Abstract
Accumulating evidence indicates that enhancer of zeste homolog 2 (EZH2) promotes the metastatic ability of solid tumors, but the role of EZH2 in extramedullary infiltration (EMI) in acute myeloid leukemia (AML) has not been thoroughly explored. In the present study, we investigated the possible association between EZH2 and EMI. We found that the messenger RNA (mRNA) and protein expression levels of EZH2 in AML patients were both significantly higher than in idiopathic thrombocytopenic purpura (ITP) patients. Furthermore, a positive correlation between EZH2 mRNA expression and percentage of peripheral blood blasts wa s found in AML patients (r = 0.404, p = 0.009). The migratory capacities of Kasumi-1 and HL-60, which both show a high level of EZH2 expression, were markedly higher than those of U937 and KG-1α. In contrast, silencing of EZH2 resulted in reduction in proliferation and migration ability and an increase in apoptosis. The latter observation was accompanied by reduced expression of associated proteins p-ERK, p-cmyc, and matrix metalloproteinase 2 (MMP-2) and an increase in epithelial cadherin (E-cadherin). These data suggest that higher expression of EZH2 may be associated with extramedullary infiltration in acute myeloid leukemia and affect pathogenesis via activation of the p-ERK/p-cmyc/MMP-2 and E-cadherin signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
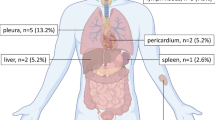
As the most common type of adult acute leukemia, acute myeloid leukemia (AML) is a malignant proliferative disease that occurs in hematopoietic stem/progenitor cells. It is characterized by unlimited proliferation of leukemia cells originating from the myeloid lineage and often accompanied by infiltration in extramedullary tissues. Thirty to forty percent of newly diagnosed AML patients present with extramedullary infiltration (EMI), of which common sites include skin, lymph nodes, gingiva, liver, spleen, and central nervous system [1]. EMI is reported to be more common in M4/M5 subtypes (French-American-British (FAB) classification) and associated with poorer treatment response [2–4], especially in AML patients with the t(8;21) translocation [5].
Enhancer of zeste homolog 2 (EZH2), known as the catalytic subunit of polycomb repressive complex 2 (PRC2), has intrinsic histone methyltransferase activity and is involved in trimethylated modification of H3K27 [6–8]. It is well established that EZH2 plays an important role in cell proliferation, embryonic development, X chromosome inactivation, maintenance of stem cells, and oncogenesis through transcriptional inhibition of target genes [9–12]. An enhancing effect of EZH2 up-regulation on proliferation was first demonstrated in hematopoietic cells [13]. Subsequently, overexpression of EZH2 has been found in a variety of human malignancies, including esophageal neoplasm, lung cancer, prostate cancer, and breast cancer, and is closely correlated with tumor aggressiveness, metastasis, and poor prognosis [14–17].
In malignant myeloid disorders, current research shows that EZH2 overexpression in high-risk myelodysplastic syndrome (MDS) and AML transformed from MDS confers poor prognosis [18]. In addition, high EZH2 has been found to be associated with high lactate dehydrogenase (LDH), high WBC count, and poor prognosis in bone marrow tissues from patients with de novo AML [19]. However, whether and how EZH2 is involved in the EMI process of leukemia cells remains largely unexplored. Therefore, to this end, we measured expression of EZH2 in bone marrow cells and tissues from patients with AML. We used four different AML cell lines (U937, KG-1α, Kasumi-1, and HL-60) as models to verify the effect of EZH2 expression on cell migration ability. Finally, we used EZH2 knockdown to investigate this gene’s role in the growth and migration of Kasumi-1 cells and the associated molecular mechanisms.
Material and methods
Patient samples
Patients enrolled in this study were diagnosed between October 2005 and February 2013 in Nanfang Hospital (Guangzhou, China). Bone marrow mononuclear cells were obtained from 42 cases of de novo AML patients (including 37cases of hospitalized patients and 5 cases of outpatients), and bone marrow paraffin-embedded trephine biopsies were analyzed from another 23 AML patients (including 18 cases of de novo AML and 5 cases of relapsed AML). Bone marrow mononuclear cells from 10 normal donors, 10 cases of idiopathic thrombocytopenic purpura (ITP) patients, and bone marrow paraffin-embedded biopsies from 5 patients with ITP were used as controls. All patients were diagnosed by morphological analysis, immunohistochemical staining or immunophenotyping, or combinations thereof. Subtypes were classified according to the FAB classification and World Health Organization criteria. Informed consent was obtained from all patients according to institutional guidelines and in accordance with the Declaration of Helsinki. Patients’ characteristics are listed in Table 1.
Cell lines and cell culture
The human AML cell lines U937, HL-60, KG-1α, and Kasumi-1 were purchased from Institutes for Biological Sciences Cell Resource Center, Chinese Academy of Sciences (Shanghai, China). U937, HL-60, and KG-1α were cultured in Roswell Park Memorial Institute (RPMI)-1640 medium (Hyclone, MA, USA) supplemented with 10 % heat-inactivated fetal bovine serum (Hyclone). Kasumi-1 was cultured in RPMI-1640 medium (Gibco, USA), supplemented with 20 % heat-inactivated fetal bovine serum (Hyclone) and 100 μg/L L-glutamine. All cell lines were cultured in medium supplemented with 100 U/mL penicillin and 100 μg/mL streptomycin and incubated in a humidified atmosphere of 5 % CO2 at 37 °C.
Reagents
RNA extraction reagent kit, PrimerScript reverse transcription (RT) reagent kit, and polymerase chain reaction (PCR) kit were purchased from Dalian Biotechnology Company (TaKaRa, China). Primers for EZH2 and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) were designed and synthesized by Shanghai Yingjun Biotechnology Company (Yingjun, China). Nuclear protein/cytosolic protein kit and monoclonal antibodies against GAPDH were purchased from FDbio Science. Monoclonal antibodies against EZH2, H3, H3K27me3, ERK, p-ERK, amyloid precursor protein (APP), and matrix metalloproteinase 2 (MMP-2) and horseradish peroxidase-conjugated mouse anti-rabbit IgG were purchased from Cell Signaling Technology Company (CST, USA). Monoclonal antibodies against c-myc and p-cmyc were purchased from Abcam. A monoclonal antibody against epithelial cadherin (E-cadherin) was purchased from Abclonal (Boston, USA). Goat anti-rabbit IgG was purchased from Dako (DAKO, Denmark). Diaminobenzidine (DAB), as the developing agent, was purchased from Beijing Zhongshan Golden Bridge Biotechnology (Zhongshan Jinqiao, China). The Cell Counting Kit-8 (CCK-8) was purchased from DOJINDO (Shanghai, China).
Lentivirus conduction and infection
Three individual EZH2-specific small interfering RNAs (siRNAs) were used for EZH2 knockdown in Kasumi-1 (siRNA-1 AACAGCTGCCTTAGCTTCA, siRNA-2 AACAGCTCTAGACAACAAA, and siRNA-3 GGATAGAGAATGTGGGTTT). A non-targeting scrambled RNA GV118 vector was used as a negative control (TTCTCCGAACGTGTCACGT). All siRNAs were purchased from Genechem (Shanghai, China). Kasumi-1 was planted in 6-well plates. We then used the three different siRNAs and the negative control lentivirus to transfect the Kasumi-1 cells, marked siRNA-1, siRNA-2, siRNA-3, and NC groups, respectively. After a 72-h incubation at 37 °C, we captured images of the cells under a fluorescence microscope. We selected the green fluorescent protein (GFP)-positive cells for culturing with flow cytometry. The gene silencing effects were confirmed by real-time reverse transcription quantitative polymerase chain reaction (RT-qPCR) and Western blot. The siRNA with the greatest gene silencing effect was chosen for subsequent experiments.
RNA isolation and RT-qPCR
The expression of EZH2 in AML primary cells and cell lines was measured by RT-qPCR. RNA extraction and RT-qPCR were performed as described previously [20]. PrimerScript RT Reagent Kit (TaKaRa) was used to synthesize cDNA. The real-time PCR was carried out using a SYBR Green PCR mix in Applied Biosystems 7500 system. Primers used were as follows: EZH2 5′-TTGTTGGCGGAAGCGTGTAAAATC-3′ (forward primer) and 5′-TCCCTAGTCCCGCGCAATGAGC-3′ (reverse primer) and GAPDH 5′-GTGAAGGTCGGAGTCAACG-3′ (forward primer) and 5′-CTGGGGAAGTAACTGGAGT-3′ (reverse primer).
Western blot
The protein expression levels of EZH2, H3, HEK27me3, ERK, p-ERK, c-myc, p-cmyc, MMP-2, E-cadherin, APP, and GAPDH in AML cell lines were detected by Western blot (WB). WB was performed as described previously by our group [20]. All experiments were performed in triplicate.
Immunohistochemistry
Immunohistochemistry (IHC) was employed to evaluate the protein expression level of EZH2 in paraffin-embedded biopsies. Antigen retrieval was undertaken by microwaving in citrate buffer for 10 min. Hydrogen peroxide at 0.3 % was used to block activity of endogenous peroxidase for 15 min, and normal goat serum was used to block non-specific binding site for 20 min. The tissue slides were then incubated with EZH2 antibody (1:80 dilution) overnight at 4 °C in a moist chamber. Subsequently, the slides were incubated with the secondary antibody for 1 h at room temperature. Diaminobenzidine was used as chromogen substrate and counterstained with Mayer’s hematoxylin. PBS was used in place of the primary antibody as a negative control, and known positive tissues from breast cancer were used as positive controls. A semi-quantitative integral analysis system including staining intensity and percentage of positive cells was adopted to determine the expression of EZH2 protein. Nuclear staining intensity was scored as follows: 0, no visible staining; 1, weak; 2, moderate; and 3, strong. One-thousand tumor cells were selected randomly from 10 microscopic fields at higher magnification to calculate the average percentage of positive cells. The percentage of tumor cells was scored as follows: 0, none; 1, 1–25 %; 2, 26–50 %; 3, 51–75 %; and 4, 76–100 %. The score of intensity multiplied by the score of percentage counts was used as the final score. For further analysis, final scores of 0–3 and 4–12 were considered to indicate low and high expression levels, respectively. This semi-quantitative integral analysis system is in keeping with that published by Yan-Wei Lin et al. [21].
CCK-8 assay
The capacity for cellular proliferation was measured using a CCK-8 assay. Cells were divided into the three following groups: untreated Kasumi-1 cells (wild), siRNA/EZH2-treated Kasumi-1 cells (siEZH2), and scrambled siRNA-treated Kasumi-1 cells (NC). Cells were plated at 104 per well in 96-well plates with three replicate wells for each condition. After culturing for 0, 24, 48, 72, and 96 h, 10 μL of 5 mg/mL CCK-8 was added to each well. After that, cells were incubated in 5 % CO2 at 37.0 °C for 3 h, after which the optical density was determined with a microplate reader at 450 nm. Each experiment was performed in triplicate.
Cell migration assay
Capacity of cell migration was evaluated by using a transwell migration chamber with millipore membranes. The cell migration assay was performed as described previously [20]. In addition, migrating cells attached to the lower surface of the filter were fixed and stained with hematoxylin for counting. We then captured images of the cells on the lower chamber and the membranes. Each migration experiment was repeated three times.
Flow cytometry analysis of apoptosis
The Annexin V-PI Apoptosis Detection Kit (NanJing KeyGen Biotechnology, NanJing, China) was used to detect and quantify apoptosis by flow cytometry. The three groups of cells (wild, NC, and siEZH2 groups) were washed with 1× binding buffer, and then, 5 μL of Annexin V was added to 100 μL of the cell suspension. After incubating for 15 min, we added 5 μL of propidium iodide for 20 min and analyzed using a FACScan flow cytometer Becton (Dickinson, CA, USA). Each experiment was repeated three times.
Statistical analysis
Statistical analysis was performed with the statistical package SPSS 20.0 (IBM Corp., Armonk, NY). Data from this study were reported as mean ± standard deviation, and t test or one-way ANOVA was used to assess the values and percentages between groups. The association between EZH2 protein expression and AML patients’ clinical features were assessed by the chi-squared test, Mann-Whitney U test, and Kruskal-Wallis H test. P values < 0.05 were considered significant.
Results
The expression levels of EZH2 messenger RNA and protein in 65 cases of patients with AML
RT-qPCR was used to measure the messenger RNA (mRNA) expression of EZH2 gene in bone marrow mononuclear cells from 42 cases of de novo AML patients; 10 cases of normal donors and 10 cases of ITP patients were as the control. As Fig. 1 shows, the expression of EZH2 mRNA in AML patients (1.69 ± 0.72) was significantly higher than the normal control group (0.88 ± 0.66, p = 0.002) and the ITP group (1.06 ± 0.55, p = 0.001). Further analysis showed that there was no difference between ITP group and control group (p = 0.549). In addition, the levels of EZH2 protein in bone marrow biopsies from 23 patients with AML were evaluated by IHC staining. According to the semi-quantitative integral analysis system described earlier, high expression of EZH2 was observed in 14/23 (60.9 %) of the bone marrow biopsies from patients with AML but none of the biopsies from ITP patients (Fig. 2). These observations support a role for EZH2 leukemia pathogenesis.
Immunohistochemical staining of EZH2 protein in bone marrow biopsies from 23 cases of patients with AML and ITP (SP, ×400). a HE stain of bone marrow biopsies from idiopathic thrombocytopenic purpura (ITP) patients. b HE stain of bone marrow biopsies from AML patients. c Low expression of EZH2 protein in ITP biopsies. d High expression of EZH2 protein in AML biopsies
Association of EZH2 expression with clinical features and prognosis in AML
On analysis of 42 cases of de novo AML, a significant positive correlation was observed between EZH2 mRNA expression and percentage of peripheral blood blasts (r = 0.404, p = 0.009; Fig. 3). To further investigate the relationship between EZH2 expression and clinical features, the two groups of AML patients (one group of 42 cases and the second group of 23 cases) were combined. A total of 65 cases were then divided into two groups according to level of expression of EZH2 mRNA or protein as follows: EZH2 mRNA above the median or high expression of EZH2 protein was defined as the high expression group, and the opposite was defined as the low expression group. A summary of our analysis of the relationship between EZH2 expression and clinical characteristics is shown in Table 2. High EZH2 expression was closely correlated with male gender, higher percentage of peripheral blood blasts, higher white blood cell counts, a higher level of lactate dehydrogenase, and the occurrence of leukemic extramedullary infiltration (p < 0.05) but showed no correlation with age, percentage of bone marrow blasts, FAB subtype, or cytogenetic risk group (in the latter analysis, patients without cytogenetic data were excluded; p > 0.05). When we compared EZH2 expression in the EMI group with that in the group without EMI, we found a higher average expression in the EMI group and a higher percentage of patients with high expression of EMI patients (84.4 % of EMI patients versus 25 % of non-EMI patients in high EZH2 expression group). CR rate and CR duration were used to reflect the response to chemotherapy. The 21 patients who died or were lost to follow-up before consolidation therapy were excluded from the study. The patients with high EZH2 expression had similar CR rates after 2 cycles compared to the patients with low expression (100.0 versus 88.9 %, respectively; p = 0.054). However, 46.2 % of AML patients relapsed within 6 months of achieving first CR in the high EZH2 expression group, which was significantly more than in the low EZH2 expression group (16.7 %, p = 0.042). When followed up for 12 months, the patients with high EZH2 expression remained more likely to relapse than patients with low EZH2 expression (61.5 versus 16.7 %, p = 0.003). This observation suggests that the expression level of EZH2 may indicate a high tumor burden; furthermore, EZH2 may be an important predictive marker of EMI.
Effect of EZH2 expression on migration in AML cell lines
Transcription and protein levels of EZH2 in the AML cell lines U937, KG-1α, Kasumi-1, and HL60 were measured by RT-qPCR and WB. As shown in Fig. 4a, expression of EZH2 mRNA in U937 cells was 0.04 ± 0.03 by one-way ANOVA analysis, which was significantly lower than in Kasumi-1 (0.11 ± 0.01, p = 0.000) and HL60 (0.14 ± 0.03, p = 0.000) cells. The EZH2 mRNA expression in KG-1α (0.06 ± 0.03) cell was also lower than Kasumi-1 (p = 0.001) and HL60 (p = 0.000) cells, but there was no difference in expression between U937 and KG-1α and between Kasumi-1 and HL60 (p > 0.05). The same findings were also obtained by immunoblotting (Fig. 4b). Images in Fig. 4c were taken from the lower chamber of the migration assay at the time of 18 h. Consistent with the trend of EZH2 expression, statistical analysis revealed that lower chamber cell counts in U937 and KG-1α were significantly lower than for Kasumi-1 and HL60 (3.78 ± 2.11 × 104, 5.00 ± 2.52 × 104, 8.06 ± 2.19 × 104, and 9.28 ± 1.95 × 104 for U937, KG-1α, Kasumi-1, and HL-60, respectively; p < 0.05; Fig. 4d).
Expression of EZH2 and migration capacity in AML cell lines. a Transcriptional levels of EZH2 in Kasumi-1 and HL-60 cells were significantly higher than in U937 and KG-1α cells (p < 0.05). b EZH2 protein in different AML cell lines (U937, KG-1α, Kasumi-1, and HL-60). The expressions of EZH2 in Kasumi-1 and HL-60 cells were higher than in U937 and KG-1α cells (p < 0.05). c Cell migration detected by transwell migration chamber (SP, ×100). d The cell counts of the lower chamber were more in Kasumi-1 and HL-60 cells indicating greater migratory capacity (p < 0.05)
EZH2 knockdown by RNA interference
To further explore the role and mechanism by which EZH2 performs in AML cells, we used specific siRNAs to knock out EZH2 expression in Kasumi-1. Figure 5 shows Kasumi-1 cells 72 h after transduction with siRNA-1, siRNA-2, siRNA-3, and the scrambled control siRNA. We selected the GFP-positive cells for culturing with flow cytometry. Then, RT-qPCR and WB were used to measure mRNA and protein expression levels of EZH2, respectively (Fig. 5B e, f). We found that EZH2 mRNA expression was significantly down-regulated following exposure to siRNA-1 (0.009 ± 0.0004, p = 0.000), siRNA-2 (0.0284 ± 0.0030, p < 0.001), and siRNA-3 (0.007 ± 0.0001, p < 0.05; Fig. 5B e). EZH2 protein expression level was also down-regulated in these three groups (Fig. 5B f). We found that siRNA-3 produced the highest efficiency of EZH2 silencing; therefore, we choose siRNA-3 with which to perform subsequent experiments (henceforth termed the siEZH2 group). mRNA and protein expression levels of EZH2 were significantly reduced in siEZH2 group compared to wild and NC groups (0.124 ± 0.007, 0.115 ± 0.009, and 0.007 ± 0.0001 for expressions of EZH2 mRNA in wild, NC, and siEZH2 groups, respectively; **p < 0.001; Fig. 5B g, h).
A Lentivirus transduction and infection. Images of lentivirus transduction in Kasumi-1 taken under a fluorescence microscope. a–d Three siRNAs targeting different sequences of EZH2 (siRNA-1, siRNA-2, and siRNA-3) and a negative control lentivirus, respectively (SP, ×200). B RT-qPCR and Western blot to measure EZH2 gene and protein expressions, respectively, after silencing of EZH2 in Kasumi-1. e, f The mRNA and protein expression levels of EZH2 were significantly reduced after depletion of EZH2 by siRNA-1 and siRNA-3 (p < 0.001); furthermore, the knockout efficiency of EZH2 in siRNA-3 group is the most obvious (*p < 0.05). g, h The mRNA and protein expression levels of EZH2 were significantly down-regulated in the siEZH2 group compared to the untreated (wild) and NC groups (**p < 0.001)
EZH2 associated with migration of AML cells
It has been reported that EZH2 promotes invasion and metastasis in many solid tumor types such as esophageal, lung, prostate, breast, and renal cell carcinoma. There are certain parallels between metastasis in solid tumor and EMI in AML; therefore, we performed a cell migration assay to investigate the relationship between migration and EZH2 in AML cells. In our study, a transwell migration chamber was used to test the migration ability of Kasumi-1 with and without expression of EZH2. Figure 6a–c shows images captured in the lower compartments of the invasion chambers; we found that the cell number in lower chamber for siEZH2-transduced Kasumi-1 cells was significantly reduced compared to the wild and NC cells (p < 0.05; Fig. 6a–d). When the ratio of migrated to non-migrated cells was compared, the cells in the siEZH2 arm showed a significantly lower ratio than either of the control arms (p < 0.05; Fig. 6d). Finally, the siEZH2 group had markedly fewer cells on the membrane than the control groups (Fig. 6e–h). Therefore, our data suggest that EZH2 may be involved in the migration of AML cells, thus supporting a role for EZH2 in EMI in AML patients.
The effects of siEZH2 on Kasumi-1 cell migration measured using a transwell migration chamber (SP, ×200). a–c Cells in the lower chamber of transwell plates of wild, NC, and siEZH2 groups, respectively. d When comparing the ratio of migrated cells, we found that the ratio of siEZH2 group was lower than the other groups. e–g The number of cells in the wild, NC, and siEZH2 groups, respectively, on the membrane after staining with hematoxylin. h When comparing the number of cells on the membrane, we found that the number of cells of siEZH2 group was significantly less than the two control groups (*p < 0.05)
EZH2 promotes proliferation and induces apoptosis of AML cells
To investigate whether a high level of EZH2 is associated with disease aggressiveness in AML, we used the CCK-8 assay and flow cytometry to measure proliferation and apoptosis in Kasumi-1 cells with and without EZH2 expression, respectively. We observed that proliferative capacity was significantly lower after knocking down EZH2 (p < 0.05; Fig. 7a). In addition, the ratio of apoptosis in siEZH2-treated cells (27.00 ± 1.45) was higher than in untreated cells (6.91 ± 0.23, p = 0.000) and those treated with a scrambled siRNA (7.60 ± 0.78, p = 0.000; Fig. 7b–d).
CCK-8 assay to measure the proliferation and apoptosis of Kasumi-1 and Western blot to examine the related protein. a The proliferation of the siEZH2 group was significantly lower than that of the other groups (p < 0.05). b–d Apoptosis was increased after silencing of EZH2 (p < 0.05). e EZH2 promotes migration via regulating the signaling pathway of p-ERK/p-cmyc/MMP-2 and E-cadherin. Western blot analysis of GAPDH, EZH2, H3, H3K27me3, ERK, p-ERK, c-myc, p-cmyc, MMP-2, and APP expressions after knockdown of EZH2. We show that H3K27me3, p-ERK, p-cmyc, and MMP-2 are up-regulated and E-cadherin increased markedly after down-regulation of EZH2
EZH2 regulates migration of AML cells via the EZH2/p-ERK/p-cmyc/MMP-2 and E-cadherin signaling pathways
To investigate the possible mechanism via which EZH2 is involved in migration, proliferation, and apoptosis, we measured the level of several proteins associated with these processes by WB. Several studies have reported that MMP-2 was associated with migration [22, 23]. We have previously shown that the APP can promote extramedullary infiltration of AML1/ETO+ leukemic cells by activating the p-ERK/c-myc/MMP-2 signaling pathway [20]. We therefore assessed the level of all these proteins in EZH2-positive and EZH2-negative AML cells in the present study. We found that H3K27me3 is remarkably down-regulated by knockdown of EZH2. In addition, p-ERK, p-cmyc, and MMP-2 are significantly reduced, while levels of ERK, c-myc, and APP remain essentially unchanged. Furthermore, E-cadherin, a protein associated with invasion and metastasis of malignant tumors, is obviously up-regulated (Fig. 7e). These findings suggest that EZH2 may modulate migration via the p-ERK/p-cmyc/MMP-2 and E-cadherin signaling pathways in AML cells.
Discussion
EZH2, as a catalytic subunit of PRC2, can repress its target genes transcriptionally by trimethylation of lysine 27 on histone H3 (H3K27), thereby promoting proliferation and aggressiveness of cancer cells [6, 7, 24]. A variety of studies show that EZH2 is overexpressed in prostate, breast, lung, esophageal, and kidney cancers and its expression is associated with tumor malignancy, tumor invasion, metastasis, and poor outcome [14–17, 25]. In addition, EZH2 has been found to be overexpressed in AML, lymphoma, and high-risk myelodysplastic syndrome (MDS) [18, 26]. Fiskus et al. [24] reported that 3-Deazaneplanocin A (DZNep), a non-specific inhibitor of EZH2, can down-regulate EZH2 and induce apoptosis in AML cell lines and primary cells. Tanaka et al. [6] observed that EZH2 can promote leukemogenicity by promoting differentiation blockage and found that inhibiting the expression of EZH2 decreased cell proliferation in AML. These findings suggest that EZH2 may contribute to disease aggressiveness in AML by enhancing cell migration and proliferation.
EMI is one of the common clinical characteristics of acute leukemia. Due to differences in definitions and inclusive criteria of EMI, the association between EMI and outcome remains a controversial issue. However, the majority of studies have shown that the occurrence of EMI is closely associated with low CR rate, high risk of recurrence, and poor prognosis [18]. In this study, we found that patients expressing a high level of EZH2 had a higher likelihood of EMI at diagnosis and were also more likely to have relapsed at 6- and 12-month time points.
In the present study, we show that EZH2 mRNA and protein expressions in bone marrow mononuclear cells were significantly higher in AML than the control group. Furthermore, we detected up-regulation of EZH2 in AML patients with EMI. Our observation of overexpression of EZH2 in AML pathogenesis is consistent with the results of previous research [19, 27]. Tanaka et al. [6] found that EZH2 can inhibit differentiation in AML by down-regulating cell cycle and differentiation-related genes such as Cdkn2a and Egr1. Chen et al. [28] found that the overexpression of EZH2 can augment leukemogenesis through methylation of H3K27. In our study, high EZH2 expression was closely correlated with male gender, a higher percent of peripheral blood blasts, higher white blood cell counts, higher level of lactate dehydrogenase, and a greater likelihood of leukemic EMI. These results provide evidence that EZH2 may play a role in leukemic EMI; however, the precise nature of this role and its molecular mechanism require further investigation.
To determine whether EZH2 expression contributes to disease progression and EMI in AML, we choose four kinds of AML cell lines for the study. We found that in concordance with higher expression of EZH2, the migratory capacities of Kasumi-1 and HL-60 were obviously greater than those of U937 and KG-1α, suggesting that EZH2 enhances cell migration. To further explore the possible mechanism and the relationship between EZH2 and migration, proliferation, and apoptosis, we silenced EZH2 in Kasumi-1 with siRNAs. We found that both the proliferation and migration abilities of Kasumi-1 were reduced and the apoptotic rate increased by knockout of EZH2. A series of studies has demonstrated that EHZ2 promotes leukemogenesis and proliferation in AML [29, 30]. These studies further support a role for EZH2 as an adverse prognostic factor in AML. Many investigators have demonstrated that H3K27me3 is down-regulated by suppression of EZH2 expression [24, 25, 30, 31]. In the current study, we demonstrate that knockdown of EZH2 inhibits trimethylation of lysine 27 on histone H3. Inhibitory effect of EZH2 on target genes is weakened; therefore, proliferation and migration were weakened and apoptosis was increased in AML cells by silencing EZH2.
As with invasion and metastasis of tumor cells, EMI is a complex multi-step process in AML. An increasing body of evidence has proven that the abnormal expression of adhesion factors in the bone marrow microenvironment in leukemia cell surface leads to a decrease in their ability to adhere and migrate, facilitating their escape into the peripheral blood. Cells then move into the endothelium with the help of chemokines, and begin to secrete cell matrix metalloproteinase to degrade the extracellular matrix (ECM), promoting their migration to extramedullary tissue [20, 22, 32]. Shin et al. found that EZH2 can depress tissue inhibitor of matrix metalloproteinases (TIMPs) and raises MMPs by methylating TIMP; the latter promoting the degradation of the extracellular matrix and enhancing the migratory ability of prostate cancer cells [23]. Furthermore, the authors confirmed that EZH2 may be a major contributor to the process of shifting the MMP/TIMP balance in favor of MMP activity, thus promoting ECM degradation and subsequent invasion of prostate cancer cells [23]. In a separate study, MMPs were found to be up-regulated and to show characteristics associated with infiltration in acute myeloid leukemia [33]. We have previously shown that APP can promote the migratory ability of AML cells by regulating the signaling pathway of p-ERK/cmyc/MMP-2 [21]. ERK is a member of the mitogen-activated protein kinase (MAPK) signaling pathway, and when stimulated, converts to p-ERK, which activates expression of MMP-2 [20]. The MAPK pathway is closely linked to the formation, proliferation, and differentiation of tumors [34]. In this study, we found a significantly reduced expression of p-ERK, p-cmyc, and MMP-2. This is consistent with published findings of solid tumors. It has been shown that EZH2 can promote the migration of cancer cells in prostate cancer and renal cell carcinoma by up-regulating the expression of E-cadherin [23, 25]. In the present study, we also found up-regulation of E-cadherin on down-regulation of EZH2.
In conclusion, our data suggest that EZH2 might be associated with the migratory ability of AML cells via the p-ERK/p-cmyc/MMP-2 and E-cadherin signaling pathways. The preliminary results of this study provide a rational basis to explore combining chemotherapy with a targeted EZH2 inhibitor in AML with EMI to improve therapeutic efficacy. Further investigation is needed to confirm the biological and clinical bases for this approach.
References
Hiçsönmez G, Çetin M, Tuncer AM, Yenicesu İ, Aslan D, Özyürek E, et al. Children with acute myeloblastic leukemia presenting with extramedullary infiltration: the effects of high-dose steroid treatment. Leukemia Res. 2004;28:25–34.
Rege K, Swansbury GJ, Atra AA, Horton C, Min T, Dainton MG, et al. Disease features in acute myeloid leukemia with t(8;21)(q22;q22). Influence of age, secondary karyotype abnormalities, CD19 status, and extramedullary leukemia on survival. Leuk Lymphoma. 2000;40:67–77.
Chang H, Brandwein J, Yi Q, Chun K, Patterson B, Brien B. Extramedullary infiltrates of AML are associated with CD56 expression, 11q23 abnormalities and inferior clinical outcome. Leukemia Res. 2004;28:1007–11.
Kobayashi R, Tawa A, Hanada R, Horibe K, Tsuchida M, Tsukimoto I. Extramedullary infiltration at diagnosis and prognosis in children with acute myelogenous leukemia. Pediatr Blood Cancer. 2007;48:393–8.
Byrd JC, Weiss RB, Arthur DC, Lawrence D, Baer MR, Davey F, et al. Extramedullary leukemia adversely affects hematologic complete remission rate and overall survival in patients with t(8;21)(q22;q22): results from Cancer and Leukemia Group B 8461. J Clin Oncol. 1997;15:466–75.
Tanaka S, Miyagi S, Sashida G, Chiba T, Yuan J, Mochizuki-Kashio M, et al. EZH2 augments leukemogenicity by reinforcing differentiation blockage in acute myeloid leukemia. Blood. 2012;120:1107–17.
Cao R, Wang L, Wang H, Xia L, Erdjument-Bromage H, Tempst P, et al. Role of histone H3 lysine 27 methylation in Polycomb-group silencing. Science. 2002;298:1039–43.
Kim SH, Yang WI, Min YH, Ko YH, Yoon SO. The role of the polycomb repressive complex pathway in T and NK cell lymphoma: biological and prognostic implications. Tumor Biol. 2015.
Xiaojing Yang RKMK, Miller PBOT: CDKN1C(p57KIP2) is a direct target of EZH2 and suppressed by multiple epigenetic mechanisms in breast cancer cells
Nakagawa S, Okabe H, Sakamoto Y, Hayashi H, Hashimoto D, Yokoyama N, et al. Enhancer of zeste homolog 2 (EZH2) promotes progression of cholangiocarcinoma cells by regulating cell cycle and apoptosis. Ann Surg Oncol. 2013;20:667–75.
Seward S, Semaan A, Qazi AM, Gruzdyn OV, Chamala S, Bryant CC, et al. EZH2 blockade by RNA interference inhibits growth of ovarian cancer by facilitating re-expression of p21waf1/cip1 and by inhibiting mutant p53. Cancer Lett. 2013;336:53–60.
Plath K, Fang J, Mlynarczyk-Evans SK, Cao R, Worringer KA, Wang H, et al. Role of histone H3 lysine 27 methylation in X inactivation. Science. 2003;300:131–5.
Visser HP, Gunster MJ, Kluin-Nelemans HC, Manders EM, Raaphorst FM, Meijer CJ, et al. The Polycomb group protein EZH2 is upregulated in proliferating, cultured human mantle cell lymphoma. Br J Haematol. 2001;112:950–8.
Yamada A, Fujii S, Daiko H, Nishimura M, Chiba T, Ochiai A. Aberrant expression of EZH2 is associated with a poor outcome and P53 alteration in squamous cell carcinoma of the esophagus. Int J Oncol. 2011;38:345–53.
Cao W, Ribeiro RO, Liu D, Saintigny P, Xia R, Xue Y, et al. EZH2 promotes malignant behaviors via cell cycle dysregulation and its mRNA level associates with prognosis of patient with non-small cell lung cancer. Plos One. 2012;7:e52984.
Kong D, Heath E, Chen W, Cher ML, Powell I, Heilbrun L, et al. Loss of let-7 up-regulates EZH2 in prostate cancer consistent with the acquisition of cancer stem cell signatures that are attenuated by BR-DIM. Plos One. 2012;7:e33729.
Tiwari N, Tiwari VK, Waldmeier L, Balwierz PJ, Arnold P, Pachkov M, et al. Sox4 is a master regulator of epithelial-mesenchymal transition by controlling EZH2 expression and epigenetic reprogramming. Cancer Cell. 2013;23:768–83.
Xu F, Li X, Wu L, Zhang Q, Yang R, Yang Y, et al. Overexpression of the EZH2, RING1 and BMI1 genes is common in myelodysplastic syndromes: relation to adverse epigenetic alteration and poor prognostic scoring. Ann Hematol. 2011;90:643–53.
Wu SH, Zheng CP, Xu J. A preliminary study on the relationship between EZH2 and microRNA-101 and the prognostic role of EZH2 in acute myeloid leukemia. Zhonghua Xue Ye Xue Za Zhi. 2012;33:232–5.
Jiang L, Yu G, Meng W, Wang Z, Meng F, Ma W. Overexpression of amyloid precursor protein in acute myeloid leukemia enhances extramedullary infiltration by MMP-2. Tumor Biol. 2013;34:629–36.
Lin Y, Ren L, Xiong H, Du W, Yu Y, Sun T, et al. Role of STAT3 and vitamin D receptor inEZH2-mediated invasion of human colorectal cancer. J Pathol. 2013;230:277–90.
Wang C, Chen Z, Li Z, Cen J. The essential roles of matrix metalloproteinase-2, membrane type 1 metalloproteinase and tissue inhibitor of metalloproteinase-2 in the invasive capacity of acute monocytic leukemia SHI-1 cells. Leukemia Res. 2010;34:1083–90.
Shin YJ, Kim J. The role of EZH2 in the regulation of the activity of matrix metalloproteinases in prostate cancer cells. Plos One. 2012;7:e30393.
Fiskus W, Wang Y, Sreekumar A, Buckley KM, Shi H, Jillella A, et al. Combined epigenetic therapy with the histone methyltransferase EZH2 inhibitor 3-deazaneplanocin a and the histone deacetylase inhibitor panobinostat against human AML cells. Blood. 2009;114:2733–43.
Liu L, Xu Z, Zhong L, Wang H, Jiang S, Long Q, et al. Enhancer of zeste homolog 2 (EZH2) promotes tumour cell migration and invasion via epigenetic repression of E-cadherin in renal cell carcinoma. BJU Int. 2015;117(2):351–62.
Lee SCW, Phipson B, Hyland CD, Leong HS, Allan RS, Lun A, et al. Polycomb repressive complex 2 (PRC2) suppresses E-myc lymphoma. Blood. 2013;122:2654–63.
Grubach L, Juhl-Christensen C, Rethmeier A, Olesen LH, Aggerholm A, Hokland P, et al. Gene expression profiling of Polycomb, Hox and Meis genes in patients with acute myeloid leukaemia. Eur J Haematol. 2008;81:112–22.
Chen J, Li J, Han Q, Sun Z, Wang J, Wang S, et al. Enhancer of zeste homolog 2 is overexpressed and contributes to epigenetic inactivation of p21 and phosphatase and tensin homolog in B-cell acute lymphoblastic leukemia. Exp Biol Med. 2012;237:1110–6.
Nishioka C, Ikezoe T, Yang J, Yokoyama A. Tetraspanin family member, CD82, regulates expression of EZH2 via inactivation of p38 MAPK signaling in leukemia cells. Plos One. 2015;10:e125017.
Zhou J, Bi C, Cheong LL, Mahara S, Liu SC, Tay KG, et al. The histone methyltransferase inhibitor, DZNep, up-regulates TXNIP, increases ROS production, and targets leukemia cells in AML. Blood. 2011;118:2830–9.
Fiskus W, Pranpat M, Balasis M, Herger B, Rao R, Chinnaiyan A, et al. Histone deacetylase inhibitors deplete enhancer of zeste 2 and associated polycomb repressive complex 2 proteins in human acute leukemia cells. Mol Cancer Ther. 2006;5:3096–104.
Kirmizis A, Bartley SM, Kuzmichev A, Margueron R, Reinberg D, Green R, et al. Silencing of human polycomb target genes is associated with methylation of histone H3 Lys 27. Genes Dev. 2004;18:1592–605.
Janowska-Wieczorek A, Marquez LA, Matsuzaki A, Hashmi HR, Larratt LM, Boshkov LM, et al. Expression of matrix metalloproteinases (MMP-2 and -9) and tissue inhibitors of metalloproteinases (TIMP-1 and -2) in acute myelogenous leukaemia blasts: comparison with normal bone marrow cells. Br J Haematol. 1999;105:402–11.
Yasuda T. MAP kinase cascades in antigen receptor signaling and physiology. Curr Top Microbiol Immunol. 2015;393:211–31.
Authors’ contributions
Fanyi Meng, Qiuhua Zhu, and Lingxiu Zhang conceptualized and designed the study, collected and analyzed data, and drafted the paper; Qiuhua Zhu and Lingxiu Zhang performed the experiments. Qiuhua Zhu and Lingxiu Zhang contributed equally to this work. Fanyi Meng and Hongsheng Zhou helped to revise the paper. All authors read and approved the final manuscript.
Funding
This work was supported by Guangzhou Science and Technology Plan Projects (No. 2013J4100109) and the Specialized Research Fund for the Doctoral Program of Higher Education (No. 20124433110001). National Natural Science Foundation of China (No. 81500138), Natural Science Foundation of Guangdong Province, China (No. 2014A030313270), Medical Research Foundation of Guangdong Province, China (No. B2014250).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Qiuhua Zhu and Lingxiu Zhang are co-first author.
Rights and permissions
About this article
Cite this article
Zhu, Q., Zhang, L., Li, X. et al. Higher EZH2 expression is associated with extramedullary infiltration in acute myeloid leukemia. Tumor Biol. 37, 11409–11420 (2016). https://doi.org/10.1007/s13277-016-4983-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-016-4983-4