Abstract
Cyclins are a group of cell cycle regulatory proteins. Cyclin B acts as an activator to cyclin-dependent kinase 1 (CDK1), a protein kinase essential for G2/M phase transition. Deregulation of cyclins has been linked to a number of malignant neoplasms, but the impact on clinicopathological parameters seems to be cancer-specific. Overexpression of cyclin B has been shown to affect survival in some malignant tumors, including breast and esophageal cancer, but its impact on endometrial cancer has not been extensively studied. For this study, 211 endometrial endometrioid adenocarcinoma samples were obtained from patients surgically treated at the Oulu University Hospital. The samples were immunohistochemically stained and analyzed for cyclin B expression. The relationships between cyclin B expression and conventional prognostic factors were analyzed. A discrimination threshold for survival analyses was calculated by utilizing the receiver operator characteristic (ROC) method. Cyclin B expression correlated with grade and advanced stage. Survival analyses showed that cyclin B expression affects cancer-specific survival in univariate analysis. In multivariate analysis, the results were indicative that cyclin B may hold independent prognostic significance, but further studies are required to assess this.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometrial cancer is the most common gynecological malignancy in Western countries. In Finland, the age-adjusted incidence and mortality rates were 12.9 and 2.2 per 100,000 women in 2012, respectively [1]. The majority of the cases are diagnosed in the early stages of the disease, giving an overall 5-year survival rate of 80 %. Endometrioid type forms the most common histopathological type, comprising 84 % of the cases [2].
Age, histopathological grade, and surgically defined stage form conventional prognostic factors in endometrial cancer [2, 3]. In addition to these, many biomarkers have been studied in an effort to find new factors to determine the aggressiveness of the tumor [4].
One of the key events in the development of malignant tumors is uncontrolled proliferation. Therefore, factors affecting cell cycle form an interesting area of study in cancer research. Among these factors are cyclins, cell cycle regulatory units, which play a key role in the control of cell cycle by regulating the activity of cyclin-dependent kinases (CDKs) [5, 6].
Cyclins were first identified in the early 1980s as proteins that degraded at the end of each M phase cycle in sea urchin embryos. Later in the decade, it was established that the previously identified maturation-promoting factor (MPF) was in fact a complex consisting of cell division cycle protein 2 (Cdc2) and cyclin B (Cdc2, subsequently renamed CDK1). The discovery was followed by the identification of other cyclin-CDK complexes [7].
Cyclin-CDK complex levels oscillate in a specific manner during the cell cycle. Cyclin D-CDK4/CDK6 and cyclin E-CDK2 complexes control G1 and S phase progression, whereas cyclin B-CDK1 complex regulates the transition between G2 and M phase. Cyclin A, on the other hand, has specificity for both CDK1 and CDK2 and, along with cyclin B and cyclin E, influences both S phase progression and G2/M transition [5, 6].
The aim of this study was to investigate the impact of cyclin B expression on cancer-specific survival as well as its correlation with conventional prognostic factors in endometrial endometrioid adenocarcinoma. Deregulation of cyclin B has previously been linked to a number of malignancies, including non-small cell lung cancer [8, 9], esophageal squamous cell carcinoma [10, 11], and breast cancer [12, 13]. The expression of cyclin B, however, has not been extensively studied in endometrial cancer.
Materials and methods
The patient population consisted of 211 patients who underwent operation for endometrial endometrioid adenocarcinoma at the Department of Obstetrics and Gynecology of the Oulu University Hospital between 1992 and 2000. Extrafascial hysterectomy, bilateral salpingo-oophorectomy, and pelvic lymphadenectomy were the operative treatment in most cases. Two patients had preoperative, 134 patients postoperative, and two pre- and postoperative radiotherapy. Four patients received neoadjuvant and 45 adjuvant cisplatin-based chemotherapy. The median age of the patients was 64 years (range 37–98) and median BMI was 29.7 kg/m2 (range 19.8–49.1). Median follow-up time was 77 months (range 0–136 months). At the end of the follow-up, 33 out of the 211 patients had died of the disease, 20 of other causes.
All the cases were staged according to the International Federation of Gynecology and Obstetric (FIGO) classification (2009). Formalin-fixed, paraffin-embedded tissue samples were obtained from the Department of Pathology. Stage I tumors were present in 140, stage II in 30, stage III in 36, and stage IV in five patients. There were 112 grade 1, 66 grade 2, and 33 grade 3 tumors.
Immunohistochemical stainings for cyclin B
Four-micrometer-thick sections were cut from a representative paraffin block. The sections were first deparaffinized in xylene and rehydrated in descending ethanol series. To enhance immunoreactivity, the sections were incubated in 10 mM citrate buffer (pH 6.0) and boiled in a microwave oven for 2 min at 850 W and after that for 8 min at 350 W. Endogenous peroxidase activity was eliminated by incubation in 0.1 % hydrogen peroxide in absolute methanol for 10 min. After incubation with the polyclonal rabbit cyclin B antibody (sc-752, Santa Cruz Biotechnology, Santa Cruz, California, USA), a biotinylated secondary anti-rabbit antibody was applied (dilution, 1:400), followed by the avidin-biotin-peroxidase complex (all from Dakopatts, Glostrup, Denmark). The color was developed using 3,3′-diaminobenzidine, and the sections were lightly counterstained with hematoxylin and mounted with Eukitt (Kindler, Freiburg, Germany). Replacement of the primary antibody by PBS at pH 7.2 was used as negative controls.
Cyclin B positivity was evaluated as a percentage of positive cells by evaluating the whole tumor section (Fig. 1).
Statistical analyses
All statistical analyses were carried out by using the SPSS for Mac version 21 software. The relationships between the clinicopathological variables and cyclin B were assessed with the Kruskal-Wallis or Mann-Whitney U test. Receiver operator characteristic curve (ROC) was used to determine the accuracy of cyclin B as a discriminator between patients with a good and poor prognosis over a range of cutoff points. The prognostic significance of different clinical variables was assessed by univariate analysis. Cumulative survival was analyzed by Kaplan-Meier analysis. The differences between the subgroups were compared by means of a log-rank test. The Cox proportional hazards model was used in multivariate analysis (backward stepwise Wald) to assess the independency of the prognostic factors. A p value >0.1 was used for model exclusion.
Results
Only eight samples out of the 211 had negative staining for cyclin B. Staining for cyclin B was not performed in three samples due to a limited number of tumor sections. The median labeling index (LI) of cyclin B was 10 % (range 0–100) and mean 13.3 % (SD 14.4).
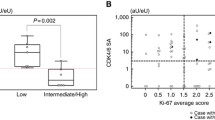
The median LI in grade 1 tumors was 5 %. This increased twofold for grade 2 tumors and threefold for grade 3 tumors. The differences were statistically significant (Fig. 2).
In stage I tumors, the median LI for cyclin B was 10 % (range 0–50). This remained the same for stage II tumors, with little difference in the range (1–50). In stage III tumors, the median LI increased to 20 % (range 1–100). In stage IV tumors, the median LI was 5 % (range 3–10). The difference between stage I and stage III tumors was statistically significant, whereas the number of stage IV tumors was insufficient for statistical analysis (Table 1).
The median LI for those who died of the disease was 12.5 % (range 1–100), whereas for those who survived or died of other causes, the median LI was 10 % (range 0–70). This difference was statistically significant (p = 0.015).
Utilizing the ROC method, a cutoff value of 12.5 % for cyclin B was calculated for survival analysis (sensitivity 0.516, specificity 0.699; area under the curve 0.637 (95 % confidence interval (CI) 0.535–0.738); p = 0.016). In the patient group with a cyclin B LI of 12.5 % or less, the Kaplan-Meier analysis showed a 5-year survival rate of 90 %, whereas in the group with a LI of over 12.5 %, the 5-year survival rate decreased to 77 % (Fig. 3).
Stepwise regression analysis was performed with the following factors: cyclin B expression, age, FIGO stage, and tumor grade. The analysis showed that the independent prognostic factors were cyclin B expression, FIGO stage, and tumor grade. However, the calculated hazard ratio in the patient group with a cyclin B LI of over 12.5 % was 1.9 with a 95 % confidence interval of 0.9–4.1 and a p value of 0.091. Cox univariate analysis gave the group a hazard ratio of 2.3 (95 % CI 1.1–4.5; p = 0.021).
Discussion
To our knowledge, this study is the largest cyclin B immunohistochemistry study on endometrial cancer published so far. All of the patients were treated in the same facility, Oulu University Hospital. Follow-up was organized systematically and was sufficiently long to show the relapses and deaths from the disease. Systematical surgical staging was performed in accordance with the FIGO criteria, and all of the histological samples were treated and analyzed with a uniform protocol.
In this study, we show that cyclin B expression correlates with grade and, to a degree, with stage in endometrial endometrioid adenocarcinoma. When comparing tumors extending outside the uterus to those limited to the uterus, the difference in cyclin B expression produced near-significant results. Statistically significant results were obtained by comparing the difference in the expression between stage I and stage III tumors, implicating a correlation between cyclin B expression and advanced stage.
In general, previous studies have not found any significant correlation between cyclin B expression and FIGO stage [14–18]. Interestingly, Rijcken et al. [17] showed that in hereditary nonpolyposis colon cancer (HNPCC)-related endometrial cancer, the overall expression of cyclin B was higher than in sporadic cancer. In their study, cyclin B expression did correlate with advanced stage, but only in HNPCC-related tumors. In contradiction to the previous studies, advanced stage seemed to correlate with cyclin B expression in our study.
In conjunction with our results, high expression of cyclin B has previously been linked to tumor grade by Milde-Langosch et al. [15] and Rijcken et al. [17]. On the other hand, conflicting evidence also exists [14, 16, 18]. The differences in the results may be explicable in terms of our comparatively large patient population of over 200 individuals in comparison to the few dozens of individuals in the previous studies, as well as various staining procedures used.
Deregulation of different cyclins has been studied in a number of neoplasms, but interestingly, the impact on prognosis seems to be cancer-specific [19–22]. High expression of cyclin B has been reported to affect survival adversely in gastric cancer [23], non-small cell lung cancer [8, 9], esophageal squamous cell carcinoma [10, 11], and breast cancer [12, 13]. An interesting addition to these are the findings of Shin et al. [24], who reported a better survival for patients with high expression of cyclin B in pancreatic neuroendocrine tumors.
In endometrial cancer, high expression of cyclin A and H has been shown to be independent prognostic factors [16, 18, 25]. On the other hand, previous studies have not found a correlation between cyclin B expression and prognosis [16, 18]. In this study, cyclin B is shown to be a prognostic factor in univariate analysis. Furthermore, cyclin B reached a level close to statistical significance in the Cox proportional hazard model. These results are indicative that cyclin B may be an independent prognostic factor, but further studies are required to assess this.
The impact of age on prognosis in endometrial cancer has been debated in recent years [26, 27]. Age was included in our survival analysis, but it proved not to be a prognostic factor. This may be explicable in terms of our study design, which only included patients who underwent surgical treatment, as it has been suggested that the impact age has on survival is related to less aggressive treatment options and inaccuracies in clinical cancer staging [2, 26].
Disadvantages of our study include the subjectivity of interpreting immunohistochemical staining and the retrospective study design. Furthermore, a small number of patients received therapy for their tumors prior to operation, possibly affecting cyclin B levels in some samples.
In conclusion, we have shown here that cyclin B expression correlates with tumor grade and FIGO stage. Furthermore, cyclin B expression correlates with survival, but only in univariate analysis.
References
Finnish Cancer Registry. Cancer Statistics. 2012. http://www.cancer.fi/syoparekisteri/en/statistics/. Accessed: 9 May 2014.
Creasman WT, Odicino F, Maisonneuve P, Quinn MA, Beller U, et al. Carcinoma of the corpus uteri. FIGO 26th annual report on the results of treatment in gynecological cancer. Int J Gynecol Obstet. 2006;95 Suppl 1:S105–43.
Creasman W. Revised FIGO staging for carcinoma of the endometrium. Int J Gynecol Obstet. 2009;105(2):109.
Gadducci A, Cosio S, Genazzani AR. Tissue and serum biomarkers as prognostic variables in endometrioid-type endometrial cancer. Crit Rev Oncol Hematol. 2011;80(2):181–92.
Harashima H, Dissmeyer N, Schnittger A. Cell cycle control across the eukaryotic kingdom. Trends Cell Biol. 2013;23(7):345–56.
Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9(3):153–66.
Doree M, Hunt T. From Cdc2 to Cdk1: When did the cell cycle kinase join its cyclin partner? J Cell Sci. 2002;115(Pt 12):2461–4.
Singhal S, Vachani A, Antin-Ozerkis D, Kaiser LR, Albelda SM. Prognostic implications of cell cycle, apoptosis, and angiogenesis biomarkers in non-small cell lung cancer: a review. Clin Cancer Res. 2005;11(11):3974–86.
Cooper WA, Kohonen-Corish MR, McCaughan B, Kennedy C, Sutherland RL, Lee CS. Expression and prognostic significance of cyclin B1 and cyclin A in non-small cell lung cancer. Histopathology. 2009;55(1):28–36.
Nozoe T, Korenaga D, Kabashima A, Ohga T, Saeki H, Sugimachi K. Significance of cyclin B1 expression as an independent prognostic indicator of patients with squamous cell carcinoma of the esophagus. Clin Cancer Res. 2002;8(3):817–22.
Takeno S, Noguchi T, Kikuchi R, Uchida Y, Yokoyama S, Muller W. Prognostic value of cyclin B1 in patients with esophageal squamous cell carcinoma. Cancer. 2002;94(11):2874–81.
Aaltonen K, Amini RM, Heikkila P, Aittomaki K, Tamminen A, et al. High cyclin B1 expression is associated with poor survival in breast cancer. Br J Cancer. 2009;100(7):1055–60.
Nimeus-Malmstrom E, Koliadi A, Ahlin C, Holmqvist M, Holmberg L, et al. Cyclin B1 is a prognostic proliferation marker with a high reproducibility in a population-based lymph node negative breast cancer cohort. Int J Cancer. 2010;127(4):961–7.
Horree N, van Diest PJ, van der Groep P, Sie-Go DM, Heintz AP. Progressive derailment of cell cycle regulators in endometrial carcinogenesis. J Clin Pathol. 2008;61(1):36–42.
Milde-Langosch K, Bamberger AM, Goemann C, Rossing E, Rieck G, et al. Expression of cell-cycle regulatory proteins in endometrial carcinomas: correlations with hormone receptor status and clinicopathologic parameters. J Cancer Res Clin Oncol. 2001;127(9):537–44.
Kayaselcuk F, Erkanli S, Bolat F, Seydaoglu G, Kuscu E, Demirhan B. Expression of cyclin H in normal and cancerous endometrium, its correlation with other cyclins, and association with clinicopathologic parameters. Int J Gynecol Cancer. 2006;16(1):402–8.
Rijcken F, van der Zee A, van der Sluis T, Boersma-van Ek W, Kleibeuker J, Hollema H. Cell cycle regulators and apoptosis-associated proteins in relation to proliferative activity and degree of apoptosis in HNPCC versus sporadic endometrial carcinoma. Histopathology. 2006;48(3):275–85.
Shih HC, Shiozawa T, Kato K, Imai T, Miyamoto T, et al. Immunohistochemical expression of cyclins, cyclin-dependent kinases, tumor-suppressor gene products, ki-67, and sex steroid receptors in endometrial carcinoma: positive staining for cyclin A as a poor prognostic indicator. Hum Pathol. 2003;34(5):471–8.
Yam CH, Fung TK, Poon RY. Cyclin A in cell cycle control and cancer. Cell Mol Life Sci. 2002;59(8):1317–26.
Xu XL, Chen SZ, Chen W, Zheng WH, Xia XH, et al. The impact of cyclin D1 overexpression on the prognosis of ER-positive breast cancers: a meta-analysis. Breast Cancer Res Treat. 2013;139(2):329–39.
Huang LN, Wang DS, Chen YQ, Li W, Hu FD, et al. Meta-analysis for cyclin E in lung cancer survival. Clin Chim Acta. 2012;413(7–8):663–8.
Gould Rothberg BE, Bracken MB, Rimm DL. Tissue biomarkers for prognosis in cutaneous melanoma: a systematic review and meta-analysis. J Natl Cancer Inst. 2009;101(7):452–74.
Begnami MD, Fregnani JH, Nonogaki S, Soares FA. Evaluation of cell cycle protein expression in gastric cancer: cyclin B1 expression and its prognostic implication. Hum Pathol. 2010;41(8):1120–7.
Shin JU, Lee CH, Lee KT, Lee KH, Kim KM, et al. Prognostic significance of ATM and cyclin B1 in pancreatic neuroendocrine tumor. Tumor Biol. 2012;33(5):1645–51.
Santala S, Talvensaari-Mattila A, Soini Y, Honkavuori-Toivola M, Santala M. High expression of cyclin A is associated with poor prognosis in endometrial endometrioid adenocarcinoma. Tumor Biol. 2014;35(6):5395–9.
Ahmed A, Zamba G, DeGeest K, Lynch CF. The impact of surgery on survival of elderly women with endometrial cancer in the SEER program from 1992–2002. Gynecol Oncol. 2008;111(1):35–40.
Benedetti Panici P, Basile S, Salerno MG, Di Donato V, Marchetti C, et al. Secondary analyses from a randomized clinical trial: age as the key prognostic factor in endometrial carcinoma. Am J Obstet Gynecol. 2014;210(4):363.e1–10.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santala, S., Talvensaari-Mattila, A., Soini, Y. et al. Prognostic value of cyclin B in endometrial endometrioid adenocarcinoma. Tumor Biol. 36, 953–957 (2015). https://doi.org/10.1007/s13277-014-2676-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-014-2676-4