatr 5(3):4449–4455. https://doi.org/10.22038/IJP.2017.8263
Kattih O, Almoosa ZA, Alibraheem A (2022) Contained Jejunal Perforation Secondary to Ingestion of Magnet Balls in a Nonfatal Drowning Child’. Cureus. https://doi.org/10.7759/CUREUS.29741
Moussa A, Gouda M, Jallouli M (2022) Unnoticed ingestion of magnetic balls mimics acute appendicitis. J Pediatr Surg Case Rep. https://doi.org/10.1016/J.EPSC.2022.102424
Othman MY, Srihari S (2016) Multiple magnet ingestion: The attractive hazardst. Med J Malaysia 71(4):211–212
Han Y, Youn JK, Oh C, Lee S, Seo JM, Kim HY (2020) Ingestion of multiple magnets in children. J Pediatr Surg 55(10):2201–2205. https://doi.org/10.1016/J.JPEDSURG.2019.11.021
Lemoine A, Mamann N, Larroquet M, Tounian P, Irtan S, Lemale J (2019) Ingestion of neodymium magnet spheres: Three case studies. Arch Pediatr 26(3):179–181. https://doi.org/10.1016/J.ARCPED.2019.02.001
Al-Saied G, Alsamay O, Ibrahim M, et al (2022) Enteroenteric fistulae after ingestion of multiple magnets in children. J Pediatr Surg Case Rep 76:102090. https://doi.org/10.1016/J.EPSC.2021.102090
Seguier-Lipszyc E, Samuk I, Almog A, Silbermintz A, Kravarusic D (2022) Multiple magnet ingestion in children: A problem on the rise. J Paediatr Child Health 58(10):1824–1828. https://doi.org/10.1111/JPC.16117
Bucci C, Ferrara D, Quitadamo P, et al (2022) Value of intestinal ultrasound in pediatric magnet ingestion: a case report. J Ultrasound 25(4):861–864. https://doi.org/10.1007/S40477-021-00631-6
Birkhold M, Habib JR, Kang J, Diaz-Calderon L, Lumpkins K, Strauch E (2022) Magnetic Appendix: An Uncommon Indication for Appendectomy’. Cureus. https://doi.org/10.7759/CUREUS.31096
Centers for Disease Control and Prevention (CDC), ‘Gastrointestinal Injuries from Magnet Ingestion in Children --- United States, 2003--2006’. Accessed: Oct. 15, 2023. [Online]. Available: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5548a3.htm
Dotlacil V, Frybova B, Vyhnanek M, Zeman L, Rygl M (2020) Removal of Ingested Magnetic Bodies via Laparoscopic Appendectomy. European J Pediatr Surg Rep. https://doi.org/10.1055/S-0040-1714669
Dutta S, Barzin A (2008) Multiple magnet ingestion as a source of severe gastrointestinal complications requiring surgical intervention. Arch Pediatr Adolesc Med 162(2):123–125. https://doi.org/10.1001/ARCHPEDIATRICS.2007.35
Grosshauser M, Ohletz T, Oesch V, Muller CO (2022) Tips and Tricks-3 Use Cases of Interdisciplinary Knowledge Transfer in Minimally Invasive Pediatric Surgery. Children (Basel). https://doi.org/10.3390/CHILDREN9091270
Macedo M, Velhote MCP, Maschietto RF, Waksman RD (2013) Intestinal fistula after magnets ingestion. Einstein 11(2):234. https://doi.org/10.1590/S1679-45082013000200018
Nicoara M, Liu S, Ferzli G (2018) Laws of attraction: management of magnetic foreign body ingestion. BMJ Case Rep. https://doi.org/10.1136/BCR-2018-225939
Pak SM, Lee YJ, Hwang JY (2022) Diagnosis of Nonmigrating Metallic Foreign Bodies in the Abdomen Using Ultrasound: An Alternative Approach Using a Traditional Method. Pediatr Gastroenterol Hepatol Nutr 25(1):87. https://doi.org/10.5223/PGHN.2022.25.1.87
Pederiva F, Daniela C, Scarpa M-G, Guida E, Dragovic D, Martelossi S (2014) An Asymptomatic Multiple Magnet Ingestion with Transmesenteric Entero-Enteric Fistula. APSP J Case Rep 5(2):16
Sanchez D, Prada A, Martinez C, Herrera N, Ortiz C, Mosquera-Klinger G (2022) Multiple magnet ingestion in paediatrics, high risk of complications and surgery interventions. J Pediatr Gastroenterol Nutr. https://doi.org/10.1097/MPG.0000000000003446
S. Scholz and D. Stewart (2011) The underestimated danger of multiple magnet ingestion: Case report, literature review and clinical algorithm.’, in 40th International Symposium Pediatric Surgery, E. Horcher and W. Krois, Eds., Springer Wien
Naji H, Isacson D, Svensson JF, Wester T (2012) Bowel injuries caused by ingestion of multiple magnets in children: a growing hazard. Pediatr Surg Int 28(4):367–374. https://doi.org/10.1007/S00383-011-3026-X
Afzal M, Almakki AA, Abugrain HH, Alsaeed MM, Alzahir BS, Sulis NA (2022) Laparoscopic assisted extraction of multiple ingested magnets leading to entero-enteric fistulae- Case report of three patients. J Pediatr Surg Case Rep. https://doi.org/10.1016/J.EPSC.2022.102357
Hao J, Feng Y, Huang X (2021) A foreign body causing a spontaneous gastrojejunostomy in a young child. Natl Med J India 34(1):27–28. https://doi.org/10.4103/0970-258X.323444
Kosut JS, Johnson SM, King JL, Garnett G, Woo RK (2013) Successful treatment of rare-earth magnet ingestion via minimally invasive techniques: a case series. J Laparoendosc Adv Surg Tech A 23(4):405–408. https://doi.org/10.1089/LAP.2012.0461
Oh RG, Lee CG, Park YN, Lee YM (2021) Successful removal of two magnets in the small intestine by laparoscopy and colonoscopy: A case report. World J Clin Cases 9(27):8226. https://doi.org/10.12998/WJCC.V9.I27.8226
Palanivelu C, Rangarajan M, Rajapandian S, Vittal SK, Maheshkumaar GS (2007) Laparoscopic retrieval of “stubborn” foreign bodies in the foregut: a case report and literature survey. Surg Laparosc Endosc Percutan Tech 17(6):528–531. https://doi.org/10.1097/SLE.0B013E31815AC599
Adikibi BT, Arnold M, Van Niekerk G, Alexander A, Numanoglu A, Millar AJW (2013) Magnetic bead toy ingestion: uses and disuses in children. Pediatr Surg Int 29(7):741–744. https://doi.org/10.1007/S00383-013-3275-Y
Ghallab A, Wilkson A, Daniel R (2022) Undisclosed Multiple Magnet Ingestion Simulating Appendicular Mass in a 5-Year-Old Girl—a Case Report and Review of Literature. SN Compreh Clin Med. https://doi.org/10.1007/S42399-022-01152-X
Mercurio DC, Scace C, Shah B, Weiner E, Prasad R (2018) Abdominal Pain Caused by a Potentially Fatal Attraction. Pediatr Emerg Care 34(11):e211–e213. https://doi.org/10.1097/PEC.0000000000000954
Morulana TG, Tshifularo N, Ngwenya TR, Motloung E (2021) Small bowel fistula caused by ingested magnetic beads. J Pediatr Surg Case Rep. https://doi.org/10.1016/J.EPSC.2021.101899
Munipalle PC, Luther A, Blake S, Burt C (2014) Takes two to tango. BMJ Case Rep. https://doi.org/10.1136/BCR-2013-202794
Strickland M, Diamond IR, Rosenfield D (2020) Case Discussions and Radiographic Illustration of Magnet-Related Injuries in Children. J Emerg Med 58(6):902–909. https://doi.org/10.1016/J.JEMERMED.2020.03.022
Wong HHL, Phillips BA (2009) Opposites attract: a case of magnet ingestion. CJEM 11(5):493–495. https://doi.org/10.1017/S1481803500011696
Wooten KE, Hartin CW, Ozgediz DE (2012) Laparoscopic Diagnosis of Magnetic Malrotation with Fistula and Volvulus. JSLS 16(4):644. https://doi.org/10.4293/108680812X13517013316474
Zefov V, Al Hashemi H, Javaid U (2022) Accidental ingestion of magnetic foreign body in a pediatric patient: A potentially fatal attraction’. Radiol Case Rep. https://doi.org/10.1016/J.RADCR.2022.04.007
August A, Mueller C (2016) Early recognition is important when multiple magnets masquerade as a single chain after foreign body ingestion. J Pediatr Surg Case Rep 13:8–9. https://doi.org/10.1016/J.EPSC.2016.07.006
Tsai J, Shaul DB, Sydorak RM, Lau ST, Akmal Y, Rodriguez K (2013) Ingestion of Magnetic Toys: Report of Serious Complications Requiring Surgical Intervention and a Proposed Management Algorithm. Perm J 17(1):11. https://doi.org/10.7812/TPP/12-097
Bauman B, McEachron K, Goldman D, et al (2019) Emergency Management of the Ingested Magnet: An Algorithmic Approach. Pediatr Emerg Care 35(8):e141–e144. https://doi.org/10.1097/PEC.0000000000001168
Rosenfield D, Strickland M, Fecteau A (2013) Magnet ingestion by a 3-year-old boy. CMAJ Can Med Assoc J 185(11):972–974. https://doi.org/10.1503/CMAJ.121847/-/DC1
Khalaf Z, Al Hindi S, Alsayegh R (2021) Laparoscopic assisted removal of multiple ingested magnetic foreign bodies in a child. J Pediatr Surg Case Rep. https://doi.org/10.1016/J.EPSC.2021.101950
Kusluk BK, Ozcakir E, Okay ST, Kaya M (2022) A Case of Intestinal Perforation Due To Multiple Magnet Ingestion: Minimally invasive approach is possible. Turk J Pediatr Surg 36:1
Oyewole B, Sandhya A, Maheswaran I, Campbell-Smith T (2020) Lockdown dilemma: ingestion of magnetic beads presenting as right iliac fossa pain and subacute small bowel obstruction. BMJ Case Rep. https://doi.org/10.1136/BCR-2020-236429
Li XL, Zhang QM, Lu SY, et al (2020) Clinical report and analysis of 24 cases of multiple magnetic beads foreign body in gastrointestinal tract of children. Turk J Gastroenterol 31(11):819–824. https://doi.org/10.5152/TJG.2020.19600
Te Cai D, Zhang SH, Gao ZG, Shu Q, Liu J (2020) Surgical treatment of multiple magnet ingestion in children: A single-center study. World J Clin Cases 8(23):5988. https://doi.org/10.12998/WJCC.V8.I23.5988
Altokhais T (2021) Magnet Ingestion in Children Management Guidelines and Prevention. Front Pediatr. https://doi.org/10.3389/FPED.2021.727988
Huang X, Hu J, Xia Z, Lin X (2021) Multiple magnetic foreign body ingestion in pediatric patients: a single-center retrospective review. Pediatr Surg Int 37(5):639–643. https://doi.org/10.1007/S00383-020-04814-W/FIGURES/3
Jin Y, Gao Z, Zhang Y, et al (2022) Management of multiple magnetic foreign body ingestion in pediatric patients. BMC Pediatr 22(1):448. https://doi.org/10.1186/S12887-022-03501-0/FIGURES/4
Huang YK, Hong SX, Tai IH, Hsieh KS (2021) Clinical characteristics of magnetic foreign body misingestion in children. Scie Rep. https://doi.org/10.1038/s41598-021-96595-y
Sola R, Rosenfeld EH, Yu YR, St. Peter SD, Shah SR (2018) Magnet foreign body ingestion: rare occurrence but big consequences. J Pediatr Surg. https://doi.org/10.1016/J.JPEDSURG.2017.08.013
Nicholson T, Tiruchelvam V (2023) Comparison of Laparoscopic-Assisted Appendectomy with Intracorporal Laparoscopic Appendectomy and Open Appendectomy. JSLS 5(1):47
Martínez-Pérez A, de'Angelis N, Brunetti F, et al (2017) Laparoscopic vs. open surgery for the treatment of iatrogenic colonoscopic perforations: a systematic review and meta-analysis. World J Emerg Surg 12:8. https://doi.org/10.1186/S13017-017-0121-X
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
RH (data curation, formal analysis, investigation, methodology, project administration). AKS (conceptualization, methodology, supervision and review and editing).
Corresponding author
Ethics declarations
Conflict of interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
For this type of study ethical approval is not required.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hayward, R.K., Saxena, A.K. Surgical management of pediatric multiple magnet ingestions in the past two decades of minimal access surgery- systematic review of operative approaches. Updates Surg 76, 1203–1211 (2024). https://doi.org/10.1007/s13304-023-01750-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01750-x