Abstract
Pulmonary sclerosing pneumocytoma (PSP) arising from the hilar lesion is extremely rare. We report an asymptomatic 70-year-old female with a thoracic tumor of unknown origin. Contrast-enhanced chest tomography showed a poorly and heterogeneously enhanced 40-mm tumor compressing the left upper lobe, bronchus, and pulmonary arteries. Positron-emission tomography did not detect abnormal integration in the tumor. Surgical resection was planned to confirm diagnosis and avoid further compression on the structures. Intraoperative findings revealed a dark red-colored tumor, projecting from the left upper lobe in the hilar lesion. Left upper lobectomy was performed through video-assisted thoracoscopic surgery to achieve complete resection and avoid contact bleeding. Immunohistochemical examination revealed the presence of PSP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Pulmonary sclerosing pneumocytoma (PSP) is an uncommon benign tumor [1]. We present a rare case of PSP projecting from left upper lobe in the hilar lesion.
Case
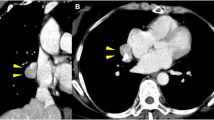
A 70-year-old asymptomatic female was referred to our hospital in 20xx for surgical treatment of a left thoracic tumor, which was accidentally detected through chest computed tomography (CT) in 20xx-1 and followed up annually. In the retrospective evaluation, chest X-rays revealed the tumor was less progressive (Fig. 1a). Contrast-enhanced CT showed weak staining on the periphery and heterogeneous enhancement inside the tumor compressing the anterior segmental artery of the left upper lobe (Fig. 1b). The localization of the tumor was well visually recognized through three-dimensional CT (Fig. 1c). Magnetic resonance imaging could not confirm the tumor origin (not shown). Fluorodeoxyglucose positron-emission tomography (FDG/PET) (Fig. 1d) did not detect abnormal integration in the tumor. Surgical resection was planned to avoid further compression and confirm the pathological diagnosis.
Preoperative imaging examinations. a Chest X-ray revealed the presence of a less progressive tumor (arrows). b Contrast-enhanced computed tomography (CT) performed in 20XX showed the solid 40-mm tumor between the heart and the left upper lobe, pressing the anterior segmental pulmonary artery (PA) of the upper lobe. c Three-dimensional CT showed that the tumor was adjacent to the lingular and anterior segmental bronchus of the left upper lobe and compressed these structures. d Positron-emission tomography did not detect abnormal integration in the tumor
Thoracoscopic examination revealed the presence of a dark red-colored subpleural tumor projecting mainly from the lingular segment in the hilar lesion (Fig. 2a, b). We performed left upper lobectomy with lymph-node dissection through video-assisted thoracoscopic surgery without intraoperative biopsy to achieve complete resection and avoid contact bleeding. The patient was discharged 4 days after surgery without complications.
Intraoperative thoracoscopic view (a, b) and macroscopic image of the section (b). a A dark red subpleural tumor, projecting mainly from the lingular segment, did not invade the surrounding areas outside the lung. b Dissecting mediastinal pleura could separate the tumor from the mediastinum. c The tumor was well circumscribed, partially lobulated, and filled with hemoid contents
Gross inspection of the surface revealed that the tumor was covered with visceral pleura and well circumscribed, partially lobulated, and filled with hemoid contents (Fig. 2c). Microscopically, the solid lesion was mostly composed of surface cells and spaces were filled with coagula. Immunohistochemical examination demonstrated positive staining for cytokeratin and thyroid transcription factor-1, and negative staining for CD31 and CD34 (Fig. 3). The Ki-67 labeling index was less than 1% and the atypia of the cells was not seen. These findings revealed the presence of PSP.
Histopathological examinations. Hematoxylin and eosin (HE) staining showed the hemorrhagic pattern, composed of large blood-filled spaces. The cells lining the surface of the spaces were positive for the pneumocyte markers (Keratin and TTF-1) and negative for the vascular endothelial markers (CD31 and CD34). The endothelial cells in the intrinsic capillary blood vessels were positive for both CD31 and CD34. Scale bars for the low-power field (LPF) and the high-power field (LPF) were 200 µm and 50 µm, respectively. Keratin; pan-cytokeratin. TTF-1; thyroid transcription factor-1
Discussion
PSP is an uncommon benign tumor, occurring predominantly in middle-aged females in East Asia [2,3,4]. PSP accounts for 5.8% of surgically resected benign tumors in Japan [1]. Hung et al. reported a rare case of PSP arising from the right hilar lesion [5], but intraoperative image was not presented. Considering the localization and vascular-rich appearance of PSP in our case, careful surgical procedure was required to avoid contact bleeding.
Although various imaging findings obtained through CT [2], FDG/PET [2], and MRI [3, 4] have been reported, it is difficult to diagnose PSP preoperatively because of its less specific features.
Histologically, PSP is characterized by a distinct pattern of two types of epithelial cells (i.e., surface cells and round cells). These types of cells form four architectural patterns, namely papillary, sclerotic, solid, and hemorrhagic [6]. In the present case, the hemorrhagic pattern occupied a large part of the tumor; thus, the presence of cavernous hemangioma was suspected. However, the cells lining the spaces were positive for cytokeratin and TTF-1 (indicating pneumocyte differentiation) and negative for CD31 and CD34 (indicating vascular endothelial differentiation) [6]. These immunohistochemical examinations are crucial for the diagnosis of PSP.
Conclusion
We reported a rare case of PSP projecting from left upper lobe in the hilar lesion. Left upper lobectomy was required to achieve complete resection and avoid contact bleeding. Immunohistochemical examination is essential for the diagnosis of PSP.
References
Masuda M, Endo S, Natsugoe S, Shimizu H, Doki Y, Hirata Y, et al. Thoracic and cardiovascular surgery in Japan during 2015. Gen Thorac Cardiovasc Surg. 2018. https://doi.org/10.1007/s11748-018-0968-0.
Shin SY, Kim MY, Oh SY, Lee HJ, Hong SA, Jang SJ, et al. Pulmonary sclerosing pneumocytoma of the lung: CT characteristics in a large series of a tertiary referral center. Medicine. 2015;94:1–10.
Kim YP, Lee S, Park HS, Park CH, Kim TH. Sclerosing pneumocytoma with a wax-and-wane pattern of growth: a case report on computed tomography and magnetic resonance imaging findings and a literature review. Korean J Radiol. 2015;16:947–50.
Fujiyoshi F, Ichinari N, Fukukura Y, Sasaki M, Hiraki Y, Nakajo M. Sclerosing hemangioma of the lung: MR findings and correlation with pathological features. J Comput Assist Tomogr. 1998;22:1006–8.
Hung JH, Hsueh C, Liao CY, Ho SY, Huang YC. Pulmonary hilar tumor: an unusual presentation of sclerosing hemangioma. Case Rep Med. 2016. https://doi.org/10.1155/2016/8919012.
Keylock JB, Galvin JR, Franks TJ. Sclerosing hemangioma of the lung. Arch Pathol Lab Med. 2009;133(5):820–5. https://doi.org/10.1043/1543-2165-133.5.820.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that all authors have no commercial associations that might pose a conflict of interest in connection with the submitted article, especially regarding any materials referred to in this report. No funding for this study was received from any sponsors.
Informed consent
Written informed consent was obtained from the patient for the publication of this report.
Rights and permissions
About this article
Cite this article
Ikeda, M., Okada, Y., Hagiwara, K. et al. A case of pulmonary sclerosing pneumocytoma in the hilar lesion. Gen Thorac Cardiovasc Surg 67, 818–820 (2019). https://doi.org/10.1007/s11748-018-1043-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-018-1043-6