Abstract
The St. Jude Cancer Education for Children Program (SJCECP) aims to teach children about cancer and cancer control behaviors. During the 2012–2014 academic year, we conducted a pilot evaluation of the SJCECP curriculum to determine its impact on cancer risk awareness, attitudes, and behavioral intentions among fourth-grade students participating in the program. Nine local schools and 426 students from the Memphis area participated in the program evaluation. The results of this study show an increase in fourth-grade students’ overall cancer risk factor awareness, attitudes, and behavioral intentions after participation in the intervention. The study also compared the mean change score for unaware students (e.g., those whose mean item score was < 3.5 on the pre-test) between students from racially identifiable/high-poverty schools (school group 1; six schools) and racially diverse/affluent schools (school group 2; three schools). Comparison of the mean change score for unaware students between school group 1 and school group 2 showed that increases in overall cancer risk factor awareness in school group 1 were higher than the increases of unaware students seen in school group 2; however, no differences between the changes in attitudes towards cancer risk factors and cancer control intentions and behaviors between the school groups were observed. We conclude that the SJCECP curriculum is successful in promoting cancer risk factor awareness, positive attitudes towards cancer risk factors, and increased cancer control intentions and behaviors among students at the fourth-grade level regardless of school demographics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The American Cancer Society (ACS) predicted that there would be approximately 1,688,780 new cancer cases diagnosed in 2017 in the USA and approximately 600,920 Americans are expected to die of cancer, accounting for one in every four deaths [1]. Research has shown that individuals from racial and ethnic minorities, medically underserved populations, and low socioeconomic (SES) backgrounds are disproportionately impacted by the burden of cancer [2]. Factors most likely to contribute to the disparities in cancer incidence and mortality include inequalities in risky lifestyle habits, such as smoking, obesity, physical inactivity, diet, and alcohol use [2]. Since lifestyle habits are often developed in childhood, health education targeting young children is essential for establishing healthy behaviors that may reduce future cancer risk and thus minimizing these disparities [3,4,5,6]. Schools, therefore, provide an excellent avenue for delivering health promotion programs to children in the USA, including those from racial and ethnic minority groups, medically underserved populations, and low socioeconomic backgrounds.
While the nationwide gaps in cancer outcomes for racial minority and low SES community members are the cause for considerable concern, the challenges in Memphis, TN, are even greater. The Shelby County School (SCS) district is the largest in the Memphis area, serving over 100,000 students. Of these students, 78.0% are black, 12.3% are Hispanic, 7.7% are white, and 59.1% are economically disadvantaged, resulting in several racially identifiable (the proportion of students of one race is at least 75%), high-poverty schools (defined as having greater than 75% of students qualifying for free or reduced lunches) [7]. The municipal school districts in the Memphis suburbs combined serve approximately 31,000 students. Of these students, 20.8% are black, 8.4% are Hispanic, 66.1% are white, and 11.3% are economically disadvantaged [7]. The disproportionate number of students from traditionally underserved racial/ethnic groups and low SES in the SCS district provides an opportunity in the Memphis area to partner with the SCS district to target cancer health disparities with educational intervention strategies.
The St. Jude Cancer Education for Children Program (SJCECP) partners with local schools and community organizations to disseminate health and science curricula designed to educate students about the science of cancer formation, cancer treatment, and cancer risk reduction through healthy lifestyle habits. Specifically, the program addresses physical fitness, nutrition, tobacco prevention, and reductions in sun exposure, important issues in promoting childhood health, and primary cancer prevention. When the program began in 2006, the school outreach team developed an upper elementary school curriculum for grades 3–4, as this is when the SCS first introduce the scientific concept of cells in their curriculum. A formal evaluation of the upper elementary school curriculum showed significant gains in knowledge related to cells, cancer, and healthy living among fourth graders that participated in the program intervention [8, 9]. The implication of these findings is that such knowledge may be the foundation for reducing behaviorally mediated cancers in adulthood.
Knowledge acquisition, however, is only one possible predictor of behavior change. Classical health behavior change theories such as the Health Belief Model and Theory of Planned Behavior suggest that knowledge, attitudes, and beliefs predict individual behavior change mediated by behavioral intention [10, 11]. Health behavior changes are often influenced by multiple variables, including socio-demographic factors such as race, gender, and economic status, and psychological factors [12]. Looking at how attitudes, beliefs, perceptions of susceptibility and severity, intentions, and self-reported health behaviors of individuals differ across socio-demographics can provide a more complete picture of the program’s impact on behavior change [12, 13]. Building upon our prior work, this paper describes the impact of the SJCECP study with regard to changes in the students’ cancer risk factor awareness, attitudes towards cancer risk factors, and cancer control intentions and behaviors over time. Comparisons regarding the impact of the SJCECP between schools that are racially identifiable/high-poverty schools and racially diverse/affluent schools are also provided.
Methods
Study Design and Materials
This study utilized a single-group, pre-test/post-test design to determine the impact of the SJCECP fourth-grade curriculum on the cancer risk factor awareness, attitudes towards cancer risk factors, and cancer control intentions and behaviors of fourth-grade students. The SJCECP intervention consists of three illustrated children’s books, video presentations, and hands-on activities, and was delivered by classroom teachers. All of the educational materials were developed and reviewed by a multidisciplinary team composed of St. Jude faculty and staff and local educators. There are three educational modules: cells (presented as the basic unit of life), cancer (presented as a disease of unhealthy cells), and healthy Living (health behaviors as a means of cancer prevention including safe sun exposure, tobacco avoidance, and weight management through nutrition and physical activity). A more detailed report of the SJCECP intervention materials has been published previously [8].
Study Sample
Before student study enrollment, letters were sent to school principals through the local school boards, inviting all affiliated public schools with classes in grade 4 to participate in the study. We also sent letters to the principals at private elementary schools in the area for recruitment purposes. Through 2012–2014, 18 teachers and 426 students from nine local schools participated in the SJCECP intervention evaluation. Approximately 93% of the students were from public schools, and this reflected the approximate distribution of public to private students in the region. Student participants in the study were fourth-grade boys and girls aged 8–11 years enrolled in traditional curriculum classrooms with the cognitive capacity to complete questionnaires (as determined by the teacher), whose teacher agreed to participate in the study, and who attended a school in Shelby County (SCS District, municipal district, or private school). All classroom teachers gave their written informed consent prior to their participation in the study. In addition, all parents of students were given an informed consent document providing them the opportunity to opt-out of participation, as approved by the Institutional Review Board at St. Jude Children’s Research Hospital.
The school distribution of racial and ethnic groups and students that qualified for free or reduced lunches were recorded. While the overall demographic data of participating schools, when adjusted for number of student participants, reflect that of the Shelby County population (Table 1), six of the nine schools were racially identifiable, high-/mid-high-poverty schools (Table 2).
Measures
To assess students’ awareness of cancer-related risk factors, attitudes towards cancer risk factors, and cancer control intentions/behaviors, a 39-item questionnaire was designed with 19 questions related to cancer risk factor awareness, 8 questions related to attitudes towards cancer risk factors, and 12 questions related to cancer control intentions and behaviors. Questions were scored on a 5-point Likert scale (strongly disagree to strongly agree) with a neutral option in the center. For each section, Cronbach’s alphas were calculated to determine internal reliability of the question sets.
Teachers administered the survey within 7 ± 1 days before delivering the SJCEP curriculum to students (Timepoint = T1) and again 7 ± 1 days after completing the educational curriculum (Timepoint = T2). There was no time limit on individuals to complete the survey—time given was at the discretion of the teacher. Differences in the scores from pre- to post-assessment were utilized in subsequent analyses.
Cancer Risk Factor Awareness
Students’ cancer risk awareness regarding tobacco use, sun protection, nutrition, and physical fitness was assessed using student responses to 19 survey questions, covering topics related to general awareness (2 items), tobacco use (4 items), sun protection (4 items), nutrition (5 items), and physical activity (4 items). With the exception of general awareness, the internal reliability coefficients (e.g., Cronbach alphas) ranged from 0.63–0.67.
General Awareness
General awareness of cancer risk factors was measured using the following items: “What someone does as a young adult has little effect on their chance of getting cancer later in life,” “Cancer can be cured if caught early enough.”
Tobacco Use
Awareness of the impact of tobacco on cancer risk was measured using the following items: “I believe that using chewing tobacco or dip can cause cancer,” “I believe that the smoke from other people’s cigarettes cause you to get cancer,” “I can reduce my chances of cancer by not using tobacco,” “My chances are higher that I will get cancer if I smoke or use tobacco now or in the future.”
Sun Protection
Awareness of the impact of sun protection on cancer risk was measured using the following items: “I believe it is important to wear sunscreen to reduce my chance of skin cancer,” “I believe that going tanning can cause cancer,” “I can reduce my chance of cancer by protecting my skin from sun damage,” “My chances are higher that I will get cancer if I go to tanning salons now or in the future.”
Nutrition
Awareness of the impact of nutrition on cancer risk was measured using the following items: “I am aware of the energy (calorie) content in foods that I eat,” “I believe fruits and vegetables are important to eat to reduce my chance of getting cancer,” “I believe that a hamburger and French fries is a healthy meal,” “I can reduce my chance of cancer by eating healthy food,” “My chances are higher that I will get cancer if I eat unhealthy foods now or in the future.”
Physical Activity
Awareness of the impact of nutrition on cancer risk was measured using the following items: “I believe physical activity is important for reducing my chances of getting cancer,” “I believe I have opportunities to be active outside of school,” “I can reduce my chance of cancer by getting at least 60 minutes of physical activity each day,” “My chances are higher that I will get cancer if I get less than 60 minutes of physical activity every day.”
Attitudes Towards Cancer Risk Factors
Students’ attitudes towards cancer risk regarding tobacco use, sun protection, nutrition, and physical fitness were assessed using student responses to 8 survey questions, covering topics related to tobacco use (2 items), sun protection (2 items), nutrition (2 items), and physical activity (2 items). The internal reliability coefficients (e.g., Cronbach alphas) ranged from 0.33–0.58.
Tobacco Use
Attitudes towards tobacco use were measured using the following items: “Breathing in someone else’s smoke bothers me,” “I feel smoking or using tobacco makes a person look cool or grown up.”
Sun Protection
Attitudes towards sun protection were measured using the following items: “I feel healthy when I have a nice tan,” “I feel it is a lot of trouble to apply sunscreen.”
Nutrition
Attitudes towards nutrition were measured using the following items: “I can reduce my chance of cancer by eating healthy food,” “I prefer healthy snacks over junk food,” “I feel better when I eat healthy foods.”
Physical Activity
Attitudes towards physical fitness were measured using the following items: “I feel it is a lot of trouble to do 60 minutes of physical activity every day,” “I feel better when I do physical activity.”
Cancer Control Intentions and Behaviors
Students’ cancer control intentions and behaviors in regard to tobacco use, sun protection, nutrition, and physical fitness were assessed using student responses to 12 survey questions, covering topics related to tobacco use (4 items), sun protection (2 items), nutrition (3 items), and physical activity (3 items). The internal reliability coefficients (e.g., Cronbach alphas) ranged from 0.29–0.64.
Tobacco Use
Intentions and behaviors related to tobacco use were measured using the following items: “I might try smoking cigarettes in the future,” “I might smoke or use tobacco in the future if my friends did,” “I have used tobacco in the past 7 days,” “I have been around others while they have been smoking in the past 7 days.”
Sun Protection
Intentions and behaviors related to sun protection were measured using the following items: “I plan to use sun protection methods in the future to reduce my chance of cancer,” “I might go to a tanning salon in the future.”
Nutrition
Intentions and behaviors related to nutrition were measured using the following items: “I plan to make healthy food choices in the future to help reduce my chance of getting cancer,” “I plan to ask my family to eat healthy foods in the future to help reduce their chance of getting cancer,” “I have eaten fruits and vegetables on most days in the past 7 days.”
Physical Activity
Intentions and behaviors related to physical fitness were measured using the following items: “I plan to do at least 60 minutes of physical activity every day in the future to help reduce my chance of getting cancer,” “I plan to ask my family to do more physical activity in the future,” “I have been physically active for at least 60 minutes on most days in the past 7 days.”
Analysis
The comparison of pre- and post-test of the three domains and their sub domains was analyzed by treating them as continuous variables. Since these are paired tests and the data were not normally distributed, the Wilcoxon signed rank test was used to calculate the p value. p values < 0.05 were considered statistically significant.
To assess the generalizability of the intervention, the data were stratified based on school demographic data. Study participants were divided into either school group 1 or school group 2 based on the proportion of economically disadvantaged students and whether or not the school was racially identifiable. School group 2 included all schools that were both racially identifiable and high-poverty schools (schools 1, 2, 3, 7, 8, and 9; Table 2). The remaining schools (schools 4, 5, and 6) were placed into school group 1. Students from both groups that scored a mean item score of greater than or equal to 3.5 for each subdomain on the pre-test were excluded from this analysis in order to assess the impact of the program on the most at-risk students (those students that were the most unaware, had most unfavorable attitudes and lowest behavioral intentions) in each school group. The Kruskal-Wallis test was used to compare the mean change (pre vs. post) between school group 1 and school group 2 as they are independent groups and the scores were not normally distributed.
Results
Cancer Risk Factor Awareness
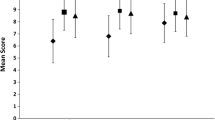
The overall mean score for the cancer risk factor awareness survey increased from 69.35 (T1) (12.15 SD) to 74.57 (T2) (12.42 SD) with a mean change of 6.00 (p < 0.0001). The mean score values were also calculated for the following subdomains (max score): cancer risk (10), smoking (20), sun protection (20), nutrition (25), and physical activity (20). The mean score for the cancer risk subdomain increased from 6.42 (T1) (1.45 SD) to 6.67 (T2) (1.57 SD) with a mean change of 0 (p = 0.01). The mean score for the smoking subdomain increased from 15.63 (T1) (3.06 SD) to 16.96 (T2) (3.06 SD) with a mean change of 1.00 (p < 0.0001). The mean score for the sun protection subdomain increased from 14.16 (T1) (3.19 SD) to 15.98 (T2) (3.11 SD) with a mean change of 2.00 (p < 0.0001). The mean score for the nutrition subdomain increased from 19.28 (T1) (3.45 SD) to 20.09 (T2) (3.80 SD) with a mean change of 1.00 (p < 0.0001). The mean score for the physical activity subdomain increased from 14.83 (T1) (3.02 SD) to 15.59 (T2) (3.16 SD) with a mean change of 1.00 (p = 0.0001). Analysis showed a significant increase in students’ overall cancer risk factor awareness as well as for each subdomain (Table 3).
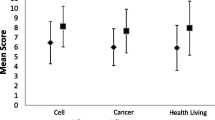
Comparison of the mean change score for unaware students (e.g., those whose mean item score was < 3.5 on the pre-test) between school group 1 and school group 2 showed that increases in overall cancer risk factor awareness in school group 1 were significantly higher than the increases of unaware students seen in school group 2 as well as for each subdomain, with the exception of smoking (Table 4).
Attitudes Towards Cancer Risk Factors
The overall mean score for the cancer risk factor awareness survey increased from 31.45 (T1) (4.89 SD) to 32.57 (T2) (4.96 SD) with a mean change of 1.00 (p < 0.0001). The mean score values were also calculated for the following subdomains (max score): smoking (10), sun protection (10), nutrition (10), and physical activity (10). The mean score for the smoking subdomain increased from 8.81 (T1) (1.73 SD) to 8.99 (T2) (1.55 SD) with a mean change of 0 (p = 0.04). The mean score for the sun protection subdomain increased from 7.03 (T1) (1.78 SD) to 7.41 (T2) (1.94 SD) with a mean change of 0 (p = 0.001). The mean score for the nutrition subdomain increased from 8.01 (T1) (1.81SD) to 8.34 (T2) (1.71 SD) with a mean change of 0 (p = 0.002). The mean score for the physical activity subdomain increased from 7.94 (T1) (1.86 SD) to 8.15 (T2) (1.81 SD) with a mean change of 0 (p = 0.05). Analysis showed a significant increase in students’ overall attitudes towards cancer risk factors as well as for each subdomain (Table 3).
Comparison of the mean change score for unaware students (e.g., those whose mean item score was < 3.5 on the pre-test) between school group 1 and school group 2 showed no significant difference between the changes in attitudes towards cancer risk factors between school group 1 and school group 2 (Table 4).
Cancer Control Intentions and Behaviors
The overall mean score for the cancer risk factor awareness survey increased from 43.77 (T1) (7.02 SD) to 45.03 (T2) (6.75 SD) with a mean change of 2.00 (p < 0.0001). The mean score values were also calculated for the following subdomains (max score): smoking (20), sun protection (10), nutrition (15), and physical activity (15). The mean score for the smoking subdomain increased from 12.64 (T1) (2.07 SD) to 12.73 (T2) (1.88 SD) with a mean change of 0 (p = 0.26). The mean score for the sun protection subdomain increased from 7.47 (T1) (1.82 SD) to 8.08 (T2) (1.94 SD) with a mean change of 0 (p < 0.0001). The mean score for the nutrition subdomain increased from 9.80 (T1) (2.24 SD) to 10.01 (T2) (2.25 SD) with a mean change of 0 (p < 0.02). The mean score for the physical activity subdomain increased from 14.01 (T1) (2.81 SD) to 14.38 (T2) (2.77 SD) with a mean change of 0 (p < 0.01). Analysis showed a significant increase in students’ overall cancer control intentions and behaviors as well as for each subdomain (Table 3).
Comparison of the score mean change between school group 1 and school group 2 showed no significant difference between the changes in cancer control intentions and behaviors of unaware students (e.g., those whose mean item score was < 3.5 on the pre-test) between school group 1 and school group 2 (Table 4).
Discussion
Significant gains in awareness of smoking, sun protection, nutrition, and physical activity as cancer risk factors were observed after participation in the intervention. In addition, students showed more positive attitudes towards cancer risk factors and increased cancer control intentions and behaviors after participation in the intervention. It should be noted that students demonstrated greater increases in awareness (pre-post paired = 6.00) compared to attitudes (pre-post paired = 1.00) and behavior and intentions (pre-post paired = 2.00). This is likely due to the fact that the intervention was delivered in a structure education system, which specializes in student knowledge acquisition. Attitudes and behaviors are more likely to be influenced by external factors that may not be addressed in a structured school environment, such as family health habits, food deserts, access to parks, and neighborhood safety. More study is needed to determine the impact of school and community characteristics on health-promoting interventions.
Students from more affluent schools appeared to have significantly more gains in cancer risk factor awareness than students from racially identifiable/high-poverty schools; however, there was no observed difference between the changes in attitudes towards cancer risk factors overall and for nearly all of the subdomains. Students from racially identifiable/high-poverty schools may have benefitted more from the nutrition portion of the intervention, although it is unclear what factors might contribute to this increased benefit or whether or not this was an artifact in the data. Further study is still needed to determine whether or not any true benefit exists in regard to attitudes towards nutrition. No significant difference in changes to cancer control intentions and behaviors between the school group 1 and school group 2 was observed. This reinforces the idea that the school environment may play an important role in the extent to which a health intervention will be effective. More study is needed to determine whether or not systemic differences between schools and school districts influence the success of health interventions.
Despite the differences in gains to cancer risk factor awareness, the results of this study suggest that the SJCECP may still be a useful tool for changing attitudes towards cancer risk factors and cancer control intentions and behaviors in fourth graders regardless of school demographics. Health education curriculum, however, is only one element in the school culture that influences students’ attitudes and behaviors towards healthy living [14, 15]. Classroom health education needs to be reinforced by a school wellness policy that promotes a holistic approach to improving student health across four key elements: school curriculum, school environment, school nutrition and health services, and the school community [11, 12]. Future efforts should engage schools and communities in community-based participatory research to identify barriers and limitations to implementing school wellness policies in racially identifiable/high-poverty schools and developing strategies for overcoming these barriers. Future studies should also consider the role of institutions in promoting student health and inequities that may exist across schools and school districts.
This study had limitations. We used a pre-post design rather than a randomized trial and did not have control schools; this design was chosen because of available resources and feasibility for implementation. We are therefore unable to rule out the possibility that our findings were a result of differences between study groups despite controlling for key demographic factors in all analyses. While study participation was made available to all fourth-grade teachers in the area, it is possible that a degree of self-selection bias occurred whereby only teachers interested in providing cancer education to their students agreed to participate in the study. The teachers’ motivation may have influenced the positive results and may not translate to classrooms with teachers less motivated to provide cancer education. Another limitation of the study is that we relied on self-reporting for cancer control intentions/behaviors with relatively low internal reliability measures (Chronbach alphas). Future research should incorporate more valid measures of behavior (bioverification of secondhand smoke exposure or tobacco use, BMI changes, etc.) as opposed to self-report.
Conclusion
The results of this study suggest that the SJCECP curriculum is successful in promoting cancer risk factor awareness, positive attitudes towards cancer risk factors, and increased cancer control intentions and behaviors among students at the fourth-grade level regardless of school demographics. In total, these results support the idea of using the SJCECP curriculum to target disparity gaps in the Memphis area through a school-based educational strategy.
References
American Cancer Society (2017) Cancer facts & figures 2017. American Cancer Society, Atlanta https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2017/cancer-facts-and-figures-2017.pdf. Accessed 27 June 2017
Singh GK, Jemal A (2017) Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health 2017:1–19. https://doi.org/10.1155/2017/2819372
White MC, Peipins LA, Watson M, Trivers KF, Holman DM, Rodriguez JL (2013) Cancer prevention for the next generation. J Adolesc Health 52(5 Suppl):S1–S7
Holman DM, Rodriguez JL, Peipins L, Watson M, White MC (2013) Highlights from a workshop on opportunities for cancer prevention during preadolescence and adolescence. J Adolesc Health 52(5 Suppl):S8–S14
Haverkos L (2010) Pediatric behavior and health promotion research program, Washington, DC, National Institutes of Health http://www.nichd.nih.gov/about/org/crmc/cdb/prog_pbhp/index.cfm. Accessed 14 October 2016
Tremblay MS, LeBlanc AG, Kho ME, Saunders TJ, Larouche R, Colley RC et al (2011) Systematic review of sedentary behaviour and health indicators in school-aged children and youth. Int J Behav Nutr Phys Act 8:98
TN Department of Education. State report cards. https://www.tn.gov/education/topic/report-card. Accessed 30 June 2017
Ayers K, Villalobos A, Li Z, Krasin M (2016) The St. Jude Cancer Education for Children Program pilot study: determining the knowledge acquisition and retention of 4th-grade students. J Cancer Educ 31:26–30. https://doi.org/10.1007/s13187-014-0752-5
Ayers K, Li Z, Quintana Y, Villalobos AVK, Klosky JL (2016) St. Jude Cancer Education for Children Program: the impact of a teacher-led intervention on student knowledge gains. J Cancer Educ 32:808–813. https://doi.org/10.1007/s13187-016-1010-9
Ajzen I (1991) The theory of planned behavior. Organ Behav Hum Decis Process 50(2):179–211
Rosenstock IM (1974) The health belief model and preventive health behavior. Health Educ Monogr 2(4):354–386
Sheeran P, Maki A, Montanaro E, Avishai-Yitshak A, Bryan A, Klein WMP, Miles E, Rothman AJ (2016) The impact of changing attitudes, norms, and self-efficacy on health-related intentions and behavior: a meta-analysis. Health Psychol 35(11):1178–1188 ISSN 0278-6133
Glanz K, Rimer BK, Viswanath K (2008) Health behavior and health education: theory, research, and practice. 465–82. Jossey-Bass, San Francisco
World Health Organization. (2006). Food and nutrition policy for schools. http://www.euro.who.int/__data/assets/pdf_file/0019/152218/E89501.pdf?ua=1. Accessed 15 March 2016
World Health Organization. (2008). School policy framework: implementation of the WHO global strategy on diet, physical activity and health. http://www.who.int/dietphysicalactivity/SPF-en-2008.pdf?ua=1. Accessed 15 March 2016
Acknowledgments
We thank the St. Jude Children’s Research Hospital International Outreach Program.
Funding
This study was funded by the American Lebanese and Syrian Associated Charities (ALSAC) of St. Jude Children’s Research Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights
This study was reviewed and approved by the St. Jude Children’s Research Hospital Institutional Review Board for Human Subjects Research and therefore was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All classroom teachers and parents of students gave their informed consent prior to their inclusion in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Ayers, K., Klosky, J., Li, Z. et al. Evaluation of the St. Jude Cancer Education for Children Program on Cancer Risk Awareness, Attitudes, and Behavioral Intentions Among Fourth-Grade Science Students: Comparisons Between Racially Identifiable/High-Poverty Schools and Racially Diverse/Affluent Schools. J Canc Educ 35, 380–387 (2020). https://doi.org/10.1007/s13187-019-1476-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-019-1476-3