Abstract
The opioid epidemic is a major public health challenge and physicians in medical settings must be equipped to identify and manage opioid use disorder (OUD). Nearly 20% of hospitalized patients have a substance use disorder (SUD) and it’s estimated that 44% of illicit drug users may actively continue to use substances while admitted. Unidentified and untreated substance use in hospitalized patients can result in overdose, withdrawal, other negative medical sequelae, and is linked to patients leaving against medical advice. Patients may not disclose substance use to clinicians due to fear of stigmatization or negative unforeseen consequences. Clinicians must screen all admitted patients for SUD with a comprehensive history, physical examination, and appropriate laboratory tests and urine toxicology when indicated. Repeat urine toxicology and clinical assessments may be needed throughout hospitalization in cases where there is ongoing substance use. Differentiating between various substance intoxication and withdrawal presentations is important to avert potential negative medical outcomes. Opioid overdose requires acute medical intervention and these individuals are high risk for repeat overdose and should be started on MOUD when feasible prior to discharge from the inpatient setting. Acute opioid withdrawal should be managed using clinical assessment tools and medications including opioid agonists, alpha-2 adrenergic agonists, and other supportive medications. Management of opioid withdrawal alone is not treatment for individuals with OUD and patients should be started on MOUD and linked with outpatient treatment. New rapid-induction protocols for buprenorphine and naltrexone are becoming more established and feasible in inpatient settings. Methadone can also be started while inpatient although availability of outpatient treatment at a federally certified opioid treatment program may be limited. All individuals with OUD or other SUDs should receive a naloxone kit and linked with outpatient treatment prior to discharge from the inpatient setting. Early identification and management of OUD and other SUDs during acute hospitalization improves medical outcomes and reduces overdose deaths.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Opioid use disorder
- Substance use disorder
- Opioid withdrawal
- Opioid overdose
- Urine toxicology
- Stigmatization
- Buprenorphine
- Methadone
- Naltrexone
- Naloxone
34.1 Introduction
Nearly 20% of hospitalized patients have a substance use disorder (SUD) [1, 2]. Opioid use disorder (OUD) is commonly encountered in hospitalized patients with increasing prevalence amongst the opioid epidemic. Over two million individuals meet criteria for OUD and ten million people misused opioids in the past year [3]. Hospitalized patients with OUD are more likely to have negative medical outcomes and leave without completing treatment against medical advice [4].
Patients may not disclose ongoing substance use while inpatient for various reasons including fear of stigmatization and unforeseen consequences. Providers must be equipped to address OUD while inpatient and reduce these fears of stigmatization through reassurance that disclosure of substance use will not negatively impact medical care. Comprehensive evaluations and screening for OUD or other SUDs should be done in a nondiscriminatory manner and with intent of optimizing medical care and providing evidence-based OUD treatment.
Initiating evidence-based treatment for OUD in the acute hospital setting is feasible and effective [5,6,7,8,9] and results in better medical and substance use disorder outcomes [6, 8]. Currently there are three FDA-approved medications for OUD: methadone, buprenorphine, and extended-release injectable naltrexone. All patients with OUD not on pharmacologic management should be recommended one of these treatment options while inpatient and connected with outpatient substance use treatment [10,11,12,13]. Without substance use treatment, the majority of individuals will return to substance use upon discharge and are at high risk for poor outcomes and opioid overdose [14, 15]. Engaging patients in treatment for OUD while inpatient improves outcomes for some of the highest risk individuals [7].
This chapter will review best management strategies for identifying opioid misuse or OUD, opioid overdose, acute withdrawal, initiating medications for opioid use disorder (MOUD) while inpatient, and connecting inpatients with substance use treatment prior to discharge.
34.2 Why Do Patients Not Disclose Substance Use?
Patients may decide to not disclose substance use for various reasons. Patients with SUDs may expect to be treated negatively by healthcare providers based on previous experiences in medical settings. They may withhold information from providers for fear of stigmatization, negative reactions, and unforeseen consequences. These fears are not unfounded as studies have shown that providers often possess negative attitudes and feel ill equipped in managing patients with SUDs [16,17,18,19,20,21,22].
Patients may also have concerns about confidentiality of the medical record and disclosure of substance use potentially impacting their job, insurance payments, medical care, and providers’ willingness to prescribe some medications including controlled substances such as opioid analgesics for pain conditions [16]. For instance, patients with opioid use disorder (OUD) on opioid agonist treatment (methadone or buprenorphine) fear a reduction in dosing or that their pain will be undertreated in an acute medical setting [20, 21]. This is often based on previous interactions with providers who believe prescribing opioids for pain will increase the risk of relapse or worsen addiction [23, 24]. There is no evidence that exposure to opioid analgesics in the presence of pain increases relapse in patients on opioid agonist treatment [20, 25, 26]. Patients are more likely to relapse or access opioids analgesics from external sources when their pain is undertreated, and may resort to illicit substance use while inpatient [27, 28].
Aside from fear of stigmatization, patients may not be ready to disclose substance use, accept diagnosis of a SUD, or be motivated to start treatment. Motivation to change substance use behavior is an important component of the recovery process and therapeutic interventions exist to enhance motivation such as motivational interviewing [29]. In some cases, hospitalized patients may use substances to avoid acute withdrawal and do not disclose this to their provider. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) characterizes a substance use disorder by a pronounced craving and preoccupation for the substance, inability to refrain from using it, and escalation of use despite negative consequences [30]. Patients that do not disclose opioid use carry risk for overdose while inpatient. Those at greatest risk are perhaps those who do not disclose prior opioid use and are not using opioids while inpatient. These individuals have decreased tolerance and are at increased risk of opioid overdose upon discharge [12].
Providers can reduce fear of stigmatization through reassurance that disclosure of substance use will not negatively impact medical care or prevent adequate pain management. History-taking and screening for SUDs should be done in a nondiscriminatory manner and with intent of optimizing medical care and providing evidence-based SUD treatment. Choice of substance use treatment, in particular initiating medication for opioid use disorder (MOUD), should be a shared decision between the patient and clinician. MOUD includes buprenorphine, methadone, and extended-release injectable naltrexone. More providers should be trained in screening for SUDs and delivering treatment so that providers feel more equipped to manage patients with SUDs and have improved attitudes overall [11, 12].
34.3 Management of Acute Opioid Withdrawal
34.3.1 Opioid Withdrawal Syndrome
Opioid withdrawal syndrome refers to a range of symptoms that occur after stopping or dramatically reducing the dose of opioids after prolonged use. Opioid withdrawal symptoms include mydriasis, lacrimation, rhinorrhea, diaphoresis, nausea, vomiting, abdominal cramps, diarrhea, piloerection, muscle pain, and anxiety [10, 13]. Common signs of opioid withdrawal can be seen in Table 34.1. Withdrawal symptoms emerge within 12 h of the last dose of short-acting opioids such as heroin and within 30 h of the last long-acting opioid such as extended-release oxycodone. Withdrawal symptoms generally persist anywhere from 3 to 5 days for short-acting opioids and 10 days for long-acting opioids [13]. The duration of withdrawal symptoms can be influenced by patient factors including age, duration of opioid exposure, type of opioid, physical condition and medical comorbidities [12].
Withdrawal states can be particularly challenging for patients with comorbid psychiatric and pain conditions. Patients with comorbid psychiatric disorders in opioid withdrawal may experience an exacerbation of psychiatric symptoms such as dysphoria, anxiety, difficulty sleeping, suicidality, and irritability [12, 13]. Patients with comorbid pain conditions may experience worsening pain when in opioid withdrawal and request additional pain medication. Distinguishing between pain from a pre-existing condition and pain related to opioid withdrawal can be difficult. Clinicians must correlate perceived pain with diagnostic work-up and clinical findings related to medical condition, as well as duration and quantity of opioid use prior to hospitalization [11].
Opioid withdrawal states may be spontaneous or precipitated by medication. Spontaneous withdrawal occurs with cessation of opioid use or dramatic reduction in opioid dosing. Precipitated withdrawal states can occur when an opioid-tolerant patient receives an opioid antagonist (naloxone or naltrexone) or the partial opioid agonist buprenorphine. Buprenorphine has a high affinity for the mu-opioid receptor relative to other opioids and can precipitate withdrawal. Precipitated opioid withdrawal states can be severe and require further inpatient management, particularly in cases where fentanyl and other high potency synthetic analogs are in heroin supplies. The time for maximal precipitated withdrawal occurs varies between agents and can be seen in Table 34.2 [12].
There are various clinical scenarios where an inpatient may enter an opioid withdrawal state and several examples are listed in Table 34.3. Many opioid-tolerant patients administered naloxone will enter an acute opioid withdrawal state that requires management. Patients admitted medically with opioid use disorder may be interested in starting buprenorphine prior to discharge and will need to enter a state of mild-moderate opioid withdrawal before induction. Opioid use outside of the hospital might be difficult to quantify for some patients, increasing risk of both withdrawal and overdose. In cases where a patient is incidentally found to be in acute opioid withdrawal without prior report of opioid-dependence, a thorough evaluation and history should be obtained before starting opioid agonists. This also presents the opportunity to engage patients with OUD in treatment and potentially start MOUD while inpatient. Initiating MOUD is discussed in further detail in this chapter.
Opioid withdrawal is rarely life threatening but if untreated can lead to negative patient outcomes. Patients may leave against medical advice to obtain opioids to treat the withdrawal or succumb to opioid cravings [31]. These patients are at risk for poor medical outcomes with abbreviated medical intervention. The opportunity to engage the patient in treatment for OUD and start pharmacotherapy is also lost in these settings. Opioid withdrawal management is critical in mitigating risk for negative medical sequelae, opioid overdose, and death. Opioid withdrawal management alone though is not considered effective treatment of opioid use disorder given high rate of relapse [32]. Patients should be offered standard treatment with MOUD and be connected with outpatient providers and appropriate psychosocial interventions.
34.3.2 Assessment of Opioid Withdrawal
Assessment of a patient in opioid withdrawal should include a comprehensive medical history and physical examination. There are scales to assess opioid withdrawal listed below. Objective signs are more reliable than subjective when available, although both are valuable and can be done in conjunction. These scales can be administered on initial assessment and intermittently when treating opioid withdrawal [10,11,12].
-
1.
Objective Opioid Withdrawal Scale (OOWS) is an objective measure where the clinician assesses for 13 signs of opioid withdrawal [33].
-
2.
Clinical Opioid Withdrawal Scale (COWS) is a clinical assessment for 11 medical signs of opioid withdrawal [34].
-
3.
Subjective Opioid Withdrawal Scale (SOWS) is a measure of 16 subjective symptoms of withdrawal reported by the patient on a five-point scale [33].
34.3.3 Medications in Opioid Withdrawal
Withdrawal symptoms can be managed with alpha-2 adrenergic agonists (clonidine, lofexidine, and dexmeditomidine), antidiarrheal medications, anxiolytics, and sleep aids [10,11,12]. Opioid agonists can be administered or standing opioid doses increased to target withdrawal symptoms. Clinical judgment and objective assessment of withdrawal symptoms is recommended before adjusting opioid regimen or considering initiation of an opioid agonist (methadone or buprenorphine) for dual management of pain and OUD. Referral to a pharmacologically managed detoxification program may be needed following inpatient medical hospitalization.
34.3.3.1 Opioid Agonists
Methadone and buprenorphine are both recommended in opioid withdrawal management. The use of either is more complex in inpatient cases with OUD on concurrent acute pain management regimens. Patients on standing opioids other than buprenorphine or methadone for pain incidentally found to have OUD should be transitioned to MOUD when feasible.
If a patient is already on methadone or buprenorphine, dosing can be adjusted to target opioid withdrawal symptoms and pain concurrently. For patients on methadone for pain and with comorbid OUD, they must be connected with a federally certified opioid treatment program that will provide methadone, which can also be a barrier to treatment if spots are unavailable at the time of discharge. Additionally, these programs often request collaboration in dosing protocols to assure seamless transition to starting doses at the methadone clinic. For patients on buprenorphine for pain and with comorbid OUD, they must be connected with an outpatient provider that has the special waiver to prescribe buprenorphine for OUD. Patients may decline initiation of opioid agonist therapy for comorbid OUD while inpatient and acute withdrawal can be managed with opioid agonists or adjustment in standing opioid regimens as needed per clinical assessments during inpatient stay.
For patients not on standing opioids already, buprenorphine can be started 12–18 h after the last dose of a short-acting opioid such as heroin and 24–48 h after the last dose of a long-acting opioid such as extended-release oxycodone [10]. A dose ranging 4–16 mg per day is generally sufficient to suppress withdrawal symptoms and can be tapered if patient declines to continue as MOUD [10,11,12,13]. Buprenorphine doses may be higher in settings where a patient has used heroin with fentanyl or other high potency synthetic analogs. Methadone can be started in doses ranging 20–30 mg per day. Patients that decline continuation of either opioid agonist should be assessed for appropriateness of discharge to outpatient provider versus referral to detoxification program or substance use rehabilitation program [10,11,12,13].
34.3.3.2 Alpha-2 Adrenergic Agonists
A hallmark feature of opioid withdrawal is the hyperexcitability of the nervous system. Alpha-2 adrenergic agonists directly combat the enhanced noradrenergic tone and are effective in alleviating withdrawal symptoms [35]. Both clonidine and lofexidine are effective in managing opioid withdrawal symptoms. Clonidine has been used off-label for opioid withdrawal management in the United States for years. Lofexidine has been long available in Europe for opioid withdrawal, but only recently approved in the United States in 2018. Lofexidine has a better safety profile and less hypotensive effects than clonidine [36, 37].
Clonidine is generally started at 0.1 mg every 4–6 h for opioid withdrawal and can be increased 0.1–0.2 mg per day up to a maximum of 1.2 mg per day. Lofexidine is started at 0.54 mg every 5–6 h and the dose can be increased daily based on symptoms up to a maximum of 2 mg per day [10, 37]. While administering alpha-2 agonists, blood pressure and heart rate should be closely monitored. Alpha-2 agonists may cause dose-dependent reductions in heart rate and may enhance the AV-blocking effect of beta-blockers. Sinus node dysfunction may also be enhanced [37]. Baseline and regular monitoring of EKG is recommended with risk for QT prolongation, particularly if dosed in conjunction with other QT prolonging agents such as methadone.
Both clonidine and lofexidine are primarily metabolized via the cytochrome P450-2D6 (CYP2D6) enzyme. Medications that inhibit CYP2D6 such as the antidepressant paroxetine can increase the patient’s exposure to lofexidine by as much as 28% and may exacerbate side effects of bradycardia or orthostatic hypotension [38]. Alpha-2 agonists should be tapered and dose decreased gradually before discontinuation to avoid rebound hypertension. Not all opioid withdrawal symptoms are alleviated with alpha-2 agonists and other medications may be indicated [10].
34.3.3.3 Other Medications
Other medications may be needed to alleviate opioid withdrawal symptoms. Benzodiazepines and other anxiolytics can be administered for anxiety. Caution should be used with benzodiazepine dosing in patients with a history of benzodiazepine use disorder and benzodiazepine withdrawal symptoms differentiated from opioid withdrawal symptoms (tremor and more autonomic hyperactivity). Loperamide can be used for diarrhea and ondansetron for nausea or vomiting. Non-opioid analgesics such as acetaminophen and nonsteroidal anti-inflammatory agents (NSAIDs) can be used for muscle aches. Many of these agents cause QT prolongation (ondansetron, alpha2-adrenergic agonists) and regular EKG monitoring is needed particularly in conjunction with other QT-prolonging agents [10,11,12,13].
34.3.4 Opioid Withdrawal in NPO Patients
In certain circumstances, opioid withdrawal will need to be managed in patients not tolerating oral medications. This could be patients with gastrointestinal pathology, upcoming surgery, or impaired mental status. Both methadone and buprenorphine are available as intravenous formulations. Additionally, there is some although limited research supporting use of transdermal clonidine and intravenous dexmedetomidine. Further research will need to be done to determine ideal dosages. Studies done on dexmedetomidine have used doses ranging from 0.5 to 1.4 mcg/kg/h [39].
34.3.5 Anesthesia-Assisted Withdrawal Management
Rapid opioid detoxification with opioid antagonist induction using general anesthesia uses large doses of naloxone to precipitate acute opioid withdrawal. Patients are under general anesthesia and may experience mild withdrawal symptoms for about 6 days upon awakening compared with similar withdrawal symptoms on a 20-day methadone taper [40, 41]. Anesthesia-assisted rapid opioid detoxification is not recommended due to serious complications including cardiac arrest and death [10, 42]. A systematic review of five randomized trials concluded lack of benefit, potential serious harms, and high costs for anesthesia-assisted rapid opioid detoxification [43].
34.4 Management of Acute Opioid Overdose
34.4.1 Presentation
Acute opioid overdose is one of the major concerns when treating a patient found to be using illicit opioids while admitted to the hospital. Miosis, stupor, and respiratory depression are signs suggestive of opioid overdose. Of these the most reliable and most correlated to the need for acute treatment is respiratory depression. Stupor and miosis both have poor specificity. In fact, patient with opioid overdose may have mydriasis in the setting of using multiple other substances [44]. In a monitored setting, the presenting sign of overdose is often hypoxia. In an unmonitored setting, patients may present with varying levels of sedation including comatose and unresponsive.
34.4.2 Naloxone
Naloxone is a competitive opioid mu-receptor antagonist used as an antidote for opioid overdose. In the hospital setting, parenteral administration is often the preferred route although it is also available as intranasal and inhalational formulations. Onset of action is less than 2 min and duration of action is between 20 and 90 min. In patients with opioid tolerance, initial plasma levels are lower and volume of distribution is greater leading to slower onset and longer duration [44].
34.4.3 Acute Management
Initial management of a patient with concern for opioid overdose is supportive. The primary pathophysiology is hypoventilation leading to hypercarbia and hypoxia. Patient should be ventilated with a bag-valve mask with goals to achieve normocarbia and adequate oxygen saturation.
The initial dose of naloxone is 0.04 mg intravenously with a repeat dose of 0.5 mg after 2–3 min if patient does not respond. Subsequent doses after patient responds should be titrated to prevent respiratory depression without precipitating withdrawal in opioid-tolerant patients and/or uncontrolled pain in patients being treated for acute pain. Despite these concerns, priority should be given to ensuring adequate reversal of opioid effects as opioid withdrawal symptoms are rarely life-threatening. Common withdrawal symptoms include diaphoresis, myalgias, vomiting, and diarrhea. The precise dose required depends on the dose and affinity of the competing opioid [44].
34.4.4 Recurrent Respiratory Depression
Patients are at risk for recurrent respiratory depression due to naloxone’s short duration of action relative to most opioids. Additionally, duration of action of opioids can be significantly increased in the setting of an overdose due to altered pharmacokinetics from enzymatic saturation [44]. A through history and physical exam should be performed to identify the causal agent. All transdermal applications should be removed and activated charcoal considered for oral ingestions within the previous hour [44].
Patients who overdosed on short-acting opioids should be monitored closely for at least 4–6 h and potentially discharged after this time frame if they no longer show feature concerning for opioid overdose. Patients who overdosed on long-acting opioids will need to be placed on a naloxone infusion and transferred to an intensive-care unit [44]. The recommended starting infusion rate is 2/3 of that required for initial reversal of respiratory depression per hour [45].
34.4.5 Aspiration Pneumonitis and Pneumonia
Aspiration events such as pneumonitis and pneumonia are the most frequent indications for ICU admission after opioid overdose. About a quarter of patients treated with naloxone went on to have aspiration pneumonitis or pneumonia based on a recently published, large retrospective, cross-sectional study. Patients using multiple substances are at greatest risk as they may develop vomiting from opioid withdrawal from naloxone while still having impaired airway reflexes from other substance use. However, this study showed that only about 3.7% of patients with pulmonary complications had episodes of emesis after administration of naloxone suggesting a majority of aspiration occurs prior to patients receiving medical attention. The study also showed that higher doses of naloxone were correlated with higher risk of pulmonary complications [46]. It is unclear if this is due to patients requiring higher naloxone had a more severe level of intoxication or an inherent causal property of naloxone.
34.4.6 Pulmonary Edema
Pulmonary edema has long been associated with naloxone with incidence estimated to be about 1.1%. Two proposed mechanisms of action are negative pressure pulmonary edema from inspiration against a closed glottis and due to increased permeability from a catecholamine surge in patients who develop opioid withdrawal [46]. However, no study has been able to establish a causal relationship. The aforementioned cross-sectional study suggested that higher doses of naloxone had a higher odds ratio of developing pulmonary edema. However, the study was not able to show statistical significance partly due to the low incidence of this complication. It is unclear if there is a confounding factor implicated in these results as other studies have demonstrated that pulmonary edema also occurs in patients with opioid overdose who never received naloxone [44, 46].
34.5 Assessment of Opioid Use Disorder while Inpatient
34.5.1 Comprehensive Assessment
A comprehensive assessment should be conducted in patients with opioid misuse or opioid use disorder. These patients are likely to have co-occurring medical conditions, psychiatric disorders, and other substance use disorders. Often these individuals are not receiving treatment for both medical and psychiatric comorbidities and are at higher risk for poor outcomes [47].
The medical history should include routine screening for medical conditions with particular attention to hepatitis, HIV, TB, trauma, and IV drug use and related infections [10,11,12,13]. The substance use history should include amount and frequency of current substance use, current treatment, and prior treatments or pharmacotherapies. Patients not already in treatment should be assessed for interest in initiating treatment and offered MOUD while inpatient. A psychosocial assessment can inform what barriers exist to accessing treatment and additional supports offered prior to discharge from the inpatient setting [10].
A thorough pain assessment and history of previous regimens is critical when initiating an inpatient pain regimen. Communication with outpatient pain physicians and review of the Prescription Drug Monitoring Program (PDMP) is helpful in seeing recent controlled substance prescriptions and assessing for any potential misuse. Methadone and buprenorphine prescriptions are not seen in the PDMP and outpatient providers and clinics must be contacted to confirm recent dosing.
34.5.2 Physical Exam
A routine physical examination should be completed on initial presentation and repeated in settings where there is concern for substance use while inpatient. The examination should include assessment for acute intoxication or withdrawal from other substances seen in Table 34.4 [10,11,12,13]. Special attention should be given to current or historical signs of IV drug use. New or old puncture marks may be seen at common injection sites such as the cubital fossa and the forearm [10].
34.5.3 Laboratory Tests
Initial lab testing should include hepatitis serology, HIV with patient’s consent, a complete blood count and liver function tests to assess for infection or liver dysfunction [10]. If clinically indicated, testing for tuberculosis and sexually transmitted infections can be completed. Pregnancy testing should be completed in all women of reproductive age. A baseline electrocardiogram is helpful in assessing for cardiac conditions and QT prolongation as medications for treatment of opioid use disorder can cause QT prolongation. The clinician’s assessment and judgment of each patient case can guide further testing.
34.5.4 Assessment for Substance Use Disorders
Evidence-based screening tools for substance use disorders should be part of the comprehensive assessment. The Substance Abuse and Mental Health Services Administration (SAMHSA) has multiple tools accessible to clinicians [48]. CAGE-AID is a brief four-question screening tool for substance use disorders [49]. Other screening tools include the Opioid Risk Tool and Screening, Brief Intervention, and Referral to Treatment (SBIRT). If a patient screens positive, then the inpatient treatment team should involve psychiatric and addiction specialists during the patient’s hospitalization to provide further interventions and assure outpatient follow-up prior to discharge.
34.5.5 Risk Factors for Opioid Use Disorder and Opioid Overdose
Risk factors to developing OUD include comorbid substance use or psychiatric disorders, suicidal history, prior opioid overdose, long-term opioid therapy and higher daily dosing. Patients are at higher risk for overdose if they are on opioid doses greater than 90-mg morphine equivalents daily and longer-acting opioids, such as methadone and extended-release oxycodone. Concomitant use of alcohol and sedatives such as benzodiazepines and baseline respiratory disease also increase risk of overdose [47, 50]. Prior suicide attempts and intentional or unintentional overdoses are associated with greater risk of overdose [50,51,52,53]. A thorough initial evaluation and history is important for identifying these risk factors and guiding further management. Various risk factors for opioid overdose and developing OUD are discussed in another chapter.
34.5.6 Assessment for Comorbid Psychiatric Disorders
Comprehensive psychiatric assessment is needed in individuals with OUD. Individuals with OUD and opioid misuse are more likely to have co-occurring psychiatric disorders such as depression, anxiety, PTSD, personality disorder, and other substance use disorders [3]. Suicide risk is 16 times greater in those with OUD than that of the general population [53]. Amongst this population about half receive treatment for co-occurring psychiatric and substance use disorders [3]. Psychiatric specialists can initiate treatment for these patients while inpatient including psychopharmacotherapy and psychosocial interventions such as cognitive behavioral therapy (CBT), motivational interviewing (MI), and contingency management (CM) [10,11,12,13]. Psychiatric evaluation can also be helpful in distinguishing primary psychiatric disorders from acute symptoms of dysphoria, anxiety, irritability, and sleep difficulty related to substance withdrawal or intoxication.
34.5.7 Inventory of Patient and Visitor Belongings
Individuals may continue to use substances while hospitalized. This can put them at risk for poor outcomes while inpatient [10, 54]. On initial admission, each patient should have a comprehensive evaluation and part of the substance use assessment should include inquiry of possession of substances or drug paraphernalia. Inventory of the patient or visitor belongings should only be done with the individual’s consent. Individuals presenting to psychiatric settings must comply with full inventory checks and have limitations to certain belongings that may pose risk of harm to self or others and elopement.
In cases where there is concern for substance use while inpatient, a thorough physical examination should first be carried out and assure medical stability in the patient. Assessment should include differentiation between other substance intoxication presentations and potential medical risks [10]. These can be reviewed in Tables 34.1 and 34.4. Future withdrawal presentations should be foreseen and treated.
A patient may not be in agreement with a search of their belongings during a medical hospitalization. Starting the patient on a safety watch can mitigate the risks with ongoing substance use, and those declining a search of their belongings. Visitor restrictions may be needed for those who continue to present to the hospital despite requests to leave and there is ongoing concern for substance possession. Confiscation of substances should be handled as detailed in each hospital policy. The patient is protected under confidentiality rights. Reassurance should be given to the patient that the goal of intervening on substance use is not for punitive or for legal reasons, rather it is for their safety and medical stability.
34.5.8 Urine Toxicology and Drug Testing
Drug testing has become a routine tool for pain physicians to assess patient compliance and comorbid substance use. Common testing samples include blood, urine, hair, saliva, sweat, and nails. Urine has become the most widely used due to its convenience of collection [55]. Until recently, standard practice was sequential testing with an initial screening immunoassay followed by confirmatory liquid or gas chromatography-mass spectroscopy testing [55].
More recently, there has been a shift towards doing a single-step chromatography-mass spectroscopy testing to reduce false-positives from immunoassay cross-reactivity and false-negatives as chromatography-mass spectroscopy methods have lower detection thresholds [56]. Additionally, this approach decreases turnaround time until final diagnostic results are obtained and cost by elimination of the initial screening immunoassay. This approach has been shown to potentially be effective in large academic centers that have the volume to establish an in-hospital chromatography-mass spectroscopy testing laboratory [56].
34.5.9 Immunoassay Testing and Gas Chromatography-Mass Spectroscopy
Immunoassay testing involves selective targeting via binding of antibodies. The three main types are enzyme-multiplied immunoassays, enzyme-linked immunosorbent assays, and fluorescence polarization assays. These techniques can be performed as point-of-care (POC) or laboratory testing. Turnaround time is usually less than 10 min for POC testing [57] and less than 60 min for laboratory-based testing [58]. The major limitation with these tests is the risk of cross-reactivity. Immunoassays target a specific substrate or component of the desired drug. Unfortunately, this can lead to false-positive detection of similarly structured compounds. Thus all immunoassay results need to be confirmed with diagnostic chromatography-mass spectroscopy testing.
Gas chromatography-mass spectroscopy allows quantitative analysis for specific molecular structure minimizing the risk of false-positives. However, this form of testing is more time-consuming, expensive, and requires specialized laboratory testing to perform [55]. Another similar testing method, liquid chromatography-tandem mass spectroscopy [56] has been used at some institutions as it may be more time-efficient [55].
34.5.10 Test of Choice in Inpatients
The test appropriate in each clinical scenario depends on the required turnaround time. POC immunoassays are used to in the emergency department when managing an unstable, acutely intoxicated patient [57, 58]. Similarly, the direct-to-diagnostic approach without sequential testing has been used in the outpatient chronic patient setting. This method requires several days before any results are obtained [56]. Inpatient pain medicine providers will encounter scenarios traversing both ends of this spectrum and will need to use clinical judgment to decide which test to order (Table 34.5).
34.5.11 Compounds to Test and Choice of Panel
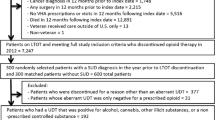
Standard drug panels typically test for amphetamines, cocaine, marijuana, phencyclidine, benzodiazepine, and opiates. Opiates are opioids derived from poppy seeds. The two commonly used opiates in clinical practice are codeine and morphine. Pain providers should add additional opioid-specific panels assessing for various synthetic and semisynthetic opioids and their metabolites [55, 56]. Figure 34.1 shows the metabolic pathways for common opioids that will direct choice of panel and interpretation of results. Using panels that incorporate metabolites as well as primary drugs can reduce risk of false-negatives and help identify adulterated samples.
34.5.12 Urine Sample Adulteration
Patients attempt various techniques to falsify urine toxicology results. Commonly used techniques include urine dilution, substitution with another individual’s urine, addition of household substances, addition of commercially available masking agents, and addition of medication directly into urine sample. Physical properties of sample, such as temperature, pH, and specific gravity, can be measured to assess sample validity [55]. Additionally, a thorough understanding of drug metabolism pathways can help with interpreting results.
Table 34.7 shows several commonly encountered urine toxicology examples. One more unique example is a patient prescribed Suboxone presenting with a sample positive for both buprenorphine and naloxone. When ingested orally as prescribed, naloxone is metabolized by first-pass metabolism and should not be identified in urine. This is likely either simulated compliance from adding Suboxone directly [56] to urine sample or attempted intravenous abuse of Suboxone. As with all diagnostic tests, urine toxicology results should be interpreted in the clinical context.
34.6 Inpatient Management
34.6.1 Risk Reduction Methods
Risk reduction strategies are increasingly being employed worldwide to combat the opioid epidemic. At the community level, Supervised Injection Facilities (SIF) have demonstrated significant public health benefits. The first SIF was opened in Switzerland in 1986. Since that time, SIFs have been developed throughout Europe [59]. The first government-sanctioned SIF in North America was established in Vancouver, British Columbia, Canada [59, 60] there have never been any government-supported SIFs in the United States, multiple clandestine SIFS have functioned since 2014. Research has shown the SIFs reduce opioid overdoses, decrease public injections, decrease publicly discarded needles, and facilitate referral to OUD treatment without increasing overall drug-use or drug-related crimes in the surrounding areas. Despite these successes, operating SIFs has remained a controversial issue.
Currently most hospitals operate under an abstinence-based policy. This policy places people with substance use (PWSU) at significant health risks. At baseline PWSU often have poor health in part due to prevalence of blood-borne infections such as HIV and have high rates of inpatient admissions. According to a prospective cohort study that followed patients for 3 years, 35% of PWSU were hospitalized at least once and 20% were hospitalized multiple times. The two most common reasons for admission were pneumonia and soft-tissue infection [61].
Due to the hospital-abstinence policies, PWSU often turn to high-risk drug practices such as needle sharing and injecting alone [62]. According to one study, 44% of PSWUD who have been admitted to a hospital report to have actively used illicit drugs while admitted [63]. The inability to access illicit drugs, also leads to high rates of discharge against medical advice, which is estimated to occur in about 30% of admitted injection drug users [62]. This leads to inappropriate medical care and frequent readmissions.
There has been increasing interest in offering a SIF for inpatients. One study whose primary outcome was to assess PSWUD willingness to participate if admitted to the hospital showed that about two-thirds of PWSU would participate. About 90% of patients who had left a hospital AMA in the past and about 75% of patients who had used illicit drugs while admitted to a hospital reported they would be interested if offered. The most common reason for PWSU interest in the SIF was that it would allow them to stay in the hospital for their medical care. This study was performed in Vancouver, Canada which already has a functioning outpatient SIF [62]. All three studies that have addressed this same question in the United States have concluded that PWSU would be interested in using inpatient SIFs [63].
There continues to be significant resistance to establishing such practices beyond the legal limitations. Opponents advocate that funds would be better allocated to provide these patients with preventative and treatment services [59, 60]. However, SIF facilities provide an opportunity to engage and educate PWSU about treatment and therapy options. Estimates vary widely, with 10–42% of outpatient SIF users entering an addiction treatment program [59,60,61,62,63,64].
34.6.2 Initiating OUD Treatment While Inpatient
Initiating treatment for substance use disorders in the acute hospital setting is feasible and effective [5,6,7,8,9] and results in better medical and substance use disorder outcomes including decreased emergency visits, increased completion of medical treatment, and transition to outpatient substance use treatment [6, 8]. Without substance use treatment, the majority of individuals will return to substance use upon discharge from an inpatient setting and are at high risk for poor outcomes particularly for opioid use disorder and overdose [14, 15]. Engaging patients in treatment for opioid use disorder improves outcomes for some of the highest risk individuals [7].
Currently there are three FDA-approved medications for OUD: methadone, buprenorphine, and extended-release injectable naltrexone. All patients with OUD not on pharmacologic management should be recommended one of these treatment options and connected with outpatient substance use treatment [10,11,12,13]. The choice of treatment should be a shared decision between the clinician and patient. Inpatient psychiatric and substance use disorder specialists can assist in this process with consideration of the patient’s preference, previous treatment, and setting of treatment (supervised opioid treatment program versus outpatient office setting for buprenorphine or naltrexone). Patients declining pharmacotherapy for OUD should be provided with outpatient referrals for substance use treatment and an intranasal naloxone kit upon discharge.
Although all effective treatments, there are specific considerations and limitations in the inpatient setting surrounding each OUD medication.
34.6.3 Opioid Agonists
Both methadone and buprenorphine can be used to treat pain and as MOUD. Buprenorphine is different than methadone in that it can precipitate opioid withdrawal given its higher affinity for the mu-opioid receptors than other opioids. Opioid-tolerant patients will need to enter a state of mild to moderate opioid withdrawal or a COWS score greater than 10 prior to initiating buprenorphine [34]. Generally initiation of buprenorphine is at least 6–12 h after last use of short-acting opioids or 24–72 h after last dose of long-acting opioids [10]. It is important to symptomatically manage opioid withdrawal as subjective pain might increase and untreated withdrawal symptoms will limit comfort in transition to buprenorphine. Specific considerations in initiating methadone or buprenorphine are similar to principles discussed in the section “Medications in Opioid Withdrawal.”
34.6.4 Extended-Release Injectable Naltrexone
Extended-release injectable naltrexone in the inpatient setting is limited to those whose pain is managed with non-opioid analgesics and individuals not on opioids for 7–14 days. There are current studies looking at more rapid induction methods although not yet widely practiced [65]. This timeline is often a barrier to initiating extended-release injectable naltrexone, and it is not widely available on hospital formularies. For those who have been off opioids for this timeline, an oral naloxone challenge can be useful before initiating naltrexone treatment. A dose of 0.4–0.8 mg of naloxone is administered and the patient is observed for precipitated withdrawal [10]. Careful consideration should be given to those interested in outpatient follow-up for extended-release injectable naltrexone as individuals will need to abstain from opioid use for an extended period of time and are at high risk for relapse and overdose.
34.6.5 Naloxone Kit and Outpatient OUD Treatment on Discharge
All patients discharged on daily opioid dosing greater than 90-mg morphine equivalents, those on longer-acting opioids (methadone or extended-release oxycodone), and those with a history of OUD or substance misuse should be discharged with an intranasal naloxone kit [66]. Patients at high risk for opioid overdose and those with OUD also need early follow-up with substance use treatment. Substance use treatment includes MOUD, counseling and other supportive services, and is offered by treatment programs or providers in the outpatient setting. It is encouraged to involve family members and significant others in education and training in naloxone administration prior to discharge.
34.7 Managing Pain in Inpatients Continuing to Use Outside Drugs
PWSU are at increased risk for presenting to the emergency department or be admitted for management of pain. Lacerations, physical assault, fracture, abdominal pain, and musculoskeletal problems are among the ten most common reasons PWUD present to the emergency department. Fractures, lacerations, trauma, osteomyelitis, and pyelonephritis are all common reasons PWUD get admitted to the hospital [61]. In addition, many of these patients will require surgical intervention for various reasons including treating the conditions mentioned above.
As mentioned earlier, fear of not having pain adequately treated is one of the main reasons PWUD continue to use illicit drugs while admitted. The most important step in managing pain in these patients is to open a dialogue with the patients to answer questions and assuage their concerns. The patient needs to understand that their pain will be taken seriously and addressed by the pain management provider and primary team. The pain management provider should also discuss the risks associated with the patient concurrently using outside substances. Patients using outside illicit opioids while also being treated with inpatient prescribed opioids increases risk of overdose and makes it difficult for providers to assess opioid requirements leading to even worse analgesia. In cases where prevention-based approach to using outside substances has failed, providers should focus on a multimodal plan to minimize opioids and choose opioids with lowest risk of overdose.
Regional anesthetic techniques can be used to target the source of pain. All patients without contraindications should be prescribed NSAIDs and acetaminophen. Other non-opioid pharmacologic options include ketamine and lidocaine infusions. Both of these drugs can be administered safely in unmonitored settings. Although ketamine is not a respiratory depressant, airway reflexes will be impaired in a dose-dependent fashion. These risks need to be considered in the context of the patient’s primary pathology. Patients receiving lidocaine infusions need to be monitored closely for signs of local-anesthetic systemic toxicity. Multimodal analgesia in the context of opioid-tolerant individuals is discussed in detail in another chapter. When opioid-based analgesia is required, short-acting opioids should be used to minimize the risk of overdose. Patient-controlled analgesia are ideal options as the patient will be able to titrate medications to desired effect.
34.8 Summary
-
Identifying and managing patients with OUD remains a complex issue for inpatient medical providers.
-
Patients with OUD have increased incidence of hospital admission and are at risk for poor medical outcomes [4].
-
It is estimated that up to 44% of illicit drug users may actively continue to use substances while admitted [63]. Unidentified and untreated substance use carries risks of overdose, withdrawal, and is linked to patients leaving against medical advice. Managing acute opioid withdrawal using clinical assessment tools and medications, such as opioid and alpha-2 agonists, can decrease discomfort and risk of patients leaving against medical advice.
-
All admitted patients should be screened for SUD with a comprehensive history and physical examination.
-
Further testing with urine toxicology may be considered on a case-by-case basis for both diagnostic or monitoring purposes. Currently, only 20% of all patients with OUD are on appropriate MOUD therapy [67].
-
The inpatient admission is an ideal opportunity to start patients on MOUD and establish appropriate [67] outpatient follow-up.
-
New rapid-induction protocols that allow initiation of therapy while inpatient are becoming more established for buprenorphine and naltrexone [10].
-
Methadone can also be started as an inpatient but is often limited by outpatient access to a federally certified opioid treatment program.
-
Early identification and management of OUD and other SUDs during acute hospitalization improves medical outcomes and reduces overdose deaths.
References
Center for Health Information and Analysis. Behavioral health & readmissions in Massachusetts acute care hospitals. 2016. https://archives.lib.state.ma.us/handle/2452/4229382016. Accessed 19 Sep 2019.
Walley A, Paasche-Orlow M, Lee E, Forsythe S, Chetty V, Mitchell S, Jack B. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6(1):50–6.
Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health. Center for Behavioral Health Statistics and Quality; 2019. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf. Accessed 10 Sep 2019.
Ronan M, Herzig S. Hospitalization related to opioid abuse/dependence and associated serious infections increase sharply 2002–2012. Health Affairs (Milwood). 2016;35(5):823–37.
Liebschutz J, Crooks D, Herman D, Anderson B, Tsui J, Meshesha L, Dossabhoy S, Stein M. Buprenorphine treatment for hospitalized, opioid-dependent patients: a randomized clinical trial. JAMA Intern Med. 2014;174(8):1369–13716.
O’Toole T, Conde-Martel A, Young J, Price J, Bigelow G, Ford D. Managing acutely ill substance-abusing patients in an integrated day hospital outpatient program: medical therapies, complications, and overall treatment outcomes. J Gen Intern Med. 2006;21(6):570–6.
Shanahan C, Beers D, Alford D, Brigandi E, Samet J. A transitional opioid program to engage hospitalized drug users. J Gen Intern Med. 2010;25(8):803–8.
Wei J, Defries T, Lozada M, Young N, Huen W, Tulsky J. An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. J Gen Intern Med. 2015;30(3):365–70.
Trowbridge P, Weinstein Z, Kerensky T, Roy P, Regan D, Samet J, Walley A. Addiction consultation services—linking hospitalized patients to outpatient addiction treatment. J Subst Abus Treat. 2017;79:1–5.
Kampman K, Jarvis M. American Society of Addiction Medicine National Practice Guidelines for the use of medications in the treatment of addiction involving opioid use. J Addict Med. 2015;9(5):358–67.
Center for Substance Abuse Treatment. Detoxification and substance abuse treatment. treatment improvement protocol (TIP) series, no. 45. HHS Publication No. (SMA) 15-4131. Rockville, MD: Center for Substance Abuse Treatment; 2006.
Center for Substance Abuse Treatment. Addressing opioid use disorder in general medical settings for healthcare professionals. Treatment improvement protocol (TIP) series 63 part 2. Substance abuse and mental health services administration. HHS Publication No. (SMA) 18-5063. Center for Substance Abuse Treatment; 2018.
Herron A, Brennan T. The ASAM essentials of addiction medicine, vol. 12. 2nd ed. Philadelphia: Wolters Kluwer; 2015. p. 535–65.
Chutuape M, Jasinski D, Fingerhood M, Stitzer M. One-, 3-, and 6- month outcomes after brief inpatient opioid detoxification. Am J Drug Alcohol Abuse. 2001;27(1):19–44.
Volkow N, Freiden T, Hyde P, Cha S. Medication-assisted therapies—tackling the opioid-overuse epidemic. N Engl J Med. 2014;370:2063–6.
McNeely J, Kumar P, Rieckmann T, Sedlander E, Farkas S, Chollak C, Kannry J, Vega A, Waite E, Peccoralo L, Rosenthal R, McCarty D, Rotrosen J. Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: a qualitative study of patients, providers, and staff. Addict Sci Clin Pract. 2018;13:8, 1–15.
Avery J, Knoepflmacher D, Mauer E, Kast K, Greiner M, Avery J, Penzner J. Improvement in resident’s attitudes toward individuals with substance use disorders following an online training module on stigma. Hosp Spec Surg. 2018;15(1):31–6.
Wakeman S, Pham-Kanter G, Donelan K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus. 2016;37:635–41.
Brener L, Von Hippel W, Von Hippel C, Resnick I, Treloar C. Perceptions of discriminatory treatment by staff as predictors of drug treatment completion: utility of a mixed methods approach. Drug Alcohol Rev. 2010;29:491–7.
Alford D. Management of acute and chronic pain. In: Handbook of office-based buprenorphine treatment of opioid dependence. Amer Psychiatric Pub Inc; Second edition, New York, 2018. pp. 213–222.
Merrill J, Rhodes L, Deyo R, Marlatt G, Bradley K. Mutual mistrust in the medical care of drug users: the keys to the “narc” cabinet. J Gen Intern Med. 2002;17:327–33.
Link B, Phelan J. Stigma and its public health implications. Lancet. 2006;367:528–9.
Baldacchino A, Gilchrist G, Fleming R, Bannister J. Guilty until proven innocent: a qualitative study of the management of chronic non-cancer pain among patients with a history of substance abuse. Addict Behav. 2010;35:270–2.
Berg K, Arnstern J, Sacajiu G, Karasz A. Providers’ experiences treating chronic pain among opioid-dependent drug users. J Gen Intern Med. 2009;24:482–8.
Kantor T, Cantor R, Tom E. A study of hospitalized surgical patients on methadone maintenance. Drug Alcohol Depend. 1980;6:163–73.
Manfredi P, Gonzales G, Cheville A, Kornick C, Payne R. Methadone analgesia in cancer pain patients on chronic methadone maintenance therapy. J Pain Symptom Manage. 2001;21:169–74.
Karasz A, Zallman L, Berg K, Gourevitch M, Selwyn P, Arnsten J. The experience of chronic severe pain in patients undergoing methadone maintenance treatment. J Pain Symptom Manage. 2004;28:517–25.
Ti L, Voon P, Dobrer S, Montaner J, Wood E, Kerr T. Denial of pain medication by health care providers predicts in-hospital illicit drug use among individuals who use illicit drugs. Pain Res Manage. 2015;20:84–8.
Motivational Interviewing/SAMHSA-HRSA. In: Integration.samhsa.gov. 2012. https://www.integration.samhsa.gov/clinical-practice/motivational-interviewing#resources. Accessed 4 Sep 2019.
American Psychiatric Association, editor. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
McNeil R, Small W, Wood E, Kerr T. Hospitals as a risk environment: an ethno-epidemiological study of voluntary and involuntary discharge from hospital against medical advice among people who inject drugs. Soc Sci Med. 2014;105:59–66.
Katz E, Brown B, Schwartz R, O’Grady K, King S, Devang. Transitioning opioid-dependent patients from detoxification to long-term treatment: efficacy of intensive role induction. Drug Alcohol Depend. 2011;117:24–30.
Handelsman L, Cochrane K, Aronson M, Ness R, Rubinstein K, Kanof P. Two new rating scales for opiate withdrawal. Am J Drug Alcohol Abuse. 1987;13:293–308.
Wesson D, Ling W. The clinical opiate withdrawal scale (COWS). J Psychoactive Drugs. 2003;35:253–9.
Burma N, Kwok C, Trang T. Therapies and mechanisms of opioid withdrawal. Pain Manage. 2017;7:455–9.
Gorodetzky C, Walsh S, Martin P, Saxon A, Gullo K, Biswas K. A phase III, randomized, multi-center, double blind, placebo controlled study of safety and efficacy of lofexidine for relief of symptoms in individuals undergoing inpatient opioid withdrawal. Drug Alcohol Depend. 2017;176:79–88.
Gowing L, Farrell M, Ali R, White J. Alpha2-adrenergic agonists for the management of opioid withdrawal. Cochrane Database Syst Rev. 2009;2:CD002024. https://doi.org/10.1002/14651858.CD002024.pub3.
Pergolizzi J, Annabi H, Gharibo C, LeQuang J. The role of lofexidine in management of opioid withdrawal. Pain Ther. 2019;8:67–78.
Albertson T, Chenoweth J, Ford J, Owen K, Sutter M. Is it prime time for alpha2-adrenocepter agonists in the treatment of withdrawal syndromes? J Med Toxicol. 2014;10(4):369–81.
Collins E, Kleber H, Whittington R, Heitler N. Anesthesia-assisted versus buprenorphine- or clonidine-associated heroin detoxification and naltrexone induction: a randomized trial. J Am Med Assoc. 2005;294:903–13.
American Society of Addiction Medicine. Public policy statement on rapid and ultra rapid opioid detoxification. 2005. https://www.asam.org/docs/default-source/public-policy-statements/1rod-urod-rev-of-oadusa-4-051.pdf. Accessed 4 Sep 2019.
Hamilton R, Olmedo R, Shah S, Hung O, Howland M, Perrone J, Nelson L, Lewin N, Hoffman R. Complications of ultrarapid opioid detoxification with subcutaneous naltrexone pellets. Acad Emerg Med. 2002;9:63–8.
Gowing L, Ali R, White J. Opioid antagonists under heavy sedation or anaesthesia for opioid withdrawal. Cochrane Database Syst Rev. 2010;1:CD002022.
Boyer E. Management of opioid analgesic overdose. N Engl J Med. 2012;367(2):146–55.
Goldfrank L, Weisman R, Errick J, Lo M. A dosing nomogram for continuous infusion intravenous naloxone. Ann Emerg Med. 1986;15(5):566–70.
Farkas A, Lynch M, Westover R, Giles J, Siripong N, Nalatwad A, et al. Pulmonary complications of opioid overdose treated with naloxone. Ann Emerg Med. 2020;75:39–48.
Centers for Disease Control and Prevention. Number of poisoning deaths involving opioid analgesics and other drugs or substances—United States, 1999–2010. Morb Mortal Wkly Rep. 2013;62:234.
Screening/SAMHSA-HRSA. In: Integration.samhsa.gov. 2019. https://www.integration.samhsa.gov/clinical-practice/sbirt/screening. Accessed 30 July 2019.
Brown R, Rounds L. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94:135–40.
Centers for Disease Control and Prevention. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths—United States, 2010. Morb Mortal Wkly Rep. 2014;63:881–8.
Tintinalli J, Stapczunski J, Ma O, Yealy D, Meckler G, Cline D. Tintinalli's emergency medicine: a comprehensive study guide. 8th ed. New York: McGraw-Hill Education; 2016.
Madadi P, Persaud N. Suicide by means of opioid overdose in patients with chronic pain. Curr Pain Headache Rep. 2014;18:460.
Oquendo M, Volkow N. Suicide: a silent contributor to opioid overdose deaths. N Engl J Med. 2018;378:1567–9.
Rosenthal E, Karchmer A, Theisen-Toupal J, Castillo R, Rowley C. Suboptimal addiction interventions for patients hospitalized with injection drug use associated infective endocarditis. Am J Med. 2016;129(5):481–5.
Moeller K, Kissack J, Atayee R, Lee K. Clinical interpretation of urine drug tests. Mayo Clin Proc. 2017;92(5):774–96.
Gencheva R, Petrides A, Kantartjis M, Tanasijevic M, Dahlin J, Melanson S. Clinical benefits of direct-to-definitive testing for monitoring compliance in pain management. Pain Phys J. 2018;21(6):E583–92.
Lager P, Attema-de Jonge M, Gorzeman M, Kerkvliet L, Franssen E. Clinical value of drugs of abuse point of care testing in an emergency department setting. Toxicol Rep. 2018;5:12–7.
Tenenbein M. Do you really need that emergency drug screen? Clin Toxicol. 2009;47(4):286–91.
Gostin L, Hodge J, Gulinson C. Supervised injection facilities. JAMA. 2019;321(8):745–6.
Kerr T, Mitra S, Kennedy M, McNeil R. Supervised injection facilities in Canada: past, present, and future. Harm Reduct J. 2017;14(1):28.
Palepu A, Tyndall M, Leon H, Muller J, O'Shaughnessy M, Schechter M, et al. Hospital utilization and costs in a cohort of injection drug users. CMAJ. 2001;165(5):415–20.
Ti L, Buxton J, Harrison S, Dobrer S, Montaner J, Wood E, et al. Willingness to access an in-hospital supervised injection facility among hospitalized people who use illicit drugs. J Hosp Med. 2015;10(5):301–6.
Harris R, Richardson J, Frasso R, Anderson E. Perceptions about supervised injection facilities among people who inject drugs in Philadelphia. Int J Drug Policy. 2018;52:56–61.
Rosenstein R. Fight drug abuse, don’t subsidize it. N Y Times. 2018;A:23. https://www.nytimes.com/2018/08/27/opinion/opioids-heroin-injectionsites.html.
Sigmon S, Bisaga A, Nunes E, O’Connor P, Kosten T, Woody G. Opioid detoxification and naltrexone induction strategies: recommendations for clinical practice. Am J Drug Alcohol Abuse. 2012;38:187–99.
Miller M, Barber C, Leatherman S, Fonda J, Hermos J, Cho K, Gagnon D. Prescription opioid duration of action and the risk of unintentional overdose among patients receiving opioid therapy. JAMA Intern Med. 2015;175:608–15.
Ward E, Quaye A, Wilens T. Opioid use disorders. Anesth Analg. 2018;127:539–47.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Mainkar, O., Greiner, M., Avery, J., Mehta, N. (2020). Incidentally Identified Opioid Misuse and Opioid Use Disorder While Inpatient. In: Abd-Elsayed, A. (eds) Guide to the Inpatient Pain Consult. Springer, Cham. https://doi.org/10.1007/978-3-030-40449-9_34
Download citation
DOI: https://doi.org/10.1007/978-3-030-40449-9_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-40448-2
Online ISBN: 978-3-030-40449-9
eBook Packages: MedicineMedicine (R0)