Abstract
Pneumocytoma is a rare benign neoplasm which was described over 50 years ago. Over the years its nomenclature and histogenesis has been a subject of much debate and controversy. We would like to report a case of a lady who presented with complaints of cough and hemoptysis. X-ray chest and computerized tomography (CT) scan showed a solitary pulmonary nodule. Biopsy was inconclusive. She underwent a left lower lobectomy. Her postoperative period was uneventful. Her final diagnosis was of pneumocytoma. She is on regular follow-up and is asymptomatic at present.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pneumocytoma is a rare benign neoplasm which was described over 50 years ago. Over the years, its nomenclature and histogenesis has been a subject of much debate and controversy and still continues to be so. We present a case of a 67-year-old lady who was suspected to have carcinoma lung and underwent left lower lobectomy and on final histopathology was diagnosed as pneumocytoma.
Case Report
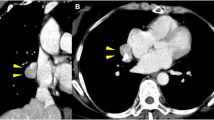
A sixty-seven-year-old lady presented with complaints of cough and hemoptysis since 2 months. She underwent an X-ray chest which showed a cannonball lesion in the lower lobe of the left lung. CT scan showed a solitary pulmonary nodule of size 4.3 × 3.6 × 3.6 cm in the anterobasal segment of the left lower lobe [Fig. 1]. Spotty calcifications were present. No lymph nodal metastasis was present. FNAC done in the peripheral hospital was suspicious of adenocarcinoma. However, slide review at our institute was inconclusive. A trucut biopsy done at our center showed only atypical cells. A working diagnosis of carcinoma lung was made. Her metastatic workup was negative. She underwent a left lower lobectomy with mediastinal lymph node sampling [Fig. 2]. Her postoperative period was uneventful. Her final histopathological diagnosis was of pneumocytoma. On microscopy, there were papillary and solid sheets of cuboidal and stromal cells [Fig. 3]. On immunohistochemistry (IHC), the cells were epithelial membrane antigen (EMA) and thyroid transcription factor-1 (TTF-1) positive [Fig. 4]. The MIB 1 index was very low. All the nodes were negative for malignancy. She has completed one and a half years of regular follow-up and is currently asymptomatic.
Discussion
Pneumocytoma is a benign lung neoplasm, first described in 1956 by Liebow and Hubbel [1]. They considered this tumor to be of vascular (endothelial) origin due to prominent angiomatoid features and coined the term sclerosing hemangioma. However, now, these tumors are not considered to be of vascular origin as they are immunonegative for CD34, CD31, factor VIII, and Ulex europaeus agglutinin [2]. Due to disputed histogenesis, it has received several names throughout history, including sclerosing hemangioma of the lung, benign pulmonary histiocytoma, and xanthomatous pseudotumor [1]. Currently, ultrastructural study and immunohistochemical techniques suggest that this is an epithelial tumor with differentiation to type II pneumocytes, hence the name pneumocytoma. The first to coin the term pneumocytoma were Tanaka et al. in 1986 [2]. Pneumocytoma, is predominant in 50-year olds, with a female to male ratio of 5:1 in this patient group [3]. It is mainly found incidentally; over 70% of the patients are asymptomatic. If present, the common symptoms include hemoptysis, chronic cough, and chest pain. On chest radiographs, Pneumocytoma typically presents as a peripheral, solitary, well-defined, homogeneous nodule or mass without predilection for a particular lobe [4]. Computed tomography of the chest demonstrates a round to oval nodule or mass with smooth margins that enhances following injection of intravenous contrast agents [5]. It demonstrates low to moderate uptake on FDG PET imaging; however, false positive results may also be present [6]. It is now generally accepted that pneumocytoma of the lung is a benign lesion and surgical excision alone is curative [7]. Surgery consists of either lobectomy or wedge resection. Complete surgical resection with preservation of normal pulmonary tissue should be done. It is histologically characterized by the presence of hemorrhagic, papillary, solid, or sclerotic areas. Most tumors show at least three of these histological characteristics. It is mainly composed of two types of cells: eosinophilic cuboidal surface cells that tend to differentiate into type II pneumocytes, and polygonal or round stromal cells that have considerable multilineage differentiation potential [8]. Niho et al., based on an X-chromosome-linked polymorphic marker, human androgen receptor, concluded that pneumocytoma is a neoplastic lesion and both the cells of the tumor have a common origin, i.e., they are monoclonal [9]. However, Wang et al. concluded that stromal cells are true tumor cells originating from the primitive respiratory epithelium while surface epithelial cells originate from the reactive proliferation of type II pneumocytes [10].
Thus, due to conflicting results, further studies are required to confirm whether these two cell types are monoclonal or not. On immunohistochemical study, both the lining cells and round cells show a positive reaction to EMA and TTF-1. However, surface cells are usually positive for pancytokeratin (CK) while round cells are usually negative for the same [10]. The expression of TTF-1 in the absence of surfactant proteins A and B and Clara cell antigens in the stromal cells suggests that they are derived from primitive respiratory epithelium. The surface alveolar pneumocytes may either represent phenotypic differentiation of a primitive respiratory epithelial component or they may correspond to non-neoplastic entrapped or hyperplastic elements [11].
This immunoprofile helps in differentiation from bronchogenic adenocarcinoma showing papillary pattern in which the tumor cells in both the solid areas and the surface of the papillae share similar immunoprofile (EMA+ CK+ TTF-1+). Though it is rarely malignant, IHC study can help differentiate it from adenocarcinoma of the lung. Pneumocytoma may rarely metastasize, especially to mediastinal or hilar lymph nodes [12]. Unusual cases of extralobar pneumocytoma have been reported. There were three hypotheses to explain these findings [8]; first one was that the extrapulmonary lesions, such as mediastinal masses, were metastatic foci of the primary pulmonary lesions. Second, tumors might derive from the ectopic lung tissues. Third, the lesion developed as a pedunculated pleural mass from the lung and moved towards the lung surface or mediastinum. Surgery is the treatment for all these lesions and there is no role for any adjuvant therapy. The prognosis of these patients is good and local and systemic recurrence is rare.
References
Liebow AA, Hubbel DS (1956) Sclerosing hemangioma (histiocytoma, xanthoma) of the lung. Cancer 9:53–75
Tanaka I, Inoue M, Matsui Y, Oritsu S, Akiyama O, Takemura T et al (1986) A case of pneumocytoma (so called sclerosing hemangioma) with lymph node metastasis. Jpn J Clin Oncol 16:77–86
Kuo KT, Hsu WH, Wu YC, Huang MH, Li WY (2003) Sclerosing hemangioma of the lung: an analysis of 44cases. J Chin Med Assoc 66:33–38
Haaga J, Lanzier CF, Gilkeson RC (2003) CT and MR imaging of the whole body. 1 vol. 4th ed. Mosby, St. Louis, Missouri
Cheung YC, Ng SH, Chang JW, Tan CF, Huang SF, Yu CT (2003) Histopathological and CT features of pulmonary sclerosing haemangiomas. Clin Radiol 58:630–635
Lin KH, Chang CP, Liu RS, Wang SJ (2011) F-18 FDG PET/CT in evaluation of pulmonary sclerosing hemangioma. Clin Nucl Med 36:341–343
Feng FY, Cheng GY, Gao SG, Liu XY, Mao YS, Tan FW et al (2012) Diagnosis and surgical treatment of pulmonary sclerosing hemangioma. Zhonghua Yi Xue Za Zhi 92(17):1190–1193
Wang Y, Dai S, Wang E. Differential gene expressions of polygonal cells and cuboidal cells in so-called pulmonary sclerosing hemangioma. Zhongguo Fei Ai Za Zhi 2007;10:466–470.
Niho S, Suzuki K, Yokose T, Kodama T, Nishiwaki Y, Esumi H (1998) Monoclonality of both pale cells and cuboidal cells of sclerosing hemangioma of the lung. Am J Pathol 152(4):1065–1069
Wang E, Lin D, Wang Y, Wu G, Yuan X (2004) Immunohistochemical and ultrastructure markers suggest different origins for cuboidal and polygonal cells in pulmonary sclerosing hemangioma. Hum Pathol 35:503–508
Devouassoux-Shisheboran M, Hayashi T, Linnoila R, Koss MN, Travis WD (2000l) A clinicopathologic study of 100 cases of pulmonary sclerosing hemangioma with immunohistochemical studies: TTF-1 is expressed in both round and surface cells, suggesting an origin from primitive respiratory epithelium. Am J Surg Pathol 24(7):906–916
Chien NC, Lin CW, Tzeng JE (2009) Sclerosing haemangioma with lymph node metastasis. Respirology 14:614–616
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhargavan, R., Chandramohan, K., Mathew, A.P. et al. Pneumocytoma: a Case Report and Review of Literature. Indian J Surg Oncol 8, 423–425 (2017). https://doi.org/10.1007/s13193-017-0652-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-017-0652-3