Abstract
Despite remarkable progress in imaging modalities and surgical management, persistence or recurrence of primary hyperparathyroidism (PHPT) still occurs in 2.5–5% of cases of PHPT. The aim of this review is to expose the management of persistent and recurrent hyperparathyroidism. A literature search was performed on MEDLINE using the search terms “recurrent” or “persistent” and “hyperparathyroidism” within the past 10 years. We also searched the reference lists of articles identified by this search strategy and selected those we judged relevant. Before considering reoperation, the surgeon must confirm the diagnosis of PHPT. Then, the patient must be evaluated with new imaging modalities. A single adenoma is found in 68% of cases, multiglandular disease in 28%, and parathyroid carcinoma in 3%. Others causes (<1%) include parathyromatosis and graft recurrence. The surgeon must balance the benefits against the risks of a reoperation (permanent hypocalcemia and recurrent laryngeal nerve palsy). If surgery is necessary, a focused approach can be considered in cases of significant imaging foci, but in the case of multiglandular disease, a bilateral neck exploration could be necessary. Patients with multiple endocrine neoplasia syndromes are at high risk of recurrence and should be managed regarding their hereditary pathology. The cure rate of persistent-PHPT or recurrent-PHPT in expert centers is estimated from 93 to 97%. After confirming the diagnosis of PHPT, patients with persistent-PHPT and recurrent-PHPT should be managed in an expert center with all dedicated competencies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Persistent primary hyperparathyroidism (P-PHPT) is defined as hypercalcemia within 6 months after primary surgery for PHPT, whereas recurrent primary hyperparathyroidism (R-PHPT) is defined as hypercalcemia which presents after at least 6 months of normocalcemia following successful primary surgery for PHPT [1]. Usually, patients are diagnosed with P-PHPT soon after the initial surgery, and R-HPT typically occurs much later than 6 months in the majority of cases. The rate of P-PHPT or R-PHPT used to be approximately 30% in the 1990’s. Nowadays, despite remarkable progress in parathyroid preoperative imaging modalities and surgical management, persistence or recurrence still occurs in 2.5–5% of cases of sporadic PHPT [2, 3]. Before considering reoperation, the surgeon must confirm the diagnosis of PHPT. After confirmation of persistence or recurrence, adequate management should be proposed to the patient regarding the operative risks of redo surgery [permanent hypocalcemia and recurrent laryngeal nerve (RLN) palsy] and expected benefits. A single adenoma is found in 68% of cases, multiglandular disease in 28%, and parathyroid carcinoma in 3%. Others causes (<1%) include parathyromatosis and graft recurrence [4]. Finally, the cure rate of P-PHPT or R-PHPT in expert/specialist centers is estimated to range from 93 to 97% [5, 6]. Patients with multiple endocrine neoplasia (MEN) syndromes are at high risk of recurrence and should be managed regarding their hereditary pathology.
In this review, we will first present the predictive factors and the different causes of P-PHPT and R-PHPT reported in the literature, then we will focus on the appropriate preoperative imaging modalities, and finally, we will discuss the role and place of surgical management comparing its risk–benefit profile to other strategies (medical or invasive). A specific discussion relating to the management of patients with MEN syndromes is also included.
Methods
A literature search was performed on MEDLINE using the search terms “recurrent” or “persistent” and “hyperparathyroidism”. We largely selected publications in the past 10 years, but did not exclude commonly referenced and highly regarded older publications. Using “recurrent” OR “persistent” AND “hyperparathyroidism” 224 articles were identified, with 17 reviews. We also searched the reference lists of articles identified by this search strategy and selected those we judged relevant. Review articles and international guidelines are cited to provide readers with additional details and more references which are outside the scope of this review.
Results and discussion
Diagnostic confirmation of PHPT
PHPT is characterized by an increased level of total calcium associated with an increased or maladjusted level of parathormone (PTH) without vitamin D deficiency and without hypocalciuria. Before any reoperation for R-PHPT or P-PHPT, the diagnosis of PHPT must be confirmed. Indeed, it has been reported that 2–10% of surgical failures could be attributed to an incorrect diagnosis [7]. The main differential diagnoses of PHPT are isolated hyperparathormonemia associated with vitamin D deficiency, renal dysfunction, or benign familial hypocalciuric hypercalcemia (BFHH). In the former, although hyperparathormonemia can be seen in vitamin D deficiency, it is associated with low or normal serum calcium. Secondary hyperparathormonemia can be associated with renal failure, but calcium levels are generally low initially. The surgical management of secondary hyperparathyroidism usually requires subtotal parathyroidectomy. Thus, in cases of unknown renal failure prior to the initial surgery, the patient may not have had the appropriate surgical procedure, which explains the persistence of HPT. Finally, PHPT must be differentiated from BFHH. BFHH is defined as hypercalcemia in association with normal or slightly raised levels of PTH with hypocalciuria. In BFHH, biochemical investigations usually show a mildly elevated calcium level, and decreased urinary calcium: the increased calcium level is due to a loss-of-function mutation of the calcium sensing receptor (CASR) resulting in an inability to accurately sense elevations in circulating calcium as a consequence, the PTH level is not appropriately decreased in response to hypercalcemia. The abnormal calcium sensor also leads to an abnormal regulation of urinary calcium which is found to be decreased (despite the elevated plasma calcium level). Urinary calcium should thus be performed systematically in any patient with a suspicion of PHPT. In the Fourth International Workshop on the Management of Asymptomatic Primary Hyperparathyroidism, they suggested the use of urinary calcium and calcium-creatinine clearance ratio (UCCR) to differentiate BFHH from PHPT with an UCCR less than 0.01 in favor of BFHH. Unfortunately, UCCR has limitations (vitamin D deficiency, renal failure, and African-American origins) and patients with BFFH have been misdiagnosed to have PHPT in more than 20% of cases [8, 9]. Moreover, 20% of patients with BFHH have UCCR greater than 0.01. BFHH must be investigated with in all cases of PHPT with decreased urinary calcium, as patients with this condition do not benefit from surgical parathyroidectomy.
Thus, reviewing the patient chart prior to his first surgery is mandatory to confirm the initial diagnosis of PHPT and be sure that vitamin D deficiency, renal failure, and BFHH have been excluded.
Diagnostic confirmation of persistence or recurrence
Once the diagnostic of PHPT is established, P-PHPT should be differentiated from persistent hyperparathormonemia in which calcium levels are generally normal or low. Wang et al. reported that 15% of patients who underwent surgery for PHPT had hyperparathormonemia after primary surgery among which 66% had normocalcemia [10]. This increased level of HPT may be the first sign of P-PHPT but can also be an adaptive reaction to vitamin D deficiency or renal failure. Vitamin D deficiency accounts for 4.7% of patients with supposed R-PHPT or P-PHPT and thus should be systematically investigated in these cases. Renal failure has been associated with hyperparathormonemia and its role in post-operative elevated PTH has been confirmed [11]. The increased level of PTH can be a secondary response to bone remineralization, mainly due to hungry bone syndrome which can lead to hyper stimulation of residual parathyroid tissue. However, persistent hyperparathormonemia can also be the first sign of P-PHPT and R-PHPT. It is difficult to estimate how many patients with persistent hyperparathormonemia will develop hyperparathyroidism and how long they must be followed. Thus, if no adaptive reaction has been found, patients must be followed for several months or years with repeated measures of calcium, PTH, vitamin D, creatinine level, and calciuria. No consensus exists on how to follow up these patients, but annual monitoring of calcium and PTH levels is recommended [11, 12]. As we reported above, P-PHPT or R-PHPT must be differentiated from BFHH. In 1980, Marx et al. reported that at least 9% of patients referred after unsuccessful parathyroidectomy had BFHH [13]. As the level of calcium is rarely above 2.7 mmol/l, there is no indication to perform surgery, and the use of genetic testing (CASR, AP2S1, and GNA11 genes) to differentiate BFHH from PHPT is necessary especially in patients with UCCR between 0.01 and 0.02.
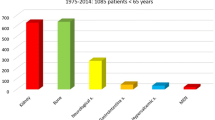
Predictive factors of R-PHPT or P-PHPT
Yeh et al. analyzed the effect of demographics, clinical features, and hospital volume on P-PHPT and R-PHPT on a large series of patient who underwent parathyroidectomy for PHPT irrespective of surgical technique [mini-invasive parathyroidectomy (MIP) or bilateral neck exploration (BNE)]. Age greater than 70 years, low hospital volume (lower than 50 cases per year) or low surgeon experience, and equivocal sestamibi results were significantly associated with P-PHPT or R-PHPT [2]. Obesity and ASA3 have also been reported as predictive factors of P-PHPT and R-PHPT [14]. Those predictive parameters have been confirmed by other studies [15, 16]. These findings indicate that parathyroid surgery should be performed in high volume centers by experienced surgeons with adequate imaging modalities.
R-PHPT occurs more frequently in patients with double adenoma than with single adenoma (7.3 vs 1.7%) but is most frequent in patients with MGD [17]. Thus, the initial parathyroid pathology of the patient influences the risk of recurrence.
With the increase of MIP, studies have evaluated the impact of surgical strategy on the cure rates of PHPT in comparison to BNE. Both MIP and BNE have an excellent cure rate. In their recent meta-analysis, Ospina et al. reported that the cure rate was 98% with BNE and 97% with MIP, with lower morbidity for MIP [18]. In a large series of patients, Lee et al. reported that the major cause of operative failure was the surgeon’s failure to identify abnormal glands and the absence of performing BNE in case of an inadequate decrease in intra-operative PTH levels (IOPTH) [19]. The use of IOPTH improves the outcome of MIP to 99% success rate if MIAMI criteria are respected and if BNE is performed when IOPTH does not drop, although there appears to be an increased rate of P-PHPT in cases of conversion from MIP to BNE [20, 21]. Thus, when MIP and BNE criteria are respected (single adenoma on ultrasound and scintigraphy, use of IOPTH during MIP, conversion from MIP to BNE if IOPTH does not drop-off), surgical strategy does not seem to influence the rate of R-PHPT or P-PHPT. Data are summarized in Table 1.
Reasons for failed primary surgery in PHPT
The major cause of P-PHPT is the inability of the surgeon to locate the abnormal gland either in ectopic or in eutopic position. In 1996, Clark et al. reported that reasons for failed parathyroid operations included an adenoma in ectopic position in 53% patients and adenoma in normal position missed during the previous surgery in 7%. More recently, in their retrospective study, Nawrot et al. reported that a missed parathyroid gland was found on reoperation in eutopic position 55.5% patients and in ectopic position in 44.3% patients. Of the ectopic glands, approximately 50% were cervical ectopy and 50% were mediastinal ectopy (including intrathymic) [4, 22]. Parathyroid glands are derived from the third and fourth branchial arch and their locations in eutopic and in ectopic positions are highly correlated with their embryologic migration. The prevalence of ectopic parathyroid is about 2–43% in anatomical series and up to 16% in patients with PHPT [23]. The endocrine surgeon must be well aware of parathyroid anatomy and embryology to be able to know where to look for a parathyroid adenoma at primary surgery and thus to avoid P-PHPT. Another cause of P-PHPT is the incomplete resection of multiple abnormal glands which can occur in 37% of cases [22]. Supernumerary parathyroid glands are rare (from 5 to 13% supernumerary glands are found in anatomical series [24] and generally in ectopic positions but can lead to P-PHPT. Rarely, incomplete resection of parathyroid carcinoma can lead to P-PHPT with the need to perform a delayed thyroid resection and regional clearance.
R-PHPT implies that the patient has been cured during 6 months after primary surgery. The main cause of R-PHPT is MGD in case of familial history of PHPT due to regrowth of a previously resected parathyroid or recurrence in a hyperfunctional graft after total parathyroidectomy or autotransplantation. The development of a second adenoma in a previously normal gland is rare and is most commonly observed in patients with a history of neck radiation [7]. R-PHPT also occurs in 20–50% of parathyroid carcinomas due to local recurrence or distant metastasis after successful primary surgery [25]. Finally, parathyromatosis is a rare cause of R-PHPT. It consists of hyper functioning parathyroid tissues scattered throughout the neck mainly due to intraoperative tissue spillage at the primary surgery. Few cases have been reported [26, 27]. Management involves complete surgical extirpation of all identifiable residual foci parathyroid tissue [28].
Localization studies
Once the diagnosis is confirmed, the surgeon must define the surgical strategy for reoperation. It has been proven that localization studies before reoperation improve the cure rate of P-PHPT or R-PHPT [5], although the cure rate of reoperation by an expert surgeon (when the first surgery has been done by an inexperienced surgeon) is up to 95% without any localization studies [29]. Ultrasound and parathyroid scintigraphy are the first-line imaging modalities, and for some the only imaging modalities used with a sensitivity of 73–90% and 78–90%, respectively, and a positive predictive value (PPV) of 86–93% and 83–94% [5, 30]. Recently, a 123I/MIBI subtraction protocol was found to be more accurate than dual phase protocol in the localization of parathyroid tissue prior to reoperation [31]. The uses of hybrid cameras provide both anatomical and functional information. Shin et al. have shown that the combination of imaging studies and the clinical scenario (single adenoma or MGD suspected on clinical history by an expert surgeon) is the most accurate approach to cure the patient with a PPV of 95% in single adenoma and 100% in MGD [6]. The concordance of both imaging modalities should be considered as sufficient for guiding reoperation. If parathyroid scintigraphy shows a major ectopia in the mediastinum, a computed tomography (CT) or magnetic resonance imaging (MRI) is required to confirm the results of scintigraphy and guide the surgeon towards the more suitable surgical approach (cervical vs thoracic). CT and especially 4D CT can also be useful in cases of negative, discordant or indeterminate results on the first-line imaging studies [32]. Finally, 11C-methionine PET can also been performed but requires an on-site cyclotron due to the short half-life of carbon-11. More recently, 18F-choline has shown very promising results at diagnosis and in patients with persistent/recurrent disease [33, 34]. If all non-invasive procedures are negative, selective venous sampling with assessment of PTH can correctly localize the anatomical region where the lesion is located with sensitivity from 73 to 100% [35, 36]. When used together, imaging techniques correctly identify abnormal glands in nearly 95% of cases and can reduce the operating time and operative morbidity.
Treatment
Is surgery necessary and when?
Once the diagnosis is confirmed, the surgeon must evaluate the benefits and the risks of a reoperation. Not every patients needs to be re-operated and sometimes a mild asymptomatic hypercalcemia is better than a definitive hypocalcemia or an RLN palsy. Very early reoperation can be performed (24–72 h) if the adenoma has not been found, but in that situation, imaging modalities must be redone immediately after the primary surgery and the location must be unequivocal. In our experience, early surgery is generally performed in cases of low-quality preoperative imaging and the possibility to perform imaging modalities in an expert center (for example, MIBI subtraction if simple isotope MIBI has been performed before) and a reoperation by an experienced surgeon within 24 h. Most often, early reoperations for P-PHPT are not required. The surgeon needs to take the time to reevaluate the patient history, confirm the diagnosis, and to perform localization studies. Moreover, reoperation in the first weeks after primary surgery may present higher morbidity due to inflammatory scarring. Thus, reoperations for P-PHPT are generally performed after a delay of 4–6 months [7] .
Morbidity of redo surgery
Before the use of MIP, reoperation for P-PHPT or R-PHPT had a risk of permanent hypoparathyroidism greater than 10% and a risk of permanent RLN palsy 5 times higher than in primary surgery [37]. Nowadays, the morbidity of redo surgery has decreased but is not insignificant. Transient RLN palsy occurs in 11% of case, while permanent RLN palsy occurs in 6–9% of cases. The increased risk of RLN palsy compared to the initial surgery calls for precise preoperative assessment of the state of the vocal cords. Nerve monitoring may be useful in parathyroid reoperation. Post-operative hypocalcemia is reported in 81% of cases, while permanent hypocalcemia occurs in 3–13% of cases [4, 31]. Other complications such as wound infection or bleeding are rare either in the initial or redo surgery.
Which surgical approach and the use of IOPTH
The surgical management will depend on the result of imaging modalities and suspected parathyroid disease. In case of suspected MGD, a revision of cervicotomy with bilateral neck exploration must be performed, but in cases of a single adenoma, a focused approach can be proposed. En-bloc resection is essential in cases of parathyromatosis, recurrent parathyroid carcinoma, intrathyroid adenoma, or graft recurrence. In cases of negative imaging modalities, the surgeon must evaluate the benefit of a reoperation. Mediastinal explorations using a thoracic access, even thoracoscopic, are too invasive to be recommended. In the neck, this depends on the suspected disease. When a MGD is highly suspected, revision cervicotomy with BNE can be proposed, because localization studies are often negative. However, in cases of a probable missed adenoma, the success of reoperation is doubtful when imaging studies are negative and many surgeons prefer to wait and observe [7]. Studies have reported that IOPTH accurately predicted cure in 97–100% of cases and failure in 78% of cases of reoperation for P-PHPT or R-PHPT [31, 32]. Thus, the use of IOPTH is highly recommended in reoperation for R-PHPT or P-PHPT.
Decisional management of P-PHPT and R-PHPT is summarized in Fig. 1.
Revision of cervicotomy and Bilateral Neck Exploration
Revision of cervicotomy and BNE is a long and technically challenging procedure and should be performed by an expert surgeon with full knowledge of anatomy and parathyroid embryology. It is the standard reoperation in case of suspected MGD. The surgeon must study the previous surgery and pathology reports to know which parathyroids have previously been removed. Localization studies can be very helpful but are more likely to be negative in case of MGD. Ideally, all parathyroid tissue must be seen which indicates that the surgeon must also look for intrathymic parathyroids. Due to post-operative fibrosis, the infra-hyoid muscles might have fused to the underlying thyroid and trachea. Thus, even if the previous incision is generally used, a lateral approach is frequently employed, by mobilizing the plane between the lateral side of the infra-hyoid muscles and the medial side of the ipsilateral sternocleidomastoid muscle [1]. Revision of cervicotomy and BNE carries a high risk of post-operative hypoparathyroidism. The need to perform an autotransplantation of parathyroid must be discussed with the patient pre-operatively. Richards et al. suggested the use of IOPTH to decide when to perform autotransplantation with a decrease PTH cutoff of 84% [31]. This should be confirmed in further studies. Transplantation of hyperfunctional tissue can result in recurrent disease in 7–17% of patients and grafts may fail to function in 6–50% of transplanted tissue. Most surgeons routinely abstain from immediate autotransplantation at the time of the parathyroidectomy; however, it can be done if the surgeon is certain that successive procedures have led to the excision of at least three normal glands if the gland found is a solitary adenoma and if there is no available facility for cryopreservation [7].
Focused approach
A single missed parathyroid adenoma is the most common cause for a failed primary parathyroid operation [38]. With the increased utility and accuracy of imaging modalities, most parathyroid reoperations can be performed by a unilateral or focused approach leading to a minimized risk of permanent RLN palsy and decreased prevalence of permanent hypoparathyroidism [38]. The superiority of minimally invasive parathyroidectomy compared with BNE has been demonstrated. In their retrospective study, Nawrot et al. performed a focused approach in 66.3% of cases with a cure rate of 94% [4]. To perform a focused approach, it is usually recommended to have 2 concordant imaging modalities. A cervical focused approach can be performed in cases of a single adenoma missed during the initial surgery (P-PHPT), a recurrence due to a single adenoma or a recurrence of MGD on a parathyroid stump. A lateral approach is generally preferred but a thyrothymic approach can also be performed in cases of intrathymic adenoma. The initial incision is used but the infra-hyoid muscles are divided as low as possible to allow direct access to the thyrothymic ligaments and thus to avoid any dissection near the thyroid or the trachea. Mediastinal approaches are indicated in l–2% of mediastinal adenomas, which are virtually inaccessible by cervicotomy [7]. Mediastinal adenomas are a good indication for video-assisted thoracoscopy and are mostly between the aorto-pulmonary windows. The use of IOPTH and nerve monitoring is highly recommended in focused approaches.
En-bloc resection
In cases of parathyromatosis, all remaining parathyroid tissues must be removed. IOPTH can be useful, but these patients are difficult to cure. Moreover, it can be very difficult to separate the RLN from parathyroid tissues, and thus, the patient should be aware of the high risk of RLN palsy [28].
The treatment of choice for parathyroid carcinoma is en-bloc resection (thyroid lobectomy associated with central lymph node resection), but the diagnosis is generally made after primary surgery and thus delayed thyroid lobectomy can be performed to avoid recurrence [39]. Recurrence of parathyroid carcinoma occurs in about 50% of cases. Recently, Young et al. suggested the absence of benefit of extensive resection [40]. Nevertheless, it is still recommended to remove all tissues en-bloc, together with invaded neighboring organs if necessary [7].
Graft recurrence after autotransplantation can be observed in secondary hyperparathyroidism. Before considering a reoperation in the graft (generally in the arm), one should be sure that there is no cervical or mediastinal recurrence. Radio-guided parathyroidectomy can be useful [41]. Reoperations on grafts are very difficult, because grafts are often embedded in muscle and it is difficult to evaluate the volume of tissue that has to be removed or left. Thus, there is a high risk of permanent hypocalcemia as most surgeons prefer to remove as much as transplanted tissue as possible.
Intrathyroid adenomas are rare (0.5–3.5%) and may require an en-bloc lobectomy resection [42]. In the majority of cases, adenomas are located just under thyroid capsule and thus can be removed without performing a lobectomy. In cases of true intrathyroid adenoma, the surgeon should not hesitate to perform thyroid lobectomy and thus to avoid potential parathyromatosis or P-PHPT. Intra-operative ultrasound can be useful in this setting. In contrast, a prophylactic lobectomy should not be performed in P-PHPT or R-PHPT if the missing adenoma is not found.
Other treatments modalities and medical treatment
Besides surgical exploration, other invasive treatments have recently been investigated. Yu et al. reported the potential benefit of microwave ablation in patients with recurrent or persistent secondary hyperparathyroidism in an 11 case retrospective study [43]. Ospina et al. reported the efficacy of percutaneous parathyroid ethanol ablation in patients with R-PHPT and MEN 1 with a low rate of complications [44]. These treatments require further investigations prior to widespread clinical uptake or consideration.
Finally, the use of Cinacalcet in secondary or sometimes in primary hyperparathyroidism is now well established. Its use in P-PHPT or R-PHPT should be reserved for patients who are at high surgical risk [45]. In contrast, several studies have shown the benefit of Cinacalcet in kidney transplanted patients with persistent or recurrent hyperparathyroidism [46, 47]. In those cases, surgery should not be the first option. Cinacalcet is usually well-tolerated, even if mild or rarely strong intolerance with nausea can be observed. The treatment can be given on a long-term basis, with biochemical follow-up based on calcium and PTH levels.
The particular case of P-PHPT and R-PHPT in MEN
The initial surgical management of MEN1 and MEN2 patients is essential to avoid persistent or recurrent hyperparathyroidism. Indeed, in MEN1, persistence or recurrence occurs from 9% to more than 50% cases depending on the primary surgical strategy [45, 48]. Recurrence can occur either on the parathyroid stump or on the autotransplanted graft but can also be the consequence of a supernumerary parathyroid [49]. The indications for reintervention are the same as those for PHPT. Imaging modalities (US and MIBI) are necessary prior to surgery even in the previous subtotal parathyroidectomy, although they often show the hypertrophied half-gland remnant with a sensitivity to localize all remnant parathyroids (parathyroid stump, supernumerary gland) of 61% [50]. Indeed, several studies showed that localization studies failed to identify all residual parathyroid tissue. Thus, a positive parathyroid scintigraphy for a single lesion does not imply that a focused approach will be successful, particularly if thymectomy was not performed in the first surgery [45, 50]. Reoperations are technically difficult, because most of these patients will have had previous subtotal parathyroidectomy with an increased risk of permanent hypoparathyroidism or RLN palsy. Thus, BNE or a focused approach in MEN patients with persistent or recurrent hyperparathyroidism is still debated. The surgeon must evaluate the benefit of a minimally invasive approach (if single focus is located on localization studies) with low risk of complications but with the risk of a second persistence compared to a systematic BNE with higher morbidity but a low risk of second recurrence. The initial surgery must be taken into account to decide the surgical strategy.
Conclusions
P-PHPT and R-PHPT occur in 2.5–5% of sporadic hyperparathyroidism. After confirming the diagnosis of PHPT, the patient must be evaluated with new imaging modalities and the surgeon must balance the benefits against the risks of a reoperation. If surgery is necessary, a focused approach can be considered in cases of significant imaging foci (with strong correlation between two concordant imaging studies), but in the case of MGD, a BNE could be necessary. The patient must be well informed of the potential complications, particularly permanent RLN palsy and permanent hypoparathyroidism. MEN syndrome patients should be managed according to the initial surgery. In any cases, patients with P-PHPT and R-PHPT should be managed in an expert/specialist center (with all dedicated competencies) by experienced surgeons.
References
Udelsman R (2011) Approach to the patient with persistent or recurrent primary hyperparathyroidism. J Clin Endocrinol Metab 96(10):2950–2958
Yeh MW, Wiseman JE, Chu SD, Ituarte PHG, Liu I-LA, Young KL et al (2011) Population-level predictors of persistent hyperparathyroidism. Surgery 150(6):1113–1119
Venkat R, Kouniavsky G, Tufano RP, Schneider EB, Dackiw APB, Zeiger MA (2012) Long-term outcome in patients with primary hyperparathyroidism who underwent minimally invasive parathyroidectomy. World J Surg 36(1):55–60
Nawrot I, Chudziński W, Ciąćka T, Barczyński M, Szmidt J (2014) Reoperations for persistent or recurrent primary hyperparathyroidism: results of a retrospective cohort study at a tertiary referral center. Med Sci Monit Int Med J Exp Clin Res 20:1604–1612
Hessman O, Stålberg P, Sundin A, Garske U, Rudberg C, Eriksson L-G et al (2008) High success rate of parathyroid reoperation may be achieved with improved localization diagnosis. World J Surg 32(5):774–781
Shin JJ, Milas M, Mitchell J, Berber E, Ross L, Siperstein A (2011) Impact of localization studies and clinical scenario in patients with hyperparathyroidism being evaluated for reoperative neck surgery. Arch Surg 146(12):1397–1403 (Chic Ill 1960)
Henry J-F (2010) Reoperation for primary hyperparathyroidism: tips and tricks. Langenbecks Arch Surg 395(2):103–109
Eastell R, Brandi ML, Costa AG, D’Amour P, Shoback DM, Thakker RV (2014) Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the Fourth International workshop. J Clin Endocrinol Metab 99(10):3570–3579
Eldeiry LS, Ruan DT, Brown EM, Gaglia JL, Garber JR (2012) Primary hyperparathyroidism and familial hypocalciuric hypercalcemia: relationships and clinical implications. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 18(3):412–417
Wang TS, Ostrower ST, Heller KS (2005) Persistently elevated parathyroid hormone levels after parathyroid surgery. Surgery 138(6):1130–1136
Denizot A, Pucini M, Chagnaud C, Botti G, Henry JF (2001) Normocalcemia with elevated parathyroid hormone levels after surgical treatment of primary hyperparathyroidism. Am J Surg 182(1):15–19
Oltmann SC, Maalouf NM, Holt S (2011) Significance of elevated parathyroid hormone after parathyroidectomy for primary hyperparathyroidism. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 17(Suppl 1):57–62
Marx SJ, Stock JL, Attie MF, Downs RW, Gardner DG, Brown EM et al (1980) Familial hypocalciuric hypercalcemia: recognition among patients referred after unsuccessful parathyroid exploration. Ann Intern Med 92(3):351–356
Kuo LE, Wachtel H, Fraker D, Kelz R (2014) Reoperative parathyroidectomy: who is at risk and what is the risk? J Surg Res 191(2):256–261
Chen H, Wang TS, Yen TWF, Doffek K, Krzywda E, Schaefer S et al (2010) Operative failures after parathyroidectomy for hyperparathyroidism: the influence of surgical volume. Ann Surg 252(4):691–695
McIntyre CJ, Allen JLY, Constantinides VA, Jackson JE, Tolley NS, Palazzo FF (2015) Patterns of disease in patients at a tertiary referral centre requiring reoperative parathyroidectomy. Ann R Coll Surg Engl 97(8):598–602
Alhefdhi A, Schneider DF, Sippel R, Chen H (2014) Recurrent and persistence primary hyperparathyroidism occurs more frequently in patients with double adenomas. J Surg Res 190(1):198–202
Singh Ospina NM, Rodriguez-Gutierrez R, Maraka S, Espinosa de Ycaza AE, Jasim S, Castaneda-Guarderas A et al (2016) Outcomes of parathyroidectomy in patients with primary hyperparathyroidism: a systematic review and meta-analysis. World J Surg 40(10):2359–2377
Lee S, Ryu H, Morris LF, Grubbs EG, Lee JE, Harun N et al (2014) Operative failure in minimally invasive parathyroidectomy utilizing an intraoperative parathyroid hormone assay. Ann Surg Oncol 21(6):1878–1883
Barczynski M, Konturek A, Cichon S, Hubalewska-Dydejczyk A, Golkowski F, Huszno B (2007) Intraoperative parathyroid hormone assay improves outcomes of minimally invasive parathyroidectomy mainly in patients with a presumed solitary parathyroid adenoma and missing concordance of preoperative imaging. Clin Endocrinol (Oxf) 66(6):878–885
Hughes DT, Miller BS, Park PB, Cohen MS, Doherty GM, Gauger PG (2013) Factors in conversion from minimally invasive parathyroidectomy to bilateral parathyroid exploration for primary hyperparathyroidism. Surgery 154(6):1428–1435
Shen W, Düren M, Morita E, Higgins C, Duh QY, Siperstein AE et al (1996) Reoperation for persistent or recurrent primary hyperparathyroidism. Arch Surg Chic Ill 1960 131(8):861–869
Noussios G, Anagnostis P, Natsis K (2012) Ectopic parathyroid glands and their anatomical, clinical and surgical implications. Exp Clin Endocrinol Diabetes Off J Ger Soc Endocrinol Ger Diabetes Assoc 120(10):604–610
Lappas D, Noussios G, Anagnostis P, Adamidou F, Chatzigeorgiou A, Skandalakis P (2012) Location, number and morphology of parathyroid glands: results from a large anatomical series. Anat Sci Int 87(3):160–164
Mehta A, Patel D, Rosenberg A, Boufraqech M, Ellis RJ, Nilubol N et al (2014) Hyperparathyroidism-Jaw Tumor syndrome: results of surgical management. Surgery 156(6):1315–1325
Hage MP, Salti I, Fuleihan GEH (2012) Parathyromatosis: a rare yet problematic etiology of recurrent and persistent hyperparathyroidism. Metabolism 61(6):762–775
Lee PC, Mateo RB, Clarke MR, Brown ML, Carty SE (2001) Parathyromatosis: a cause for recurrent hyperparathyroidism. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 7(3):189–192
Jain M, Krasne DL, Singer FR, Giuliano AE (2017) Recurrent primary hyperparathyroidism due to Type 1 parathyromatosis. Endocrine 55(2):643–650. doi:10.1007/s12020-016-1139-7
Ippolito G, Palazzo FF, Sebag F, Henry JF (2007) Long-term follow-up after parathyroidectomy for radiation-induced hyperparathyroidism. Surgery 142(6):819–822
Feingold DL, Alexander HR, Chen CC, Libutti SK, Shawker TH, Simonds WF et al (2000) Ultrasound and sestamibi scan as the only preoperative imaging tests in reoperation for parathyroid adenomas. Surgery 128(6):1103–1110
Richards ML, Thompson GB, Farley DR, Grant CS (2008) Reoperative parathyroidectomy in 228 patients during the era of minimal-access surgery and intraoperative parathyroid hormone monitoring. Am J Surg 196(6):937–943
Yen TWF, Wang TS, Doffek KM, Krzywda EA, Wilson SD (2008) Reoperative parathyroidectomy: an algorithm for imaging and monitoring of intraoperative parathyroid hormone levels that results in a successful focused approach. Surgery 144(4):611–621
Cham S, Sepahdari AR, Hall KE, Yeh MW, Harari A (2015) Dynamic Parathyroid Computed Tomography (4DCT) Facilitates Reoperative Parathyroidectomy and Enables Cure of Missed Hyperplasia. Ann Surg Oncol 22(11):3537–3542
Traub-Weidinger T, Mayerhoefer ME, Koperek O, Mitterhauser M, Duan H, Karanikas G et al (2014) 11C-methionine PET/CT imaging of 99mTc-MIBI-SPECT/CT-negative patients with primary hyperparathyroidism and previous neck surgery. J Clin Endocrinol Metab 99(11):4199–4205
Seehofer D, Steinmüller T, Rayes N, Podrabsky P, Riethmüller J, Klupp J et al (2004) Parathyroid hormone venous sampling before reoperative surgery in renal hyperparathyroidism: comparison with noninvasive localization procedures and review of the literature. Arch Surg Chic Ill 1960 139(12):1331–1338
Sun PY, Thompson SM, Andrews JC, Wermers RA, McKenzie TJ, Richards ML et al (2016) Selective parathyroid hormone venous sampling in patients with persistent or recurrent primary hyperparathyroidism and negative, equivocal or discordant noninvasive imaging. World J Surg 40(12):2956–2963
Grant CS, Thompson G, Farley D (1960) van Heerden J (2005) Primary hyperparathyroidism surgical management since the introduction of minimally invasive parathyroidectomy: Mayo Clinic experience. Arch Surg Chic Ill 140(5):472–479
Jaskowiak N, Norton JA, Alexander HR, Doppman JL, Shawker T, Skarulis M et al (1996) A prospective trial evaluating a standard approach to reoperation for missed parathyroid adenoma. Ann Surg. 224(3):308–321
Cetani F, Pardi E, Marcocci C (2016) Update on parathyroid carcinoma. J Endocrinol Invest 39(6):595–606
Young S, Wu JX, Li N, Yeh MW, Livhits MJ (2016) More extensive surgery may not improve survival over parathyroidectomy alone in parathyroid carcinoma. Ann Surg Oncol 23(9):2898–2904
Ardito G, Revelli L, Giustozzi E, Giordano A (1009) Radioguided parathyroidectomy in forearm graft for recurrent hyperparathyroidism. Br J Radiol 2012(85):e1–e3
Wheeler MH, Williams ED, Wade JS (1987) The hyperfunctioning intrathyroidal parathyroid gland: a potential pitfall in parathyroid surgery. World J Surg 11(1):110–114
Yu M-A, Yao L, Zhang L, Peng L, Zhuo L, Zhang Y et al (2016) Safety and efficiency of microwave ablation for recurrent and persistent secondary hyperparathyroidism after parathyroidectomy: a retrospective pilot study. Int J Hyperth Off J Eur Soc Hyperthermic Oncol North Am Hyperth Group 32(2):180–186
Singh Ospina N, Thompson GB, Lee RA, Reading CC, Young WF (2015) Safety and efficacy of percutaneous parathyroid ethanol ablation in patients with recurrent primary hyperparathyroidism and multiple endocrine neoplasia type 1. J Clin Endocrinol Metab 100(1):E87–E90
Salmeron MDB, Gonzalez JMR, Sancho Insenser J, Fornos JS, Goday A, Perez NMT et al (2010) Causes and treatment of recurrent hyperparathyroidism after subtotal parathyroidectomy in the presence of multiple endocrine neoplasia 1. World J Surg 34(6):1325–1331
Paschoalin RP, Torregrosa J-V, Sánchez-Escuredo A, Barros X, Durán CE, Campistol JM (2012) Cinacalcet treatment for stable kidney transplantation patients with hypercalcemia due to persistent secondary hyperparathyroidism: a long-term follow-up. Transplant Proc 44(9):2588–2589
Serra AL, Savoca R, Huber AR, Hepp U, Delsignore A, Hersberger M et al (2007) Effective control of persistent hyperparathyroidism with cinacalcet in renal allograft recipients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 22(2):577–583
Pieterman CRC, van Hulsteijn LT, den Heijer M, van der Luijt RB, Bonenkamp JJ, Hermus ARMM et al (2012) Primary hyperparathyroidism in MEN1 patients: a cohort study with longterm follow-up on preferred surgical procedure and the relation with genotype. Ann Surg 255(6):1171–1178
Kim BK, Lee J, Sun WY (2016) Recurrent hyperparathyroidism due to proliferation of autotransplanted parathyroid tissue in a multiple endocrine neoplasia type 2A patient. Ann Surg Treat Res 91(3):145–148
Shepherd JJ, Burgess JR, Greenaway TM, Ware R (2000) Preoperative sestamibi scanning and surgical findings at bilateral, unilateral, or minimal reoperation for recurrent hyperparathyroidism after subtotal parathyroidectomy in patients with multiple endocrine neoplasia type 1. Arch Surg Chic Ill 1960 135(7):844–848
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Research involving Human Participants and/or Animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Funding
This study has received no funding.
Rights and permissions
About this article
Cite this article
Guerin, C., Paladino, N.C., Lowery, A. et al. Persistent and recurrent hyperparathyroidism. Updates Surg 69, 161–169 (2017). https://doi.org/10.1007/s13304-017-0447-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-017-0447-7