Abstract
CXC chemokines and their cognate receptors have been implicated wildly in cancer pathogenesis. In the present study, we report a critical cause relationship between CXCR4 expression and tumorigenesis in the setting of human esophageal squamous cell carcinoma (ESCC). In ESCC cells, CXCR4 expression was significantly higher than in human esophageal epithelial cells (HEEC). Reduction of CXCR4 in ESCC cells reduced cell proliferation and invasion in vitro and tumor growth in vivo. Among the potential downstream targets of CXCR4-CXCL12 are RhoA, Rac-1, and Cdc42, which are likely to contribute to the invasiveness of ESCC cells. Finally, we found that CXCR4-CXCL12/AKT axis regulates RhoA, Rac-1, and Cdc42 to modulate cell invasion and tumor metastasis. Together, these results demonstrate a role for CXCR4 in ESCC metastasis and progression and suggest potential targets for therapeutic intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal cancer (EC) is one of the most aggressive malignancies worldwide. It is often far advanced at the time of detection. Only a small number of patients are considered for curative resection and long-term survival. Despite important refinements of surgical technique and significant progress in perioperative care, EC remains highly lethal. The overall 5-year survival rate after esophagectomy is 30 %, and about half of the patient exhibit recurrence within 2 to 3 years after surgery. The main pattern of recurrence is locoregional recurrence [1, 2]. In China, EC is the fifth most common cancer and the fourth leading cause of cancer-related deaths [3]. Interestingly, EC has different characteristics in Eastern and Western countries: 90 % of EC in China is esophageal squamous cell carcinoma (ESCC), whereas in Western countries, adenocarcinoma is predominant [4]. This implies that there might be differences in the prognosis and therapeutic strategies for EC patients in China and Western countries.
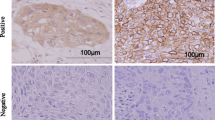
The tumor metastatic process is quite similar to the “homing” behavior of hematopoietic stem cells to the bone marrow. In the previous study, our group found that CXCR4 was highly expressed in ESCC and correlated with MMP-9, VEGF, clinicopathological features, and prognosis [5]. Moreover, we further confirmed heterogeneous expression of CXCR4 in esophageal squamous cell cancer cell lines (KYSE70, Eca109, and CaEs-17) by flow cytometry analysis. CXCR4-positive cells showed stronger migration ability than CXCR4-negative cells. In immunohistochemistry assay, CXCR4 was heterogeneously expressed in tumor tissues [6]. This suggested that CXCR4 might play an important role in esophageal squamous cell cancer. Although the function of CXCR4 has been revealed gradually [7, 8], little is known about the mechanism of CXCR4 in esophageal squamous cell cancer. In the present study, the possible role of CXCR4 in the progression and metastasis of ESCC was investigated.
Materials and methods
Human esophageal epithelial cell (HEEC) line (Cell Bank, Type Culture Collection of Chinese Academy of Science) and human esophageal squamous cell lines Eca109 and CaEs-17 (Cell Bank, Type Culture Collection of Chinese Academy of Science) were cultured in RPMI1640 with high glucose (Thermo Scientific) supplemented with 10 % fetal bovine serum (Invitrogen), 100 IU/ml penicillin G and 100 mg/ml streptomycin sulfate (Sigma-Aldrich) at 37 °C in a humidified atmosphere containing 5 % CO2.
Quantitative reverse transcription-PCR
Total RNA was isolated with Trizol (Invitrogen), digested by DNase; complementary DNA (cDNA) was synthesized from total RNA. The following primers were used for amplification: human CXCR4 forward, 5′-GAACTTCCTATGCAAGGCAGTCC-3′, reverse, 5′-CCATGATGGCTGAAACTGGAAC-3′; human β-actin forward, 5′-CTCCATCCTGGCCTCGCTGT-3′, reverse, 5′-GCTGTCACCTTCACCGTTCC-3′. Real-time PCR was performed using a SYBR premix Ex TaqII (Takara) and ABI 7900HT Fast Real-Time PCR System (Applied Biosystems). All samples were performed in triplicate for three times.
Western blot analysis
Total protein was prepared from the cell lines or tissue samples. The protein samples were separated in 10 % SDS-polyacrylamide gel and electrophoretically transferred to polyvinylidene difluoride membrane (Amersham). The membrane was blotted with 10 % nonfat milk, washed, and then probed with each primary antibody that is listed in Table 1. After washing, the membrane was incubated with horseradish peroxidase-conjugated anti-mouse or rabbit or goat antibody (Amersham). Chemiluminescent detection were performed and images were captured by the ImageQuant LAS 4000 mini (GE Healthcare).
Lentivirus production and host cell infection
Transient and stable transfections with CXCR4-short hairpin RNA (shRNA) (h) lentiviral particles (sc35421-v) and control-shRNA (h) lentiviral particles (sc108080) (Santa Cruz Biotechnology, Santa Cruz, CA, USA) were carried out according to the manufacturer’s protocol. Eca109 cells were infected with lentivirus particles containing the shRNA, and stable transfectants were selected and cultured in medium containing 1 ng/μl puromycin.
The coding sequence of CXCR4 gene was amplified by PCR using Eca109 cDNA as a template with the following primers: forward, 5′-AAAGAATTCRATGGAGGGGATCAGTATATACACTT-3′, reverse, 5′-AAAGCGGCCGCTTAGCTGGAGTGAAAACTTGAAGA-3′. The resulting amplicon was then inserted into the pCDH-CMV-MCS-EF1-copGFP vector. The plasmid was confirmed by sequencing. Western blot assay was used to detect their transfection efficiency.
Invasion assay
Matrigel-coated transwell cell invasion assays were conducted using 8-μm pore size chambers (Corning Costar). 5 × 104/ml cells were added into the upper chamber of each insert coated with 150 μg Matrigel (BD Bioscience). After a 48-h of incubation at 37 °C, cells that had migrated or invaded were fixed and stained with crystal violet. In some experiments, recombinant human SDF-1α (CXCL12) (300-28A, Peprotech) was added (100 ng/ml) into both chambers at the beginning of the experiment. The cells that had migrated or invaded were counting in 5 random fields at ×200 magnification and imaged using Leica DFC200 microscope (Leica Microsystems). Three independent experiments were done in triplicate.
Cell proliferation assay
Cell proliferation was evaluated by Cell Counting Kit-8 (Dojindo Corp). One thousand cells were plated into each well of a 96-well plate. To evaluate proliferation, 10 μl of CCK-8 was added per well, and the cells were subsequently incubated for 1 h at 37 °C, and the attendance was measure at 450 nm. Three independent experiments were performed in triplicate.
Animal experiments
Mice were manipulated and housed according to the protocols approved by the Shanghai Medical Experimental Animal Care Commission. To evaluate in vivo tumor growth, 1 × 107 Eca109/shCXCR4 or control cells were suspended in 100 μl germ-free PBS and subcutaneously injected in the left flank of each mouse, respectively (five in each group, BALB/c-nu/nu mice, 4–6 weeks). Tumor sizes were measured weekly. On day 42, mice were sacrificed, and tumors were measured right after being dissected. Tumor tissue sections were prepared and stained with H&E.
Statistical analysis
Statistical analysis was performed using SPSS 20.0 software. ANOVA and Student’s t test were used to determine the statistical significance of differences between experimental groups. P < 0.05 was considered significant.
Results
Expression of CXCR4 in esophageal carcinoma cell lines
As highly expressed CXCR4 in ESCC clinical samples associates with poor prognosis [5, 6], we hypothesized that CXCR4 may play some important roles in ESCC. To test this hypothesis, we chose in vitro ESCC cell lines to analyze CXCR4’s functions and related mechanisms. We first examined the expression of CXCR4 in a HEEC cell line and two ESCC cell lines (Eca109 and CaEs-17). Consistent with our findings in ESCC clinical samples, CXCR4 is significantly overexpressed in both human ESCC cell lines compared to the HEEC cell line (Fig. 1). As Eca109 showed the highest expression of CXCR4 among those cells, we used this cell line for further analysis in this study.
CXCR4 knockdown impaired the proliferation and invasive activity of ESCC cells in vitro
Our clinical findings suggested that CXCR4 might play a role in the tumor progression of esophageal carcinoma. Therefore, we evaluated the function of CXCR4 in cell proliferation and invasion. We select Eca109 cell lines with relatively high expression of CXCR4 and HEEC cell lines with very low expression of CXCR4. Cells with CXCR4 overexpression and downregulation were established separately using a lentiviral infection system. Western blot assay was used to detect their transfection efficiency (Figs. 2a and 3a). We then detected cell growth and invasion by proliferation assay and transwell assay in these cells. As expected, we observed a significant decrease of cell proliferation and cell invasion in Eca109/shCXCR4 compared to parental cells or scramble control cells (Fig. 2b, c). Conversely, overexpression of HEEC prompts cell proliferation and invasion in HEEC-CXCR4 cells compared to parental cells or HEEC-vector cells (Fig. 3b, c).
CXCR4 expression affects the proliferation and invasive activity of esophageal carcinoma cells in vitro. a Expression of CXCR4 in Eca109 with gene downregulation. CXCR4 knockdown in Eca109 cells were detected by Western blotting. b The growth curves for Eca109, Eca109/shCtl, and Eca109/shCXCR4 cells in vitro proliferation assays. c Results of transwell assays showed the representative images of invasive Eca109/shCtl and Eca109/shCXCR4 cells. d Results of transwell assays showed the representative images of invasive Eca109/shCtl and Eca109/shCXCR4 cells treated with CXCL12 as indicated
CXCR4 overexpression affects the proliferation and invasive activity of HEEC in vitro. a Expression of CXCR4 in HEEC with gene transfection. CXCR4 overexpression in HEEC cells was detected by Western blotting. b The growth curves for HEEC, HEEC-vector, and HEEC-CXCR4 cells in vitro proliferation assays. c Result of transwell assays showed the representative image of invasive HEEC, HEEC-vector, and HEEC-CXCR4 cells
To further confirm these effects directly through CXCR4, we treated the cells with SDF-1α/CXCL12 and checked cell invasion under CXCL12 stimulation. As shown in Fig. 2d, CXCL12 could prominently promote invasion of scramble control Eca109 cells but hardly of CXCR4 knockdown cells. These results further confirmed that CXCR4 can regulate cell invasion in ESCC cells.
CXCR4 knockdown repressed the expression of RhoA, Rac-1, and Cdc42 through AKT pathways
To elucidate the mechanisms under the CXCR4-regulated cell invasion in ESCC cells, we checked the effect of CXCR4 knocking down on expression of adhesion-/invasion-associated proteins. As Rho protein family members, RhoA, Rac-1, and Cdc42, were found to be involved in regulating cell adhesion/invasion in many kinds of cancers including ESCC [9–11], we first checked the expression of RhoA, Rac-1, and Cdc42 in CXCR4 knockdown cells. Interestingly, we found that knocking down CXCR4 can significantly downregulate all those three Rho family members in Eca109 cells when compared with scramble control cells (Fig. 4a). To further confirm the regulation of Rho family members directly through CXCR4 pathway, we checked the expression of RhoA, Rac-1, and Cdc42 under CXCL12 stimulation. We found that CXCL12 (100 ng/ml) treatment markedly increased the expression of RhoA, Rac-1, and Cdc42 in Eca109 scramble control and had much less effect on Eca109 CXCR4 knockdown cells (Fig. 4c).
CXCR4 knockdown inhibition of the expression of RhoA, Rac-1, and Cdc42 with AKT pathways involved. a Expression of RhoA, Rac-1, and Cdc42 in Eca109/shCtl and Eca109/shCXCR4 cells was detected by Western blotting. b Expression and phosphorylation of AKT and ERK in Eca109/shCtl and Eca109/shCXCR4 cells were detected by Western blotting. c Eca109/shCtl and Eca109/shCXCR4 cells were treated with CXCL12 as indicated. Expression of indicated molecules was detected by Western blotting
It is already known that CXCR4 regulates AKT and ERK pathways [12, 13]. We also found that knocking down CXCR4 in Eca109 cells markedly decreased phosphorylation of AKT and ERK (Fig. 4b). As AKT and ERK pathways are involved in cell growth and migration, we wonder whether the expression change of Rho family members in CXCR4 knockdown cells is regulated by these pathways. Eca109 cells were treated with CXCL12 to stimulate CXCR4 pathway, and PI3K/AKT inhibitor LY294002 or ERK inhibitor U0126 were added into the cells to block PI3K/AKT or ERK pathways, respectively. Interestingly, we found that treatment with LY294002 but not U0126 dramatically reduced RhoA, Rac-1, and Cdc42 expression (Fig. 5b). Consistent with the downregulated RhoA, Rac-1, and Cdc42 expression, blocking AKT pathway by LY294002 also dramatically repressed cell invasion (Fig. 5a). These results suggest that the regulation of Rho family members by CXCR4 is through AKT pathway.
CXCR4-CXCL12 interaction impacts on invasive activity of esophageal carcinoma cells via modulating RhoA, Rac-1, and Cdc42, with AKT pathway involved. a Transwell assays of Eca109 cell invasion with indicated treatments. b Eca109 cells were treated with CXCL12, U0126, and LY294002 as indicated. Expression of indicated molecules was detected by Western blotting. U0126, an ERK inhibitor; LY294002, a PI3K/AKT inhibitor
CXCR4 knockdown inhibits tumorigenicity
To further explore the effect of CXCR4 knockdown in vivo, CXCR4 knockdown and control Eca109 cells were injected into nude mice. We found that Eca109/shCXCR4 formed smaller tumors than scramble control cells and wild-type cells (Fig. 6a, b). All the primary tumors were evaluated by pathologic examination. The results showed that the number of tumor cell necrosis was significantly decreased in tumor formed by CXCR4 knockdown cells (Fig. 6c). These data suggest that downregulation of CXCR4 expression inhibits tumorigenicity.
Effect of downregulation of CXCR4 on tumor growth. a The morphologic characteristics of tumor xenografts. b Significant differences in tumor volumes were revealed among the Eca109 group, control group, and Eca109/shCXCR4 group. c Representative different degrees of necrosis in tumor xenograft samples with H&E staining. d Representative expression of CXCL12 in tumor xenograft samples with Western blotting
We further checked CXCR4 expression in xenograft tumors. Consistent with the in vitro results, xenograft tumor derived from CXCR4 knockdown cells still kept the low expression of CXCR4. Interestingly, we observed a dramatic decrease of CXCL12 in the tumors derived from CXCR4 knockdown cells (Fig. 6d). These results indicated that the concentration of CXCL12 in xenograft tumors may be related with CXCR4 expression.
Discussion
EC metastases result from several critical steps involving numerous interactions between cancer cells and the host. However, the detailed mechanism that truly promotes tumor growth and metastasis is still controversial. In the present study, we showed that the expression of CXCR4 was higher in ESCC than in HEEC. Highly expressed CXCR4 can promote ESCC growth and invasion by upregulating Rho family members through active AKT pathway. Furthermore, in mouse subcutaneous xenografts, downregulation of CXCR4 led to severe suppression of tumor growth. In line with these finds, CXCL12 and CXCR4 have also been found to be the key elements in the growth of metastatic prostate cancer cells [14, 15]. Although a few studies reveal that high expression of CXCR4 predicts poor prognosis in breast cancer [16], ovarian cancer [17], malignant melanoma [18], and esophageal carcinoma [7], contrasting conclusions also exists. Spano et al. reported that strong CXCR4-positive nuclear staining was associated with a significantly better outcome in early-stage NSCLC [19], whereas in our previous study [5, 6], patients with ESCC with high expression of CXCR4 were prone to suffer from increased recurrence and reduced survival.
Our results suggested that CXCR4-CXCL12 signaling may affect esophageal carcinoma cell invasion through regulating of Rho GTPase including RhoA, Rac-1, and Cdc42. Evidence has indicated that Rho family GTPase regulates cell migration through their effects on the cytoskeleton, cell-cell, and cell-substratum adhesions, thereby influencing invasion and metastasis [20–23]. Rho family members can also influence cell survival, growth, and proliferation in vitro [24]. Lin et al. have reported that SDF-1α-induced EC cell invasion can be inhibited by suppressing the formation of the lipid raft-associated Ra-1-PI3K-AKT signaling complex [25]. Thus, RhoA, Rac-1, and Cdc42 might be the underlying mechanism for enhanced cell-cell adhesion and reduced tumor metastases resulting from CXCR4 knockdown. Moreover, the parallel dynamics of RhoA, Rac-1, and Cdc42 with AKT and ERK activation prompted us to hypothesize that AKT and ERK may be involved in the regulation of RhoA, Rac-1, and Cdc42 expression. However, we only observed the dampened AKT activities and concomitant downregulation of RhoA, Rac-1, and Cdc42 in CXCR4 knockdown cells, which coupled with reduced invasion of ESCC. We believe that ERK signaling pathway also participates in invasion of ESCC cell line; the involved downstream signaling molecules have yet to be studied. Taken together, we hypothesis that CXCR4 knockdown inhibited phosphorylation of AKT, leading to downregulation of RhoA, Rac-1, and Cdc42 whereby modulating cell invasion and inhibiting tumor metastasis.
We also showed that CXCR4 expression might be required for tumor survival. In EC cell mouse subcutaneous xenografts, we observed that interruption of CXCR4 expression led to severe suppression of tumor growth. These findings are consistent with those reported by Rubin JB et al. in which small molecular antagonists to CXCR4 impeded tumor growth in vivo [26]. Tumor growth and metastasis require a complex interplay between the local microenvironment and various cytokines—most notably chemokines. Herein, we showed that CXCL12 levels in xenograft tumors changed along with CXCR4 expression: they were significantly decreased in CXCR4-konckdown tumors. It has been reported that tumor cell production of CXCL12 weakens immunity by attracting and protecting CXCR4-expressing preDC2 cell [27]. Increasing tumor cell survival can, in turn, lead to larger tumors. The mechanism by which CXCL12 levels are regulated with CXCR4 expression remains unclear, and the exact function of CXCR4 in promoting tumor growth has yet to be identified. Additional future studies are needed to investigate in order to answer these questions.
In summary, CXCR4 is a promising marker for ESCC progression. The abrogation of CXCR4 could influence the ESCC cell phenotype including cell proliferation and cell invasion; moreover, we also observed that interruption of CXCR4 expression led to severe suppression of tumor growth in xenograft models. Collectively, these data showed that strategies designed to targeting CXCR4 may provide a venue to ameliorate tumor progression. Given the complex nature of the tumor microenvironment, targeting of components in combination might advance the field.
References
Chen G, Wang Z, Liu XY, Liu FY. Recurrence pattern of squamous cell carcinoma in the middle thoracic esophagus after modified Ivor-Lewis esophagectomy. World J Surg. 2007;31(5):1107–14.
Dresner SM, Griffin SM. Pattern of recurrence following radical oesophagectomy with two-field lymphadenectomy. Br J Surg. 2000;87(10):1426–33.
Chen WQ, Zheng RS, Zhang SW, Zeng HM, Zou XN. The incidences and mortalities of major cancers in China, 2010. Chin J Cancer. 2014;33(8):402–5.
Brown LM, Devesa SS. Epidemiologic trends in esophageal and gastric cancer in the United States. Surg Oncol Clin N Am. 2002;11(2):235–56.
Lu CL, Ji Y, Ge D, Guo J, Ding JY. The expression of CXCR4 and its relationship with matrix metalloproteinase-9/vascular endothelial growth factor in esophageal squamous cell cancer. Dis Esophagus. 2011;24(4):283–90.
Lu CL, Guo J, Gu J, Ge D, Hou YY, Lin ZW, et al. CXCR4 heterogeneous expression in esophageal squamous cell cancer and stronger metastatic potential with CXCR4-positive cancer cells. Dis Esophagus. 2014;27(3):294–302.
Wu J, Wu X, Liang W, Chen C, Zheng L, An H. Clinicopathological and prognostic significance of chemokine receptor CXCR4 overexpression in patients with esophageal cancer: a meta-analysis. Tumour Biol. 2014;35(4):3709–15.
Gockel I, Schimanski CC, Heinrich C, Wehler T, Frerichs K, Drescher D, et al. Expression of chemokine receptor CXCR4 in esophageal squamous cell and adenocarcinoma. BMC Cancer. 2006;6:290.
Faried A, Faried LS, Usman N, Kato H, Kuwano H. Clinical and prognostic significance of RhoA and RhoC gene expression in esophageal squamous cell carcinoma. Ann Surg Oncol. 2007;14(12):3593–601.
Yang Q, Luo GY, Li Y, Shan HB, Wang HY, Xu GL. Expression of Rac-1 related to tumor depth, lymph node metastasis and patient prognosis in esophageal squamous cell carcinoma. Med Oncol. 2013;30(4):689.
Zhao ZH, Tian Y, Yang JP, Zhou J, Chen KS. RhoC, vascular endothelial growth factor and microvascular density in esophageal squamous cell carcinoma. World J Gastroenterol. 2015;21(3):905–12.
Lv B, Yang X, Lv S, Wang L, Fan K, Shi R et al. CXCR4 Signaling induced epithelial-mesenchymal transition by PI3K/AKT and ERK pathways in glioblastoma. Mol Neurobiol. 2014.
Yang P, Wang G, Huo H, Li Q, Zhao Y, Liu Y. SDF-1/CXCR4 signaling up-regulates survivin to regulate human sacral chondrosarcoma cell cycle and epithelial-mesenchymal transition via ERK and PI3K/AKT pathway. Med Oncol. 2015;32(1):377.
Ponomaryov T, Peled A, Petit I, Taichman RS, Habler L, Sandbank J, et al. Induction of the chemokine stromal-derived factor-1 following DNA damage improves human stem cell function. J Clin Invest. 2000;106(11):1331–9.
Wang J, Wang J, Dai J, Jung Y, Wei CL, Wang Y, et al. A glycolytic mechanism regulating an angiogenic switch in prostate cancer. Cancer Res. 2007;67(1):149–59.
Kato M, Kitayama J, Kazama S, Nagawa H. Expression pattern of CXC chemokine receptor-4 is correlated with lymph node metastasis in human invasive ductal carcinoma. Breast Cancer Res. 2003;5(5):R144–50.
Wang J, Cai J, Han F, Yang C, Tong Q, Cao T, et al. Silencing of CXCR4 blocks progression of ovarian cancer and depresses canonical Wnt signaling pathway. Int J Gynecol Cancer. 2011;21(6):981–7.
Scala S, Ottaiano A, Ascierto PA, Cavalli M, Simeone E, Giuliano P, et al. Expression of CXCR4 predicts poor prognosis in patients with malignant melanoma. Clin Cancer Res Off J Am Assoc Cancer Res. 2005;11(5):1835–41.
Spano JP, Andre F, Morat L, Sabatier L, Besse B, Combadiere C, et al. Chemokine receptor CXCR4 and early-stage non-small cell lung cancer: pattern of expression and correlation with outcome. Ann Oncol. 2004;15(4):613–7.
Itoh K, Yoshioka K, Akedo H, Uehata M, Ishizaki T, Narumiya S. An essential part for Rho-associated kinase in the transcellular invasion of tumor cells. Nat Med. 1999;5(2):221–5.
Clark EA, Golub TR, Lander ES, Hynes RO. Genomic analysis of metastasis reveals an essential role for RhoC. Nature. 2000;406(6795):532–5.
Ridley AJ. Rho GTPases and cell migration. J Cell Sci. 2001;114(Pt 15):2713–22.
Etienne-Manneville S, Hall A. Rho GTPases in cell biology. Nature. 2002;420(6916):629–35.
Sahai E, Marshall CJ. RHO-GTPases and cancer. Nat Rev Cancer. 2002;2(2):133–42.
Lin ML, Lu YC, Chen HY, Lee CC, Chung JG, Chen SS. Suppressing the formation of lipid raft-associated Rac1/PI3K/Akt signaling complexes by curcumin inhibits SDF-1alpha-induced invasion of human esophageal carcinoma cells. Mol Carcinog. 2014;53(5):360–79.
Rubin JB, Kung AL, Klein RS, Chan JA, Sun Y, Schmidt K, et al. A small-molecule antagonist of CXCR4 inhibits intracranial growth of primary brain tumors. Proc Natl Acad Sci U S A. 2003;100(23):13513–8.
Zou W, Machelon V, Coulomb-L'Hermin A, Borvak J, Nome F, Isaeva T, et al. Stromal-derived factor-1 in human tumors recruits and alters the function of plasmacytoid precursor dendritic cells. Nat Med. 2001;7(12):1339–46.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None
Grant support
The study was supported by Natural Science Foundation of Ningbo, Zhejiang province, China (No. 2014A610218), National Natural Science Foundation of China (No. 81302099), and ZHU XUE Program of Fudan University.
Additional information
Jing Guo and Xiaofang Yu contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
Western blotting analysis of phosphorylation AKT in Eca109 cell lines and HEEC cell lines (a). Western blotting analysis of phosphorylation AKT, RhoA, Rac-1, and Cdc42 in HEEC cells, HEEC-vector cells, and HEEC-CXCR4 cells (b). (GIF 24 kb)
Supplementary Figure 2
Expression of CXCR4 in Eca109 with gene downregulation (a). Western blotting analysis of phosphorylation AKT, RhoA, Rac-1, and Cdc42 in Eca109/shCtl cells, Eca109/shCXCR4 cells, and Eca109/shCXCR4-AKT cells (b). The growth curves for Eca109/shCtl cells, Eca109/shCXCR4 cells, and Eca109/shCXCR4-AKT cells in vitro proliferation assays (c). Results of transwell assays showed the representative images of invasive Eca109/shCtl cells, Eca109/shCXCR4 cells, and Eca109/shCXCR4-AKT cells (d). (GIF 70 kb)
Rights and permissions
About this article
Cite this article
Guo, J., Yu, X., Gu, J. et al. Regulation of CXCR4/AKT-signaling-induced cell invasion and tumor metastasis by RhoA, Rac-1, and Cdc42 in human esophageal cancer. Tumor Biol. 37, 6371–6378 (2016). https://doi.org/10.1007/s13277-015-4504-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4504-x