Abstract
Background
Neuromyelitis optica (NMO) is an inflammatory demyelinating disorder featured with the presence of serum aquaporin-4 immunoglobulin G antibodies (AQP4-IgG).
Objective
Osteopontin (OPN) was reported to be upregulated in NMO; however, the detailed function of OPN in NMO is obscure.
Results
Downregulation of OPN alleviated demyelination, axonal loss, microglia activation, neutrophil infiltration, inflammatory response and astrocyte apoptosis, but increased neurotrophic factor levels in murine spinal cords. Moreover, knockdown of OPN suppressed the expression of its downstream molecules, including interferon-gamma (IFN-γ), nuclear factor kappa B (NF-kB) and interleukin-12 (IL-12).
Conclusion
OPN promotes microglia activation and facilitates the pathogenesis of NMO by activating the IFN-γ/NF-kB/IL-12 signaling pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuromyelitis optica (NMO) is an inflammatory demyelinating disorder of the central nervous system (CNS) (Patterson and Goglin 2017). NMO mainly affects optic nerves and/or the spinal cord which may lead to blindness, paraplegia, loss of sensation, respiratory failure and even death (Yick et al. 2020). The pathology of NMO is featured with the presence of serum aquaporin-4 immunoglobulin G antibodies (AQP4-IgG), which targets the water channel AQP4 expressed on astrocytes in the CNS (Tradtrantip et al. 2021). Moreover, prominent microglia activation was observed in NMO lesions, indicating that microglia play a crucial role in the pathogenesis of NMO (Chen et al. 2020). NMO is a relapsing–remitting disease and recurrent attacks can result in severe visual impairment, limb dysfunction and other sequelae (Chen et al. 2021). The therapies available for NMO are limited and in most cases only partially effective (Wu et al. 2019). Therefore, it is of great significance to find more effective approaches for the treatment of NMO.
Osteopontin (OPN) is a highly phosphorylated acidic glycoprotein which presents in a range of tissues, such as bone marrow, brain and kidney (Hu et al. 2021). As a multifunctional protein, OPN has been revealed to play a critical part in multiple disorders. For examples, OPN-loaded nanoparticles were found to increase the intestinal mucosal barrier and inhibit inflammatory response by regulating nuclear factor kappa B (NF-kB) signaling (Wei et al. 2020). Importantly, previous studies demonstrated that OPN was upregulated in NMO brain lesions (Satoh et al. 2008). Elevated OPN level in plasma is related to disease activity in NMO (Shimizu et al. 2013). Furthermore, enhanced expression of OPN has been shown in cerebrospinal fluid and OPN facilitates macrophage chemotaxis by interacting with integrin αvβ3 and activating downstream signaling pathways (Kariya et al. 2015). However, the role of OPN in cervical spinal cords in vivo has not been studied.
Accumulating evidence has revealed that OPN elevates macrophages and T cells in the process of inflammation and increases the levels of type 1 cytokines including interferon-gamma (IFN-γ) and interleukin-12 (IL-12) (Mas et al. 2007). The IL-12 family is a critical regulator in autoimmune diseases including NMO (Zhang et al. 2016). Additionally, OPN exerts its effect in multiple disorders by modulating the NF-kB signaling pathway. For example, OPN promotes the proliferation of chondrocytes in an osteoarthritis rat model by activating NF-kB signaling (Sun et al. 2020). In periapical periodontitis, OPN facilitates bone destruction also by promoting the activation of NF-kB signaling (Dong et al. 2018). Intriguingly, NF-kB signaling was reported to drive pro-granulocytic astrocyte to respond to IgG in NMO (Walker-Caulfield et al. 2015).
This study aimed to probe the role of OPN in regulating the progression of NMO in vivo. It was hypothesized that OPN exerted its regulatory effects on NMO by regulating downstream signaling pathways. Our findings might provide a credible therapeutic target for the treatment of NMO.
Materials and methods
Isolation of AQP4-IgG
AQP4-IgG was purified according to previous description (Saadoun et al. 2010). Briefly, serum was obtained from five patients diagnosed with AQP4-IgG-positive NMO and three healthy controls. Informed consent was collected from all participants. IgG was purified with the Melon Gel IgG Purification Kit (Thermo, Waltham, MA, USA), eluted with glycine and neutralized in 1 M Tris buffer. Then IgG was concentrated with Amicon Ultra-15 centrifugal filters (Millipore, Germany) at a final concentration of 20 mg/ml. IgG from NMO patients and healthy controls was termed as AQP4-IgG or Con-IgG, respectively. The study was approved the Ethics Committee of Xiantao First People's Hospital Affiliated to Yangtze University (Hubei, China) and performed following the 1964 Helsinki declaration.
NMO mouse models
Adeno-associated virus (AAV) vectors containing small interfering RNA (siRNA) for OPN (AAV-si-OPN) and the negative control (AAV-NC) were synthesized by GeneChem (Shanghai, China). Thirty-two female wild-type C57BL/6 mice (6–8 weeks old; HFK Bioscience, Beijing, China) were randomly divided into four groups: sham + AAV-NC, sham + AAV-si-OPN, model + AAV-NC and model + AAV-si-OPN, with eight mice per group. The establishment of NMO mouse models was performed as previously described (Saadoun et al. 2010). All mice were anesthetized with ketamine (100 mg/kg) and xylazine (10 mg/kg). Then mice were subcutaneously injected with complete Freund’s adjuvant (CFA, 50 μl; BD Biosciences, San Jose, CA, USA) with heat killed H37Ra Mycobacterium tuberculosis (Difco, 50 μg) and intraperitoneally injected with pertussis toxin. Seven days after disruption of blood–brain-barrier (BBB), mice in the model groups were intraperitoneally injected with 4 mg AQP4-IgG daily for eight days, while mice in the sham groups received equal amount of Con-IgG. At the fourth day of injection, mice received injection of AAV-si-OPN or AAV-NC vectors, respectively. Eight days after injection of IgG, mice were killed by cervical dislocation under anesthesia. Murine cervical spinal cords were collected and stored at − 80 °C for the following experiments. All animal experiments were approved by the Ethics Committee of Xiantao First People's Hospital Affiliated to Yangtze University (Hubei, China) and were performed strictly following the guidelines of the Guide for the Care and Use of Laboratory Animals.
Western blotting
Murine spinal cords were homogenized using RIPA buffer containing protease/phosphatase inhibitors (Roche Diagnostics, Tokyo, Japan). The supernatant was harvested, and protein concentration was quantified with a BCA assay kit (Bio-Rad, Hercules, CA, USA). Then equal amounts of protein samples (20 μg) were separated on 10% SDS-PAGE gels and transferred to polyvinylidene fluoride membranes (Bio-Rad). After blocking with 5% defatted milk, the membranes were incubated with primary antibody against OPN (ab63856, Abcam, Cambridge, MA, USA) at 4 °C overnight, followed by incubation with the secondary antibody (ab288151, Abcam) at room temperature for 2 h. Eventually, protein bands were visualized with an enhanced chemiluminescent detection system (Thermo) and quantified by densitometry analysis using Quantity One software (Bio-Rad).
Immunofluorescence (IF) staining
Sections of murine cervical spinal cords were prepared using a cryostat (Thermo). The sections were fixed in 4% formaldehyde, blocked using 0.1% gelatin in phosphate buffer saline (PBS) for 30 min and then incubated with primary antibodies against: neurofilament heavy polypeptide (NF-H, ab207176, 1:100), myelin basic protein (MBP, ab216590, 1:200), ionized calcium-binding adapter molecule 1 (Iba-1, ab178846, 1:500) (all from Abcam) and lymphocyte antigen 6 complex locus G (Ly6G, BP0075-1, 1:200; Bio X Cell, West Lebanon, NH, USA) overnight at 4 °C. Subsequently, the sections were incubated with corresponding Alexa-Fluor-conjugated secondary antibodies (Thermo) for 1 h at room temperature, counterstained with DAPI and mounted with anti-fade reagent (Thermo). Images were captured using a fluorescence microscope (LEICA TCSSP8, Germany) and were digitalized with SPOT 5.0 software (Diagnostic Instruments Inc., Sterling Heights, MI, USA) in identical settings. Signal intensity was quantified using ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Enzyme-linked immunosorbent assay (ELISA)
Murine spinal cords were homogenized with a lysis buffer containing phosphatase inhibitor and protease inhibitor cocktail. The levels of proinflammatory factors, brain-derived neurotrophic factor (BDNF) and OPN downstream molecules were measured using corresponding ELISA kit: IL-1β (ab197742, Abcam), TNF-α (ab208348, Abcam), IL-6 (ab222503, Abcam), BDNF (EK5128, SAB Biotech, Nanjing, China), IFN-γ (EK1123, SAB Biotech), NF-kB (ab176647, Abcam) and IL-12 (EK0345, SAB Biotech) according to the instructions of manufacturers.
Glial fibrillary acidic protein/Terminal deoxynucleotidyl transferase mediated nick end labeling (GFAP/TUNEL) double staining
TUNEL staining was conducted using the In-situ Cell Death Detection Kit (Roche, Penzberg, Germany). After TUNEL staining, murine spinal cord sections were washed with PBS and incubated with anti-GFAP primary antibody (1:500, sc-33673, Santa Cruz Biotechnology, Santa Cruz, CA, USA) overnight at 4 °C, followed by incubation with the secondary antibody (Abcam). The sections were mounted with anti-fade reagent (Thermo), and astrocyte apoptosis was measured by counting GFAP/TUNEL-positive cells using a fluorescence microscope (Olympus, Tokyo, Japan).
Statistical analysis
Data are presented as the mean ± standard deviation. SPSS 18.0 software (SPSS, Chicago, IL, USA) was used for statistical analysis. Each experiment was conducted in triplicate. Differences between two groups were analyzed with Student’s t test, while those among more groups were evaluated using analysis of variance (ANOVA) followed by Turkey post hoc analysis. p˂0.05 was considered as statistically significant.
Results
OPN silencing attenuates demyelination and axonal loss in mice
First, western blotting was performed to assess the efficiency of OPN knockdown. As shown by the results, OPN protein expression was significantly downregulated in si-OPN-treated groups in comparison to corresponding NC-treated groups (Fig. 1A). Then we tested whether OPN had an effect on myelin and axons in murine spinal cords. IF staining was used to evaluate the expression of MBP and NH-F which act as the marker for myelin and axons, respectively. As shown in Fig. 1B and C, compared to the sham group, the model group exhibited prominent and patchy loss of myelin and axons, and OPN silencing significantly enhanced MBP and NH-F signals in murine spinal cords. Assessment of IF intensity further elucidated the increased MBP expression in si-OPN-treated model mice compared to NC-treated model mice (Fig. 1D). Similarly, AQP4-IgG induced the loss of axons in murine spinal cords and OPN silencing was shown to attenuate this effect, as shown by the number of NH-F spots (Fig. 1E). Collectively, these results revealed that knocking down OPN can mitigate AQP4-IgG-induced demyelination and axonal loss in murine spinal cords.
OPN silencing attenuates demyelination and axonal loss in mice. A Western blotting for assessing protein levels of OPN in each group. B, C IF staining of MBP and NF-H in murine spinal cords. D Measurement of relative IF intensity of MBP in each group. E Quantification of the number of NF-H spots. N = 8 mice/group. *p < 0.01, **p <0.01, ***p < 0.001
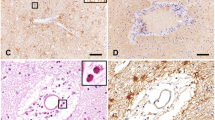
Knockdown of OPN inhibits microglia activation and neutrophil infiltration
Microglia activation and neutrophil infiltration play critical roles in the pathogenesis of NMO (Chen et al. 2021). Next, we tested whether OPN affected microglia activation and neutrophil infiltration in mice. Iba-1 and Ly6G were used as markers for microglia activation and neutrophil infiltration, respectively. Significant elevation in Iba-1 and Ly6G levels was displayed in murine spinal cords of the model groups and knockdown of OPN markedly alleviated the elevation (Fig. 2A, B), indicating that knockdown of OPN might inhibit microglia activation and neutrophil infiltration. This was further verified by the evaluation of IF intensity which showed that OPN silencing significantly attenuated AQP4-IgG-induced enhancement in Iba-1 and Ly6G expression in mice (Fig. 2C, D).
Knocking down OPN suppresses inflammatory response
Activated microglia secrete proinflammatory factors which promote the progression of NMO (Yick et al. 2020). ELISA was used to investigate the impact of OPN on inflammation in NMO mice. As demonstrated by the results, AQP4-IgG stimulated the secretion of proinflammatory factors (IL-1β, TNF-α, and IL-6), however, knocking down OPN markedly decreased their levels (Fig. 3A–C). Hence, depletion of OPN has an inhibitory effect on inflammatory response in spinal cords of NMO mice.
OPN depletion inhibits the apoptosis of astrocytes
Subsequently, to further probe the role of OPN on NMO, GFAP/TUNEL double staining was conducted to analyze OPN impact on cell apoptosis. GFAP was used as a marker for astrocytes. As revealed by the results, apoptotic cells in the model + AAV-NC group were significantly increased in comparison to the sham group and silencing of OPN reduced the apoptotic cells in spinal cords of mice (Fig. 4A, B). Furthermore, to further characterize the protective effect of OPN on astrocytes, we evaluated the concentration of BDNF in spinal cords. Astrocytes have been found to be a main source of neurotrophic factors including BDNF. It was revealed that compared with that in the sham group, the concentration of BDNF in the model + AAV-NC group was significantly reduced (Fig. 4C). Notably, OPN knockdown increased the concentration of BDNF in mice of the model group, as displayed by ELISA (Fig. 4C). These indicated that OPN silencing can suppress AQP4-IgG-induced apoptosis of astrocytes in murine spinal cords.
OPN downregulation inactivates IFN-γ/IL-12/NF-kB signaling
To reveal the potential mechanism of OPN underlying the progression of NMO, we analyzed the downstream molecules of OPN. ELISA was used to evaluate the accumulation of IFN-γ, NF-kB and IL-12 in spinal cords of each group. The results revealed that in comparison to the sham group, the model + AAV-NC group exhibited enhanced levels of IFN-γ, NF-kB and IL-12 and in the model + AAV-si-OPN group, the enhancement was found to be attenuated (Fig. 5A–C). Collectively, downregulation of OPN can suppress the activation of IFN-γ/IL-12/NF-kB signaling pathway in murine spinal cords.
Discussion
NMO is an autoimmune inflammatory disorder characterized by the presence of AQP4-IgG which binds to AQP4 and leads to demyelination and inflammation (Tradtrantip et al. 2021). Based on the evidence, we established a NMO mouse model by passively transferring human AQP4-IgG to mice with disruption of BBB. It is suggested that AQP4-IgG-induced animal models exhibit marked NMO-like pathology including neutrophil infiltration, microglia activation, astrocyte damage, demyelination (Yick et al. 2018). Microglia, CNS-resident innate immune cells, should be the first responder to reactive astrocytes after the onset of NMO pathology (Moinfar and Zamvil 2020). Numerous studies have illustrated the significance of microglia activation in the pathogenic process of NMO (Moinfar and Zamvil 2020; Ma et al. 2021).
OPN is a cytokine-like matrix protein that has been indicated to be implicated in physiological and pathological processes of various diseases, including cardiovascular disease, immune diseases and cancers (Hao et al. 2021; Shirakawa and Sano 2021; Rittling and Singh 2015). Importantly, OPN was reported to be upregulated in NMO and released by infiltrating macrophages, astrocytes, oligodendroglia, and neurons (Shimizu et al. 2013). Nevertheless, the detailed role of OPN in cervical spinal cords in vivo is unclear. Here, we knocked down OPN in a NMO mouse model and found that downregulation of OPN alleviated demyelination and axonal loss in murine spinal cords. Moreover, knockdown of OPN inhibited microglia activation and neutrophil infiltration in model mice, indicating that OPN downregulation might act as a suppressor in the pathogenesis of NMO.
Furthermore, studies have showed that OPN can affect inflammatory response in several diseases. For example, in a mouse model of atopic asthma, OPN was found to inhibit inflammation, alleviate tissue damage and prevent pneumococcal infection (Kasetty et al. 2019). Intriguingly, overexpression of OPN aggregates brain damage and inflammatory response in hypoxia–ischemia-induced cerebral immune cells (Xin et al. 2021). Activated microglia release more proinflammatory cytokines which further promote inflammation in tissues (Chen et al. 2021). In the present study, we detected the levels of proinflammatory cytokines in murine spinal cords and found that OPN downregulation significantly decreased the secretion of proinflammatory cytokines. This indicated that OPN might exert a proinflammatory effect on NMO. Increasing evidence has linked OPN expression to cell apoptosis (Dalal et al. 2016; Mazaheri et al. 2018). In this study, downregulated OPN was shown to attenuate AQP4-IgG-induced astrocyte apoptosis. Astrocytes have been indicated to be the main source of neurotrophic factors which act as crucial regulators in the maintenance and survival of glial cells and neurons in the CNS (Yick et al. 2020). It was found in this study that OPN silencing markedly elevated the level of BDNF, indicating that knocking down OPN can protect against astrocyte damage.
It has been indicated that OPN can stimulate macrophages to release the Th1 cytokines including IL-12 and IFN-γ (Li et al. 2003). IFN-γ was reported to be upregulated in the plasma of NMO patients (Correale and Fiol 2011). Additionally, OPN affects the progression of multiple disorders by modulating the NF-kB signaling pathway (Wei et al. 2020; Mohammadi et al. 2016). Activation of NF-kB signaling stimulates the expression of proinflammatory cytokines, consequently leading to inflammation (Lawrence 2009). Here, we tested whether OPN had an effect on the IFN-γ/NF-kB/IL-12 signaling pathway in NMO. It was disclosed that depletion of OPN inhibited the activation of the IFN-γ/NF-kB/IL-12 signaling pathway in spinal cords of NMO mice.
In conclusion, we investigated the role of OPN in affecting the pathogenesis of NMO. The results revealed that downregulation of OPN can alleviate demyelination, axonal loss, microglia activation, neutrophil infiltration, inflammatory response and suppress astrocyte apoptosis in spinal cords of a NMO mouse model. Moreover, OPN depletion inactivates the IFN-γ/NF-kB/IL-12 signaling pathway. Collectively, OPN-mediated microglia activation promotes the progression of NMO via the IFN-γ/NF-kB/IL-12 signaling pathway. Our findings might provide a credible therapeutic target for treating NMO.
Availability of data and material
The datasets used during the current study are available from the corresponding author on reasonable request.
References
Chen T, Lennon VA, Liu YU, Bosco DB, Li Y, Yi MH et al (2020) Astrocyte-microglia interaction drives evolving neuromyelitis optica lesion. J Clin Investig 130(8):4025–4038
Chen T, Bosco DB, Ying Y, Tian DS, Wu LJ (2021) The emerging role of microglia in neuromyelitis optica. Front Immunol 12:616301
Correale J, Fiol M (2011) Chitinase effects on immune cell response in neuromyelitis optica and multiple sclerosis. Multiple Scler (houndmills, Basingstoke, Engl) 17(5):521–531
Dalal S, Zha Q, Singh M, Singh K (2016) Osteopontin-stimulated apoptosis in cardiac myocytes involves oxidative stress and mitochondrial death pathway: role of a pro-apoptotic protein BIK. Mol Cell Biochem 418(1–2):1–11
Dong M, Yu X, Chen W, Guo Z, Sui L, Xu Y et al (2018) Osteopontin promotes bone destruction in periapical periodontitis by activating the NF-κB pathway. Cell Physiol Biochem 49(3):884–898
Hao C, Cui Y, Lane J, Jia S, Ji J, Jiang WG (2021) Distinctive prognostic value and cellular functions of osteopontin splice variants in human gastric cancer. Cells 10(7):1820
Hu B, Zhang J, Jiang Y, Tong W, Lai S, Ren Y (2021) Quantitative determination of osteopontin in bovine, buffalo, yak, sheep and goat milk by ultra-high performance liquid chromatography-tandem mass spectrometry and stable isotope dimethyl labeling. Food Chem 343:128489
Kariya Y, Kariya Y, Saito T, Nishiyama S, Honda T, Tanaka K et al (2015) Increased cerebrospinal fluid osteopontin levels and its involvement in macrophage infiltration in neuromyelitis optica. BBA Clin 3:126–134
Kasetty G, Bhongir RKV, Papareddy P, Tufvesson E, Stenberg H, Bjermer L et al (2019) Osteopontin protects against pneumococcal infection in a murine model of allergic airway inflammation. Allergy 74(4):663–674
Lawrence T (2009) The nuclear factor NF-kappaB pathway in inflammation. Cold Spring Harb Perspect Biol 1(6):a001651
Li X, O’Regan AW, Berman JS (2003) IFN-gamma induction of osteopontin expression in human monocytoid cells. J Interferon Cytokine Res 23(5):259–265
Ma X, Qin C, Chen M, Yu HH, Chu YH, Chen TJ et al (2021) Regulatory T cells protect against brain damage by alleviating inflammatory response in neuromyelitis optica spectrum disorder. J Neuroinflammation 18(1):201
Mas A, Martínez A, de las Heras V, Bartolomé M, de la Concha EG, Arroyo R et al (2007) The 795CT polymorphism in osteopontin gene is not associated with multiple sclerosis in a Spanish population. Multiple Sclerosis (houndmills, Basingstoke, Engl) 13(2):250–252
Mazaheri N, Peymani M, Galehdari H, Ghaedi K, Ghoochani A, Kiani-Esfahani A et al (2018) Ameliorating effect of osteopontin on H(2)O(2)-induced apoptosis of human oligodendrocyte progenitor cells. Cell Mol Neurobiol 38(4):891–899
Mohammadi S, Ghaffari SH, Shaiegan M, Zarif MN, Nikbakht M, Akbari Birgani S et al (2016) Acquired expression of osteopontin selectively promotes enrichment of leukemia stem cells through AKT/mTOR/PTEN/β-catenin pathways in AML cells. Life Sci 152:190–198
Moinfar Z, Zamvil SS (2020) Microglia complement astrocytes in neuromyelitis optica. J Clin Investig 130(8):3961–3964
Patterson SL, Goglin SE (2017) Neuromyelitis optica. Rheum Dis Clin North Am 43(4):579–591
Rittling SR, Singh R (2015) Osteopontin in immune-mediated diseases. J Dent Res 94(12):1638–1645
Saadoun S, Waters P, Bell BA, Vincent A, Verkman AS, Papadopoulos MC (2010) Intra-cerebral injection of neuromyelitis optica immunoglobulin G and human complement produces neuromyelitis optica lesions in mice. Brain J Neurol 133(Pt 2):349–361
Satoh J, Obayashi S, Misawa T, Tabunoki H, Yamamura T, Arima K et al (2008) Neuromyelitis optica/Devic’s disease: gene expression profiling of brain lesions. Neuropathology 28(6):561–576
Shimizu Y, Ota K, Ikeguchi R, Kubo S, Kabasawa C, Uchiyama S (2013) Plasma osteopontin levels are associated with disease activity in the patients with multiple sclerosis and neuromyelitis optica. J Neuroimmunol 263(1–2):148–151
Shirakawa K, Sano M (2021) Osteopontin in cardiovascular diseases. Biomolecules 11(7):1047
Sun PF, Kong WK, Liu L, Liu Y, Liu FM, Liu WJ et al (2020) Osteopontin accelerates chondrocyte proliferation in osteoarthritis rats through the NF-κb signaling pathway. Eur Rev Med Pharmacol Sci 24(6):2836–2842
Tradtrantip L, Yeaman MR, Verkman AS (2021) Cytoprotective IgG antibodies in sera from a subset of patients with AQP4-IgG seropositive neuromyelitis optica spectrum disorder. Sci Rep 11(1):21962
Walker-Caulfield ME, Guo Y, Johnson RK, McCarthy CB, Fitz-Gibbon PD, Lucchinetti CF et al (2015) NFκB signaling drives pro-granulocytic astroglial responses to neuromyelitis optica patient IgG. J Neuroinflammation 12:185
Wei F, Lang Y, Shen Q, Xu L, Cheng N, Chu Y et al (2020) Osteopontin-loaded PLGA nanoparticles enhance the intestinal mucosal barrier and alleviate inflammation via the NF-κB signaling pathway. Colloids Surf B 190:110952
Wu Y, Zhong L, Geng J (2019) Neuromyelitis optica spectrum disorder: pathogenesis, treatment, and experimental models. Multiple Scler Relat Disorders 27:412–418
Xin D, Li T, Chu X, Ke H, Liu D, Wang Z (2021) MSCs-extracellular vesicles attenuated neuroinflammation, synapse damage and microglial phagocytosis after hypoxia-ischemia injury by preventing osteopontin expression. Pharmacol Res 164:105322
Yick LW, Ma OK, Ng RC, Kwan JS, Chan KH (2018) Aquaporin-4 autoantibodies from neuromyelitis optica spectrum disorder patients induce complement-independent immunopathologies in mice. Front Immunol 9:1438
Yick LW, Tang CH, Ma OK, Kwan JS, Chan KH (2020) Memantine ameliorates motor impairments and pathologies in a mouse model of neuromyelitis optica spectrum disorders. J Neuroinflammation 17(1):236
Zhang DQ, Jia K, Wang R, Li T, Zhao N, Yang LN et al (2016) Decreased serum IL-27 and IL-35 levels are associated with disease severity in neuromyelitis optica spectrum disorders. J Neuroimmunol 293:100–104
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Both two co-authors participated in the literature search, analysis and interpretation of the data, and the writing of the manuscript. All authors saw and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Fengyi Chen declares that he/she has no conflict of interest. Yanping Wang declares that he/she has no conflict of interest.
Ethical approval
All animal experiments were approved by the Ethics Committee of Xiantao First People's Hospital Affiliated to Yangtze University (Hubei, China) and were performed strictly following the guidelines of the Guide for the Care and Use of Laboratory Animals.
Consent of publication
Not applicable.
Rights and permissions
About this article
Cite this article
Chen, F., Wang, Y. Osteopontin promotes microglia activation and aggravates neuromyelitis optica via interferon-gamma/nuclear factor kappa B/interleukin-12 signaling. Mol. Cell. Toxicol. 19, 353–361 (2023). https://doi.org/10.1007/s13273-022-00265-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13273-022-00265-7