Abstract
Objective
Arterial stiffness and endothelial function are two established surrogate markers of subclinical atherosclerosis and are quantified by three arterial parameters: elasticity, viscosity and radius of the arterial wall. Yet, the current methods for their assessment are unsuitable for routine use. Post-exercise response of the cardiovascular (CV) system serves as a more sensitive detection of subclinical arterial abnormalities that are not apparent at-rest. The objective of this study is to propose a novel method that can measure post-exercise response of arterial parameters and is also suitable for routine use.
Approach
A microfluidic tactile sensor with a location-insensitive configuration was used for arterial pulse signal measurements on six asymptomatic male subjects, offering measurement reliability, ease use by a layperson, and affordability. By treating the arterial pulse signal as a vibration signal of the arterial wall, vibration-model-based analysis of only one measured pulse signal with no calibration was conducted for simultaneous estimation of three arterial parameters. Exercise-intensity-normalized percent changes in arterial parameters were utilized to remove the influence of variation in exercise intensity on post-exercise response, and then their measured values were compared for difference in post-exercise response between the subjects.
Main Results
One subject who was obese, on subject who had insomnia, and the oldest subject in the study demonstrated differences in post-exercise response at the radial artery (RA), as compared with the three subjects free of those three factors. Despite a lack of statistical significance, the observed difference at the RA between subjects was supported by (i) their consistency with the related findings in the literature, and (ii) their consistency with the measured values at the carotid artery (CA) and superficial temporal artery (STA) and the anatomical difference between the three arteries.
Significance
The proposed method has the potential of offering an affordable and convenient diagnosis tool for routine arterial health assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arterial stiffness and endothelial function are two established surrogate markers of subclinical atherosclerosis and independent risk predictors of cardiovascular (CV) events.2,11,20,27 Arterial stiffness reflects the elasticity (E) of the arterial wall. Arterial stiffening (or increased E) precedes hypertension.33,35 Endothelial function commonly refers to the adaptation of arterial radius (r0) at diastolic blood pressure (DBP) in response to blood flow change.19,55 Endothelial dysfunction occurs earlier than arterial stiffening in subclinical atherosclerosis.30,58 The viscosity (η) of the arterial wall quantifies energy dissipation in the arterial wall, and its change in response to blood flow change was recently found to be regulated by both endothelial function and vascular tone (change in r0 in response to external stimuli).40 Hypertension impairs endothelial-dependent regulation of arterial viscosity (η) and causes a large increase in η during blood flow increase and thus an increase in cardiac workload.39 As such, arterial stiffness and endothelial function are quantitatively assessed with three arterial parameters: E, η, and r0.
The current non-invasive methods for arterial stiffness assessment essentially involve arterial pulse signal measurement at the skin surface using applanation tonometry and imaging instruments (e.g., ultrasound) and estimation of various arterial indices from the measured pulse signal, based on different models of the arterial pulse signal.34,42 A tonometer is essentially a tactile sensor and measures a pulsatile pressure signal (Δp(t)). Hold down pressure (PHD) acting on the tonometer is adjusted to flatten the artery for achieving zero transmural pressure (PT) in the arterial wall, at which E is the lowest and the amplitude (Δp0) of the measured Δp(t) is maximum. The measured pulse signal with maximum Δp0 is used for arterial indices estimation. To reduce distortion in an acquired pulse signal, alignment of the transducer at the center of an artery is critical but technically challenging, due to small size of an artery.34,42 The measured Δp0 needs to be calibrated with blood pressure at the brachial artery measured by a pressure cuff, in order to determine the true Δp0 of the artery. Inevitable off-center misalignment and the calibration cause measurement unreliability of a tonometer. An imaging instrument measures r0 at DBP and the radial motion signal (ur(t)) at an artery.3 Operation complexity of a tonometer and an imaging instrument demands a high degree of technical skill for achieving measurement reliability. High cost and operation complexity rule out their suitability for routine use by untrained individuals.
By treating the arterial pulse signal as a propagation wave signal (from the heart to the periphery), global and regional arterial stiffness are estimated from the pulse signals at two artery sites with a distance (L), which are measured using two tonometers. The time delay t between the two pulse signals is calculated for estimating the carotid-femoral pulse wave velocity (cfPWV), which is indicative of global arterial elasticity (E):3,34
where ρb is constant blood density and h is constant arterial wall thickness. cfPWV is the gold standard for global arterial stiffness, due to its acceptable measurement reliability (resulting from no need to calibrate the measured Δp0) and ease of measurement (no imaging instruments).35 Regional PWVs, such as carotid-radial PWV and ankle-brachial PWV are also measured.27,31
By treating the arterial wall as a viscoelastic material model, local arterial elasticity and viscosity are related to the Δp(t) and ur(t) signals measured at an artery site:24
where ρw is constant arterial wall density. One Δp(t) signal and one ur(t) signal are simultaneously measured by a tonometer and an imaging instrument at an artery site, respectively, to obtain a pressure-diameter hysteresis loop, which is analyzed by system-identification algorithms for estimating local viscosity. The local PWV is estimated by the amplitudes (Δp0 and \( u_{{r_{0} }} \)) of the two measured signals:
Due to its non-invasive nature, brachial Flow-Mediated Dilation (FMD) is the gold standard for endothelial function assessment. An imaging instrument is used to measure r0 at baseline and post-cuff release after a pressure cuff at the brachial artery is inflated for 5 min at 250 mmHg.18 Brachial FMD is assessed as the peak percent change in arterial diameter between post-cuff release and baseline.18
A bout of aerobic exercise induces changes in the cardiovascular (CV) system. Then, post-exercise response of the CV system manifests its functional regulation in response to external stimuli, and has been found to serve as a more sensitive detection of subclinical arterial anormalities that are not apparent at-rest.5,12,14,26,29,36,37,44,53 Numerous studies were conducted on post-exercise reponse of different CV parameters for their clinical values, but these studies varied greatly in exercise used (e.g., duration, intensity and modality) and the timing of the measurement post-exercise.5,12,14,26,29,36,37,44,53 Furthermore, post-exercise response of the CV system was found to vary greatly with both exercise intensity22,23,28 and the timing of the measurement post-exercise.32
To address all the above-mentioned concerns, this work aimed to propose a novel method that was built upon our previous studies.16,50,51 We developed a microfluidic tactile sensor for distributed-load detection16 and investigated its performance for arterial pulse signal measurements.51 The measured pulse signals by the sensor were found to capture the difference in pulse waveform between the radial artery (RA) and the carotid artery (CA) and the derived tonometric parameters were not sensitive to hold-down pressure used during pulse measurements.51 Recently, we developed vibration-model-based analysis of a measured pulse signal with no calibration for simultaneously extracting three arterial parameters: elasticity, viscosity, and radius of the arterial wall, and validated its feasibility of tracking their percent changes immediately post-exercise at the RA and the CA relative to at-rest with a small sample size (n = 5: one female and four male).50 Due to variation in exercise intensity, comparison in post-exercise response between the subjects was not conducted. Yet, comparison of post-exercise response of a subject against healthy condition holds the key for early detection of subclinical arterial abnormalities.5,12,14,26,29,36,37,44,53
Most recently, we measured pulse signals of two more young male subjects at the RA and the superficial temporal artery (STA). Among the six male subjects measured so far, one was obese, one had insomnia, and one (47 years old) was much older than the other five subjects. Since obesity, insomnia, and aging are all CV risk factors, this work attempted to examine the measured data for their capability of capturing difference in post-exercise response of the subjects under the factors, as compared with the rest subjects. The original contributions of this work include: (1) Exercise-intensity-normalized percent changes in arterial parameters were defined to remove the influence of variation in exercise intensity on post-exercise response so as to enable comparison of post-exercise response between the subjects; (2) The measured pulse signals of the four male subjects at the RA and the CA50 and the two male subjects at the RA and the STA were combined for analysis; and (3) the observed difference in post-exercise response at the RA between the subjects was validated by their consistency with the related findings in the literature and their consistency with the measured data at the CA and the STA and the anatomical difference between the three arteries. Taken together, the proposed method comprises of three key elements: (1) the microfluidic tactile sensor with a transducer array, (2) vibration-model-based analysis of a measured pulse signal for extracting three arterial parameters, and (3) exercise-intensity-normalized percent changes in arterial parameters relative to at-rest for comparison between subjects. Finally, it must be pointed out that since the measured data were not originally designed for the effect of aging, obesity, or insomnia on post-exercise response of arterial parameters, this work served as only a proof-of-concept study of the proposed method with no statistical significance.
Methods
A microfluidic tactile sensor with a location-insensitive configuration
As illustrated in Fig. 1a, the microfluidic tactile sensor is built on a Pyrex substrate. The core of the sensor is a polydimethylsiloxane (PDMS) microstructure with an electrolyte-filled microchannel embedded underneath. The two reservoirs are used to fill the microchannel with electrolyte and afterwards are sealed with PDMS. Five Au/Cr electrode pairs on the substrate are aligned along the microchannel length. Electrolyte in the microchannel and the five electrode pairs form a 5 × 1 resistive transducer array.16 Distributed-load acting on the microstructure deforms the microstructure and registers as resistance changes by the transducer array. Affordability of the sensor results from a standard microfluidics technology used for its fabrication. The details about the sensor design, fabrication, and operation can be found in the literature.16 As shown in Figs. 1b and 1c, in a pulse measurement, the sensor is flipped over and the transducer array is aligned perpendicular to the artery. The 6 mm-long transducer array allows a layperson to easily align at least one transducer above an artery. By pressing the sensor against an artery with a hold-down pressure (PHD), the pulsatile pulse signal (Δp(t)) in an artery deflects the microstructure and registers as a resistance change (ΔR(t)) by the transducer at the artery. As depicted in Fig. 1d, a location-insensitive configuration: a large flat sensor-artery contact zone (> 100 mm2) with the transducer array at the sensor center, offers immunity of location variation of the sensor relative to an artery for eliminating off-center misalignment and thus improving measurement accuracy.51 Figure 1e shows a measured pulse signal using the sensor. The details about the sensor and its use for arterial pulse measurements can be found in the literature.51
A microfluidic tactile sensor for arterial pulse signal measurements. (a) Schematic of the sensor, (b) working principle for pulse measurements, (c) picture of the sensor aligned at the RA, (d) schematic of the transducer array aligned at the center of a large flat sensor-artery contact zone for symmetrical arterial flattening (d) a measured pulse signal 0–5 min post-exercise.
Vibration-Model-Based Analysis of a Measured Pulse Signal for Estimation of Arterial Parameters
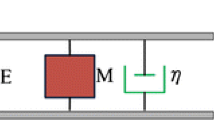
The details about vibration-model-based analysis of a measured pulse signal for estimation of arterial parameters can be found in the literature.50 For completeness, a brief description of this analysis is given here. The measured pulse waveform ΔR(t) is considered as the arterial radius waveform ur(t).52 Due to its time-harmonic nature, ur(t) is treated as a vibration signal of the arterial wall, which is then modeled as a unit-mass dynamic system (M = 1) with a driving force (Fr), as shown in Fig. 2:50
Vibration model of the arterial wall. (a) The arterial wall undergoes vibrations ur(t) in the radial direction upon the pulsatile pressure Δp(t) in the artery with diastolic blood pressure (DBP), (b) the arterial wall is modeled as a unit-mass dynamic system for mathematically describing its vibrations.
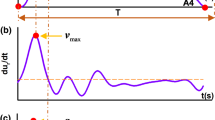
The arterial parameters dictate the spring stiffness (K) and damping coefficient (D). They are derived from the key features in the measured pulse waveform (ur(t)) and its two derivatives, as labeled in Fig. 3a. Note that the vibration amplitude is \( u_{{r_{0} }} \) in ur(t) and the maximum velocity is vmax in the 1st derivative of ur(t). Based on Eq. (4), the spring force amplitude is product of the spring stiffness and the vibration amplitude: K·\( u_{{r_{0} }} \), and the damping force amplitude is product of the damping coefficient and the maximum velocity: D·vmax. Here, the maximum change in acceleration (amax − amin) from the 2nd derivative of ur(t) is used to represent the driving force amplitude (Fr0):
An arterial radius pulse waveform, its 1st-order derivative (velocity), and 2nd-order derivative (acceleration) of Subject 6 at the RA. (a) at-rest (or pre-exercise) with all the key features being labeled for extraction of spring stiffness and damping coefficient, (b) comparison of the measured pulse waveform and its two derivatives between at-rest and 0–5 min post-exercise.
where T is the pulse duration and Δt/T factors in heart rate (HR) change accompanying changes in arterial parameters. The spring force amplitude (K·\( u_{{r_{0} }} \)) and the damping force amplitude (D·vmax) are expected to be proportional to \( F_{{r_{0} }} \):
As shown in Fig. 3b, both the pulse duration is shortened and all the key features in ur(t) and its two derivatives are altered 0–5 min post-exercise, relative to pre-exercise (or at-rest), possibly indicating that the arterial parameters might be different between at-rest and 0–5 min post-exercise.
Based on the hemodynamic model of blood flow,50 the arterial parameters and PWV at an artery site can be related to K and D by:
No calibration is needed for the true amplitudes of the measured pulse waveform and its derivatives, since E, η, r0 and PWV are essentially estimated by taking their ratios. As ratios, the estimated values are relative, have no units, and thus do not represent true values of arterial parameters and PWV.
Post-exercise Response of Arterial Parameters
The measured pulse signal results from a combination of the sensor, the arterial wall, the true pulse signal in an artery, and subject-specific factors (i.e., overlying tissue above an artery, artery size, and DBP).45 Given the same sensor design, estimated values of arterial parameters are influenced by subject-specific factors and artery sites, and thus are unsuitable for comparison between subjects and between artery sites.45 To remove the influence of subject-specific factors on the estimated values, we estimate the percent changes in arterial parameters and PWV 0–5 min post-exercise of a subject, relative to at-rest:
where \( \Delta E = E_{\text{post - exer}} - E_{\text{at - rest}} \), \( \Delta \eta = \eta_{\text{post - exer}} - \eta_{\text{at - rest}} \), \( \Delta r_{0} = r_{{0\;{\text{post - exer}}}} - r_{{0\;{\text{at - rest}}}} \), and \( \Delta PWV = PWV_{\text{post - exer}} - PWV_{\text{at - rest}} \).
It is unpractical to precisely control exercise intensity for different subjects, but percent changes in arterial parameters and PWV vary with exercise intensity.22,23,28 Since exercise intensity is linearly proportional to heart rate (HR) increase and there is inter-subject variation in HR at-rest,17 the percent change in HR 0–5 min post-exercise, relative to at-rest, is defined to quantify exercise intensity:
Then, we normalize the percent changes in arterial parameters and PWV to exercise intensity:
These exercise-intensity-normalized percent changes remove the influence of variation in exercise intensity on post-exercise response and are suitable for comparison between subjects.
Arterial Pulse Signal Measurements At-Rest and 0–5 Min Post-exercise
This study was approved by the Institutional Review Board (IRB) of Old Dominion University. Under one protocol, four asymptomatic male subjects (n = 4) were measured at the RA and the CA,50 and their blood pressure was not measured, due to the lack of a medical instrument for its measurement. Later on, under another protocol, two other asymptomatic male subjects (n = 2) were measured at the RA and the STA, and their systolic/diastolic blood pressure (SBP/DBP) was measured using a PARAMED blood pressure monitor. In a measurement, a subject stayed in a sitting position and remained still, and the pulse signals at two artery sites on the right side of the body were simultaneously measured using two sensors of identical design. Afterwards, the subject performed moderate-intensity exercise (either jump up/down or squat) for 5 min. The pulse signals at the same two artery sites were simultaneously measured 0–5 min post-exercise. Five pulse cycles from each measured pulse signal at-rest and 0–5 min post-exercise were processed to estimate the exercise-intensity-normalized percent changes in arterial parameters and PWV in Eq. (10). Note that the measured pulse signals at the CA of one subject (Subject 3 in Table 1) were unclear and were not included in the results. SBP/DBP was measured on the left brachial artery simultaneously with the pulse signals. The recorded SBP/DBP was the average of three measurements at-rest and 0–5 min post-exercise, respectively. Pulsatile pressure (ΔP) was calculated as the difference between SBP and DBP: ΔP = SBP − DBP.
Results
Table 1 summarizes the age, body mass index (BMI) and the estimated values of arterial parameters, PWV, HRat-rest and ΔHR% of the six subjects. Except HR, the estimated values of arterial parameters and PWV do not represent their true values, because all of these parameters are estimated from the K and D values that include the contributions of subject-specific factors and artery sites. For instance, the arterial radius decreases from the CA, the RA to the STA, but the estimated r0 values at the three artery sites reveal the opposite. Similarly, the estimated values of E, η and PWV at the same artery site of these subjects bear the influence of subject-specific factors.
As shown in Fig. 4a, Subjects 2, 3 and 5 are physically active and revealed low \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the RA, as compared with Subjects 1 and 6. As the oldest in the group, Subject 1 revealed higher \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values than the three physically active subjects. As the obese and the youngest subject in the group, Subject 6 revealed the highest \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the RA, and his \( \overline{\Delta E} \% \) value was higher than those of the physically active subjects, but was much lower than that of Subject 1. Subject 4 suffered insomnia for several days prior to the measurement and revealed a much higher \( \overline{\Delta E} \% \) value, which was comparable with that of Subject 1, but his \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values were comparable with their counterparts of the physically active subjects. As shown in Fig. 4b, the two subjects who were either obese or suffered from insomnia and the oldest subject all registered a high \( \overline{\Delta PWV} \% \) value, as compared with the three physically active subjects.
As illustrated in Fig. 5, the \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \), and \( \overline{\Delta PWV} \% \) values at the CA of Subject 1 were all higher than those of Subject 2. The \( \overline{\Delta E} \% \) and \( \overline{\Delta PWV} \% \) values at the CA of Subject 4 were much higher than those of Subject 2, but were comparable with those of Subject 1. The \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values of Subject 4 were comparable with those of Subject 2. The \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \), and \( \overline{\Delta PWV} \% \) values at the CA of the three subjects were consistent with their counterparts at the RA. Interestingly, the RA registered much higher values for all these parameters than the CA.
Figures 6a and 6b compare the difference in \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \), and \( \overline{\Delta PWV} \% \) values between the RA and the STA of Subjects 5 and 6, respectively. While Subject 5 revealed much higher \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the STA than at the RA, Subject 6 registered the opposite. The \( \overline{\Delta E} \% \) values at the STA and the RA were comparable in Subject 5. In contrast, Subject 6 registered an extremely high \( \overline{\Delta E} \% \) value at the STA, compared with that at the RA. The \( \overline{\Delta PWV} \% \) value at the STA was higher than that at the RA in the two subjects. This consistency in \( \overline{\Delta PWV} \% \) value between the two artery sites in the two subjects justified that this high \( \overline{\Delta E} \% \) value at the STA in Subject 6 was not a measurement error.
Comparison in energy-intensity-normalized percentage changes in arterial parameters and PWV between the RA and the STA of (a) Subject 5 and (b) Subject 6. Comparison in exercise-intensity-normalized percentage changes in arterial parameters, PWV and ΔP (c) at the STA and (d) at the RA between the two subjects.
Figures 6c and 6d compare the difference in \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \), \( \overline{\Delta PWV} \% \), and \( \overline{\Delta (\Delta P)} \% \) values at the RA and the STA, respectively, of the two subjects, where \( \overline{\Delta (\Delta P)} \% = {{(\Delta (\Delta P)} \mathord{\left/ {\vphantom {{(\Delta (\Delta P)} {\Delta P_{\text{at - rest}} }}} \right. \kern-0pt} {\Delta P_{\text{at - rest}} }})/\Delta HR\% \) is the exercise-intensity-normalized percent change in pulsatile pressure (ΔP). Subject 5 revealed much lower \( \overline{\Delta PWV} \% \) values at the two artery sites than Subject 6, which were consistent with the difference in their \( \overline{\Delta (\Delta P)} \% \) values. While the \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the STA in Subject 5 were higher than those in Subject 6, these values at the RA in Subject 5 were much lower than those in Subject 6. The \( \overline{\Delta E} \% \) values at the two artery sites in Subject 5 were both lower than those in Subject 6.
Discussion
Technical Advantages
Arising from the dependence of a measured pulse signal on subject-specific factors, the estimated values of arterial parameters and PWV at-rest are influenced by subject-specific factors and artery sites, and thus are unsuitable for comparison between subjects and between artery sites. As can be seen in Table 1, Subjects 2, 3, and 5 are physically active, but their estimated values of E, η and PWV do not indicate better or poorer arterial health, as compared with the other three subjects. Similarly, applanation tonometers, as tactile sensors, are also subject to the influence of subject-specific factors and this is the reason that their measured pulse signals need to be calibrated for estimation of local E and η. Since the calibration for applanation tonometers cannot take subject-specific factors into account, measurement errors in their calibrated results are still contaminated by subject-specific factors (e.g., high BMI vs. low BMI).50 In contrast, as defined in Eq. (8), percent changes in these parameters relative to at-rest are immune to subject-specific factors.
The location-insensitive configuration in the sensor warrants symmetrical arterial flattening in a measurement and thus eliminates distortion in a measured pulse signal due to off-center misalignment. The main concern is variation in transmural pressure (PT) between different measurements. As shown in Fig. 2(a), PT is the difference between the external pressure outside the arterial wall and DBP: PT = Pext − DBP, and has a notorious effect on E, since E is a sigmoid function of PT: when PT = 0, E is the lowest and E dramatically increases when PT is either negative or positive.49PT variation causes unpredictable errors in the estimated values from a measured pulse signal. Since PHD affects PT through Pext, the estimated value of E is affected by PHD. No studies have reported on the effect of PT on η. For practical utility, we used two fingers to hold the sensor at an artery and adjusted finger-holding strength to qualitatively control PHD for achieving PT ≅ 0 through monitoring the pulse signal for its maximum amplitude. Moreover, moderate exercise intensity (ΔHR% ≥ 30%) introduced relatively large changes in arterial parameters between at-rest and 0–5 min post-exercise, and thus alleviated the influence of PT variation between the two measurements on percent changes in arterial parameters and PWV. It is worth mentioning that a feedback-control mechanism (as used in a tonometer) might not be practical for achieving PT ≅ 0 here, because it constantly adjusts PHD to respirations of a subject and thus introduces extra distortion to the measured pulse signal and also undermines the operation simplicity and affordability of the proposed method.
In our previous work,50 we manually controlled PT and successfully tracked the percent changes defined in Eq. (8) relative to at-rest with statistical significance, which are consistent with findings in the literature:32E goes up dramatically 0–5 min post-exercise and then drops over time post-exercise; r0 drops 0–5 min post-exercise and then goes up. η was found to go up dramatically 0–5 min post-exercise and then drop. No other studies have reported on post-exercise response of η. However, our previous work50 focused on validating the feasibility of the vibration-model-based analysis to track percent changes in Eq. (8) at the RA and the CA, and comparison of the measured values between the subjects was not conducted, due to variation in energy intensity between the subjects. In this work, exercise-intensity-normalized percent changes were defined in Eq. (10) to remove the influence of variation in exercise intensity on post-exercise response so that their measured values became suitable for comparison between subjects.
Qualitative Validation of the Measured Data
Related Findings on Arterial Stiffness and Endothelial Function in the Literature
Since arterial stiffness and endothelial function are well established clinical indices for diagnosis of CV diseases and surrogate markers for early detection of subclinical atherosclerosis,2,11,20,27 the effects of various CV risk factors, including aging, obesity, and insomnia, on these two indices have been studied.2,4,6,10,11,20,21,27,41,43,46,48,57 Numerous studies have established that both arterial stiffness and endothelial function deteriorate under aging.2,11,20,27 It is also established that obesity is associated with increased arterial stiffness46,57 and impaired endothelial dysfunction.4,10 Several studies found that sleep deprivation increases arterial stiffness21,48 and cause endothelial dysfunction in healthy subjects.6,41,43
Owing to technical difficulty involved in measurement of arterial stiffness and endothelial function, post-exercise response of the CV system for arterial health assessment has been mostly measured by blood pressure changes.1,7,8,9,15,25,47,54,56 An exaggerated blood pressure response to exercise has been associated with a greater risk of future hypertension, various CV risk factors, and adverse CV outcomes.15 For instance, as compared with young men, aged men exhibited a greater increase in blood pressure in response to exercise.8,47 Insomnia was found to induce a greater blood pressure response to exercise in otherwise healthy subjects.7,15 Other than an exaggerated blood pressure response,9 obesity was also found to cause a greater increase in cfPWV following exercise, as compared with normal weight.29
In this work, we hypothesize that physically active subjects register lower \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \), \( \overline{\Delta PWV} \% \), and \( \overline{\Delta (\Delta P)} \% \) values, as compared with subjects under CV risk factors, because of the following two reasons: (1) CV risk factors have been associated with an exaggerated blood pressure response to exercise;1,7,8,15,25,47,54 (2) as compared with sedentary subjects, physically active subjects have been found to need less CV adjustment to accommodate exercise and show less acute post-exercise response of multiple CV parameters to the same amount of exercise.22,23,28 Although changes in arterial stiffness and endothelial function caused by subclinical arterial abnormalities in asymptomatic subjects may not be detectable at-rest, such undetectable changes might weaken functional regulation of arterial stiffness and endothelial function by the CV system in response to exercise, given the fact that post-exercise response of the CV system reveals subclinical arterial abnormalities that are not apparent at-rest.5,12,14,26,29,36,37,44,53 As such, we further hypothesize that a high \( \overline{\Delta E} \% \) value represents weakened regulation of arterial stiffness and high \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values represent weakened regulation of endothelial function.
Consistency of the Measured Data at the RA with the Related Findings in the Literature
Subject 1 revealed higher \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the RA than the three physically active subjects: 2, 3, and 5, possibly indicating the aging of Subject 1 weakened the regulation of arterial stiffness and endothelial function. It is well established that arterial stiffness and endothelial function deteriorate under aging.2,11,20,27 One study suggested that changes in arterial stiffness might play a role in post-exercise response of pulsatile pressure.1 As compared with Subjects 2, 3, and 5, arterial stiffness and endothelial function of Subject 1 may be deteriorated due to increased age compared to the rest of the subjects, which might be the cause of the observed weakened regulation of E, η and r0.
Subject 6 revealed much higher \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values and lower \( \overline{\Delta E} \% \) value than Subject 1. The \( \overline{\Delta E} \% \) value in Subject 6 was higher than those of Subjects 2, 3, and 5. The observed difference between these subjects might indicate that obesity of Subject 6 undermines the regulation of endothelial function (or r0) to a more severe extent or at an earlier stage than the regulation of arterial stiffness and also severely weakens the regulation of endothelial-dependent η to increased blood flow.53 These observations are consistent with the findings: obesity causes both arterial stiffening and endothelial dysfunction,4,10,46,57 and endothelial dysfunction occurs earlier than arterial stiffening in subclinical atherosclerosis.39
Subject 4 revealed a much higher \( \overline{\Delta E} \% \) value, but his \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values were comparable with those of the physically active subjects, possibly indicating that short-term insomnia of Subject 4 has a more severe effect on the regulation of arterial stiffness than on the regulation of endothelial function. Acute sleep deprivation was found to undermine both arterial stiffness and endothelial function.6,21,41,43,48 However, we only observed its adverse effect on the regulation of arterial stiffness. Given the consistency in the observed post-exercise response of arterial parameters and PWV between the RA and the CA in Subject 4, the low \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \) values of Subject 4 were not believed to result from measurement errors.
Consistency of the Measured Data at the RA with Their Counterparts at the CA and the STA and the Anatomical Difference Between the Three Arteries
The anatomy, geometry, and mechanical properties of the arterial wall vary along the arterial tree,27,33 and accordingly post-exercise response of arterial parameters is expected to vary between the three arteries measured. The \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \), and \( \overline{\Delta PWV} \% \) values at the RA were higher than their counterparts at the CA. On the one hand, this difference might indicate that the RA may need to adjust its arterial parameters much more to accommodate exercise. On the other hand, as compared with the CA (an elastic artery), the RA is a muscular artery and contains more smooth muscle cells in the arterial wall.9 Thus, the RA is capable of adjusting its arterial parameters much more than the CA to accommodate exercise.
As to Subject 5, the STA registered a low \( \overline{\Delta E} \% \) value and high \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values, compared with their counterparts at the RA. Different from the RA, the STA contains numerous smooth muscle cells and very few elastic fibers and is supplied with sympathetic nerves.13 Sympathetic nerves of the STA have been considered as the cause of the vasospasm after STA-MCA (middle cerebral artery) bypass, in which the STA is used as a graft, since sympathetic nerves generally bring about vasoconstriction.38 This may explain higher \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the STA than at the RA. Consequently, a low \( \overline{\Delta E} \% \) value at the STA is needed to increase the \( \overline{\Delta PWV} \% \) value at the STA. In contrast, Subject 6 registered the opposite between the RA and the STA. This might indicate that obesity of Subject 6 impairs the function of sympathetic nerves and causes low \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) values at the STA. Accordingly, an extremely high \( \overline{\Delta E} \% \) value at the STA is needed to increase the \( \overline{\Delta PWV} \% \) value at this artery site.
The \( \overline{\Delta PWV} \% \) value at the RA is higher than that at the CA, but is lower than that at the STA. Such difference between the three arteries possibly indicates that smaller arteries need to adjust their PWV more to facilitate increased blood flow. Despite significant difference in \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), and \( \overline{{\Delta r_{0} }} \% \) values at the RA and the STA between the two subjects, the consistency of the \( \overline{\Delta PWV} \% \) value at the RA with that at the STA in the two subjects was observed. This might indicate that the three arterial parameters under different arterial health conditions compensate for each other, in order to achieve the PWV demanded by the whole CV system. As such, the unified theme of the regulation of three arterial parameters at different arteries might be the regulation of PWV along the arterial tree to achieve the essential function of the CV system—blood circulation.52 Finally, it should be noted that (i) \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \) and \( \overline{\Delta PWV} \% \) at the RA are more sensitive than \( \overline{\Delta (\Delta P)} \% \) for detecting the effects of obesity on post-exercise response of the CV system; and (ii) as compared with \( \overline{\Delta PWV} \% \), \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \) and \( \overline{{\Delta r_{0} }} \% \) can distinguish the regulation of arterial stiffness from the regulation of endothelial function and thus provide a more comprehensive assessment of arterial health.
Study Limitations
There are two major study limitations. First, since the measured data on the six subjects (n = 6) were not originally designed for different effects of aging, obesity, or insomnia on arterial stiffness and endothelial function, the observed difference in post-exercise response lacked in statistical significance. Nevertheless, the observed differences in \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \) and \( \overline{\Delta PWV} \% \) at the RA between the three subjects under these factors and the rest three subjects free of these factors was supported by their consistency with the related findings in the literature and their consistency with the measured data at the CA and the STA and the anatomical difference between the three arteries, instead of random measurement variations or errors. Second, the estimated \( \overline{\Delta E} \% \), \( \overline{\Delta \eta } \% \), \( \overline{{\Delta r_{0} }} \% \) and \( \overline{\Delta PWV} \% \) could not be quantitatively validated with the related findings in the literature, due to heterogeneity of the subject populations, the use of different measurement methodologies, and duration, intensity, and modality of exercise used, as described in a recent systematic review on post-exercise response of arterial stiffness, which summarized all the studies on assessing central and upper body peripheral arterial segments 0–5 min post-exercise, but did not conduct quantitative comparison between those studies.32
Conclusion
In this proof-of-concept study, a novel method for arterial health assessment was proposed that includes (1) a microfluidic tactile sensor with a transducer array offering low-cost and ease use by a layperson, (2) vibration-model-based analysis of a measured pulse signal with no calibration for extraction of three arterial parameters, and (3) energy-intensity-normalized percent changes of arterial parameters 0–5 min post-exercise, relative to at-rest, for comparison between subjects. Six asymptomatic male subjects were measured and two of them had either obesity or insomnia. Additionally, a third subject was identified as the oldest subject in the group. As compared with the rest of the subjects, they revealed their own difference in the measured values on energy-intensity-normalized percent changes of arterial parameters and PWV. Despite a lack of statistical significance, the observed difference at the RA between the subjects was supported by (1) their consistency with the related findings in the literature, and (2) their consistency with the measured values at the carotid artery (CA) and superficial temporal artery (STA) and the anatomical difference at the three arteries. Particularly, the measured \( \overline{\Delta PWV} \% \) of the six subjects at the three arteries identifies the unified theme of the regulation of three arterial parameters at different arteries by the CV system—the regulation of PWV along the arterial tree for achieving blood circulation. Further feasibility studies on the proposed method should be conducted for statistical significance for early detection of subclinical atherosclerosis. Evidently, the proposed method can be easily adopted for assessing coronary artery disease (CAD) through cardiac stress testing and therapeutic outcomes of CV patients. As compared with the current techniques (applanation tonometry and imaging instruments), the proposed method holds the promise of offering an affordable and convenient diagnosis tool for arterial health assessment.
References
Akazawa, N., S. G. Ra, J. Sugawara, and S. Maeda. Influence of aerobic exercise training on post-exercise responses of aortic pulse pressure and augmentation pressure in postmenopausal women. Front. Physiol. 6:268, 2015.
Anderson, T. J. Arterial stiffness or endothelial dysfunction as a surrogate marker of vascular risk. Can. J. Cardiol. 22:72B–80B, 2006.
Bruno, R. M., E. Bianchini, F. Faita, S. Taddei, and L. Ghiadoni. Intima media thickness, pulse wave velocity, and flow mediated dilation. Cardiovasc. Ultrasound 12:34, 2014.
Buie, J. J., L. S. Watson, C. J. Smith, and C. Sims-Robinson. Obesity-related cognitive impairment: The role of endothelial dysfunction. Neurobiol. Dis. 132:104580, 2019.
Bunsawat, K., S. M. Ranadive, A. D. Lane-Cordova, H. Yan, R. M. Kappus, B. Fernhall, et al. The effect of acute maximal exercise on postexercise hemodynamics and central arterial stiffness in obese and normal-weight individuals. Physiol. Rep. 5:e13226, 2017.
Calvin, A. D., N. Covassin, W. K. Kremers, et al. Experimental sleep restriction causes endothelial dysfunction in healthy humans. J. Am. Heart Assoc. 3(6):e001143, 2014.
Cincin, A., I. Sari, M. Oguz, S. Sert, M. Bozbay, H. Atas, B. Ozben, K. Tigen, and Y. Basaran. Effect of acute sleep deprivation on heart rate recovery in healthy young adults. Sleep Breath 19:631–636, 2015.
Deschenes, M. R., J. A. Carter, E. N. Matney, M. B. Potter, and M. H. Wilson. Aged men experience disturbances in recovery following submaximal exercise. J. Gerontol. Ser. A 61A(1):63–71, 2006.
Dipla, K., G. P. Nassis, and I. S. Vrabas. Blood pressure control at rest and during exercise in obese children and adults. J. Obes. 2012. https://doi.org/10.1155/2012/147385.
Engin, A. Endothelial dysfunction in obesity. Adv. Exp. Med. Biol. 960:345–379, 2017.
Federaal Kenniscentrum—Centre Fédéral d’Expertise. Non-invasive markers of subclinical atherosclerosis for predicting a primary cardiovascular event: a rapid systematic review. http://kce.fgov.be/publication/report/novel-serum-biomarkers-for-the-prediction-of-cardiovascular-risk#.WNvfcG8rJaR, 2013.
Franklin, N. C., M. Ali, M. Goslawski, E. Wang, and S. A. Phillips. Reduced vasodilator function following acute resistance exercise in obese women. Front. Physiol. 5:253, 2014.
Girerd, X., J.-J. Mourad, C. Acar, D. Heudes, S. Chiche, P. Bruneval, et al. Noninvasive measurement of medium-sized artery intima-media thickness in humans: in vitro validation. J. Vasc. Res. 31:114–120, 1994.
Gonzales, J. U., B. C. Thompson, J. R. Thistlethwaite, and B. W. Scheuermann. Association between exercise hemodynamics and changes in local vascular function following acute exercise. Appl. Physiol. Nutr. Metab. 36:137–144, 2011.
Goyal, G., R. Sharma, S. Joshi, and A. Bhardwaj. Effect of sleep deprivation on heart rate recovery after treadmill testing in otherwise healthy young adults. Natl. J. Physiol. Pharm. Pharmacol. 9(1):19–22, 2019.
Gu, W., P. Cheng, A. Ghosh, Y. Liao, B. Liao, A. Beskok, et al. Detection of distributed static and dynamic loads with electrolyte-enabled distributed transducers in a polymer-based microfluidic device. J. Micromech. Microeng. 23:035015, 2013.
Harold Laughlin, M. Cardiovascular response to exercise. Am. J. Physiol. 277(6 Pt 2):S244–S259, 1999.
Harris, R. A., S. K. Nishiyama, D. W. Wray, and R. S. Richardson. Ultrasound assessment of flow-mediated dilation. Hypertension 55:1075–1085, 2010.
Inaba, Y., J. A. Chen, and S. R. Bergmann. Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int. J. Cardiovasc. Imaging 26:631–640, 2010.
Iurciuc, S., A. M. Cimpean, F. Mitu, R. Heredea, and M. Iurciuc. Vascular aging and subclinical atherosclerosis: why such a “never ending” and challenging story in cardiology? Clin. Interv. Aging 12:1339–1345, 2017.
Kim, C. W., Y. Chang, D. Zhao, et al. Sleep duration, sleep quality, and markers of subclinical arterial disease in healthy men and women. Arterioscler. Thromb. Vasc. Biol. 35:2238–2245, 2015.
Liu, H.-B., W.-X. Yuan, K.-R. Qin, and J. Hou. Acute effect of cycling intervention on carotid arterial hemodynamics: basketball athletes versus sedentary controls. Biomed. Eng. Online 14:S17, 2015.
Liu, H.-B., W.-X. Yuan, Q.-Y. Wang, Y.-X. Wang, H.-W. Cao, J. Xu, et al. Carotid arterial stiffness and hemodynamic responses to acute cycling intervention at different times during 12-week supervised exercise training period. BioMed Res. Int. 2018. https://doi.org/10.1155/2018/2907548.
London, G. M., and B. Pannier. Arterial Functions: How to Interpret the Complex Physiology. Oxford: Oxford University Press, 2010.
Michishita, R., M. Ohta, M. Ikeda, Y. Jiang, and H. Yamato. An exaggerated blood pressure response to exercise is associated with nitric oxide bioavailability and inflammatory markers in normotensive females. Hypertens. Res. 39:792–798, 2016.
Millen, A. M., A. J. Woodiwiss, and G. R. Norton. Post-exercise effects on aortic wave reflection derived from wave separation analysis in young-to middle-aged pre-hypertensives and hypertensives. Eur. J. Appl. Physiol. 116:1321–1329, 2016.
Mitchell, G. F., S.-J. Hwang, R. S. Vasan, M. G. Larson, M. J. Pencina, N. M. Hamburg, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 121:505, 2010.
Miyai, N., M. Arita, K. Miyashita, I. Morioka, T. Shiraishi, and I. Nishio. Blood pressure response to heart rate during exercise test and risk of future hypertension. Hypertension 39:761–766, 2002.
Moore, S. M., A. J. Berrones, J. L. Clasey, M. G. Abel, and B. S. Fleenor. Arterial hemodynamics are impaired at rest and following acute exercise in overweight young men. Vasc. Med. 21:497–505, 2016.
Mudau, M., A. Genis, A. Lochner, and H. Strijdom. Endothelial dysfunction: the early predictor of atherosclerosis. Cardiovasc. J. Africa 23:222, 2012.
Munakata, M. Brachial-ankle pulse wave velocity: background, method, and clinical evidence. Pulse 3:195–204, 2015.
Mutter, A. F., A. B. Cooke, O. Saleh, Y.-H. Gomez, and S. S. Daskalopoulou. A systematic review on the effect of acute aerobic exercise on arterial stiffness reveals a differential response in the upper and lower arterial segments. Hypertens. Res. 40:146, 2017.
O’Rourke, M. F., and G. Mancia. Arterial stiffness. J. Hypertens. 17:1–4, 1999.
O’Rourke, M. F., A. Pauca, and X. J. Jiang. Pulse wave analysis. Br. J. Clin. Pharmacol. 51:507–522, 2001.
Pereira, T., C. Correia, and J. Cardoso. Novel methods for pulse wave velocity measurement. J. Med. Biol. Eng. 35:555–565, 2015.
Perissiou, M., T. G. Bailey, M. Windsor, M. C. Y. Nam, K. Greaves, A. S. Leicht, et al. Effects of exercise intensity and cardiorespiratory fitness on the acute response of arterial stiffness to exercise in older adults. Eur. J. Appl. Physiol. 118:1673–1688, 2018.
Phillips, S. A., E. Das, J. Wang, K. Pritchard, and D. D. Gutterman. Resistance and aerobic exercise protects against acute endothelial impairment induced by a single exposure to hypertension during exertion. J. Appl. Physiol. 110:1013–1020, 2011.
Reddy, S., P. Kumar, and K. Prasad. Histomorphometric and sympathetic innervation of the human superficial temporal artery. Indian J. Plast. Surg. 44:127, 2011.
Roca, F., J. Bellien, M. Iacob, and R. Joannides. Endothelium-dependent adaptation of arterial wall viscosity during blood flow increase is impaired in essential hypertension. Atherosclerosis 285:102–107, 2019.
Roca, F., M. Iacob, I. Remy-Jouet, J. Bellien, and R. Joannides. Evidence for a role of vascular endothelium in the control of arterial wall viscosity in humans. Hypertension 71:143–150, 2018.
Routledge, F. S., S. B. Dunbar, M. Higgins, A. E. Rogers, C. Feeley, O. Ioachimescu, K. Euwer, D. Eapen, and A. Quyyumi. Insomnia symptoms are associated with abnormal endothelial function. J. Cardiovasc. Nurs. 32:78–85, 2017.
Saba, P., C. Cavallini, D. Scorzoni, C. Longhini, R. Pini, and A. Ganau. Arterial tonometry: principles and clinical applications in hypertension. High Blood Press. Cardiovasc. Prev. 5:241–250, 1996.
Sauvet, F., G. Leftheriotis, and D. Gomez-Merino. Effect of acute sleep deprivation on vascular function in healthy subjects. J. Appl. Physiol. 108(1):68–75, 2010.
Shim, C. Y., W.-I. Yang, S. Park, M.-K. Kang, Y.-G. Ko, D. Choi, et al. Overweight and its association with aortic pressure wave reflection after exercise. Am. J. Hypertens. 24:1136–1142, 2011.
Singh, P., M. I. Choudhury, S. Roy, and A. Prasad. Computational study to investigate effect of tonometer geometry and patient-specific variability on radial artery tonometry. J. Biomech. 58:105–113, 2017.
Stapleton, P. A., M. E. James, A. G. Goodwill, and J. C. Frisbee. Obesity and vascular dysfunction. Pathophysiology 15:79–89, 2008.
Stratton, J., W. Levy, M. Cerqueira, R. Schwartz, and I. Abrass. Cardiovascular responses to exercise effects of aging and exercise training in healthy men. Circulation 89:1648–1655, 1994.
Sunbul, M., B. G. Kanar, E. Durmus, T. Kivrak, and I. Sari. Acute sleep deprivation is associated with increased arterial stiffness in healthy young adults. Sleep Breath 18(1):215–220, 2014.
Teng, X.-F., and Y.-T. Zhang. Theoretical study on the effect of sensor contact force on pulse transit time. IEEE Trans Biomed Eng. 54:1490–1498, 2007.
Wang, D., L. Reynolds, T. Alberts, L. Vahala, and Z. Hao. Model-based analysis of arterial pulse signals for tracking changes in arterial wall parameters: a pilot study. Biomech Model Mechanobiol 18:1629–1638, 2019.
Wang, D., J. Shen, L. Mei, S. Qian, J. Li, and Z. Hao. Performance investigation of a wearable distributed-deflection sensor in arterial pulse waveform measurement. IEEE Sens. J. 17:3994–4004, 2017.
Wang, D., L. Vahala, and Z. Hao. Radial and longitudinal motion of the arterial wall: their relation to pulsatile pressure and flow in the artery. Phys. Rev. E. 98:032402, 2018.
Yan, H., S. M. Ranadive, K. S. Heffernan, A. D. Lane, R. M. Kappus, M. D. Cook, et al. Hemodynamic and arterial stiffness differences between African-Americans and Caucasians after maximal exercise. Am. J. Physiol. Heart Circul. Physiol. 306:H60–H68, 2013.
Yang, W. I., J. S. Kim, S. H. Kim, J. Y. Moon, J. H. Sung, I. J. Kim, S. W. Lim, D. H. Cha, and S. Y. Cho. An exaggerated blood pressure response to exercise is associated with subclinical myocardial dysfunction in normotensive individuals. J. Hypertens. 32(9):1862–1869, 2014.
Yoboah, J., A. Folsom, G. Burke, C. Johnson, J. Polak, W. Post, et al. Predictive value of brachial flow mediated dilation for incident cardiovascular events in a population-based study. Circulation 120:502–509, 2009.
Yzaguirre, I., G. Grazioli, M. Domenech, A. Vinuesa, R. Pi, J. Gutierrez, A. Coca, J. Brugada, and M. Sitges. Exaggerated blood pressure response to exercise and late-onset hypertension in young adults. Blood Press. Monit. 22(6):339–344, 2017.
Zebekakis, P. E., T. Nawrot, L. Thijs, E. J. Balkestein, J. van der Heijden-Spek, L. M. Van Bortel, H. A. Struijker-Boudier, M. E. Safar, and J. A. Staessen. Obesity is associated with increased arterial stiffness from adolescence until old age. J. Hypertens. 23:1839–1846, 2005.
Zhang, B., J. Gu, M. Qian, L. Niu, and D. Ghista. Study of correlation between wall shear stress and elasticity in atherosclerotic carotid arteries. Biomed. Eng. Online 17:5, 2018.
Acknowledgment
This study was approved by the Institutional Review Board (IRB) of Old Dominion University).
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Zhongjun Wu oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hao, Z., Wang, D. & Reynolds, L. Post-exercise Response of Arterial Parameters for Arterial Health Assessment Using a Microfluidic Tactile Sensor and Vibration-Model-Based Analysis: A Proof-of-Concept Study. Cardiovasc Eng Tech 11, 295–307 (2020). https://doi.org/10.1007/s13239-020-00454-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-020-00454-2