Summary
Background
The surgical management of perforated sigmoid diverticulitis (PSD) is controversial and challenging. Hartmann’s procedure (HP) still remains the most frequently performed procedure for diffuse peritonitis. However, because less than 50% of patients never achieve restored bowel continuity, alternative surgical procedures have been proposed, including laparoscopic lavage and resection with primary anastomosis (PRA), with or without a covering ileostomy. We performed a retrospective study to compare HP vs. PRA with loop-ileostomy for the treatment of PSD with generalized peritonitis.
Methods
Data from 194 patients operated on for PSD from January 2008 to December 2018 were analyzed. Patients were classified into two groups: PRA and HP, according to the surgical procedure performed.
Results
In all, 113 (58%) patients underwent HP while PRA was performed on 81 (42%) patients. Primary anastomosis was associated with fewer postoperative major complications than HP (p < 0.05). However, patients in the PRA group were significantly younger (median 76 vs. 60 years, p < 0.05), with a reduced proportion of patients with ASA III–V grade (31% vs. 66%, p < 0.05). In 58 patients from the HP group (52%) end colostomies were reversed, whereas the stoma reversal rate after ileostomy was significantly higher (96%, p < 0.05).
Conclusion
Primary anastomosis can be performed safely without adding morbidity and mortality in cases of generalized diverticular peritonitis. Hartmann’s procedure should be reserved only for hemodynamically unstable or high-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical management of perforated sigmoid diverticulitis (PSD) with generalized peritonitis is a challenging and evolving issue [1]. Currently, resection surgery is the treatment of choice, as recommended by most guidelines [2, 3].
The traditional approach for PSD, Hartmann’s procedure (HP), is an open segmental resection of the inflamed sigmoid colon with formation of a temporary end colostomy. This approach has considerable morbidity and the challenge of stoma reversal. However, because less than 50% of patients never achieve restored bowel continuity given the considerable morbidity associated with an end colostomy reversal, alternative surgical procedures have been proposed, including laparoscopic lavage and resection with primary anastomosis (PRA), with or without a covering ileostomy. A number of systematic reviews and meta-analyses have been published comparing these two approaches [4, 5], but no definitive recommendations have been established on the topic. The proven benefit of PRA in the elective setting might be even more pronounced in emergency sigmoidectomy than in the elective setting by avoiding abdominal wall complications, e.g., abdominal wound dehiscence, incisional hernia, and wound infection and in the rate of no conversion to ostomy.
The advantage of HP is a shorter operating time without a lower risk of anastomotic insufficiency. However, reversal of the colostomy might be a more extensive, time-consuming procedure with a significant risk for complications, when compared with the reversal of a simple diverting ileostomy [6, 7]. The rate of reversal after diverting ileostomy is reported to be remarkably higher (80–90%) than closure of an end colostomy after HP (40–50%; [8, 9]).
We performed a retrospective study to compare HP with PRA with loop-ileostomy for the treatment of PSD with generalized peritonitis. The outcomes were the morbidity and mortality rates after the first intervention and stoma reversal operation in the two groups.
Methods
This was a retrospective study, comparing rates of adverse events between patients undergoing PRA vs. HP for perforated diverticulitis with peritonitis.
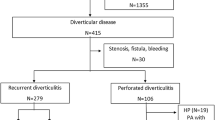
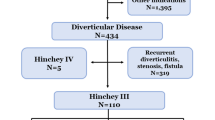
From January 2008 to December 2018, 578 consecutive patients were admitted to our Basic Surgery Unit, in the only hospital on Ischia (Gulf of Naples, Italy), for complicated colonic diverticular disease. All patients with Hinchey III and IV diverticulitis undergoing surgical treatment were included. Exclusion criteria were: (1) Hinchey I–II diverticulitis; (2) colon cancer as definitive diagnosis on histopathological analysis; (3) use of laparoscopic approach (Fig. 1).
All patients underwent computed tomography (CT) of the abdomen and pelvis. The preoperative data are listed in Table 1.
Postoperative outcomes were morbidity, scored as Clavien–Dindo I or IIIB 10 [18], mortality (within 30 days), length of hospital stay, and surgical or percutaneous re-interventions. Data on no stoma reversal and incisional hernia were collected at 12 months. All patients were given intravenous antibiotics and deep venous thrombosis prophylaxis prior to surgery with subcutaneous enoxaparin 4000 UI/day. All patients underwent intraoperative lavage of the peritoneal cavity with normal saline (0.9% NaCl). Because of the retrospective design of the present study microbiological data were not always available and therefore bacterial cultures and antibiotic sensitivity were not considered in the endpoints of the study. Closed no-suction drainage was placed along the left paracolic gutter and pouch of Douglas. Primary anastomosis was performed through a midline laparotomy. Lateral to medial mobilization of the left colon was performed and the left ureter was identified when possible. The rectosigmoid junction was identified and transacted with a stapler. Normal-appearing descending colon with no signs of inflammation or thickening of the mesentery or serosal surface was chosen for proximal transection. A purse-string suture was hand sewn on the oral end of the colon. A double-stapled anastomosis was performed. Loop-ileostomy on the right side was carried out. Nonrestorative colon resection with HP was performed according to the same technical steps. Mobilization of the spleen flexure was not always performed. Decisions to take down the splenic flexure were made individually by the surgeons. An end colostomy was created to the left side. Ileostomy reversal was performed with a peri-stoma incision. A functional end-to-end anastomosis was made using a cutting stapler. Closure of the enterotomy was accomplished with a linear stapler. When possible, the stoma reversal for the procedures was set to take place up to 3 months after the first operation of PRA and 3–6 months after the first HP operation. The same method of wound closure was utilized with double-running longest-lasting absorbable monofilament sutures. Incisional hernia was diagnosed by physical examination and when necessary by CT and by ultrasound imaging. In our surgical unit, there are 10 surgeons, of whom only three have specific skills in colorectal surgery (defined as colorectal surgeon [CS] after having undergone a training period of at least 5 years in a colorectal unit after completing general surgery training). The rest of the surgeons were considered general surgeons (GS).
Statistical analysis
Continuous variables are expressed as means ± standard error of the mean (SEM). Categorical variables are expressed as percentage. All variables were tested for normal distribution using the Kolmogorov–Smirnov test. Normally distributed variables were compared between the two groups using the two-sided, unpaired Student’s t test with the assumption of unequal variance. Statistical significance was set at p < 0.05 Rates and proportions were compared between groups of interest using the chi-square test. Statistical analysis was performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA).
Results
A total of 578 patients were admitted to our surgical unit for colon diverticulitis between January 2008 and December 2018. A total of 268 patients with purulent or fecal peritonitis (Hinchey III–IV) were operated on for perforated diverticulitis in an emergency setting; 74 patients were excluded according to the exclusion criteria. Analysis was made on 194 patients with available data (Fig. 1): 113 patients underwent HP and 81 underwent PRA with loop-ileostomy.
Patient demographics, clinical perioperative characteristics, and key laboratory data are presented in Table 1: median age was 72 years (range 56–91), with 47% males. The median BMI was 31 (range 25–33 kg/m2) and most patients had an ASA grade of I or II; 38% of patients were categorized as Hinchey III and 62% as Hinchey IV.
Comparison analysis of patient characteristics showed no statistical difference between the HP and PRA groups in terms of Hinchey classification, previous episodes of diverticulitis, and previous abdominal surgery. However, patients in the PRA group were significantly younger (median 76 vs. 60 HP vs. PRA p < 0.05), with reduced proportions of patients with ASA III–V grade (31% vs. 66%; p < 0.05), and PCR was lower compared with the HP group (p < 0.05). No difference was found for BMI. The results of the first operation alone (resection alone for HP or PA) are summarized in Table 2. There was a statistically significant difference in the rate of postoperative hospital mortality after the first intervention in the two groups, favoring PRA over HP (0% vs. 2.6% p < 0.05). However, mortality occurred in severely ill patients classified as ASA III–IV.
Although the operating time was slightly longer in the PRA group (75 vs. 130 min, p < 0.05), all the outcome measures, including complications, were comparable in both groups. Table 2 shows the distribution of the different types of complications. Two patients had anastomotic leaks in the PRA group after the first intervention (2/81, 2.4%), with one patient undergoing a radiological drainage and the other treated conservatively with medical therapy only. Three patients had anastomotic leak during reversal end colostomy; for two of them there was conversion to HP intervention and for one a loop-ileostomy was performed. No leak occurred in the cases of reversal of loop-ileostomy.
The difference in postoperative complications (grade II–IIIa) was not statistically significant in the two group; the rate of severe complications (grades IIIb–IV; 20% vs. 0%, p < 0.05), as well as the total number of complications per patient (median 1 vs. median 0, p < 0.001), was significantly higher in the HP group (Table 2).
Only 58 patients (52%) with end colostomies (after HP) had reversal, whereas the stoma reversal rate after ileostomy was significantly higher (96%; p < 0.05). The reason for not having the stoma reversed was (a) the operative risk as assessed by the surgeon in 20% of cases and (b) the patient’s choice in 80% (Table 3). Diverting ileostomies were reversed much earlier than the end colostomies after HP (median time 3 vs. 6 months, respectively).
Although the differences in postoperative complications (grade II–IIIa) were not statistically significant in the two groups with reversal operations, the rate of severe complications (grades IIIb–IV) and the total number of complications per patient were significantly higher in the end colostomy reversal group (Table 3).
Furthermore, the hospital stay (median of 9 vs. 6 days, p < 0.05) was significantly longer in the reversal end stoma group (Table 4). Total hospital stay during the first operation (HP and PRA) and the stoma closure was not statistically different. We found that both the ASA score and the C‑reactive protein level were associated with the choice for a specific surgical technique (PRA or HP; p < 0.05), whereas Hinchey IV classification was not. Morning or night did not influence the choice of the kind of surgery. Considering only the 113 patients in the HP group, we observed that only 29 (26%) patients were operated on by a CS; 79 (97%) patients in the PRA group were operated on by a CS (Table 3). At the time of stoma reversal, we found that the rate of incisional hernia was very high (22/77, 29% in the PRA group and 40/58 69% in the HP group). Similarly, almost all patients had para-stomal hernia (89% in the PRA group and 90% in the HP group).
Median incisional hernia was diagnosed in 65 patients (87%): 38 (58%) by physical examination, nine (6%) by CT, and 18 (13%) by ultrasound imaging. After stoma reversal, 12-month follow-up was possible in 98 (72%) patients, and no difference was found in the rate of median incisional hernia (22% HP group vs. 24% PRA group). In all, 121 patients developed an incisional hernia at the stoma incision site (42% HP vs. 39% PRA). For patients with permanent end colostomy, 12-month follow-up was achieved in 50 (90%) patients: 47 of 50 (95%) had a parastomal hernia. Four patients underwent urgent operation for colon occlusion.
Discussion
Grade Hinchey III and IV perforated diverticulitis is associated with high morbidity and mortality; therefore, optimization of its treatment is of paramount importance [10,11,12,13]. Most of the available guidelines recommend resection surgery in perforated diverticulitis; however, a clear preference for either PRA or HP is not well established [14, 15]. The World Society of Emergency Surgery (WSES) 2016 guidelines advise using HP for the management of generalized peritonitis in critically ill patients and in patients with multiple comorbidities [4]. However, they also advise that in clinically stable patients with no comorbidities, PRA with or without a diverting stoma may be performed [16]. The American Society of Colon and Rectal Surgeons (ASCRS) 2014 practice parameters recommend that, “following resection, the decision to restore bowel continuity must incorporate patient factors, intraoperative factors and surgeon preference” [17]. The Association of Colon proctology of Great Britain and Ireland (ACPGBI) and the Royal College of Surgeons (RCS) 2014 guidance on colonic diverticular disease states that both HP and PRA with or without a covering stoma are potential options and the decision regarding which to utilize should be made on an individual patient basis [15].
This retrospective study demonstrates that PRA with diverting ileostomy is comparable to HP in terms of outcome measures. The main advantages relate mainly to the ileostomy reversal, which is more likely to occur and is associated with less severe complications in PRA than colostomy reversal after HP.
Cirocchi et al. in a meta-analysis of all currently available RCTs comparing HP with PRA for the treatment of perforated sigmoid diverticulitis with generalized peritonitis found no significant difference between PRA and HP in terms of postoperative morbidity and mortality after the index procedure or cumulatively after inclusion of the stoma reversal surgery [18]. However, several prognostic factors influencing morbidity and mortality in acute left-sided colonic perforation, such as age, ASA score, need for emergency operation, and the severity of peritonitis, have been described [19,20,21]. With regard to the first operation (resection), the difference in the mortality rate was statistically significant, with three patients dying in the HP group (2.5%) vs. no death in the PRA group. We found comparable morbidity rates in the HP and the PRA groups based on the Cleveland Complication Score, except for the overall number of complications favoring the HP group. No difference was found when comparing the overall rate of mortality and morbidity in the HP group and the PRA group with similar ASA score I–II and III. Beside the Hinchey scale, there were no other factors influencing the choice of operation (HP vs. PRA). Other outcome parameters, such as hospital stay and intensive care unit (ICU) stay, were higher in the HP group than in the PRA group. The operation time was longer in the PRA group than in the HP group.
According to these results, mortality seems to be more likely associated with the status of the patient than with the type of operation. However, it should be noted that the HP and PRA groups had different characteristics (see Results), a recurrent bias already documented in a systematic review by Salem and Flum [19].
A systematic review published in 2006 by Constantinides et al. [4] that included 15 studies published between 1984 and 2004 and 963 patients comparing RPA with HP did not find any significant difference in terms of postoperative mortality for diverticular peritonitis (Hinchey >II).
Biondo et al. concluded [22] that one-stage colon resection and primary anastomosis can be performed safely for purulent diffuse and fecal peritonitis, with low mortality and morbidity compared with HP as well as with lower costs and faster rehabilitation. This study used intracolonic lavage 24 that may influence complication rates. Several other authors consider that PRA with and without loop-ileostomy may be a valid strategy for selected patients, and may represent a good compromise between postoperative adverse events, long-term quality of life, and risk of permanent stoma [1, 24].
Previous studies have demonstrated that PRA without a covering ileostomy is feasible; however, it can be associated with a significant rate of complications (24–84%; [23, 25, 26]).
Zingg et al. [27] reported a clinical leak rate of 28% after PRA without diverting ileostomy for perforated diverticulitis. Trenti et al. [28] observed three anastomotic leakages (11.1%). None of these patients had diverting ileostomy and all required urgent re-operations. In our experience, all patients in the PRA group had a loop-ileostomy, independent of status in terms of ASA score or Hinchey III or IV classification. Only two patients had an anastomotic leak, and none needed re-intervention. Some authors [29] emphasize that PRA and loop-ileostomy should be taken into consideration for selected patients, but selection criteria remain unclear. Predisposing factors for anastomotic leakage are multiple in the emergency setting, such as hemodynamic instability, malnutrition, coagulopathy, degree of peritoneal contamination, and surgeon experience [14]. By exploring whether the choice of the type of operation was influenced by the surgeons’ experience, we observed that CSs tend to perform more PRA with DI compared with GSs.
These results could reflect the trend among CSs to extend criteria for resection and primary anastomosis when a diverting stoma is associated with patients who would have been treated in the past by HP. Hartmann’s operation allows anastomotic leakage to be avoided, but one has to take into consideration that Hartmann’s reversal is also associated with substantial morbidity and mortality, with an anastomotic leakage of up to 25% [20, 30, 31]; for these reasons, only about half of patients have their colostomy reconstructed after HP [32, 33].
Reversal of HP is viewed by most surgeons as a more complex procedure with a higher risk of adverse events when compared with closure of a covering ileostomy [6, 7]. The main benefit of a PRA with protective ileostomy compared with HP is the significantly higher stoma reversal rate during follow-up. In our study, only 58 patients (52%) with end colostomies (after HP) underwent reversal, whereas the stoma reversal rate after ileostomy was significantly higher: 77 patients (96%, p < 0.05).
Similar reversal rates can be found in the literature, 60–70% for HP and 41–90% for PRA [34]. Oberkofler et al. [35] in MRCT reported that only 15 of 26 (58%) end colostomies (after HP) were eventually reversed, whereas the stoma reversal rate after ileostomy was significantly higher at 90% (26/29, p < 0.05; [35]). Moreover, ileostomy reversal was associated with fewer complications. In particular, one of the patients after ileostomy reversal required re-operation for intra-abdominal bleeding, whereas after colostomy reversal, three patients had to be re-operated because of intra-abdominal infection for leak and one for intra-abdominal bleeding; one required ICU admission due to pulmonary failure.
Focusing on reconstructive surgery: The two groups had an equal distribution in the percentage of ASA score. There was a statistical difference in morbidity, according to the Clavien–Dindo classification (Table 3).
The reason why the occurrence of serious complications was significantly different in the second operation is that it associated more with the difficulty of the operation in the HP group than with the condition of the patients. In fact, only patients with less comorbidity in the HP group chose to be re-canalized. Moreover, in reversal colostomy there was a higher rate of SIS, which was associated with longer hospital stays. Ever since abdominal wall surgery became routine, the occurrence of incisional or stomal hernia has been considered an inevitable late complication of any abdominal procedure [36]. The high rate of incisional hernia observed in this study is concordant with that observed in recent studies [37, 38] Risk factors for developing an incisional hernia can be divided into patient factors and surgery-related factors. Patient factors include diabetes, smoking, obesity, corticosteroids, and connective tissue disorders, including patients with an abdominal aortic aneurysm. Factors related to surgery include the incision, type of surgery, wound classification, the suture material, and the ratio of suture length to wound length [39].
The high rate of median incisional hernia and parastomal hernia in this study was probably related to contaminated and dirty wound classification and patient comorbidity. The high rate of SIS in the two groups was another risk factor for developing incisional hernia. Our study did not include quality of life (QOL) data. Both ileostomy and colostomy result in significant QOL impairment [32]. Ileostomies are generally less tolerated [33]. Given that a proportion of patients with colostomy and ileostomy did not have bowel continuity restored, the impact on QOL is an important consideration when evaluating the benefits of each surgical approach.
Conclusion
The management of complicated sigmoid diverticulitis is controversial. The literature is dominated by nonrandomized studies, the majority of which are retrospective [4,5,6,7,8].
In our experience, PRA with protective ileostomy in the treatment of acute left-sided colonic perforation with generalized peritonitis could be an effective option in selected patients. The benefit directly relates to the stoma reversal operation, which is more likely to occur and is safer in PRA vs. HP. Further investigations are required to identify a group of patients who may potentially not require a diverting ileostomy. Hartmann’s procedure is our procedure of choice in patients with a high ASA score.
References
Angenete E, Thornell A, Burcharth J. Laparoscopic lavage is feasible and safe for the treatment of perforated diverticulitis with purulent peritonitis: the first results from the randomized controlled trial DILALA. Ann Surg. 2016;263:117–22.
Schultz JK, Yaqub S, Wallon C, SCANDIV Study Group. Laparoscopic lavage vs primary resection for acute perforated diverticulitis: the SCANDIV randomized clinical trial. JAMA. 2015;314:1364–75.
Bridoux V, Regimbeau JM, Ouaissi M. Hartmann’s procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial (DIVERTI). J Am Coll Surg. 2017;225:798–805.
Constantinides VA, Tekkis PP, Athanasiou T, Aziz O, Purkayastha S, Remzi FH, et al. Primary resection with anastomosis vs. Hartmann’s procedure in nonelective surgery for acute colonic diverticulitis: a systematic review. Dis Colon Rectum. 2006;49(7):966–81.
Cirocchi R, Trastulli S, Desiderio J, Listorti C, Boselli C, Parisi A, et al. Treatment of Hinchey stage III–IV diverticulitis: a systematic review and meta-analysis. Int J Colorectal Dis. 2013;28(4):447–57.
Vermeulen J, Coene PP, Van Hout NM. Restoration of bowel continuity after surgery for acute perforated diverticulitis: should Hartmann’s procedure be considered a one-stage procedure? Colorectal Dis. 2009;11:619–24.
Aydin HN, Remzi FH, Tekkis PP. Hartmann’s reversal is associated with high postoperative adverse events. Dis Colon Rectum. 2005;48:2117–26.
Salem L, Flum DR. Primary anastomosis or Hartmann’s procedure for patients with diverticular peritonitis? A systematic review. Dis Colon Rectum. 2004;47:1953–64.
Breitenstein S, Kraus A, Hahnloser D. Emergency left colon resection for acute perforation: primary anastomosis or Hartmann’s procedure? A casematched control study. World J Surg. 2007;31:2117–24.
Zorcolo L, Covotta L, Carlomagno N, Bartolo DC. Safety of primary anastomosis in emergency colo-rectal surgery. Colorectal Dis. 2003;5:262–9.
Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E, et al. Peritonitis-Index. Chirurg. 1987;58:84–92.
Pocock SJ. When (not) to stop a clinical trial for benefit. JAMA. 2005;295:2228–30.
Lievre M, Menard J, Bruckert E. Premature discontinuation of clinical trial for reasons not related to efficacy, safety, or feasibility. BMJ. 2001;322:603–5.
Binda GA, Cuomo R, Laghi A, Nascimbeni R, Serventi A, Bellini D et al. Practice parameters for the treatment of colonic diverticular disease: Italian society of colon and rectal surgery (SICCR) guidelines. Tech Coloproctol. 2015;19(10):615–26.
ACPGBI. Commissioning guide: colonic diverticular disease RCS. 2014.
Sartelli M, Catena F, Ansaloni L, Coccolini F, Griffiths EA, Abu-Zidan FM, et al. WSES guidelines for the management of acute left sided colonic diverticulitis in the emergency setting. World J Emerg Surg. 2016;11:37.
Feingold D, Steele SR, Lee S, Kaiser A, Boushey R, Buie WD, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57(3):284–94.
Cirocchi R, Afshar S, Shaban F, Nascimbeni R, Vettoretto N, et al. Perforated sigmoid diverticulitis: Hartmann’s procedure or resection with primary anastomosis a systematic review and meta-analysis of randomised control trials. Tech Coloproctol. 2018;22(10):743–53. https://doi.org/10.1007/s10151-018-1819-9.
Salem L, Anaya DA, Roberts KE. Hartmann’s colectomy and reversal indiverticulitis: a population-level assessment. Dis Colon Rectum. 2005;48:988–95.
Tudor RG, Farmakis N, Keighley MR. National audit of complicated diverticular disease: analysis of index cases. Br J Surg. 1994;81:730–2.
Abbas S. Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis. 2007;22(4):351–7.
Jaurrieta E, Jorba R, Moreno P, Farran L, Borobia F, Bettonica C, et al. Intraoperative colonic lavage and primary anastomosis in peritonitis and obstruction. Br J Surg. 1997;84(2):222–5.
Hold M, Denck H, Bull P. Surgical management of perforating diverticular disease in Austria. Int J Colorectal Dis. 1990;5(4):195–9.
Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, Belgers EH, et al. Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. Lancet. 2015;386(10000):1269–77.
Regenet N, Pessaux P, Hennekinne S, Lermite E, Tuech JJ, Brehant O, et al. Primary anastomosis after intraoperative colonic lavage vs. Hartmann’s procedure in generalized peritonitis complicating diverticular disease of the colon. Int J Colorectal Dis. 2003;18(6):503–7.
Auguste L, Borrero E, Wise L. Surgical management of perforated colonic diverticulitis. Arch Surg. 1985;120(4):450–2.
Zingg U, Pasternak I, Dietrich M, Seifert B, Oertli D, Metzger U. Primary anastomosis vs Hartmann’s procedure in patients undergoing emergency left colectomy for perforated diverticulitis. Colorectal Dis. 2010;12(1):54–60.
Trenti L, Biondo S, Golda T, Monica M, Kreisler E, Fraccalvieri D, et al. Generalized peritonitis due to perforated diverticulitis: Hartmann’s procedure or primary anastomosis? Int J Colorectal Dis. 2011;26(3):377–84.
Schilling MK, Maurer CA, Kollmar O. Primary vs. secondary anastomosis after sigmoid colon resection for perforated diverticulitis (HincheyStage III and IV): a prospective outcome and cost analysis. Dis Colon Rectum. 2001;44:699–703. discussion 703–705.
Breitenstein S, Kraus A, Hahnloser D. Emergency left colon resection for acute perforation: primary anastomosis or Hartmann’s procedure? A casematched control study. World J Surg. 2007;31:2117–24.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332.
Silva MA, Ratnayake G, Deen KI. Quality of life of stoma patients: temporary ileostomy versus colostomy. World J Surg. 2003;27(4):421–4.
Amelung FJ, Van ’t Hullenaar CP, Verheijen PM, Consten EC. Ileostomy versus colostomy: which is preferable? Ned Tijdschr Geneeskd. 2017;161:D788.
Elliott TB, Yego S, Irvin TT. Five-year audit of the acute complications of diverticular disease. Br J Surg. 1997;84:535–9.
Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger P, Buchli C, et al. A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg. 2012;256(5):819–26. discussion 826–7.
Sandblom G. Editorial: incisional and stomal hernia prevention. Front Surg. 2018;5:46.
Bhangu A, Nepogodiev D, Futaba K. Systematic review and meta-analysis of the incidence of incisional hernia at the siteof stoma closure. World J Surg. 2012;36:973–83.
Schreinemacher MH, Vijgen GH, Dagnelie PC, Bloemen JG, Huizinga BF, Bouvy ND. Incisional hernias in temporarystoma wounds: a cohort study. Arch Surg. 2011;146(1):94–9. https://doi.org/10.1001/archsurg.2010.281.
Diener MK, Voss S, Jensen K. Elective midline laparotomy closure: the inline systematic review and meta-analysis. Ann Surg. 2010;251:843–56.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
F. Pizza, D. D’Antonio, M. Arcopinto, C. Dell’Isola and A. Marvaso declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. This article does not contain any studies with animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pizza, F., D’Antonio, D., Arcopinto, M. et al. Comparison of Hartmann’s procedure vs. resection with primary anastomosis in perforated sigmoid diverticulitis: a retrospective single-center study. Eur Surg 52, 179–186 (2020). https://doi.org/10.1007/s10353-020-00633-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-020-00633-4