Abstract
Liquid biopsy is a non-invasive diagnostic method that utilizes the detection and analysis of biomarkers in bodily fluids for the diagnosis and prognosis of various diseases. Exosomal microRNAs (miRNAs), which are remarkably stable because of the protection by extracellular vesicles (EVs), in liquid biopsy have gained considerable attention as they can regulate gene expression and serve as crucial biomarkers for the presence and progression of different types of cancer. Especially, urinary exosomal miRNAs have shown promising results as biomarkers for cancer from the urogenital system, such as bladder, renal tubular, and prostate. However, there are still significant challenges hindering the clinical utilization of urinary exosomal miRNA biomarkers, including improper sample handling, and data bias. Therefore, the detection procedure of urinary exosomal miRNAs needs to be standardized and thoroughly reviewed to ensure accurate and reliable clinical results. In this review, we have explored various detection procedures for urinary exosomal miRNAs, which have great potential as biomarkers for cancer diagnostics and prognostics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Liquid biopsy is a non-invasive diagnostic method that involves detecting and analyzing biomarkers, such as circulating tumor cells and DNA, in bodily fluids, like blood or urine, to diagnose a disease and determine its prognosis [1,2,3,4]. The use of non-invasive biomarkers is crucial for cancer diagnosis because it reduces the need for invasive diagnostic procedures, such as biopsies, which can be uncomfortable and carry risks of complications. Moreover, liquid biopsy allows for the analysis of tumor cells shed from multiple tumor sites, providing a more comprehensive and representative sampling of the heterogeneity of cancer compared to a single biopsy site. Additionally, non-invasive biomarkers enable frequent monitoring of cancer treatment effectiveness, with high accessibility for diagnosis and prognosis, enabling early detection of cancers and facilitating adjustment of treatment plans as required, thus providing personalized care to patients. Because of the benefits, liquid biopsies have been studied for decades in relation to various types of cancer [5,6,7,8,9] However, one of the challenges in liquid biopsy for cancer is finding reliable and non-invasive biomarkers that can indicate the presence and characteristics of cancer.
Extracellular vesicles (EVs) are small lipid bilayer membrane-bound nanoparticles that are secreted by various cells in varying sizes from 30 to 400 nm. EVs can be found in systemic circulation and bodily fluids and are involved in cell-to-cell communication [10,11,12,13,14,15]. As the effective transmit channel of information between cells, the contents of EVs accurately represent the intracellular composition of the cell where it originated from, including RNAs, DNAs, lipids, and proteins, which is inherent yet comprehensive information. These components make EVs a promising source of biomarkers, such as proteins and RNAs, for the diagnosis and prognosis of various diseases, including cancer (Fig. 1) [16,17,18,19,20].
Recent studies have suggested that exosomal miRNAs (miRNAs) are important biomarkers for the presence and progression of different types of cancer such as breast cancer, lung cancer, colorectal cancer, and prostate cancer [21,22,23,24]. miRNA is a small, single-stranded, noncoding RNA molecule that regulates gene expression at the post-transcription level by hybridizing to complementary sequences of target messenger RNA (mRNA) to inhibit translation. As such, miRNAs are involved in various biological processes such as cell differentiation, proliferation, cell suicide, and metabolism [25,26,27,28] In addition, since exosomal miRNAs, which are protected by exosomes, are remarkably stable in not only biological fluids, such as urine, but also harsh conditions, including the presence of enzymes, boiling, long-term storage at − 80 °C, and multiple freeze–thaw cycles [29,30,31,32].
Urine presents itself as an appealing source of extracellular vesicles (EVs) due to its advantageous properties as a biological fluid. EVs in urine originate from the urogenital system, including the renal tubular, bladder, and prostate. These specific origins of EVs can reflect the physiological and pathological conditions of these tissues and organs more precisely [33, 34] Also, unlike other bodily fluids such as blood or saliva, urine can be collected easily and without discomfort or any risk to the patient. This non-invasive nature of urine collection also reduces the cost of sample collection and processing. In addition, urine is usually sterile, which minimizes the risk of contamination during sample collection and handling [35]. Abundance is another advantage of urine that is produced daily in large volumes, providing enough EVs for analysis. The use of urine as an EV source for detecting exosomal miRNAs has the potential to improve patient outcomes through early diagnosis and personalized treatment strategies.
To summarize the above, urinary exosomal miRNAs have shown promise as potential biomarkers for cancer diagnosis and prognosis. As a result, they have been extensively studied in the diagnosis and prognosis of various types of cancer, including bladder, prostate, and renal cell cancers. Studies have shown that specific urinary exosomal miRNAs have altered expression levels in cancer patients compared to healthy individuals, indicating their potential use as diagnostic and prognostic biomarkers [36]. For instance, in bladder cancer, several studies have reported urinary exosomal miRNAs as a diagnostic and prognostic biomarker. Dozens of miRNAs, including miR-4295, miR-93-5p, miR-96-5p, miR-21-5p, and miR-155-5p were found to be significantly upregulated in urinary exosomal miRNAs, while dozens of other miRNAs, including miR-99a, and miR-125b were found to be down-regulated [36,37,38,39,40] Similarly, in prostate cancer patients, expression level of dozens of urinary exosomal miRNAs, including upregulation of miR-451a, miR-486, and miR-6090 and downregulation of miR-375 and miR-3665 have been identified as potential diagnostic biomarkers [41, 42] Additionally, researchers have found that upregulation of urinary exosomal miR-26a-5p, miR-532-5p, and miR-99b-3p can distinguish between biochemical recurrence (BCR) and non-BCR cases, demonstrating their utility for prognosis of prostate cancer [43]. In renal cell carcinoma, upregulation of miR-21-5p, and miR-30b-5p [44], and downregulation of urinary exosomal miR-30c-5p has been reported as a potential biomarker for diagnosis and prognosis, as it inhibits progression by targeting the depletion of HSPA5, which is reversing the promoting effect of the growth of clear cell renal cell carcinoma [45] It is important to note that most studies utilizing urinary exosomal miRNAs as cancer biomarkers have focused on bladder, prostate, and renal cells. This is because EVs in urine are primarily derived from the urogenital system, making urinary exosomal miRNAs more specific for detecting cancers of the urogenital system such as bladder, prostate, and renal cell cancers (Table 1) [46].
In summary, urinary exosomal miRNAs have shown great potential as non-invasive biomarkers for cancer diagnostics and prognostics. However, it is crucial to thoroughly review and standardize the detection procedure of urinary exosomal miRNAs to ensure accurate and reliable results for clinical use. In this review, we delve into the various detection procedure for urinary exosomal miRNAs, which show great potential as biomarkers for cancer diagnostics and prognostics.
2 Extraction of Exosomal miRNAs from Urine
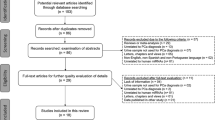
The extraction of exosomal miRNAs from urine is a critical step in the development of a reliable and non-invasive diagnostic and prognostic tool for cancer. The extraction of exosomal miRNAs from urine samples requires three steps: urine sample collection, isolation of EVs from urine, and extraction of miRNAs from EVs. Each step can affect the quality and quantity of exosomal miRNAs, affecting their detection and analysis, so the proper method should be carefully chosen (Fig. 2).
2.1 Urine Sample Collection
Midstream urine samples were collected using a non-invasive and convenient method. Participants were instructed to begin urinating, then collect the midstream urine after a few seconds. The samples were then pre-treated by centrifugation to eliminate the debris. The resulting supernatants were transferred to sterile cryovials and stored at − 80 °C until further analysis [47, 48].
2.2 Isolation of EVs from Urine
Several methods have been developed for EV isolation, including ultracentrifugation (UC), size exclusion chromatography (SEC), immunoaffinity capture, precipitation, and aqueous two-phase system (ATPS). Each of these EV isolation methods has its own advantages and disadvantages, and the choice of method depends on the accessibility and the desired level of purity and yield. It is important to carefully evaluate and compare different methods before selecting the most appropriate one for the study (Table 2).
UC is a widely used method for EV isolation and has been considered as a golden standard for EV purification, which involves multiple centrifugation steps at progressively higher speeds to pellet EVs. It can isolate pure EVs, however, it is time-consuming, and requires expensive equipment and technical expertise. Additionally, it can damage EVs during the centrifugation process, leading to a loss of functional EVs [49, 50].
SEC is another popular method for EV isolation, which separates EVs based on their size, shape, and density by passing the sample through a column of porous beads. It can also isolate pure EVs with good yield, and it is less likely to damage EVs than UC, however, it requires specialized, expensive, and disposable equipment. The inability to control the enrichment of EVs is also one of the limitations of the SEC [51,52,53] Some studies have attempted to address the issue of concentration by combining EV concentration such as ultrafiltration [54, 55] or super absorbent polymer [56].
Immunoaffinity is a method that uses EV-affinity materials such as antibodies to capture EVs based on specific surface markers. It can yield highly pure EVs that are specific to a particular antigen of interest. However, it is expensive and requires technical expertise. Also, the choice of antibodies affects the yield and purity of the isolated EVs [57, 58].
Precipitation is a relatively simple, fast, and cost-effective method for EV isolation that involves the addition of a precipitating agent such as polyethylene glycol (PEG) to the urine sample. It can isolate EVs with high yields. However, the precipitating agent can also co-precipitate other non-EV components, resulting in impure samples [59, 60].
ATPS is an alternative method for EV isolation that utilizes two phases of aqueous solutions with different polymers to separate EVs from other components in urine. It can isolate EVs with a high yield but requires careful optimization of the ATPS conditions, and residual polymers often hinder further downstream works [61, 62].
2.3 Extraction of miRNAs from EVs
To extract miRNAs from EVs, the first step is to lyse the EVs to release their contents. This can be achieved using various lysis buffers, such as TRIzol, NP-40, and Triton-X, which contain a detergent that effectively breaks down the lipid bilayer of the EVs. The choice of lysis buffer should be optimized to minimize RNA degradation and ensure high yield and purity [63,64,65].
Once the EVs are lysed, the miRNAs can be extracted from the lysate using column-based purification or phenol–chloroform extraction. Both methods are based on the principle of differential solubility of miRNAs in different solvents. In column-based purification, the lysate is applied to a column that selectively separates miRNAs from other biomolecules. The miRNAs can then be eluted from the column. This method uses a chaotropic salt solution to bind miRNAs to a silica membrane while washing away other biomolecules [66, 67]. In phenol–chloroform extraction, the lysate is mixed with phenol–chloroform, which separates the miRNAs into the aqueous phase while removing contaminants such as DNAs, proteins, and lipids. The separated miRNAs are then further purified suitable for downstream applications. This method uses an organic solvent to separate miRNAs into the aqueous phase while precipitating other biomolecules into the organic phase [68, 69].
3 The Detection Method of Urinary Exosomal miRNAs
Various methods have been used for the detection of urinary exosomal miRNAs, including microarray, quantitative real-time PCR (qPCR), and next-generation sequencing (NGS). Each of these methods has advantages and limitations that should be considered when selecting the appropriate protocol for a particular study (Fig. 3 and Table 3).
Schematics of the detection methods of urinary exosomal miRNAs. a Schematic draw of microarray. Fluorescent-labeled targets are detected by immobilized, complementary probes. Images reproduced with permission from [71]. b Schematic draw of RT-qPCR. To reverse-transcript short miRNAs, polyuridylation could be used. Images reproduced with permission from [85]. c Schematic draw of reverse transcription for RNA sequencing. The double ligation of the adapter can be used to reverse-transcript short miRNAs for sequencing. Images reproduced with permission from [94]. d Schematic draw of molecular beacon-based fluorescence imaging for detecting exosomal miRNAs. Images reproduced with permission from [107]
3.1 Microarray
Microarray technology has been used widely for urinary exosomal miRNA analysis for the past decades. To perform miRNA analysis using microarrays, extracted miRNAs are first labeled with a fluorescent dye and then hybridized into the immobilized, complementary probes. The fluorescent signals are then detected and analyzed to determine the relative abundance of each miRNA in the sample [70, 71] One of the main advantages of microarray technology is that it allows for the simultaneous analysis of hundreds or thousands of miRNAs in a single experiment. So, microarray for miRNA analysis can be designed not only to target specific sets of miRNAs, such as those involved in particular cancer but to be more comprehensive, for example, targeting all known miRNAs. It can also profile relative miRNA expression among multiple samples regardless of the different origins of miRNA or disease states in a single experiment [72]. However, microarrays have several limitations, including limited dynamic range, high background noise, and potential cross-hybridization between closely related miRNAs. These disadvantages lead to requiring a relatively large sample amount for analysis, which is a major drawback for urinary exosomal miRNAs where sample volumes are inherently low. Furthermore, the results obtained from microarrays are relative, meaning that the obtained data are expressed as fold-change values in differential groups (e.g., healthy vs cancer), and the absolute quantification is virtually limited [73, 74] Notwithstanding the aforementioned constraints, microarrays continue to be employed in diverse investigations aimed at scrutinizing urinary exosomal miRNAs. The primary rationale behind this lies in the ease of employment, the accessibility of equipment, the specialized skill set required, and the capacity to measure a vast array of miRNAs per assay. As a result of these elements, microarrays remain a viable alternative for screening purposes across a broad spectrum of research and potential biomarker candidates [75,76,77].
3.2 Reverse Transcription-Quantitative Polymerase Chain Reaction (RT-qPCR)
RT-qPCR is one of the most widely used detecting methods for the detection and quantification of urinary exosomal miRNAs in cancer diagnosis. It is a sensitive and specific method, allowing the quantification of miRNAs. It also can be used with various types of samples [78, 79]. To perform RT-qPCR, miRNA samples are first reverse transcribed into cDNA, which can then be used as a template for PCR amplification, and then cDNA amplification and quantification were performed by the procedure of qPCR. It is important to note that the target miRNAs and cDNAs have short sequences (~ 22 bases), which makes it challenging to amplify them with universal PCR primers (18–24 bases), and the miRNAs must be extended. To overcome the challenges, there are different methods to overcome by extending the target miRNAs, such as the use of specific stem-loop RT-primers [80,81,82] and polyuridylation or polyadenylation of miRNAs [83,84,85] The target miRNAs can be extended with the explicit RT-primers that is complementary to the miRNA sequence at 3’ ends, but extension forming a step-loop structure at 5’ ends. The target miRNAs also can be extended by polyadenylation or ligation of an adapter. These prior research efforts have enabled very sensitive and specific miRNA quantification analysis data. However, these methods also introduce limitations, such as limiting the number of measurable miRNAs per experiment, amplification biases, and additional primer design steps or enzymatic steps. Unlike the miRNA-specific RT step, the further qPCR step is performed similarly to a standard qPCR [86, 87]. In conclusion, RT-qPCR is a powerful tool for miRNA analysis in cancer diagnosis when the target miRNAs of interest are established, and the number is small. Despite the mentioned disadvantages above, it is a highly sensitive and specific method that can absolutely quantify miRNAs in clinical samples for cancer diagnosis and prognosis.
3.3 RNA Sequencing (RNA-seq)
RNA sequencing (RNA-seq) is high-throughput analyzing technique that can be used to identify and quantify RNA molecules in a biological sample, including urinary exosomal miRNAs for cancer diagnosis [88, 89] There are several methods for sequencing RNAs, including Sanger, and Illumina sequencing. Sanger sequencing, also known as chain-termination sequencing, is a classic technique for sequencing RNA. It involves synthesizing a complementary strand of DNA, and in vivo cloning and amplification. Amplified cDNAs are analyzed by adding different fluorescent-labeled dideoxynucleotides (ddNTPs) that terminate the chain at random positions and reading out using fluorescent detection the mixture of different-sized cDNA fragments, which can be separated by size on a gel. The cDNA fragments that differ in length can be separated by capillary electrophoresis and identified through different fluorescence [90]. While Sanger sequencing is highly accurate and was the first sequencing technique to be widely used, it is not commonly used for RNA-seq of late because of low throughput and high cost. The cost per base is higher than with next-generation sequencing (NGS), and Sanger sequencing is typically only used for small sequencing projects or for confirming the accuracy of NGS data [91, 92].
In contrast to sanger, new sequence technologies which are classified as next-generation sequencing (NGS) rapidly replaced the traditional sequencing method with higher throughput and lower costs. Illumina sequencing is the most common method for sequencing RNAs representing NGS. It dramatically decreased the time and cost of the sequencing by in vivo adaptor ligation, immobilization by hybridization, and polony array with repeated bridge amplification [93]. It involves the conversion of RNA to cDNA following double ligations of adapters to the 3’ and 5’ ends of the target miRNAs [94]. The resulting library is then PCR-amplified and then sequenced using Illumina’s sequencing-by-synthesis technology, which reads the DNA fragments in parallel using fluorescently labeled nucleotides [95]. This method ensures highly accurate and has a high throughput. However, during the ligation-based cDNA library preparation, the unwanted side products, such as adaptor dimers could introduce sequencing bias [96, 97]. To reduce the bias, the double ligation of the adapters with random nucleotides at the end or the single 3’ ligation followed by the circulation for cDNA synthesis could be employed [98, 99].
In summary, RNA-seq represents an effective analytical tool for assessing urinary exosomal miRNAs, as it enables a thorough and quantitative evaluation of the entire miRNA transcriptome in each sample, offering a more precise and sensitive cancer diagnosis. Moreover, it permits the quantification of multiple miRNAs in a single experimental setting, allowing for high-throughput analysis and the sequencing of millions of miRNAs in a solitary assay. Additionally, RNA-seq has the capacity to detect novel miRNAs without prior knowledge of their nucleotide sequence. However, it is important to note that RNA-seq does have limitations that need to be considered. Firstly, it requires substantial computational resources and bioinformatics expertise, which is costly. Secondly, it requires a relatively large amount of high-quality RNAs for successful analysis. Additionally, there is a potential for sequencing bias, particularly during the cDNA library preparation [100]. Despite these limitations, RNA-seq remains an advanced technology for studying urinary exosomal miRNAs, with the potential to contribute significantly to disease diagnosis and prognosis.
3.4 Other Methods
In addition to the existing miRNA detection technologies discussed earlier, there have been various approaches to analyze urinary exosomal miRNAs, including surface-enhanced Raman scattering (SERS), and fluorescence-based methods.
SERS method: SERS works by enhanced specific fingerprint peaks of absorbed on the surface of metal nanostructures. When laser is on a metal surface, the electromagnetic field around the metal is enhanced, leading to a dramatic increase in the Raman scattering signal from molecules adsorbed onto the metal surface. This enhancement signal allows for the detection of low concentrations of target exosomal miRNAs which were hybridized with the probes on a metallic surface [101, 102] SERS offers highly sensitive, specific analysis results, and can also provide information on the molecular structure of the analyte. However, the equipment and substrate fabrication for SERS is costly [103].
Fluorescence-based method: Fluorescence imaging works by selective visualization in the presence of target exosomal miRNAs. DNA probes, complementary to target miRNAs, which are anchored on various types of materials, including hydrogel [41, 104, 105] or molecular beacon [106, 107] could be used to selectively fluorescence-visualize the target miRNAs using hybridization. This method offers some advantages such as shorter analysis time, lower cost, and the absence of sequence bias. However, it is challenging to analyze a large number of miRNA targets simultaneously through a fluorescence-based method.
4 Perspective and Conclusion
As the urinary exosomal miRNAs are increasingly recognized as ideal biomarkers for early cancer diagnosis, prognosis prediction and clinical decision support, with numerous studies demonstrating their potential in cancer management, the well-established measurement of urinary exosomal miRNAs will play an important role in cancer management. However, there are still significant challenges hindering the clinical utilization of miRNA biomarkers, including inadequate experimental design, improper sample handling, high cost, and bias during data collection and analysis. Many of these problems stem from the lack of standardization. To address these issues, global efforts are underway to standardize procedures for the use of exosomal miRNA biomarkers in cancer diagnosis and prognosis. Moving forward, an improved understanding of the role of exosomal miRNAs in cancer development and progression is expected to lead to the discovery of new pathways for cancer treatment. Furthermore, with the anticipated advancements in technology and increased standardization, more accurate and reliable cancer diagnosis and prognosis will become possible.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Anfossi, S., Babayan, A., Pantel, K., Calin, G.A.: Clinical utility of circulating non-coding RNAs—an update. Nat. Rev. Clin. Oncol. 15, 541–563 (2018)
Kalluri, R., LeBleu, V.S.: The biology, function, and biomedical applications of exosomes. Science 367, eaau6977 (2020)
Pantel, K., Alix-Panabières, C.: Circulating tumour cells in cancer patients: challenges and perspectives. Trends Mol. Med. 16, 398–406 (2010)
Schwarzenbach, H., Hoon, D.S., Pantel, K.: Cell-free nucleic acids as biomarkers in cancer patients. Nat. Rev. Cancer 11, 426–437 (2011)
Hou, J.-M., et al.: Clinical significance and molecular characteristics of circulating tumor cells and circulating tumor microemboli in patients with small-cell lung cancer. J. Clin. Oncol. 30, 525–532 (2012)
Kim, D.-H., et al.: Real-time monitoring of biomarkers in serum for early diagnosis of target disease. BioChip J. 14, 2–17 (2020)
Krebs, M.G., et al.: Evaluation and prognostic significance of circulating tumor cells in patients with non–small-cell lung cancer. J. Clin. Oncol. 29, 1556–1563 (2011)
Paek, S.-H.: Real-time monitoring of biomarkers: current status and future perspectives. BioChip J. 14, 1–1 (2020)
Schwarzenbach, H., Pantel, K.: Circulating DNA as biomarker in breast cancer. Breast Cancer Res. 17, 1–9 (2015)
Théry, C., et al.: Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 7, 1535750 (2018)
Raposo, G., Stahl, P.D.: Extracellular vesicles: a new communication paradigm? Nat. Rev. Mol. Cell Biol. 20, 509–510 (2019)
Robbins, P.D., Morelli, A.E.: Regulation of immune responses by extracellular vesicles. Nat. Rev. Immunol. 14, 195–208 (2014)
Tkach, M., Théry, C.: Communication by extracellular vesicles: where we are and where we need to go. Cell 164, 1226–1232 (2016)
Van Niel, G., d’Angelo, G., Raposo, G.: Shedding light on the cell biology of extracellular vesicles. Nat. Rev. Mol. Cell Biol. 19, 213–228 (2018)
Yáñez-Mó, M., et al.: Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles 4, 27066 (2015)
Théry, C.: Diagnosis by extracellular vesicles. Nature 523, 161–162 (2015)
Jansen, F., Nickenig, G., Werner, N.: Extracellular vesicles in cardiovascular disease: potential applications in diagnosis, prognosis, and epidemiology. Circ. Res. 120, 1649–1657 (2017)
Revenfeld, A.L.S., et al.: Diagnostic and prognostic potential of extracellular vesicles in peripheral blood. Clin. Ther. 36, 830–846 (2014)
Verma, M., Lam, T.K., Hebert, E., Divi, R.L.: Extracellular vesicles: potential applications in cancer diagnosis, prognosis, and epidemiology. BMC Clin. Pathol. 15, 1–9 (2015)
Zhang, W., et al.: Extracellular vesicles in diagnosis and therapy of kidney diseases. Am. J. Physiol.-Renal Physiol. 311, F844–F851 (2016)
Hannafon, B.N., et al.: Plasma exosome microRNAs are indicative of breast cancer. Breast Cancer Res. 18, 1–14 (2016)
Hessvik, N.P., Sandvig, K., Llorente, A.: Exosomal miRNAs as biomarkers for prostate cancer. Front. Genet. 4, 36 (2013)
Ogata-Kawata, H., et al.: Circulating exosomal microRNAs as biomarkers of colon cancer. PLoS ONE 9, e92921 (2014)
Rabinowits, G., Gerçel-Taylor, C., Day, J.M., Taylor, D.D., Kloecker, G.H.: Exosomal microRNA: a diagnostic marker for lung cancer. Clin. Lung Cancer 10, 42–46 (2009)
Jackson, R.J., Standart, N.: How do microRNAs regulate gene expression? Sci. STKE (2007). https://doi.org/10.1126/stke.3672007re1
Rottiers, V., Näär, A.M.: MicroRNAs in metabolism and metabolic disorders. Nat. Rev. Mol. Cell. Biol. 13, 239–250 (2012)
Schratt, G.M., et al.: A brain-specific microRNA regulates dendritic spine development. Nature 439, 283–289 (2006)
Van Kouwenhove, M., Kedde, M., Agami, R.: MicroRNA regulation by RNA-binding proteins and its implications for cancer. Nat. Rev. Cancer 11, 644–656 (2011)
Kanno, S., Sakamoto, T., Fukuta, M., Kato, H., Aoki, Y.: Stability of exosomes in the postmortem serum and preliminary study on exosomal miRNA expression profiling in serum from myocardial infarction cadavers. Int. J. Legal Med. (2022). https://doi.org/10.1007/s00414-022-02913-y
Koga, Y., et al.: Exosome can prevent RNase from degrading microRNA in feces. J. Gastrointest. Oncol. 2, 215 (2011)
Sanz-Rubio, D., et al.: Stability of circulating exosomal miRNAs in healthy subjects. Sci. Rep. 8, 1–10 (2018)
Weber, J.A., et al.: The microRNA spectrum in 12 body fluids. Clin. Chem. 56, 1733–1741 (2010)
Gámez-Valero, A., Lozano-Ramos, S.I., Bancu, I., Lauzurica-Valdemoros, R., Borràs, F.E.: Urinary extracellular vesicles as source of biomarkers in kidney diseases. Front. Immunol. 6, 6 (2015)
Svenningsen, P., Sabaratnam, R., Jensen, B.L.: Urinary extracellular vesicles: Origin, role as intercellular messengers and biomarkers; efficient sorting and potential treatment options. Acta Physiol. 228, e13346 (2020)
Kass, E.H.: Pyelonephritis and bacteriuria. A major problem in preventive medicine. Ann. Intern. Med. 56, 46–53 (1962)
Yasui, T., et al.: Unveiling massive numbers of cancer-related urinary-microRNA candidates via nanowires. Sci. Adv. 3, e1701133 (2017)
Lin, H., et al.: Urinary Exosomal miRNAs as biomarkers of bladder Cancer and experimental verification of mechanism of miR-93-5p in bladder Cancer. BMC Cancer 21, 1–17 (2021)
El-Shal, A.S., et al.: Urinary exosomal microRNA-96-5p and microRNA-183-5p expression as potential biomarkers of bladder cancer. Mol. Biol. Rep. 48, 4361–4371 (2021)
Matsuzaki, K., et al.: MiR-21-5p in urinary extracellular vesicles is a novel biomarker of urothelial carcinoma. Oncotarget 8, 24668–24678 (2017)
Zhang, D.Z., et al.: Cell-free urinary microRNA-99a and microRNA-125b are diagnostic markers for the non-invasive screening of bladder cancer. PLoS ONE 9, e100793 (2014)
Kim, J., et al.: Hydrogel-based hybridization chain reaction (HCR) for detection of urinary exosomal miRNAs as a diagnostic tool of prostate cancer. Biosens. Bioelectron. 192, 113504 (2021)
Li, Z., et al.: Identification of urinary exosomal miRNAs for the non-invasive diagnosis of prostate cancer. Cancer Manag. Res. 13, 25–35 (2021)
Kim, M.Y., et al.: Urinary exosomal microRNA profiling in intermediate-risk prostate cancer. Sci. Rep. 11, 7355 (2021)
Zang, J., Maxwell, A.P., Simpson, D.A., McKay, G.J.: Differential expression of urinary exosomal microRNAs miR-21-5p and miR-30b-5p in individuals with diabetic kidney disease. Sci. Rep. 9, 1–10 (2019)
Song, S., et al.: Urinary exosome miR-30c-5p as a biomarker of clear cell renal cell carcinoma that inhibits progression by targeting HSPA5. J. Cell Mol. Med. 23, 6755–6765 (2019)
Junker, K., Heinzelmann, J., Beckham, C., Ochiya, T., Jenster, G.: Extracellular vesicles and their role in urologic malignancies. Eur. Urol. 70, 323–331 (2016)
Johnson, J.R., Stamm, W.E.: Diagnosis and treatment of acute urinary tract infections. Infect. Dis. Clin. North Am. 1, 773–791 (1987)
Lv, L.L., et al.: Isolation and quantification of microRNAs from urinary exosomes/microvesicles for biomarker discovery. Int. J. Biol. Sci. 9, 1021–1031 (2013)
Tomiyama, E., Fujita, K., Nonomura, N.: Urinary extracellular vesicles: ultracentrifugation method. Urinary Biomark. Methods Protoc. 2292, 173–181 (2021)
Théry, C., Amigorena, S., Raposo, G., Clayton, A.: Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr. Protoc. Cell Biol. 30, 3.22.21-23.22.29 (2006)
Böing, A.N., et al.: Single-step isolation of extracellular vesicles by size-exclusion chromatography. J. Extracell. Vesicles 3, 23430 (2014)
Lozano-Ramos, I., et al.: Size-exclusion chromatography-based enrichment of extracellular vesicles from urine samples. J. Extracell. Vesicles 4, 27369 (2015)
Lobb, R., Möller, A.: Size exclusion chromatography: a simple and reliable method for exosome purification. Extracell. Vesicles Methods Protoc. 1660, 105–110 (2017)
Vergauwen, G., et al.: Confounding factors of ultrafiltration and protein analysis in extracellular vesicle research. Sci. Rep. 7, 1–12 (2017)
Liga, A., Vliegenthart, A., Oosthuyzen, W., Dear, J., Kersaudy-Kerhoas, M.: Exosome isolation: a microfluidic road-map. Lab Chip 15, 2388–2394 (2015)
Yang, H.C., Ham, Y.M., Kim, J.A., Rhee, W.J.: Single-step equipment-free extracellular vesicle concentration using super absorbent polymer beads. J. Extracell. Vesicles 10, e12074 (2021)
Wiklander, O.P., et al.: Systematic methodological evaluation of a multiplex bead-based flow cytometry assay for detection of extracellular vesicle surface signatures. Front Immunol. 9, 1326 (2018)
Koliha, N., et al.: A novel multiplex bead-based platform highlights the diversity of extracellular vesicles. J. Extracell. Vesicles 5, 29975 (2016)
Royo, F., et al.: Different EV enrichment methods suitable for clinical settings yield different subpopulations of urinary extracellular vesicles from human samples. J. Extracell. Vesicles 5, 29497 (2016)
Lobb, R.J., et al.: Optimized exosome isolation protocol for cell culture supernatant and human plasma. J. Extracell. Vesicles 4, 27031 (2015)
Han, B.H., et al.: Isolation of extracellular vesicles from small volumes of plasma using a microfluidic aqueous two-phase system. Lab Chip 20, 3552–3559 (2020)
Shin, H., Park, Y.H., Kim, Y.-G., Lee, J.Y., Park, J.: Aqueous two-phase system to isolate extracellular vesicles from urine for prostate cancer diagnosis. PLoS ONE 13, e0194818 (2018)
Pisitkun, T., Shen, R.-F., Knepper, M.A.: Identification and proteomic profiling of exosomes in human urine. Proc. Natl. Acad. Sci. 101, 13368–13373 (2004)
Kumeda, N., et al.: Characterization of membrane integrity and morphological stability of human salivary exosomes. Biol. Pharm. Bull. 40, 1183–1191 (2017)
Taylor, D.D., Zacharias, W., Gercel-Taylor, C.: Exosome isolation for proteomic analyses and RNA profiling. Serum/Plasma Proteomics: Methods Protoc. 728, 235–246 (2011)
Channavajjhala, S.K., et al.: Optimizing the purification and analysis of miRNAs from urinary exosomes. Clin. Chem. Lab. Med. (CCLM) 52, 345–354 (2014)
Cheng, L., Sun, X., Scicluna, B.J., Coleman, B.M., Hill, A.F.: Characterization and deep sequencing analysis of exosomal and non-exosomal miRNA in human urine. Kidney Int. 86, 433–444 (2014)
Chen, T., et al.: Increased urinary exosomal microRNAs in children with idiopathic nephrotic syndrome. EBioMedicine 39, 552–561 (2019)
El-Khoury, V., Pierson, S., Kaoma, T., Bernardin, F., Berchem, G.: Assessing cellular and circulating miRNA recovery: the impact of the RNA isolation method and the quantity of input material. Sci Rep 6, 19529 (2016)
Liu, C.-G., et al.: An oligonucleotide microchip for genome-wide microRNA profiling in human and mouse tissues. Proc. Natl. Acad. Sci. 101, 9740–9744 (2004)
Siddika, T., Heinemann, I.U.: Bringing MicroRNAs to light: methods for MicroRNA quantification and visualization in live cells. Front. Bioeng. Biotechnol. 8, 619583 (2021)
Love, C., Dave, S.: MicroRNA expression profiling using microarrays. Hematological Malignancies 999, 285–296 (2013)
Li, W., Ruan, K.: MicroRNA detection by microarray. Anal. Bioanal. Chem. 394, 1117–1124 (2009)
Ono, S., Lam, S., Nagahara, M., Hoon, D.S.: Circulating microRNA biomarkers as liquid biopsy for cancer patients: pros and cons of current assays. J. Clin. Med. 4, 1890–1907 (2015)
Zhao, Y., et al.: Urinary exosomal MiRNA-4534 as a novel diagnostic biomarker for diabetic kidney disease. Front Endocrinol. (Lausanne) 11, 590 (2020)
Ball, C.A., et al.: Standards for microarray data. Science 298, 539–539 (2002)
Chen, J.J., Hsueh, H.-M., Delongchamp, R.R., Lin, C.-J., Tsai, C.-A.: Reproducibility of microarray data: a further analysis of microarray quality control (MAQC) data. BMC Bioinform. 8, 1–14 (2007)
Kubista, M., et al.: The real-time polymerase chain reaction. Mol. Aspects Med. 27, 95–125 (2006)
Chugh, P., Dittmer, D.P.: Potential pitfalls in microRNA profiling. Wiley Interdiscip. Rev. RNA 3, 601–616 (2012)
Chen, C., et al.: Real-time quantification of microRNAs by stem–loop RT–PCR. Nucleic Acids Res. 33, e179–e179 (2005)
Androvic, P., Valihrach, L., Elling, J., Sjoback, R., Kubista, M.: Two-tailed RT-qPCR: a novel method for highly accurate miRNA quantification. Nucleic Acids Res. 45, e144–e144 (2017)
Raymond, C.K., Roberts, B.S., Garrett-Engele, P., Lim, L.P., Johnson, J.M.: Simple, quantitative primer-extension PCR assay for direct monitoring of microRNAs and short-interfering RNAs. RNA 11, 1737–1744 (2005)
Balcells, I., Cirera, S., Busk, P.K.: Specific and sensitive quantitative RT-PCR of miRNAs with DNA primers. BMC Biotechnol. 11, 1–11 (2011)
Shi, R., Chiang, V.L.: Facile means for quantifying microRNA expression by real-time PCR. Biotechniques 39, 519–525 (2005)
Mei, Q., et al.: A facile and specific assay for quantifying microRNA by an optimized RT-qPCR approach. PLoS ONE (2012). https://doi.org/10.1371/journal.pone.0046890
Kramer, M.F.: Stem-loop RT-qPCR for miRNAs. Curr. Protoc. Mol. Biol. 95, 15.10.11-15.10.15 (2011)
Mestdagh, P., et al.: A novel and universal method for microRNA RT-qPCR data normalization. Genome Biol. 10, 1–10 (2009)
Dai, D., Tan, Y., Guo, L., Tang, A., Zhao, Y.: Identification of exosomal miRNA biomarkers for diagnosis of papillary thyroid cancer by small RNA sequencing. Eur. J. Endocrinol. 182, 111–121 (2020)
Hunt, E.A., Broyles, D., Head, T., Deo, S.K.: MicroRNA detection: current technology and research strategies. Annu. Rev. Anal. Chem. 8, 217–237 (2015)
Sanger, F., Nicklen, S., Coulson, A.R.: DNA sequencing with chain-terminating inhibitors. Proc. Natl. Acad. Sci. 74, 5463–5467 (1977)
Behjati, S., Tarpey, P.S.: What is next generation sequencing? Archives Dis. Child. Educ. Practice 98, 236–238 (2013)
Sikkema-Raddatz, B., et al.: Targeted next-generation sequencing can replace Sanger sequencing in clinical diagnostics. Hum. Mutat. 34, 1035–1042 (2013)
Shendure, J., Ji, H.: Next-generation DNA sequencing. Nat. Biotechnol. 26, 1135–1145 (2008)
Benesova, S., Kubista, M., Valihrach, L.: Small RNA-sequencing: approaches and considerations for miRNA analysis. Diagnostics 11, 964 (2021)
Bentley, D.R., et al.: Accurate whole human genome sequencing using reversible terminator chemistry. Nature 456, 53–59 (2008)
Ludwig, N., et al.: Bias in recent miRBase annotations potentially associated with RNA quality issues. Sci. Rep. 7, 1–11 (2017)
Pritchard, C.C., Cheng, H.H., Tewari, M.: MicroRNA profiling: approaches and considerations. Nat. Rev. Genet. 13, 358–369 (2012)
Barberán-Soler, S., et al.: Decreasing miRNA sequencing bias using a single adapter and circularization approach. Genome Biol. 19, 1–9 (2018)
Hafner, M., et al.: Identification of microRNAs and other small regulatory RNAs using cDNA library sequencing. Methods 44, 3–12 (2008)
Conesa, A., et al.: A survey of best practices for RNA-seq data analysis. Genome Biol. 17, 1–19 (2016)
Song, S., Lee, J.U., Jeon, M.J., Kim, S., Sim, S.J.: Detection of multiplex exosomal miRNAs for clinically accurate diagnosis of Alzheimer’s disease using label-free plasmonic biosensor based on DNA-Assembled advanced plasmonic architecture. Biosens. Bioelectron. 199, 113864 (2022)
Lee, J.U., Kim, S., Sim, S.J.: SERS-based nanoplasmonic exosome analysis: enabling liquid biopsy for cancer diagnosis and monitoring progression. BioChip J. 14, 231–241 (2020)
Pang, S., Yang, T., He, L.: Review of surface enhanced Raman spectroscopic (SERS) detection of synthetic chemical pesticides. TrAC Trends Anal. Chem. 85, 73–82 (2016)
Roh, Y.H., Sim, S.J., Cho, I.-J., Choi, N., Bong, K.W.: Vertically encoded tetragonal hydrogel microparticles for multiplexed detection of miRNAs associated with Alzheimer’s disease. Analyst 141, 4578–4586 (2016)
Choi, W., et al.: Hydrogel micropost-based qPCR for multiplex detection of miRNAs associated with Alzheimer’s disease. Biosens. Bioelectron. 101, 235–244 (2018)
Lee, J.H., Kim, J.A., Kwon, M.H., Kang, J.Y., Rhee, W.J.: In situ single step detection of exosome microRNA using molecular beacon. Biomaterials 54, 116–125 (2015)
Yang, H.C., Rhee, W.J.: Single step in situ detection of surface protein and microRNA in clustered extracellular vesicles using flow cytometry. J. Clin. Med. 10, 319 (2021)
Acknowledgements
This journal was supported by the Ministry of Science and ICT through the National Research Foundation of Korea (NRF): NRF-2020M3A9D8039920, NRF-2021M3H4A4079294, NRF-2022M3A9B6082678, NRF-2016R1A5A1010148 (the Engineering Research Center of Excellence Program). We also acknowledge support jointly from the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health and Welfare, and the Ministry of Food and Drug Safety: KMDF_PR_20200901_0072 (the Korea Medical Device Development Fund). We acknowledge support from the KIST institutional project (2E31502) and the KU-KIST Graduate School of Converging Science and Technology Program. This research was also supported by the Technology Innovation Program (20018111, Development of super-fast multiplex technology for the examination of diagnosis of infectious disease and in-body response test) funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, J., Kim, M., Kang, J.Y. et al. The Detection of Urinary Exosomal miRNAs for Cancer Diagnostics and Prognostics. BioChip J 17, 308–317 (2023). https://doi.org/10.1007/s13206-023-00108-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13206-023-00108-0