Abstract
Blood Pressure (BP) is considered a significant indicator of cardiac risk. By providing information about the hemodynamic load on the heart, BP detected in a central site may have added value with respect to the more familiar peripheral arterial pressure (i.e. measured on the brachial artery). Laser Doppler Vibrometry (LDV) has been demonstrated to be a reliable non-contact technique to measure the cardiovascular signals and parameters. LDV has a high sensitivity of acquisition and it is able to measure the skin vibrations related to cardiac activity when the laser beam is pointed in correspondence of the carotid artery. The obtainable vibrational signal (i.e. a velocity signal), VibroCardioGram (VCG), can provide relevant physiological parameters, including Heart Rate (HR) as well as more advanced features encoded in the contour of the pulse waveform. In this work, the authors aim to discuss the possibility of deriving the blood pressure signal from the vibrations of the carotid artery detected by LDV. 6 healthy participants were tested; the VCG was calibrated by means of diastolic and mean arterial pressure values measured by means of an oscillometric cuff. An exponential model was applied to the VCG signal of each participant in order to derive the pressure waveform from the displacement of the investigated vessel. Results show an average difference of around 20% between systolic pressure measured at brachial level (i.e. peripheral pressure value) and systolic pressure derived from VCG signal measured over the carotid artery (i.e. central pressure). This is consistent with the literature describing the physiological increase of Systolic Blood Pressure (SBP) and Pressure Pulse (PP) at increased distances from the heart (because of the presence of reflected waves). Moreover, the average measured displacements of the carotid artery are physiologically reliable (i.e. hundreds of micrometers). LDV seems to have the potential of correctly detecting the pressure waveform without contact. However, a comparison with a reference method is required to validate the proposed measurement technique.
Access provided by CONRICYT-eBooks. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Vital signs, such as Heart Rate (HR) and Blood Pressure (BP), are fundamental to determine the wellbeing of people. Several cardiovascular pathologies can be predicted by means of central BP assessment, which is considered an important predictive factor, even more than peripheral BP [1, 2]. Its continuous recording permits the assessment of fundamental parameters related to cardiac activity (e.g. HR) and to pulse waveform (e.g. dicrotic notch). Intra-arterial pressure catheters, containing miniature pressure transducers, represent the gold standard for the measurement of time-continuous pressure signal [3], but is uncomfortable and unsuitable for routine monitoring. Applanation tonometry is a contact non-invasive technique for the assessment of the local pressure waveform, but shows some relevant drawbacks [2]. In fact, there is a lack of studies validating the method versus invasive techniques in a general population, and for that the application of such transfer function is still subject to debate. Moreover, the application of arterial tonometry is particularly challenging in obese subjects. Other studies show alternative techniques to evaluate central BP non-invasively; in [2], intravascular magnetic resonance (MR) is used to assess blood pressure waveform. A 1.5 T [T] MR scanner has been used, just above the sino-tubular junction, to evaluate the aortic area curves. This technique allows to directly measure the variation of the vessel section during the cardiac cycle, but needs a calibration model to derive the pressure waveform from the aortic traversal area. Pulse-Wave-based Ultrasound Manometry (PWUM) is another non-invasive method that combines Pulse Wave Imaging (PWI) and vessel diameter measurements for the assessment of central BP [4]. It is based on the ultrasound scanning of the cross-section of the vessel, in order to measure its diameter variation during cardiac cycle. The use of LDV for the measurement of cardiovascular signals is datable at more of 10 years ago [5]. The first reason of the introduction of this technique has been the non-contact capability of LDV to measure the skin vibrations, in particular where it is really difficult the application of the electrodes (i.e. in burnt subjects or preterm neonates [6]). The acquisition of the carotid signal on the carotid artery with LDV provides a vibrocardiographic signal (VCG), consequent to mechanical cardiovascular events. Many studies have focused their attention to the extent of cardiovascular parameters from carotid artery [7,8,9,10,11,12,13]. In a previous work [14], the authors have made the hypothesis of using LDV to non-invasively assess the blood pressure waveform. The aim of this work is to discuss the feasibility of the application of a mathematic model to derive the arterial pressure signal, at carotid level, from the vibrational signal measured by means of a Laser Doppler Vibrometer.
2 Materials and Methods
LDV method was tested in a preliminary study on 6 healthy subjects. Participants was informed about the test and they filled a consent form to permit the study of their data.
2.1 Measurement Setup
VCG and electrocardiographic (ECG) signals were acquired simultaneously thanks to a proper A/D board (PowerLab 4/25T, 12-bit resolution). The VCG signals were measured with a single point LDV system (Polytec PDV100; calibration accuracy ±0.05 mm/s, bandwidth 0.05 Hz–22 kHz, spot diameter <1 mm, sensitivity 0.2 V/(mm/s)). The Polytec PDV100 utilizes Class 2 (eye safe) beam at 633 nm wavelength. The native output of the LDV system is a velocity signal.
Three 2-mins trials were made for each participant. Furthermore, a conventional oscillometric method was used to simultaneously assess BP at brachial level (P monitor model UA-767BT-Ci from A&D Instruments, accuracy: ±3 mm Hg).
Three measures of blood pressure was acquired for each trials and a mean of the diastolic and systolic values was considered.
During the trials, the participants were asked to lie supine and stay relaxed.
The vibrometer was placed on a tripod at a distance of 50 cm from the subject and it was pointed perpendicularly to the skin of the participant, over the left common carotid artery. A hydrating lotion (45% zinc oxide) was spread on the neck over the carotid site to improve the reflectivity of the skin and, consequently, the quality of the measurement (i.e. signal-to-noise ratio). In the present work, the carotid artery was located by a palpation method on the neck, identifying the point of maximum pulsation of the carotid artery.
A sketch of the measurement setup is represented in Fig. 1.
2.2 Signal Processing
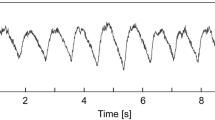
The signal processing consists of the steps reported in Fig. 2 and after described in detail.
-
Signal filtering: a 3rd order Butterworth bandpass filter was applied to raw data. 0.1–30 Hz and 0.1–40 Hz were the two frequency bands considered for VCG and ECG signals, respectively.
-
Signal integration: VCG (i.e. velocity signal) was integrated to obtain a displacement signal, which has to be calibrated to obtain absolute BP values. An operation of detrend was performed on the displacement signal to achieve a mean value equal to zero.
-
Computation of the average waveform: ECG signal was used to correctly separate the single heartbeat in VCG signal. This allowed to detect the onset and the offset of the single heart beats in the displacement signal. Then, each heartbeat was re-sampled according to the mean heart period detected from ECG signal.
-
Application of the calibration model: It was assumed that there is an exponential relationship between arterial pressure waveform and arterial cross-section [7]. Diastolic BP and Mean Arterial Pressure (MAP) values were supposed to remain fairly constant throughout the whole arterial tree. The systolic BP value extracted from the resulting pressure waveform was compared to the corresponding oscillometric BP value obtained from the brachial artery. The applied model relates the displacement d(t) achieved from LDV data to the arterial pressure waveform p(t), as described in (1) [15]:
where:
- \(\alpha = \frac{{A_{d} }}{{A\left( t \right) - A_{d} }}\,\ln \left( {\frac{SBP }{DBP}} \right)\) :
-
is a calibration parameter that quantifies the stiffness of the vessel;
- \(A\left( t \right) = \frac{{\pi d(t)^{2} }}{4}\) :
-
is the transversal cross circular section of the vessel;
- Ad :
-
is the diastolic value of the transversal section of carotid when pressure assumes its diastolic value.
3 Results
Table 1 shows the comparison between the systolic pressure measured by means of the oscillometric cuff at brachial level and the one obtained from the calibration of the VCG signal (i.e. the maximum peak of the calibrated pressure waveform).
Moreover, the displacement waveforms were discussed, in order to evaluate if the measured artery wall movements are consistent with the ones in literature. In Fig. 3, an example of displacement waveform is reported.
The mean values of the average displacement waveforms are the following ones (Table 2).
4 Discussion and Conclusions
In this preliminary study, the authors have been tested on six subjects the possibility of obtaining the pressure waveform from the integrated VCG signal, calibrated by means of brachial diastolic and mean blood pressure values measured via oscillometric method, using an exponential model [15].
The pressure values measured in the obtained waveforms have been compared with the ones measured at brachial level. The obtained systolic differences are comparable to the ones in literature (20%) [3] and express the physiological increase of systolic pressure (Fig. 4) from the central to peripheral sites.
Moreover, the average measured displacement shows values physiologically correct [3], that is of hundreds of micrometers [16].
The use of LDV to measure the displacement of carotid artery allows to observe the mechanical events related to hemodynamics with a very high sensitivity, but it involves the contribution of reflection phenomena, which may be not related to the investigated vessel.
A deeper investigation of the physiological dynamics is required in order to distinguish carotid features from the other mechanical events detected by LDV and to obtain a more accurate pressure waveform.
Moreover, the comparison with a reference method (i.e. arterial tonometry or intravascular catheter) is required to validate the described measurement method and processing algorithm.
References
J. Sharman, M. Stowasser, R. Fassett, T. Marwick, S. Franklin, Central blood pressure measurement may improve risk stratification. J. Hum. Hypertens. 22(12), 838–844 (2008)
M.A. Quail, J.A. Steeden, D. Knight, P. Segers, A.M. Taylor, V. Muthurangu, Development and validation of a novel method to derive central aortic systolic pressure from the MR aortic distension curve. J. Magn. Reson. Imaging JMRI 40(5), 1064–1070 (2014)
McDonald’s blood flow in arteries, in Theoretical, Experimental and Clinical Principles, 6th edn. (CRC Press, 29-July-2011) [Online]. Available: https://www.crcpress.com/McDonalds-Blood-Flow-in-Arteries-Sixth-Edition-Theoretical-Experimental/Nichols-ORourke-Vlachopoulos/9780340985014. Accessed 16 Apr 2016
J. Vappou, J. Luo, K. Okajima, M. Di Tullio, E.E. Konofagou, Non-invasive measurement of local pulse pressure by pulse wave-based ultrasound manometry (PWUM). Physiol. Meas. 32(10), 1653–1662 (2011)
M. Pinotti, N. Paone, F.A. Santos, E.P. Tomasini, Carotid Artery Pulse Wave Measured by a Laser Vibrometer, vol 3411 (1998), pp. 611–616
L. Scalise, N. Bernacchia, I. Ercoli, P. Marchionni, Heart rate measurement in neonatal patients using a webcamera, in 2012 IEEE International Symposium on Medical Measurements and Applications Proceedings (MeMeA), 2012, pp. 1–4
L. Scalise, U. Morbiducci, Non-contact cardiac monitoring from carotid artery using optical vibrocardiography. Med. Eng. Phys. 30(4), 490–497 (2008)
S. Casaccia, E.J. Sirevaag, E. Richter, J.A. O’Sullivan, L. Scalise, J.W. Rohrbaugh, Decoding carotid pressure waveforms recorded by laser Doppler vibrometry: effects of rebreathing, in AIP Conference Proceedings, vol 1600, 2014, pp. 298–312
P.H. Lai, J.A. O’Sullivan, M. Chen, E.J. Sirevaag, A.D. Kaplan, J.W. Rohrbaugh, A robust feature selection method for noncontact biometrics based on Laser Doppler Vibrometry, in Biometrics Symposium, 2008. BSYM ’08, 2008, pp. 65–70
M. Chen, J.A. O’Sullivan, N. Singla, E.J. Sirevaag, S.D. Kristjansson, P.H. Lai, A.D. Kaplan, J.W. Rohrbaugh, Laser Doppler vibrometry measures of physiological function: evaluation of biometric capabilities. IEEE Trans. Inf. Forensics Secur. 5(3), 449–460 (2010)
A. Campo, P. Segers, H. Heuten, I. Goovaerts, G. Ennekens, C. Vrints, R. Baets, J. Dirckx, Non-invasive technique for assessment of vascular wall stiffness using laser Doppler vibrometry. Meas. Sci. Technol. 25(6), 65701 (2014)
G. Cosoli, L. Casacanditella, E.P. Tomasini, L. Scalise, The non-contact measure of the heart rate variability by laser doppler vibrometry: comparison with electrocardiography. Meas. Sci. Tecnol. (in press)
E.J. Sirevaag, S. Casaccia, E.A. Richter, J.A. O’Sullivan, L. Scalise, J.W. Rohrbaugh, Cardiorespiratory interactions: noncontact assessment using laser Doppler vibrometry. Psychophysiology, p. n/a-n/a, Mar 2016
Non-contact assessment of blood pressure wave by means of vibrocardiography [Online]. Available: https://www.researchgate.net/publication/282867958_Non-contact_assessment_of_blood_pressure_wave_by_means_of_vibrocardiography. Accessed 15 June 2016
S.J. Vermeersch, E.R. Rietzschel, M.L. De Buyzere, D. De Bacquer, G. De Backer, L.M. Van Bortel, T.C. Gillebert, P.R. Verdonck, P. Segers, Determining carotid artery pressure from scaled diameter waveforms: comparison and validation of calibration techniques in 2026 subjects. Physiol. Meas. 29(11), 1267–1280 (2008)
C.L. Desjardins, L.T. Antonelli, E. Soares, A Remote and Non-contact Method for Obtaining the Blood-Pulse Waveform with a Laser Doppler Vibrometer, vol 6430 (2007), pp. 64301C–64301C–9
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG
About this paper
Cite this paper
Casacanditella, L., Cosoli, G., Casaccia, S., Scalise, L., Tomasini, E.P. (2018). Derived Non-contact Continuous Recording of Blood Pressure Pulse Waveform by Means of Vibrocardiography. In: Andò, B., Baldini, F., Di Natale, C., Marrazza, G., Siciliano, P. (eds) Sensors. CNS 2016. Lecture Notes in Electrical Engineering, vol 431. Springer, Cham. https://doi.org/10.1007/978-3-319-55077-0_46
Download citation
DOI: https://doi.org/10.1007/978-3-319-55077-0_46
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55076-3
Online ISBN: 978-3-319-55077-0
eBook Packages: EngineeringEngineering (R0)