Abstract
Introduction
Medical toxicology expertise has expanded into the addiction medicine realm including outpatient medication for opioid use disorder (MOUD) and addiction treatment. Concomitantly, the emergency department (ED) and hospital are increasingly seen as important sites for the screening, prevention, and treatment of patients with substance use disorders and addiction. This analysis seeks to characterize patients seen by medical toxicologists for opioid use and opioid use disorder (OUD) in the ED and inpatient consultation setting (inpatient) versus in the OUD clinic (outpatient) setting.
Methods
We searched the American College of Medical Toxicology’s Toxicology Investigators Consortium Case Registry, a prospective, de-identified, national dataset that includes patients receiving medical toxicology consultation following prescription opioid misuse. The dataset also includes patients seen in outpatient MOUD clinics during the same period between June 2013 and November 2015. Intentional self-harm patients were excluded. We analyzed medical history, drug use patterns, and other factors with odds ratios and confidence intervals.
Results
Of 110 patients identified, 60 (54.5%) were inpatients and 50 (45.5%) outpatients. Mean age (39 years), gender (68% male), and race breakdown (60% white/non-Hispanic) were similar. The outpatient group was more likely to have Medicare/Medicaid coverage (p<0.0001). By history, the outpatient group was more likely to have past alcohol misuse, intravenous drug use, prescription drug misuse, and prescription opioid misuse. Most inpatient group members sought a recreational high compared to avoiding withdrawal or treating dependence in the outpatient group.
Conclusion
Patients treated in the outpatient compared to inpatient setting were more likely to report adverse sequelae from their drug use including long-term drug use, depression, previous rehabilitation attempts, and seeking to avoid withdrawal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Opioids are common causes of overdose and are the most common cause of lethal overdose in the USA [1, 2]. The origins and evolution of the opioid epidemic and associated public health problems are complex and multifactorial. They range from a variety of public health and social factors including changing jobs and opportunities, the focus on pain as a “vital sign” with incentivization for treating pain, pharmaceutical company bias and misrepresentation of research related to the efficacy of opioids and potential for addiction, increase in opioid prescribing and availability, and the broad accessibility of heroin. The replacement of heroin with synthetic opioids, in particular fentanyl, has been one of the more recent and ominous trends as it has fueled unprecedented rates of fatal overdose [3, 4]. Some risk factors for opioid overdose are known such as co-prescription with benzodiazepines, alcohol or other sedatives, use of higher doses of opioids such as more than 50 morphine milligram equivalents per day, and certain concurrent mental health comorbidities or psychiatric disorders [5,6,7,8,9]. Other risks are less well characterized.
Opioid overdoses often occur in the context of patients developing an opioid use disorder (OUD) which, like many other chronic diseases, generally follows a relapsing and remitting course [10, 11]. Modern efforts to mitigate harms associated with opioid use and to treat OUD in particular began with the use of methadone in the early 1970s [12]. In 2000 the Congress passed the Drug Addiction Treatment Act (DATA 2000) which created an “X-waivered” certification process for physicians to become certified to prescribe specifically defined controlled substances to treat opioid dependence in an office-based setting, a place where a growing sector of the medical toxicology community practices [13, 14]. Subsequent amendments to DATA 2000 specified buprenorphine formulations and increased the number of patients X-waivered physicians who could treat first to 100 and subsequently to 275. More recently X-waiver certification was made available to nurse practitioners and physician assistants [15]. In April 2021, the US Department of Health and Human Service (HHS) enacted a new policy so that eligible DEA-registered providers could submit a Notice of Intent to the Substance Abuse and Mental Health Services Administration that they intended to treat OUD with buprenorphine for up to 30 patients. With this patient limit, the practitioner did not need to certify as to the training, counseling, or other ancillary services required under previous X-waiver regulations and certification [16].
Medical toxicologists are physicians specially trained to evaluate and treat patients suffering from the adverse effects of exposure to chemical substances, including medications. In response to the opioid epidemic, the scope of medical toxicology practice has expanded, particularly related to using buprenorphine to manage OUD [14, 17]. This scope of practice includes the treatment of substance use disorder (SUD) and addiction in the emergency department (ED) and inpatient units (together constituting the “inpatient” cohort), as well as the outpatient clinics (“outpatient” cohort). Nearly 8% of all currently board-certified medical toxicologists are also certified in addiction medicine [18].
In this study, we compared patients seen by medical toxicologists in the ED and hospital setting (“inpatient”) when the primary drug involved was a prescription opioid to patients seen in an outpatient clinic setting for the treatment of OUD. We described the opioids involved in each encounter and compared characteristics of inpatient and outpatient populations using data obtained from a well-established, prospective case registry.
Methods
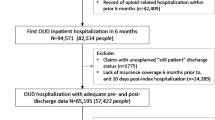
The Toxicology Investigators Consortium (ToxIC) Case Registry is a prospective national database of patients evaluated by toxicologists and has been described in detail previously [19, 20]. A focused subregistry was created to collect prospective, de-identified data related specifically to the clinical presentation and management of patients with prescription opioid misuse from June 2013 to November 2015 (see Appendix. ToxIC Prescription Opioid Misuse Subregistry Data Requested).
The subregistry inclusion criterion was treatment for prescription opioid misuse on that visit. We specifically defined prescription opioid misuse in the subregistry as the intentional inappropriate consumption of legal opioids for both medical and nonmedical reasons. It included taking more than the prescribed amount of opioid, taking them in a different manner than prescribed (e.g., crushing a tablet and then nasally insufflating or intravenously injecting), taking drugs prescribed for someone else, combining the pills with alcohol or other drugs, using the substance recreationally to achieve euphoria, or to prevent withdrawal [21,22,23]. Patients were excluded if the encounter involved an attempt at intentional self-harm or unintentional ingestions. Short-term use was defined as less than or equal to 30 days, while longer periods were referred to as long-term use. Naloxone dispensing was not tracked during this study period, and we did not differentiate between prescribed and non-prescribed buprenorphine.
Patients who incurred a complication following prescription opioid misuse and received a medical toxicology consultation were evaluated in either of two settings—in the ED/hospital setting or in an outpatient toxicology or OUD clinic (where the toxicologist saw patients in an outpatient setting). We designated the hospital-based evaluation group as “inpatient” since they were more acutely ill and were treated in a higher acuity setting, even though they may not have been admitted to the hospital. We did not distinguish between patients who were admitted or discharged in the inpatient group. Additionally, distinguishing ED from inpatient consultations is often simply related to timing of consultation and billing code, and unless specifically described as ED only in the registry, a patient seen in ED could have been admitted and had subsequent visits performed by a toxicologist.
In contrast, some patients included in the database were evaluated in the outpatient OUD pharmacotherapy clinics (designated as “outpatient”). Most patients had appointments scheduled in advance, while others were seen as referrals from the ED or hospital or other settings. The referral source, to this level, was not included for these cases in the ToxIC Registry, but there were some walk-in patients. In the outpatient OUD clinic, medical toxicologists assessed, treated, and followed all patients presenting for OUD. Outpatients were entered in the subregistry at their initial clinic presentation. Subsequent visits for continuing therapy were not included in the database. The clinic patients may or may not have had a complication requiring hospitalization in the past, but the clinic visit was related to the treatment of OUD.
All patients were evaluated by a board-certified or board-eligible medical toxicologist in both the inpatient and outpatient settings that were participating practice sites in the ToxIC Case Registry. Variables of interest encompassed patient demographics, past medical history, past and present drug use, drug source, providers’ use of their state prescription drug monitoring program (PDMP) database, and diversion patterns. For categorical data, descriptive statistics included proportions. We also used Pearson’s chi-square test of independence to determine associations and odds ratios. Odds ratios (OR) and confidence intervals (CI) are expressed as the more prevalent group compared to the less prevalent group for each characteristic. OR are significant when the CI do not contain the number one. OR were not calculated when one of the comparisons had zero respondents. Data analysis was conducted using R statistical software v3+ (Vienna, Austria).
Sites participating in the ToxIC Registry contributed cases following the permission of their respective IRB and in accordance with their policies and procedures. The Registry has also been reviewed and approved (exempt status) by the Western Institutional Review Board.
Results
One hundred and ten cases were identified in the ToxIC Prescription Opioid Misuse Subregistry comprising 60 (55%) inpatients and 50 (45%) outpatients. Patient demographic comparisons including housing and insurance status are shown in Table 1, with odds ratios and confidence intervals expressed as the more prevalent group compared to the less prevalent group for each characteristic (Appendix).
Table 2 presents the patients’ past medical history, drug use and treatment history, and the specific drug and reason for the patients’ first opioid use or exposure. Table 3 shows patient data for the current ED or SUD clinic visit, while Table 4 describes the patients’ current illicit drug use.
For the outpatient group, PDMP data were available in 100% of cases, accessed in 88%, and something was included in the PDMP report in 84%. The PDMP data were not included as a question for the inpatient group as this is a routine component of inpatient care and medication reconciliation (or at least during the time of data entry it was not common).
Discussion
In 2018 the ToxIC Registry added data collection fields specifically to evaluate the care of patients with substance use disorders. This expanded data collection related to the treatment of SUD and addiction well beyond what had previously been included in the prescription opioid misuse registry. The 2019 Annual Report summarized these data including describing an overall increase from 244 cases reported in 2018 to 476 cases reported in 2019, where addiction was the primary reason for consultation. The majority of these arose from inpatient or admitting units with 323 (69%), followed by the ED with 142 (30%). Initiation of MOUD was the most common reason for consultation (62%), followed by pain management (18%), counseling (9%), and initiation of pharmacotherapy for alcohol use disorder (7%) [20]. Our data from 2013 to 2015 represent an earlier period of the opioid epidemic and also a time when fewer medical toxicologists were focusing on the treatment of substance use disorders and addiction.
We describe different characteristics between the inpatient and outpatient groups of patients being treated for OUD despite similar demographics. The outpatients were characterized as having more depression, longer duration of substance use disorder, prior treatment for both alcohol and drug dependence, use of buprenorphine, heroin, and opioids, as well as using to avoid or to treat withdrawal symptoms. They also had an increased rate of unemployment but were more likely to have insurance, most commonly Medicaid. Many of these characteristics may simply reflect the natural trajectory of addiction and initiation of MOUD and initiation into treatment, as well as the adverse sequelae of a SUD and addiction. They also emphasize the broad framework of social, medical, and other factors to consider in treating patients with OUD, and addictions in general.
Fifty percent of the inpatient group had a current prescription for the opioid used in relation to their inpatient encounter in contrast to only 19% of the outpatient cohort. Furthermore, the inpatient group frequently cited chronic pain and initial use for back pain as reasons for opioid use. The most common opioids used were oxycodone and methadone (Table 3). Despite reporting initial opioid use for the treatment of pain, at the time of the inpatient encounter, 86% met criteria for diagnosis of OUD and had high rates of recreational use as the reason for the encounter. Thus, the inpatient group may simply represent an earlier point in a continuum of OUD compared to the outpatient group. This emphasizes the importance of screening patients for substance use disorders and initiating potentially life-saving treatment, such as initiating buprenorphine and/or dispensing naloxone and arranging appropriate outpatient continuity, while patients are still in the inpatient setting. The inpatient encounters reflect both an opportunity to intervene and to offer treatment, as well as to mitigate ongoing risk of recurrent overdose and other adverse effects of continued use.
A large number of our outpatient group were using buprenorphine in an attempt to self-treat or avoid withdrawal prior to seeking outpatient treatment or entering a program. Other research has suggested that these patients have good success with prescribed buprenorphine as they are familiar with the medication and may have a greater motivation to succeed or readiness to change [24]. Self-treatment of withdrawal with buprenorphine is less likely to result in a complication requiring hospitalization, and as buprenorphine is generally a much safer opioid than those most commonly prescribed for pain (e.g., oxycodone or hydrocodone), it is not surprising that the inpatient group did not frequently identify buprenorphine use prior to their admission [25].
Further, enhancing access to care with rapid initiation of treatment with MOUD and other supports is important for taking advantage of any readiness for change.
Several studies have previously shown that patients using illicit buprenorphine have primary motivation for buprenorphine use to reduce opioid craving, decrease withdrawal symptoms, maintain functionality, and save money prior to seeking treatment for their OUD [26]. Prior experience with buprenorphine has also been shown to correlate with positive outcomes with prescribed buprenorphine and during treatment in general [27]. The awareness that much of the illicit buprenorphine is used to self-treat withdrawal and dependence is not new; however, in recent years, it has become increasingly common to encounter patients using alternative opioids, non-controlled medications, and herbal or plant products such as kratom, gabapentin, and high-dose loperamide, to prevent drug cravings and withdrawal symptoms with their associated risks [28,29,30]. For these patients, rapid and easy access to care is an important factor in receiving the most appropriate and effective treatments for OUD such as methadone or buprenorphine [31].
Medical toxicologists are well-suited to take on an expanded role in assisting with the screening, prevention, and treatment of patients with SUD and addiction, particularly the treatment of OUD. By initiating and supporting ongoing treatment with MOUD—starting with the early identification of patients in the ED and hospital setting to treatment in the outpatient clinic—they are fulfilling a critical need at the individual institution setting and for the broader public health. Many groups, including the National Academy of Medicine, strongly recommend removing barriers to providing MOUD [15, 32, 33].
The differences noted between the inpatient and outpatient groups may inform on new approaches to treatment and should be further characterized. For the inpatient group, this may include overdose prevention with naloxone kits, overdose prevention education, MOUD initiation when appropriate, and linkage to social/behavioral services including mental health support. Specifically, in recent years, Recovery Coaches, Peer Counselors, and embedded Credentialed Alcoholism and Substance Abuse Counselors have been utilized by some of our colleagues in both the inpatient and outpatient setting. Cross training in addiction medicine or adding exposure to these ancillary services, including novel ways of connecting with patients (e.g., telemedicine use), is increasingly critical. Key interventions for the outpatient group include ongoing stabilization, relapse prevention, referral or addressing mental health needs, and primary care linkage.
Limitations
Our study has several limitations. First, we realize that the sample size may limit the generalizability of our findings to all practice settings. Our data reflect the clinical experience specific to medical toxicologists. Second, incomplete datasets limit applicability and utility; however, medical toxicologists with a high degree of knowledge and experience regarding SUDs performed the consultations and collected the data firsthand. Given that some states had not implemented a PDMP during this period, some requested data were not gathered, including PDMP data on inpatients. Whether a PDMP was queried, however, was included, but not the findings. Also, we did not ask if outpatient clinic therapy required insurance, which may have affected the results.
This analysis included only programs with medical toxicologists which may limit the generalizability of the findings. However, the ToxIC Registry receives data from a representative sample of over 50 healthcare facilities across the USA, increasing the potential for a broad array of data. Next, patients presenting to an emergent (inpatient) setting may reasonably be expected to possess different characteristics than those seen in an outpatient clinic. Specifically, what these differences are, however, is not clear. Identifying similarities and differences may ascertain opportunities to focus resources on and discover areas to research more in-depth, as well as mitigate additional adverse consequences of opioid use and the opioid epidemic overall. Further, the data are not completely verifiable. Even having trained medical toxicologists eliciting the information may limit the generalizability of the data.
Although the data were collected during 2013–2015 and pre-date some changes and interventions that have occurred in the USA and elsewhere, the opioid epidemic continues unabated with tens of thousands of deaths annually. The data generated here are still relevant, however, as factors associated with buprenorphine use in particular, an increasingly prescribed MOUD in a variety of settings, are useful for generating further hypotheses to guide better overall patient treatment and support. Also, as the hospital increasingly is utilized to begin treatment and support, including MOUD initiation, information on patients presenting related to opioid use is particularly relevant.
Conclusion
We found notable differences between patients seen in inpatient settings and outpatient clinics related to prescription opioid misuse. These differences may inform on new approaches to treatment and should be further characterized. Interventions could include overdose prevention education and naloxone kits for inpatients and other supports for treatment retention in the outpatients.
References
O'Donnell J, Gladden RM, Mattson CL, Hunter CT, Davis NL. Vital signs: characteristics of drug overdose deaths involving opioids and stimulants - 24 states and the district of Columbia, January-June 2019. MMWR Morb Mortal Wkly Rep. 2020;69(35):1189–97.
Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67(5152):1419–27.
CDC. (2019) Opioid overdose. Understanding the epidemic: CDC; [Available from: https://www.cdc.gov/drugoverdose/epidemic/index.html. Accessed 10 Jun 2021
Hedegaard H, Minino AM, Warner M. Drug overdose deaths in the United States, 1999-2017. NCHS Data Brief. 2018(329):1–8.
CDC. (2018) Calculating total daily dose of opioids for safer dosage. [Available from: https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf. Accessed 10 Jun 2021
Organization WH. (2018) Information sheet on opioid overdose: World Health Organization; [Available from: https://www.who.int/substance_abuse/information-sheet/en/. Accessed 10 Jun 2021
Dilokthornsakul P, Moore G, Campbell JD, Lodge R, Traugott C, Zerzan J, et al. Risk factors of prescription opioid overdose among Colorado Medicaid beneficiaries. J Pain. 2016;17(4):436–43.
Babu KM, Brent J, Juurlink DN. Prevention of opioid overdose. N Engl J Med. 2019;380(23):2246–55.
Krawczyk N, Eisenberg M, Schneider KE, Richards TM, Lyons BC, Jackson K, et al. Predictors of overdose death among high-risk emergency department patients with substance-related encounters: a data linkage cohort study. Ann Emerg Med. 2020;75(1):1–12.
HHS.Gov/opioids. HHS; [Available from: https://www.hhs.gov/opioids/about-the-epidemic/index.html. Accessed 10 Jun 2021
Administration SAaMHS. (2005) substance abuse treatment for persons with co-occurring disorders Treatment Improvement Protocol (TIP) Series, No. 42. In: SAMHSA H, editor. Rockville, MD: Substance Abuse and Mental Health Services Administration; p. 577.
Sullivan LE, Fiellin DA. Narrative review: buprenorphine for opioid-dependent patients in office practice. Ann Intern Med. 2008;148(9):662–70.
Samhsa H. (2018) Buprenorphine waiver management: SAMHSA; [Available from: https://www.samhsa.gov/medication-assisted-treatment/training-materials-resources/apply-for-practitioner-waiver. Accessed 10 Jun 2021
Herring AA, Perrone J, Nelson LS. Managing opioid withdrawal in the emergency department with buprenorphine. Ann Emerg Med. 2019;73(5):481–7.
Marino R, Perrone J, Nelson LS, Wiegand TJ, Schwarz ES, Wax PM, et al. ACMT position statement: remove the waiver requirement for prescribing buprenorphine for opioid use disorder. J Med Toxicol. 2019;15(4):307–9.
Becerra B (2021) Practice guidelines for the administration of buprenorphine for treating opioid use disorder. In: Services HaH, editor. Federal Register: National Archives; p. 22439-40.
A. G. The Treatment Gap. New York Times. 2018.
Carpenter JE, Murray BP, Mazer-Amirshahi M, Laes JR, Nacca N, Nelson LS, et al. Leadership roles in opioid stewardship and the treatment of patients with opioid use disorder among medical toxicologists. J Med Toxicol. 2020;16(2):204–11.
Wax PM, Kleinschmidt KC, Brent J, Investigators ATCR. The Toxicology Investigators Consortium (ToxIC) Registry. J Med Toxicol. 2011;7(4):259–65.
Spyres MB, Farrugia LA, Kang AM, Aldy K, Calello DP, Campleman SL, et al. The Toxicology Investigators Consortium Case Registry-the 2019 Annual Report. J Med Toxicol. 2020;16(4):361–87.
Katz NP, Adams EH, Chilcoat H, Colucci RD, Comer SD, Goliber P, et al. Challenges in the development of prescription opioid abuse-deterrent formulations. Clin J Pain. 2007;23(8):648–60.
Nelson LS, Paulozzi LJ. The toxicology Tower of Babel: why we need to agree on a lexicon in prescription opioid research. J Med Toxicol. 2012;8(4):331–2.
Tetrault JM, Butner JL. Non-medical prescription opioid use and prescription opioid use disorder: a review. Yale J Biol Med. 2015;88(3):227–33.
Cunningham CO, Roose RJ, Starrels JL, Giovanniello A, Sohler NL. Prior buprenorphine experience is associated with office-based buprenorphine treatment outcomes. J Addict Med. 2013;7(4):287–93.
Cicero TJ, Surratt HL, Inciardi J. Use and misuse of buprenorphine in the management of opioid addiction. J Opioid Manag. 2007;3(6):302–8.
Schuman-Olivier Z, Albanese M, Nelson SE, Roland L, Puopolo F, Klinker L, et al. Self-treatment: illicit buprenorphine use by opioid-dependent treatment seekers. J Subst Abus Treat. 2010;39(1):41–50.
Kenney SR, Anderson BJ, Bailey GL, Stein MD. Buprenorphine treatment formulations: Preferences among persons in opioid withdrawal management. J Subst Abus Treat. 2018;94:55–9.
Borron SW, Watts SH, Tull J, Baeza S, Diebold S, Barrow A. Intentional misuse and abuse of loperamide: a new look at a drug with “low abuse potential”. J Emerg Med. 2017;53(1):73–84.
Goodman CW, Brett AS. Gabapentin and pregabalin for pain - is increased prescribing a cause for concern? N Engl J Med. 2017;377(5):411–4.
Vakkalanka JP, Charlton NP, Holstege CP. Epidemiologic trends in loperamide abuse and misuse. Ann Emerg Med. 2017;69(1):73–8.
Alford DP, LaBelle CT, Kretsch N, Bergeron A, Winter M, Botticelli M, et al. Collaborative care of opioid-addicted patients in primary care using buprenorphine: five-year experience. Arch Intern Med. 2011;171(5):425–31.
Wax PM, Stolbach AI, Schwarz ES, Warrick BJ, Wiegand TJ, Nelson LS. ACMT position statement: buprenorphine administration in the emergency department. J Med Toxicol. 2019;15(3):215–6.
(2019) Medications for opioid use disorder save lives. Mancher AILaM, editor. Washington, DC: National Academies Press. 156 p.
Sources of Funding
None
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of Interest
None
Additional information
Supervising Editor: Leslie R. Dye, MD
Prior Presentation: Data in this study were presented as an abstract (A Descriptive Study of Prescription Opioid Misusers Evaluated by Medical Toxicologists) and poster (Inpatient compared to outpatient prescription opioid misusers – What’s the difference?) at the 2015 ACMT Annual Scientific Meeting, March 27–29, 2015 at Clearwater Beach, FL.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 73.7 KB)
Rights and permissions
About this article
Cite this article
Varney, S.M., Wiegand, T.J., Wax, P.M. et al. Descriptive Analysis of Inpatient and Outpatient Cohorts Seeking Treatment After Prescription Opioid Misuse and Medical Toxicology Evaluation. J. Med. Toxicol. 17, 378–385 (2021). https://doi.org/10.1007/s13181-021-00850-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-021-00850-7