Abstract
Background
Swallowing multiple magnets or a magnet and second metallic object can carry risks of intestinal obstruction, fistula and perforation because they can attach to each other with loop of bowel in between. An updated management plan and reviewing our experience are warranted because of increased incidence of magnets ingestion among children.
Methods
All the patients who had a history of single, multiple magnet or single magnet and second metallic object ingestion in Bristol Royal Hospital for children during the period from January 2014 till November 2020 were included in our study.
Results
A total of 46 patients were referred to our hospital with a history of magnet ingestion. The number of magnets ingested ranged between one and twenty one magnets. All patients had abdominal x-ray undertaken either Antero-posterior alone (AP) (n = 32) or both AP and lateral (n = 14). Surgical intervention was performed in 18 patients; Oesophago-gastro-duodenoscopy (n = 8), laparotomy/laparoscpy (n = 10) to retrieve the magnets or deal with the complications.
Conclusions
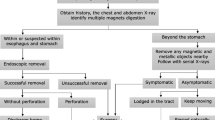
Magnets ingestion in children can be tricky when it comes to management. Complications can happen quite often and carry severe risks on children. An updated structured algorithm is proposed to manage children with magnet ingestion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Foreign body ingestion (FBI) is a very common occurrence in children aged between 6 months and 5 years [1]. Fortunately, coins are considered the commonest objects swallowed by children and usually pass easily down the alimentary tract with no intervention needed [2]. On the other hand, swallowing multiple magnets or a magnet and second metallic object can carry risks of intestinal obstruction, fistula formation and perforation because they can attach to each other across a loop of bowel [3].
The incidence of multiple ingested magnets has significantly increased in children [4]. With the increased incidence of multiple magnet ingestion among children and the possible life-threatening complications like perforation, fistula and obstruction, an updated management plan is warranted. The aim of this study is to review our experience over the past 6 years in dealing with this problem and to propose an updated management plan.
Methods
Retrospective review of medical notes of all the patients who had a history of single, multiple magnets or single magnet and second metallic object ingestion in Bristol Royal Hospital for Children, Bristol, UK, during the period from January 2014 to November 2020 were included in our study. Data reviewed from our maintained hospital database (Operative records and emergency department notes). Collected data focused on patient demographics, number and type of magnets ingested, presenting symptoms, hospital stay, type of imaging requested, surgical intervention and postoperative complications. Ethical committee approval was obtained before proceeding with this study. A chi-square statistical analysis was performed between the group of patients who swallowed either a single magnet or two magnets attached together in one hand, and the other group of patients who ingested two magnets or more separately.
Results
A total of 46 patients were referred to our tertiary children’s hospital with a history of magnet ingestion from January 2014 to November 2020. There were 28 males and 18 females with age range from 2 to 12 years (median = 6.8 years). The numbers of magnets ingested were between 1 and 21 (median = 11), with a predominance of multiple magnet ingestion. Single magnet ingestion was seen in only one child and other 45 children presented with multiple magnet ingestion.
Hospital stay ranged from 0 to 32 days (median = 16 days). 19 patients required no hospital admission after being reviewed in the emergency department or after a phone consultation with the referring hospital due to either single magnet ingestion or ingestion of two magnets together and not causing any symptoms. The remaining 27 patients (58%) required hospital admission between one to 32 days.
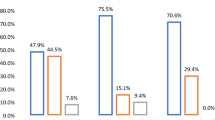
The majority of patients were asymptomatic (n = 31) while others experienced abdominal pain (n = 10), abdominal distension (n = 4) or chest pain (n = 1). The latter was due to magnet impaction in the oesophagus while abdominal symptoms were secondary to magnet-related complications; intestinal perforation, fistula or peritonitis.
One patient had a magnet impacted high in the oesophagus plus a second one in the stomach. He had a rigid endoscopic removal of the oesophageal magnet and a flexible gastroscopy to retrieve the magnet in the stomach. (Olympus scope size 11 and crocodile forceps or dormia basket through the side channel of the scope as per surgeon preferences). A second patient had three magnets in the distal oesophagus, one magnet in the jejunum and another magnet in the transverse colon. This patient underwent endoscopic removal of the oesophageal magnets, and laparotomy. In the rest of the patients, who ingested multiple magnets, these had reached the stomach, small bowel or colon by the time of admission (Table 1).
All patients had abdominal radiograph undertaken either Antero-posterior (AP) alone (n = 32) or both AP and lateral (n = 14) (Fig. 1). Surgical intervention was performed in 18 patients in the form of Oesphago-gastro-duodenoscopy (OGD) with magnet retrieval, laparoscopy or laparotomy. Nine patients underwent laparotomy either to retrieve the magnets or to deal with complications including perforation, fistula formation or intestinal obstruction (Fig. 2, case 7 in Table 1). In eight patients, OGD was successful in retrieving all ingested magnets from either the oesophagus or the stomach (Table 1, Fig. 3). One patient had laparoscopy and enterotomy through umbilical port to retrieve the magnets then closure of the enterotomy.
Abdominal X-rays showing magnets ingested (a) 2 magnets swallowed and present either in stomach or transverse colon indicating the need for lateral X-ray to differentiate. b Multiple magnets attached together obstructing the pylorus. c Lateral X-ray showing multiple magnets in the intestine. d Multiple magnets in different bowel loops causing Intestinal Obstruction
Laparotomy and on-table fluoroscopy (in two patients 6, 7 Table 1) were not sufficient to detect magnet location therefore; intra-operative formal abdominal radiograph was obtained to guide detecting the magnets (fluoroscopy failed to locate the exact site of magnet in these two cases).
A chi-square analysis was performed between the group of patients who swallowed either a single magnet or two magnets attached together in one hand, and the other group of patients who ingested two magnets or more separately. This statistical analysis between the two groups showed that the former group has a better prognosis (p value is < 0.05).
Discussion
Foreign body ingestion is considered one of the most common emergencies in children although 40% of them may pass uneventfully and unnoticed. It is far more common in children than in adults [5]. Children tend to ingest small objects like marbles, coins, and batteries, and a recent metanalysis showed that sharp objects and batteries most frequently require surgical intervention unlike other foreign bodies that will usually pass spontaneously [6].
There is a recent increase in the incidence of magnet ingestion among children, this may be attributed to the commercial availability of such magnets in toys; these new magnets are 5–20 times more powerful than ordinary iron magnets [7, 8]. Thus, a well-structured management protocol is warranted.
In our series, the median age is 6.8 years, which is comparable to other series (median age 7.9) [3]. FBI is commoner in males compared to females in the first 5 years of life and is commoner in females after the age of 15 years [3] In our study, magnet ingestion occurred in boys in 61% of cases; this is consistent with Sola et al. [3] (66% males 34% females) and Cho et al. (2 males and 1 female) [9].
Single magnet ingestion can be treated expectantly similar to other blunt foreign bodies. However, ingestion of multiple magnets or a single magnet and a second metallic object can attach together across two separate bowel loops or one loop of bowel folded back on itself especially if swallowed separately and not attached together.
Literature review suggests that emergency surgical intervention should be pursued to avoid potentially life-threatening complications, such as intestinal fistula formation, perforation and peritonitis [10,11,12,13,14].
Although ingestion of two magnets attached together is considered relatively safe and can be treated as single magnet, yet there are few data in the literature on how to deal with this situation. Our policy, for witnessed simultaneously ingestion of two magnets confirmed to be in the stomach on X-ray, is to manage them either conservatively for 14 days (as long as asymptomatic) or to retrieve them endoscopically.
Surgeons must be aware that two close magnets may be lying in two separate segments of bowel and not simply attached together in one loop. This error in interpretation of plain X-rays can occur if the magnets have already attenuated or partially penetrated the intervening bowel. That is why if there is any doubt that the magnets were not swallowed together or if the patient is symptomatic, surgical intervention should be warranted.
When more than two magnets are ingested, management depends on their position on the X-ray. Magnets that fail to pass the stomach will require OGD and retrieval but management of patients with magnets distal to the stomach will depend on clinical presentation. Symptomatic patients will undergo a laparotomy and magnet retrieval. Sola et al. managed these patients similarly however they offered routine laparoscopy as a treatment option [3]. For magnets located in the intestine in asymptomatic patients, hospital admission and serial abdominal radiograph for 48 hours is offered as many patients who require surgical intervention do not show any symptoms in the 1st 24 hours. Laparotomy is indicated if the magnet is not moving on serial abdominal radiograph after 48 hours as failure of progression on abdominal radiograph may reflect involvement of a bowel loop between adjacent magnets [10].
Magnets in the oesophagus can be removed safely with flexible or rigid endoscopy. This will save the patient from few hospital visits for “check” abdominal radiograph to locate the magnet and avoid further intervention (laparoscopy/laparotomy) if the magnet failed to move or if the patient becomes symptomatic (pyloric obstruction or abdominal pain). Asymptomatic patients with single magnet in the stomach can be treated expectantly at home with repeat abdominal radiograph two weeks post ingestion (in case of the magnet didn’t pass spontaneously which is very rare). If still in place, we advocate endoscopic removal.
“We conclude from our study that the indications for surgical intervention (laparotomy) after magnet ingestion are: (1) Symptomatic patients who swallowed ≥ 2 magnets separately or > 2 magnets swallowed together (intestinal obstruction/ peritonitis). (2) The second indication on the same group is fixed magnets on serial X-ray after 48-hours observation because of the possibility of intestinal fistula. (3) Symptomatic patients who swallowed one or two magnets together not accessible by OGD (none of our patients).”
We adopted a modified version of the structured management algorithm proposed by Sola et al. [3]. This is based on the number and location of magnets, and the presence or absence of symptoms or obstructive signs on the abdominal radiograph. The main difference between Sola’s algorithm and the one we proposed is including the management of single magnet ingestion, the management of symptomatic magnets lodged in the stomach and the management of two magnets swallowed together or separately (Fig. 4).
Our hospital admission rate was 58% (27 patients out of 46) compared to 46% (18 out of 39 patients) in other series [3]. Our low threshold policy in admitting patients post-magnet ingestion has helped in detection of early complications. However, we found that 9 patients in our series who swallowed 1 magnet or 2 magnets together (located in the stomach or the intestine and were asymptomatic) were admitted unnecessarily. Post-operative complications occurred in two patients in the form of wound infection after intestinal resection due to peritonitis. One of those two patients had mild wound infection and was managed conservatively; the other one had a severe wound infection that required surgical intervention and VAC dressing (vacuum assisted closure) for 30 days.
Although most cases in our study who were in need of surgical exploration underwent laparotomy to retrieve the magnets or deal with the magnet-related complications and only one patient had laparoscopy, the role of laparoscopy was reported by Sola et al. in 12 out of 21 patients who underwent abdominal surgery but it was unclear if this was confined to magnet retrieval or included management of magnet induced complications [3].
There are few limitations to our study; first, these data were retrospectively acquired and are at risk of inherent bias or lacking information. Both electronic and paper records were reviewed and compared. Second, although these data were collected from a tertiary centre yet it is only based on 46 cases. Thorough literature review was done and different management plans and algorithms were taken into consideration. Finally, being a single centre experience might not reflect the practice of other centres.
Conclusion
Magnet ingestion in children has potential drastic complications, thus a structured algorithm is advocated to guide surgeons on dealing with this problem.
The ingestion of 1 or 2 magnets attached together can be safely managed conservatively in asymptomatic patients. Ingesting more than two magnets might need surgical intervention, which can range from endoscopic removal up to laparotomy and multiple intestinal resections.
References
Arana A, Hauser B, Hachimi-Idrissi S, Vandenplas Y (2001) Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr 160:468–472
Sekmenli T, Ciftci I (2016) Multiple intestinal perforation and necrosis due to magnet ingestion. Eurasian J Med 48:225–227
Sola R Jr, Rosenfeld EH, Yangyang RY, Peter SD, Shah SR (2018) Magnet foreign body ingestion: rare occurrence but big consequences. J Pediatric Surgery 53:1815–1819
Strickland M, Rosenfield D, Fecteau A (2014) Magnetic foreign body injuries: a large pediatric hospital experience. J Pediatr 165(2):332–335
Uyemura MC (2005) Foreign body ingestion in children. Am Fam Physician 72:287–291
Jayachandra S, Eslick GD (2013) A systematic review of paediatric foreign body ingestion: presentation, complications, and management. Int J PediatrOtorhinolaryngol. 77:311–317
Tay ET, Weinberg G, Levin TL (2004) Ingested magnets: the force within. PediatrEmerg Care 20:466–467
Brown J, Otien JP, Drugas GT (2014) Pediatric magnet ingestions: the dark side of the force. Am J Surg 207:754–759
Cho J, Sung K, Lee D (2017) Magnetic foreign body ingestion in pediatric patients: report of three cases Cho et al. BMC Surg 17:73. https://doi.org/10.1186/s12893-017-0269-z
Kim Y, Hong J, Moon S-B (2014) Ingestion of multiple magnets: the count does matter. J PediatrSurg Case Rep 2:130–132. https://doi.org/10.1016/j.epsc.2014.02.013
US Consumer Product Safety Commission (2006) Child's death prompts replacement program of magnetic building sets, office of information and public affairs, Washington DC
Honzumi M, Shigemori C, Ito H, Mohri Y, Urata H, Yamamoto T (1995) An intestinal fistula in a 3-year-old child caused by the ingestion of magnets: report of a case. Surg Today 25:552–553
Nui A, Hirama T, Katsuramaki T, Maeda T, Meguro M, Nagayama M et al (2005) An intestinal volvulus caused by multiple magnet ingestion: an unexpected risk in children. J Pediatr Surg. 40:e9-11
Taher H, Azzam A, Khowailed O, Elseoudi M, Shaban M, Eltagy G (2019) A case report of an asymptomatic male child with multiple entero-enteric fistulae post multiple magnet ingestion. Int J Surgery Case Rep 85:50–53
Acknowledgements
We would like to thank Ms Eleri Cusick (consultant and clinical lead of paediatric surgery department in Bristol Royal Hospital for Children) for her effort in revising this work and providing some photos for publication.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mostafa, M.S., Darwish, A.A. Magnet ingestion in children and its implications: tertiary centre experience. Pediatr Surg Int 37, 937–944 (2021). https://doi.org/10.1007/s00383-021-04889-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04889-z