Abstract
The primary objective of this study was to determine whether sphincter preservation is possible among patients who develop anastomotic leakage after rectal cancer surgery. The secondary objective was to determine the factors that may contribute to anastomotic leakage. This is a retrospective review of a prospectively maintained database. All patients with rectal cancer who underwent restorative proctectomy over 1 year were included in the study. The parameters analyzed were age, preoperative hemoglobin and albumin, neoadjuvant therapy, type of surgery, level of ligation of inferior mesenteric pedicle, technique of anastomosis, and defunctioning proximal stoma. In this study, 176 cases of anterior resection were included,of which15 (8.5 %) had anastomotic leakage. None of the factors contributing to anastomotic leakage reached statistical significance on univariate analysis. Among the patients who had proximal defunctioning ileostomy (n = 9), five (56 %) required re-surgery whereas other four were managed with antibiotics and presacral drainage alone (44 %). Among the patients who didnot have proximal defunctioning ileostomy (n = 6), all (100 %) required re-surgery. Among the 12 eligible patients, stoma reversal was successful in eight (67 %) patients. This study highlights the importance of defunctioning proximal stoma in reducing the incidence and severity of anastomotic leakage as well as the need and extent of re-surgery for low rectal cancer. Sphincter preservation is possible in majority of patients who develop anastomotic leakage after rectal cancer surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of rectal cancer in India is on the rise, with an estimated age-standardized rate between 4.1–5.8 and 3.5–5.3 per 100,000 in males and in females, respectively [1]. Radical surgery with total or partial tumor-specific mesorectal excision remains the mainstay of treatment. Advances in the rectal cancer management in the form of neoadjuvant chemoradiotherapy, staging with magnetic resonance imaging (MRI), availability of staplers, and improvement in perioperative care have lead to improved oncological outcomes.
Development of the anastomotic leakage is the most feared complication after rectal cancer surgery with incidence in the published literature ranging from 1.8 to 19.8 % [2, 3]. Anastomotic leakage leads to significant morbidity to the patient with impact on oncological, clinical, and functional outcomes. It has been associated with a risk of perioperative mortality rate ranging from 6.12 to 10 % [4, 5]. In addition, it leads to prolonged hospital stay, need for systemic antibiotics, reintervention, and increased overall cost. Oncologically, those who develop anastomotic leakage, particularly those who require reintervention, have been found to have higher incidence of local recurrence and inferior overall survival [6, 7]. Functionally, it has been observed that anastomotic leakage carries high probability of permanent stoma [8, 9].
The etiology of the anastomotic leakage is multifactorial, including technical and patient factors. Technical factors include excessive tension across anastomosis, ischemia of the intestine at the suture line, the presence of local sepsis, and faulty technique. Older age (> 80 years), anemia, low albumin, associated co morbidities, and high doses of steroids are some of the patient-related factors that may also contribute to increased risk of anastomotic leakage. The purpose of this article was to review our own results with respect to the possible etiological factors for the anastomotic leakage and their management.
The primary objective was to determine whether sphincter preservation is possible among the patients who develop anastomotic leakage after rectal cancer surgery. The secondary objective was to determine the factors that may contribute to the anastomotic leakage.
Materials and Methods
This is a retrospective review of a prospectively maintained database in the Division of Colorectal Surgery, Department of Surgical Oncology at the Tata Memorial Centre, Mumbai. All patients with rectal cancer who underwent restorative proctectomy between July 1, 2013 and June 30, 2014 were included in this study. Management of rectal cancer was done according to the standard guidelines, with early tumors (T1/2 N0) operated upfront whereas those with locally advanced disease (≥T3/N+) offered neoadjuvant chemoradiotherapy followed by surgery. All treatment decisions were taken by a multidisciplinary team consisting of a colorectal surgeon, a radiation oncologist, a gastroenterologist, a medical oncologist, and a radiologist. The choice of an open or minimally invasive approach was based on the availability of facilities for minimally invasive surgery on that day.
The extent of surgery was decided based on the preoperative MRI with sphincter-preserving surgery being offered to all patients in whom external sphincter was not involved by the tumor and at least 1-cm tumor-free distal margin could be obtained. Bowel preparation was given to all the patients on the day before surgery except those with features of bowel obstruction or who unequivocally required abdominoperineal resection on preoperative MRI. Ligation of inferior mesenteric artery (IMA) pedicle was considered as high when it was performed at the root whereas it was considered as low when ligated after the origin of the left colic artery. Decision on high or low ligation was individualized depending on the length of the colon available for anastomosis with the sole objective being tension-free anastomosis.
Type of anastomosis depended on the extent of resection. For patients who underwent intersphincteric resection, hand-sewn coloanal anastomosis was performed using 3–0 Vicryl. For rest of the cases, end-to-end stapled anastomosis was performed using circular stapler of size 29. The anastomosis was considered to be low when it was situated below the level of peritoneal reflection. Air leak test was performed for all the patients after anastomosis. When the test results were positive, reinforcing sutures were placed in the areas of the leakage. A defunctioning loop ileostomy was performed for all the patients with low anastomosis as well as for those in whom anastomosis was intraoperatively considered as high risk for anastomotic leakage. These included situations such as edematous bowel wall after the resection of the tumor, emergency surgery with unprepared bowel, or positive air leak test in elderly individuals.
Anastomotic leakage was defined clinically as the presence of feculent discharge from the drain, or clinical features of intra-abdominal sepsis or dehiscence of suture lines on per rectal examination; and radiologically (Computed tomography with oral contrast and Gastrograffin enema) as anastomotic leakage of contrast or any peri-anastomotic collection requiring drainage. For patients who had prior defunctioning loop ileostomy and who were hemodynamically stable, sutures were placed at the sites of suture dehiscence trans anally after thorough lavage through perineal exploration. For patients with signs of peritonitis or hemodynamic instability or failed conservative management, exploratory laparotomy was performed. Defunctioning loop ileostomy with placement of intraperitoneal drains was performed for all these patients after thorough peritoneal lavage. Decision to disconnect the anastomosis was based on the intraoperative findings with Hartmann’s procedure performed whenever there was complete suture dehiscence or necrosis of the significant length of colon proximal to the anastomosis. All the patients were regularly followed up after the discharge and ileostomy reversal was planned at the end of adjuvant therapy or 6 weeks after the primary surgery with prior confirmation of anastomotic integrity (gastrografin enema) and adequate sphincter function (anal manometry).
Baseline characteristics and details of surgery and perioperative therapy of all the patients included in the study were collected from the database. Patient-related factors likely to influence the risk of anastomotic leakage analyzed were age, preoperative hemoglobin and albumin, and associated comorbidities. Treatment-related factors analyzed were preoperative therapy, type of surgery (open vs minimally invasive), level of ligation of IMA pedicle (high vs low), technique of anastomosis (hand-sewn vs stapled), and defunctioning proximal stoma. Statistical analysis was performed using SPSS statistical software, version 18.0. The χ 2-test or Fisher’s exact test, as appropriate, was used for univariate analysis. A logistic regression model was used to compare the two groups (those with anastomotic leakage and those without anastomotic leakage) and the study endpoints; this was adjusted for variables that were significant in univariate analysis and/or clinically expected to be of importance.
Results
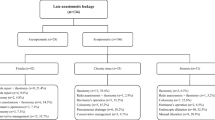
A total of 176 anterior resections were performed between July 1, 2013 and June 30, 2014. Baseline patient characteristics are shown in Table 1. Because this was a retrospective review, ASA grade was not available for 35 patients and body mass index (BMI) was not available for 40 patients. Analysis of these two parameters excluded those with missing data, but for the rest of the parameters, all data were available and hence all patients were included. None of the factors contributing to anastomotic leakage reached statistical significance on univariate analysis (Table 2).
Among the patients included in the study, 15 (8.5 %) had anastomotic leakage (Table 3). Majority presented on seventh postoperative day (POD). The patients without proximal defunctioning ileostomy presented earlier (median POD 3) than those with stoma (median POD 7). Most common presenting symptom was persistent fever (94 %). Eleven patients (74 %) required reoperation whereas four were managed conservatively (26 %). One patient died due to septicemia after the anastomotic leakage. This patient had undergone anterior exenteration and developed anastomotic leakage as well as leakage from ileal conduit. Though the patient was reexplored twice with disconnection of the anastomosis, he had developed septicemic shock and could not be revived.
Among the patients who had proximal defunctioning ileostomy (n = 9), re-surgery was required in five (56 %) whereas other four were managed with antibiotics and presacral drainage alone (44 %). Among those patients who underwent re-surgery (n = 5), perineal resuturing of the anastomosis was performed in two (40 %), transabdominal reanastomosis in one, peritoneal lavage in one, and anastomosis was disconnected in one (20 %) patient. Thus, laparotomy could be avoided in six patients (67 %) when proximal defunctioning ileostomy was performed at the time of primary surgery.
Among the patients who did not have proximal defunctioning ileostomy (n = 6), re-surgery was required in all the patients (100 %). Disconnection of the anastomosis was required in one patient and peritoneal lavage with creation of ileostomy was required in the rest. Reanastomosis during the re-surgery was not possible in any of these patients due to significant peritoneal contamination.
At a median follow-up of 18 months, one patient had perioperative mortality, two patients developed distant recurrence (one each in lung and liver) within 6 months of index surgery, and follow-up details of three patients were not available. Among the nine patients available for evaluation, stoma reversal was successful in eight. One patient developed stricture at the anastomotic site as well as radiation-induced cystitis. She has been planned for dilatation of the stricture and then stoma reversal once her general health improves. Thus, successful stoma reversal was possible in 8 of 15 patients (53 %) who developed leak. If the patient who died and those patients who developed distant recurrence were excluded, the sphincter preservation was possible in 8 of 12 patients (67 %).
Discussion
The incidence of anastomotic leakage after surgery for rectal cancer ranges between 1.8 and 19.8 % [2, 3]; however, these rates vary according to the definition used. Higher rates are reported whenever anastomotic leakage is detected by radiology (CT, or gastrografin enema). At our center, routine gastrografin enema is not the standard practice in all the postoperative patients. Hence, an anastomotic leakage rate of 8.5 % is consistent with that reported in the literature. Mortality rate in the present series (6.7 %) also is consistent with that reported in the literature (6.25–10 %) [4, 5].
Sphincter preservation is the major objective of rectal cancer surgery besides oncological safety. A permanent stoma because of the anastomotic leakage is even more distressing for the patient. Earlier studies have shown that anastomotic leakage after anterior resection has a higher probability of permanent stoma formation with stoma reversal possible in only 33 % patients who required stoma creation for the anastomotic leakage in one of the series [8, 9]. In the present series, successful stoma reversal was possible in 53 % patients. Improved results were because only two patients in this study required discontinuation of anastomosis.
Some of the identified risk factors for anastomotic leakage are male gender, nutritional status, high BMI, the location of anastomosis, diverting stoma, and history of radiation [10–13]. Men, because of the narrow pelvis, offer greater challenge during pelvic dissection, and hence increased risk of anastomotic leakage [14]. In this study, incidence of anastomotic leakage was slightly higher in men than in women though it did not reach statistical significance. An interesting association that emerged during this analysis was the association of a high tumor regression grade (by Mandard scoring system) with anastomotic leakage (16.1 % for TRG 3/4 vs 4.4 % for TRG 1/2). This might be an indication of the response of the host tissue microvasculature to radiotherapy.
The role of defunctioning proximal stoma in cases of low anterior resection has been debated for many years. Proponents stress that the stoma keeps the distal anastomosis clean and reduces the intraluminal pressure of the bowel and as a result reduces the anastomotic leakage rate and its consequences [15]. However, fecal diversion requires the patient to undergo two surgeries, and stoma reversal is associated with significant morbidity and costs [16]. In addition, even when a defunctioning proximal stoma is created, there remains a significant risk of anastomotic leakage [17]. Therefore, the benefits of a stoma in decreasing the rate of anastomotic leakage must be balanced against the morbidity and cost of reversal. Several studies in the past have found that the rate of anastomotic leakage was not reduced by the construction of defunctioning proximal stoma [11, 13, and 18]. However, couple of recent meta-analyses have shown that defunctioning proximal stoma significantly reduces the incidence as well as the consequences of the anastomotic leakage [19, 20]. In this study, rates of anastomotic leakage were higher when defunctioning proximal stoma was not constructed (14.9 % vs 6.2 %) though it did not reach statistical significance (p = 0.068). In addition, among the patients with proximal defunctioning stoma created during primary surgery, conservative management could be followed in significant number of patients (44 %). In this subgroup of patients, even when re-surgery was required, transanal resuturing of the anastomotic dehiscence was possible in significant number of patients and hence relaparotomy and its associated morbidity could be avoided in up to 40 % patients.
Anastomosis situated below the peritoneal reflection has been proposed to be at higher risk for anastomotic leakage [21]. The probable reasons for an increased leakage rate being reduced blood supply of the anorectal remnant and the large pelvic space that may predispose a patient to fluid accumulation and pelvic infection [22]. In this study, anastomotic leakage was higher for anastomosis situated below the peritoneal reflection (11.8 % vs 6 %) though it did not reach statistical significance (p = 0.18).
Some studies have identified laparoscopic surgery as a risk factor for anastomotic leakage [14] whereas others have not found any association between the approach and the incidence of anastomotic leakage [23, 24]. In this study, incidence of anastomotic leakage was slightly higher in open surgery than in laparoscopic surgery though it did not reach statistical significance. This can be explained by the fact that those who underwent open surgery had more advanced disease leading to greater technical difficulties. Radiation therapy leads to decreased oxygen delivery to the tissues and hence prevents optimum tissue healing. Earlier studies have shown that anastomotic leakage rate is higher among those who receive neoadjuvant chemoradiotherapy [11, 21, and 22]. In the present series also the anastomotic leakage rate was higher among those who received preoperative chemoradiotherapy (10.7 % vs 5.5 %) though it did not reach statistically significance (p = 0.17).
Influence of level of ligation of IMA pedicle on anastomotic leakage is highly debated. Adequate anastomotic perfusion is considered the most important prerequisite for anastomotic healing. High ligation of IMA pedicle enables anastomotic perfusion only through the marginal artery, whereas a low ligation enables anastomotic perfusion not only through the marginal artery but also through the left colic artery and its ascending branch. On the basis of this hypothesis, low ligation of the IMA pedicle should result in lower anastomotic leakage rates [25, 26]. However in this study, none of the patients with the high ligation were found to develop anastomotic leakage whereas 10.5 % patients with low ligation developed anastomotic leakage, though the difference did not reach statistical significance (p = 0.13). Better results with high ligation can be attributed to better reach of the colon into pelvis and tension-free anastomosis.
This study had its limitations. Being a retrospective analysis, it is amenable to the usual biases of the retrospective studies. Less number of events among the patients included in the study might have prevented any one of the factors from significantly influencing the rates of anastomotic leakage. However, the lower incidence of anastomotic leakage among the patients with ligation of IMA pedicle at the root as well as those with better response to neoadjuvant therapy deserves further research.
Conclusion
Defunctioning proximal stoma may reduce the incidence and severity of anastomotic leakage as well as the need and extent of re-surgery for low rectal cancer surgery. Sphincter preservation is possible in majority of patients who develop anastomotic leakage after the surgery for rectal cancer.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCON 2012. Int J Cancer 136(5):E359–E386
Choi H-K, Law W-L, Ho JWC (2006) Leakage after resection and intraperitoneal anastomosis for colorectal malignancy: analysis of risk factors. Dis Colon Rectum 49(11):1719–1725
Platell C, Barwood N, Dorfmann G, Makin G (2007) The incidence of anastomotic leaks in patients undergoing colorectal surgery. Color Dis 9(1):71–79
Branagan G, Finnis D, Wessex Colorectal Cancer Audit Working Group (2005) Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum 48(5):1021–1026
Pakkastie TE, Luukkonen PE, Järvinen HJ (1994) Anastomotic leakage after anterior resection of the rectum. Eur J Surg 160(5):293–297; discussion 299–300.
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253(5):890–899
den Dulk M, Marijnen CA, Collette L, Putter H, Påhlman L, Folkesson J, Bosset JF, Rödel C, Bujko K, van de Velde CJ (2009) Multicentre analysis of oncological and survival outcomes following anastomotic leakage after rectal cancer surgery. Br J Surg 96(9):1066–1075
Khan AA, Wheeler JMD, Cunningham C, George B, Kettlewell M, Mortensen NJM (2008) The management and outcome of anastomotic leaks in colorectal surgery. Color Dis 10(6):587–592
Arumainayagam N, Chadwick M, Roe A (2009) The fate of anastomotic sinuses after total mesorectal excision for rectal cancer. Color Dis 11(3):288–290
Irvin TT, Goligher JC (1973) Aetiology of disruption of intestinal anastomoses. Br J Surg 60(6):461–464
Matthiessen P, Hallböök O, Andersson M, Rutegård J, Sjödahl R (2004) Risk factors for anastomotic leakage after anterior resection of the rectum. Color Dis 6(6):462–469
Polese L, Vecchiato M, Frigo AC, Sarzo G, Cadrobbi R, Rizzato R, Bressan A, Merigliano S (2012) Risk factors for colorectal anastomotic stenoses and their impact on quality of life: what are the lessons to learn? Color Dis 14(3):e124–e128
Tuson JR, Everett WG (1990) A retrospective study of colostomies, leaks and strictures after colorectal anastomosis. Int J Color Dis 5(1):44–48
Krarup P-M, Jorgensen LN, Andreasen AH, Harling H, Danish Colorectal Cancer Group (2012) A nationwide study on anastomotic leakage after colonic cancer surgery. Color Dis 14(10):e661–e667
Peeters KC, Tollenaar RA, Marijnen CA, Klein Kranenbarg E, Steup WH, Wiggers T, Rutten HJ, van de Velde CJ, Dutch Colorectal Cancer Group (2005) Risk factors for anastomotic failure after total mesorectal excision of rectal cancer. Br J Surg 92(2):211–216
Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M (2008) Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum 51(2):218–222
Pakkastie TE, Ovaska JT, Pekkala ES, Luukkonen PE, Järvinen HJ (1997) A randomised study of colostomies in low colorectal anastomoses. Eur J Surg 163(12):929–933
Konishi T, Watanabe T, Kishimoto J, Nagawa H (2006) Risk factors for anastomotic leakage after surgery for colorectal cancer: results of prospective surveillance. J Am Coll Surg 202(3):439–444
Gu W-L, Wu S-W (2015) Meta-analysis of defunctioning stoma in low anterior resection with total mesorectal excision for rectal cancer: evidence based on thirteen studies. World J Surg Oncol 13(1):9
Wu S-W, Ma C-C, Yang Y (2014) Role of protective stoma in low anterior resection for rectal cancer: a meta-analysis. World J Gastroenterol 20(47):18031–18037
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M (1998) Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 85(3):355–358
Veyrie N, Ata T, Muscari F, Couchard A-C, Msika S, Hay J-M, Fingerhut A, Dziri C, French Associations for Surgical Research (2007) Anastomotic leakage after elective right versus left colectomy for cancer: prevalence and independent risk factors. J Am Coll Surg 205(6):785–793
Hua L, Wang C, Yao K, Zhang J, Chen J, Ma W (2014) Is the incidence of postoperative anastomotic leakage different between laparoscopic and open total mesorectal excision in patients with rectal cancer? A Meta-analysis Based on Randomized Controlled Trials and Controlled Clinical Trials. J Cancer Res Ther 10(Suppl 8):272–275
El-Gazzaz G, Geisler D, Hull T (2010) Risk of clinical leak after laparoscopic versus open bowel anastomosis. Surg Endosc 24(8):1898–1903
Lange MM, Buunen M, van de Velde CJH, Lange JF (2008) Level of arterial ligation in rectal cancer surgery: low tie preferred over high tie. Dis Colon Rectum 51(7):1139–1145
Seike K, Koda K, Saito N, Oda K, Kosugi C, Shimizu K, Miyazaki M (2007) Laser Doppler assessment of the influence of division at the root of the inferior mesenteric artery on anastomotic blood flow in rectosigmoid cancer surgery. Int J Color Dis 22(6):689–697
Conflict of Interest
Sudhir Jatal, Vishwas D. Pai, Jean Demenezes, Ashwin Desouza, and Avanish P. Saklani declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jatal, S., Pai, V.D., Demenezes, J. et al. Analysis of Risk Factors and Management of Anastomotic Leakage After Rectal Cancer Surgery: An Indian Series. Indian J Surg Oncol 7, 37–43 (2016). https://doi.org/10.1007/s13193-015-0457-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-015-0457-1