Abstract
Background
Evidence is growing about the benefits of laparoscopic resection with primary anastomosis (RPA) in perforated diverticulitis. However, the role of a diverting ileostomy in this setting is unclear. The aim of this study was to analyze the outcomes of laparoscopic RPA with or without a proximal diversion in Hinchey III diverticulitis.
Methods
This is a retrospective analysis of patients undergoing laparoscopic sigmoidectomy for perforated Hinchey III diverticulitis during the period 2000–2019. The sample was divided into two groups: RPA without diversion (G1) and RPA with protective ileostomy (G2). Primary outcomes of interest were 30-day overall morbidity, mortality, length of hospital stay (LOS), and urgent reoperation rates. Secondary outcomes of interest included operative time, readmission, and anastomotic leak rates.
Results
Laparoscopic RPA was performed in 94 patients: 76 without diversion (G1) and 18 with proximal loop ileostomy (G2). Mortality (G1: 1.3% vs. G2: 0%, p = 0.6), urgent reoperation (G1: 7.9% vs. G2: 5.6%, p = 0.73), and anastomotic leak rates (G1: 5.3% vs. G2: 0%, p = 0.32) were comparable between groups. Higher overall morbidity (G1: 27.6% vs. G2: 55.6%, p = 0.02) and readmission rates (G1: 1.3% vs. G2: 11.1%, p = 0.03), and longer LOS (G1: 6.3 vs. G2: 9.2 days, p = 0.02) and operative time (G1: 182.4 vs. G2: 230.2 min, p = 0.003) were found in patients with proximal diversion.
Conclusion
Laparoscopic RPA had favorable outcomes in selected patients with Hinchey III diverticulitis. The addition of a proximal ileostomy resulted in increased morbidity, readmissions, and length of stay. Further investigation is needed to establish which patients might benefit from proximal diversion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the last years, there has been an increase in hospital admissions and emergency room visits for diverticulitis [1]. Up to 2% of patients with diverticular disease presents with free perforation requiring emergent surgical treatment [2]. This scenario is associated with up to 50% of morbidity and 15–25% of mortality [3,4,5].
Traditionally, the operation of choice for patients with perforated diverticulitis has been the Hartmann’s procedure (HP). However, colostomy reversal after HP is a complex operation with considerable morbidity. Moreover, only 50 to 60% of patients undergo Hartmann’s reversal [6, 7]. In the last decade, multiple randomized controlled trials and meta-analyses have shown the superiority of resection with primary anastomosis (RPA) over HP for the management of Hinchey III diverticulitis. Most of the RPA in these studies were performed through a conventional approach and with proximal diversion [8,9,10,11,12,13,14]. Even though a protective ileostomy does not reduce the anastomotic leak rate, it could diminish its consequences, when they occur. However, performing a diverting ileostomy prolongs operative time, adds morbidity, and requires subsequent admission for reversal [15]. Moreover, laparoscopic RPA without diversion has been proved to be safe and feasible in selected patients with Hinchey III diverticulitis [16, 17].
It is not clear which patients (if any) will benefit from a protective ileostomy when RPA is performed. Therefore, the aim of this study was to evaluate the outcomes of patients undergoing laparoscopic RPA with or without protective loop ileostomy in perforated Hinchey III diverticulitis.
Materials and methods
Study design and population
A chart revision of all patients who underwent laparoscopic sigmoid resection for diverticular disease during 2000–2019 was performed. All laparoscopic sigmoid resections with primary anastomosis with or without proximal diversion for perforated Hinchey III diverticulitis were included in the analysis. Exclusion criteria were as follows: elective operations for stenosis, fistula and recurrent diverticulitis, open procedures, HP, and Hinchey IV perforated diverticulitis. The Institutional Review Board (IRB) of our hospital approved the study, and no written informed consent was needed due to the retrospective nature of the study.
The sample was divided into two groups: G1: laparoscopic RPA without proximal diversion and G2: laparoscopic RPA with a diverting loop ileostomy. Patient from G1 that underwent reoperation (laparoscopic lavage and ileostomy) for anastomotic leak was placed in RPA without ileostomy group based on intention to treat.
The indication for emergency surgery was based on clinical (persistent pain with signs of peritonitis) and imaging findings (computed tomography with diffuse pneumoperitoneum or fluid). Laparoscopic approach was used when the patient was hemodynamically stable. Patients who were hemodynamically unstable underwent open HP. Hinchey grade was assessed after exploratory laparoscopy. All patients received intravenous prophylactic antibiotics during anesthetic induction. Because of the emergent presentation, none of the patients underwent mechanical bowel preparation. The decision to perform a RPA and subsequent proximal diversion was based on the surgeon’s criteria.
Variables and outcomes
Data collected included age, gender, comorbidities, American Society of Anesthesiologists (ASA) classification, body mass index (BMI), previous episodes of diverticulitis, history of previous abdominal surgeries and laboratory findings. Operative variables such as operative time, conversion rate, intraoperative complications, and resident and colorectal specialist participation were also registered. Postoperative variables such as length of hospital stay (LOS), morbidity scored as per the Clavien–Dindo classification, anastomotic leak rates, re-intervention, and hospital readmission were also considered for analysis. Major morbidity was defined as complications ≥ 3a according to the Clavien–Dindo classification. Anastomotic leak was defined radiologically (peri-anastomotic air or contrast medium leak or on CT scan) and/or surgically (peritonitis at reoperation). Laboratory and imaging studies were performed when a postoperative complication was suspected. LOS was measured both after emergent operation and after including ileostomy reversal admission. In addition, long-term complications and non-reversal stoma rates were also registered.
Statistical analyses
The χ2 and Fisher tests were used to compare categorical variable, whereas Student’s t test was used for continuous variables. A probability (p) value of < 0.05 was considered statistically significant.
Results
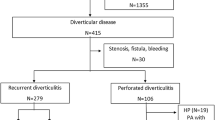
During the study period, 1829 patients underwent laparoscopic colorectal resections in our institution. Laparoscopic colectomy for diverticular disease was performed in 434 patients. After exclusion criteria were applied, 94 patients with RPA for perforated Hinchey III diverticulitis were analyzed: 76 (80.9%) without proximal diversion (G1) and 18 (19.1%) with proximal ileostomy (G2) (Fig. 1).
Demographics and preoperative variables were comparable between groups (Table 1). Mean operative time (G1:182.4 vs. G2:230.2 min p = 0.003) was significantly longer in G2. Conversion rate (G1:17.1% vs. G2:27.8% p = 0.30), intraoperative complications (G1: 3.9% vs. G2: 0% p = 0.30), and the presence of a certified colorectal surgeon (G1:67.1% vs. G2:55.5% p = 0.35) were similar between groups (Table 2).
Overall postoperative morbidity (G1: 27.6% vs. G2: 55.6% p = 0.02) was significantly higher in patients with proximal diversion. However, major morbidity (G1: 10.5% vs. G2: 11.1% p = 0.92), anastomotic leak rate (G1:5.3% vs. G2:0% p = 0.32), and mortality (G1: 1.3% vs. G2: 0%, p = 0.6) were comparable between groups. Urgent reoperation rate (G1: 7.9% vs. G2: 5.6%, p = 0.73) was also similar between groups. Six patients underwent re-intervention in G1: four laparoscopic lavage and loop ileostomy for anastomotic leak and two abdominal wall repairs for evisceration. Only one patient in G2 underwent reoperation for evisceration. No patient required conversion to HP. Patients with proximal ileostomy experienced higher readmission rates (G1: 1.3% vs. G2: 11.1%, p = 0.03), mainly due to dehydration.
Mean LOS after primary surgery (G1: 6.3 vs. G2: 9.2 days, p = 0.02) and when considering ileostomy reversal admission (G1: 6.4 vs. G2: 11.7 days, p < 0.001) was considerably longer in the G2 group (Table 3).
All patients in G2 underwent stoma reversal after an average of 82.3 (60–150) days. Similarly, the four patients in G1 who underwent urgent reoperation and ileostomy for anastomotic leak had their ileostomy reversed after a mean of 86.2 days (64–118). After ileostomy reversal, four patients had superficial wound infections that required drainage in outpatient clinic. Moreover, three (16.7%) patients from G2 required an incisional hernia repair in the ostomy reversal wound.
Discussion
The aim of this study was to analyze the outcomes after laparoscopic RPA with or without a proximal ileostomy in patients with perforated Hinchey III diverticulitis. We found that (a) reoperation, anastomotic leak, and mortality rates were comparable; (b) operative time, overall morbidity, readmission rate, and LOS were significantly higher in patients with proximal diversion; and (c) a considerable proportion of patients developed incisional hernia at ileostomy reversal’s wound.
Even though most patients hospitalized for acute diverticulitis can be managed by non-operative treatment, 15 to 32% of patients may require an emergency operation [18]. Current guidelines state that laparoscopic sigmoidectomy has benefits and is feasible in selected patients treated by experienced surgeons. Moreover, RPA with or without proximal diversion was recommended as the treatment of choice for Hinchey III diverticulitis in stable patients without significant comorbidities. Conversely, HP is still the preferred approach for patients with hemodynamic instability or multiple comorbidities [18,19,20]. However, many surgeons still believe that HP is the safer strategy when treating a patient with a diverticular perforation. A study that analyzed the national surgical quality improvement program database from 2012 to 2016 found that almost 92.4% of patients undergoing emergency surgery for acute diverticulitis had a HP and only 7.6% a RPA [21]. Moreover, the minimally invasive approaches are not widely implemented. Data from the National Health System Foundation Trusts of England have shown a significant increase in the use of laparoscopic resection through 2002 to 2016. Still, only 9.6% of operated patients underwent laparoscopic resection in the last 5-year period [22]. As previously published, in the last 5 years between 60 and 90% of perforated diverticulitis patients were managed by laparoscopic approach in our institution [23].
Several studies have shown the advantages of RPA, mostly with proximal diversion, over HP [8,9,10,11,12,13,14]. For instance, a recent meta-analysis of RCT that analyzed 382 patients (180 RPA vs. 204 HP) found that morbidity rates following the emergency operations did not differ, but organ/space surgical site infection (RPA 3.3% vs. HP 11.3%, p = 0.009) and morbidity rates following ostomy reversal (OR 0.31, 0.15–0.64, p = 0.001) were significantly lower after RPA [12]. Moreover, pooled ostomy non-reversal rates were higher after HP (RPA 16% vs. HP 35.5%). Similarly, another meta-analysis that analyzed 918 patients undergoing RPA or HP for Hinchey III/IV diverticulitis found lower stoma non-reversal rates following RPA (RPA 11.8% vs. HP 37.3%) and a reduction in overall mortality and major complications after the initial operation, stoma reversal and when combining both procedures [14]. In our series, all patients had their ileostomy reversed. Laparoscopic sigmoidectomy without proximal diversion is a procedure that combines the benefits of minimally invasive surgery and those related to the avoidance of an ostomy and its complications. When used in a selected population, this procedure has been proved to be safe and feasible [16, 17].
Scarce information is available regarding the role of a protective ileostomy in the setting of RPA for perforated diverticulitis. It seems that performing a RPA with ileostomy is an intermediate option between the most morbid HP and the one-step RPA without diversion. Although a diverting ileostomy may not reduce mortality or anastomotic leak (AL) rates, it lessens the magnitude of sepsis, morbidity, and the need for urgent reoperation if an AL develops [24]. Moreover, reversing a loop ileostomy is less complex than HP reversal. In our series, mortality and AL rates were similar between groups. Conversely, even though performing an ileostomy is technically simple, an additional stoma (and its reversal) prolongs operative time and carries their own morbidity. Anastomotic leakage, wound infections, skin irritation, parastomal herniation, dehydration, and readmissions are possible complications [25]. For instance, we found longer operative times (G1: 182.4 vs. 230.2 min, p = 0.003) and higher overall morbidity (G1: 27.6% vs. G2: 55.6%, p = 0.02) in patients with proximal ileostomy. Longer operative time could be explained by the addition of the ileostomy itself. However, it could be hypothesized that a more complex operation resulting in longer operative time was the reason for adding a protective ileostomy. A study by Wise et al. analyzing 15602 patients undergoing elective surgery for diverticular disease found that 2.2% had a proximal diversion and this was associated with increased risk of surgical site infection, acute renal failure, readmissions, and prolonged length of hospital stay [26]. Similarly, we found that patients with proximal ileostomy had higher readmission rates and longer LOS, even without considering the ileostomy reversal hospital stay. Although no major complications occurred after stoma reversal in our series, 16.7% of patients underwent surgery for an incisional hernia in the stoma reversal wound.
Limitations of this study include its retrospective nature, which is the main limiting factor. Moreover, the relatively low number of patients in group 2 might explain the lack of statistical significance in some analyses. It is possible that case selection or selection bias has influenced our results since the decision to perform a proximal ileostomy was at individual surgeon’s discretion. However, as RPA was only considered in stable patients without significant comorbidities, we believe that this bias was lower than in studies comparing RPA with HP. To our knowledge, this is one of the largest series of laparoscopic RPA in perforated Hinchey III diverticulitis, and the first study that challenges the benefits of a proximal diversion in this setting.
Conclusions
Laparoscopic RPA for perforated diverticulitis is safe and feasible in selected patients. The use of proximal diversion resulted in higher morbidity, readmission rates, and longer LOS without reducing mortality or anastomotic leak rates. Further investigation is required to define which patients might benefit from this procedure.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nguyen GC, Sam J, Anand N (2011) Epidemiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol 17:1600–1605
Ricciardi R, Baxter NN, Read TE, Marcello PW, Hall J, Roberts PL (2009) Is the decline in the surgical treatment for diverticulitis associated with an increase in complicated diverticulitis? Dis Colon Rectum 52:1558–1563
Morris CR, Harvey IM, Stebbings WS, Hart AR (2008) Incidence of perforated diverticulitis and risk factor for death in UK population 95:876–881
Constantinides VA, Tekkis PP, Senapati A (2006) A prospective multicenter evaluation of adverse outcomes following treatment for complicated diverticular disease. BJS 93:1503–1513
Abbas S (2007) Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis 22:351–357
Maggard MA, Zingmond D, O´Connell JB, Ko CY (2004) What proportion of patients with an ostomy (for diverticulitis) get reversed? Am Surg 70:928–931
Banerjee S, Leather AJ, Rennie JA, Samano N, Gonzalez JG, Papagrigoriadis S (2005) Feasibility and morbidity of reversal of Hartmann´s. Colorectal Dis 7:454–459
Binda GA, Karas JR, Serventi A, Sokmen S, Amato A, Hydo L, Bergamaschi R, Study group on diverticulitis (2012) Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis 14(11):1403–1410
Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger P, Buchli C, Grieder F, Gelpke H, Decurtins M, Tempia-Caliera AA, Demartines N, Hahnloser D, Clavien PA, Breitenstein S (2012) A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg 256:819–826
Bridoux V, Regimbeau JM, Ouaissi M, Mathonnet M, Mauvais F, Houivet E, Schwarz L, Mege D, Sielezneff I, Sabbagh C, Tuech JJ (2017) Hartmann’s procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial (DIVERTI). J Am Coll Surg 225:798–805
Lambrichts DPV, Vennix S, Musters GD, Mulder IM, Swank HA, Hoofwijk AGM, Belgers EHJ, Stockmann HBAC, Eijsbouts QAJ, Gerhards MF, van Wagensveld BA, van Geloven AAW, Crolla RMPH, Nienhuijs SW, Govaert MJPM, di Saverio S, D’Hoore AJL, Consten ECJ, van Grevenstein WMU, Pierik REGJM, Kruyt PM, van der Hoeven JAV, Steup WH, Catena F, Konsten JLM, Vermeulen J, van Dieren S, Bemelman WA, Lange JF, LADIES trial collaborators, (2019) Hartmann’s procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol 4:599–610
Gachabayov M, Tuech JJ, Tulina I, Coget J, Bridoux V, Bergamaschi R (2020) Primary anastomosis and nonrestorative resection for perforated diverticulitis with peritonitis: meta-analysis of randomized trials. Colorectal Dis. https://doi.org/10.1111/codi.15016
Halim H, Askari A, Nunn R, Hollingshead J (2019) Primary resection anastomosis versus Hartmann’s procedure in Hinchey III and IV diverticulitis. World J Emerg Surg 14:32
Ryan OK, Ryan EJ, Creavin B, Boland MR, Kelly ME, Winter DC (2020) Systematic review and meta-analysis comparing primary resection and anastomosis versus Hartmann’s procedure for the management of acute perforated diverticulitis with generalized peritonitis. Tech Coloproctol. https://doi.org/10.1007/s10151-020-02172-2
Giannakopoulos GF, Veenhof AA, van der Peet DL, Sietses C, Meijerink WJ, Cuesta MA (2009) Morbidity and complications of protective loop ileostomy. Colorectal Dis 11:609–612
Dreifuss NH, Schlottmann F, Piatti JM, Bun ME, Rotholtz NA (2019) Safety and feasibility of laparoscopic sigmoid resection without diversion in perforated diverticulitis. Surg Endosc 34:1336–1342
Vennix S, Boersema GS, Buskens CJ, Menon AG, Tanis PJ, Lange JF, Bemelman WA (2016) Emergency laparoscopic sigmoidectomy for perforated diverticulitis: a systematic review. Dig Surg 33:1–7
Hall J, Hardiman K, Lee S, Lightner A, Stocchi L, Paquette I, Steele SR, Feingold D (2020) The American Society of Colon and Rectal Surgeons clinical practice guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum 63:728–747
Francis NK, Sylla P, Abou Khalil M, Arolfo S, Berler D, Curtis NJ, Dolejs SC, Garfinkle R, Gorter-Stam M, Hashimoto DA, Hassinger TE, Molenaar CJL, Pucher PH, SchuermansV AA, Agresta F, Antoniou SA, Arulampalam T, Boutros M, Bouvy N, Campbell K, Francone T, Haggerty SP, Hedrick TL, Stefanidis D, Truitt MS, Kelly J, Ket H, Dunkin BJ, Pietrabissa A (2019) EAES and SAGES 2018 consensus conference on acute diverticulitis management: evidence-based recommendations for clinical practice. Surg Endosc 33:2726–2741
Sartelli M, Catena F, Ansaloni L, Coccolini F et al (2016) WSES guidelines for the management of acute left side colonic diverticulitis in the emergency setting. World J Emerg Surg 11:37
Lee JM, Chang BP, J, El Hechi M, Kongkaewpaisan N, Bonde A, Mendoza AE, Saillant NN, Fagenholz PJ, Velmahos G, Kaafarani HM, (2019) Hartmann’s procedure vs primary anastomosis with diverting loop ileostomy for acute diverticulitis: nationwide analysis of 2729 surgery patients. J Am Coll Surg 229:48–55
Baldock TE, Brown LR, McLean RC (2019) Perforated diverticulitis in the North of England: trends in patient outcomes, management approach and the influence of subspecialisation. Ann R Coll Surg Engl 101:563–570
Dreifuss NH, Schlottmann F, Bun ME, Rotholtz NA (2020) Emergent laparoscopic sigmoid resection for perforated diverticulitis: can it be safely performed by residents? Colorectal Dis. https://doi.org/10.1111/codi.14973
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary. Langenbecks Arch Surg 400:145–152
Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D (2006) Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum 49:1011–1017
Wise KB, Merchea A, Cima RR, Colibaseanu DT, Thomsen KM, Habermann EB (2015) Proximal intestinal diversion is associated with increased morbidity in patients undergoing elective colectomy for diverticular disease: an ACS-NSQIP study. J Gastrointest Surg 19:535–542
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to conception and design, acquisition, analysis and interpretation of data, drafting and revising of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest, financial ties, or funding/support to disclose.
Ethics approval/consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the IRB of our institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dreifuss, N.H., Bras Harriott, C., Schlottmann, F. et al. Laparoscopic resection and primary anastomosis for perforated diverticulitis: with or without loop ileostomy?. Updates Surg 73, 555–560 (2021). https://doi.org/10.1007/s13304-020-00952-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00952-x