Abstract
Effective and scalable interventions are needed to reach a greater proportion of individuals with serious mental illness (SMI) who experience alarmingly high rates of obesity. This pilot study evaluated the feasibility of translating an evidenced-based professional health coach model (In SHAPE) to peer health coaching for overweight and obese individuals with SMI. Key stakeholders collaborated to modify In SHAPE to include a transition from professional health coaching to individual and group-based peer health coaching enhanced by mobile health technology. Ten individuals with SMI were recruited from a public mental health agency to participate in a 6-month feasibility pilot study of the new model. There was no overall significant change in mean weight; however, over half (56 %) of participants lost weight by the end of the intervention with mean weight loss 2.7 ± 2.1 kg. Participants reported high satisfaction and perceived benefits from the program. Qualitative interviews with key stakeholders indicated that the intervention was implemented as planned. This formative research showed that peer health coaching for individuals with SMI is feasible. Further research is needed to evaluate its effectiveness.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Cardiovascular disease attributed to obesity and smoking is the leading cause of the estimated 25–30-year reduced life expectancy among individuals with serious mental illness (SMI) [1]. The prevalence of obesity among individuals with SMI is about twice as high as in the general population [2]. Individuals with SMI experience numerous challenges to achieving and sustaining weight loss, including the metabolic effects of psychoactive medications, poor nutrition, low participation in physical activity, and problems with motivation and depression. While there has been an upsurge in health promotion interventions adapted for individuals with SMI [3–6], the most effective treatments are time intensive, delivered by highly trained professionals and typically available to only a subset of the eligible population [3, 5]. As the burden of obesity grows in this population, innovative, cost-effective, and scalable interventions are needed that require less intensive resources while delivering effective behavior change strategies for at-risk individuals with SMI.
Peer health coaching is a promising model for extending the capacity of health promotion initiatives for individuals with SMI. Peer support is a proven strategy for motivating and sustaining behavior change in general health care populations [7–12]. Combining reduced intensity behavioral weight loss interventions with peer health coaching holds promise as a cost-effective approach to obesity treatment in the general population [13, 14]. Peer health coaches build trust with participants by sharing their lived experiences of coping with health conditions along with giving advice, sharing problem-solving strategies, role modeling, and providing emotional support for behavioral change [15, 16].
Increasing recognition that mental health recovery and physical health are intertwined has contributed to the development of novel roles for peers in health promotion for individuals with SMI. Druss and colleagues developed and pilot-tested a peer-led medical self-management program for individuals with SMI adapted from the Chronic Disease Self-Management Program [17]. The brief intervention was associated with improved patient activation in primary care visits as well as improvements in self-efficacy, illness self-management, physical and emotional well-being, and health functioning [18]. In addition, a pilot study by our group found that peer-co-led patient education and skills training was associated with improved patient activation and communication skills for medical visits [19]. Similarly, a peer navigator intervention targeting health care engagement and self-management among individuals with SMI contributed to improvements in self-reported health and decline in pain severity [20]. These studies suggest that peer health coaching may be an effective approach to addressing the physical health of individuals with SMI.
However, little is known about the potential role of peers in health promotion interventions aimed at reducing cardiovascular risk in adults with SMI. Many of the core principles, strategies, and activities of peer support in mental health recovery (e.g., instilling hope, expressing empathy, role modeling strategies to overcome barriers, and experiential learning) have direct relevance for motivating and empowering overweight and obese individuals with SMI to engage in healthy eating and exercise to better manage their weight. In addition, emerging mobile health technologies facilitated by peers may offer the frequent and personalized support needed to help consumers initiate and sustain behavior change. Peer health coaching may be an effective way to deliver evidenced-based behavior change strategies in public mental health care systems facing resource constraints. This report describes the process of translating an evidence-based professional health coach model for overweight and obese individuals with SMI to peer health coaching enhanced by mobile health technology. We present results from an initial feasibility study evaluating how key stakeholders (fitness trainers, peers, and participants) responded to the new model.
METHODS
Our intervention was adapted from the In SHAPE healthy lifestyle program aimed at promoting physical fitness, healthy eating, and weight loss in adults with SMI [21]. In SHAPE is embedded within community mental health centers (CMHCs) and consists of a fitness club membership and one-on-one sessions with a health promotion coach who is certified as a fitness trainer and has received basic training on principles of healthy eating and nutrition. Health promotion coaches meet with participants for weekly 1-h sessions at a local fitness club (e.g., YMCA) and provide fitness coaching, support, and reinforcement of exercise and healthy eating. The effectiveness of the In SHAPE program has been demonstrated in a pilot study [21], and in two separate randomized controlled trials in which half of individuals receiving In SHAPE (49 % in one trial and 51 % in the other) achieved reduced cardiovascular risk defined as either clinically significant weight loss (≥5 %) or clinically significant improved fitness (>50 meter increase on the 6-Minute Walk Test) [3, 22].
PeerFIT health promotion intervention
Despite the demonstrated effectiveness of In SHAPE, participation is typically open-ended without a specified protocol or process for transitioning from professionalized personal training to independent exercise. Our team engaged with community partners in a collaborative process of modifying In SHAPE to include a transition from a professional fitness trainer to peer health coaching enhanced with mobile health technology involving wearable activity tracking devices and smartphones to increase motivation and promote self-monitoring for weight loss. PeerFIT was conceived as a partnership between the Dartmouth Centers for Health and Aging, a peer support agency in Keene, NH, and a CMHC also located in Keene, NH. Each member of the PeerFIT team was familiar with the In SHAPE program, with the majority having had prior experience with the intervention as participants, fitness trainers, or evaluators. Larry Fricks, a national leader in peer-based health promotion, provided training and consultation during planning and implementation of the intervention.
Core components of PeerFIT included the following: (a) personalized fitness training, (b) one-on-one and group-based peer health coaching, (c) motivational text messages, and (d) physical activity sensors for monitoring and feedback. The model emphasized a health coaching team approach with a transition from fitness professionals to peer health coaching. Peer health coaching was delivered by two individuals who self-identified as experiencing success in both recovery from mental illness and health behavior change. Peers received training in the principles of fitness, nutrition, motivational interviewing, and effective health coaching strategies. Study supervisors conducted weekly 1-h team meetings to provide a venue for problem solving and identifying strategies for motivating and modeling behavior change. Peer health coaches also participated in weekly 1-h peer support supervision. From October 2012 to November 2013, our team developed and evaluated the PeerFIT intervention.
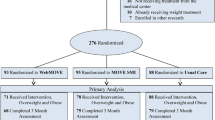
PeerFIT was delivered in three phases over a 6-month period (see Fig. 1). Phase I (weeks 1–4) involved orientation sessions with the fitness trainer and peer health coach focused on the following: (a) setting person-centered weight loss and fitness goals and (b) identifying barriers and facilitators to exercise and healthy eating. Fitness trainers and peer coaches explored participants’ past experiences and preferences for exercise and healthy eating and readiness to change behaviors. The session included a structured fitness and nutrition assessment to establish baseline patterns. Participants were also taught to use the physical activity tracking device and smartphone.
Phase II (weeks 5–12) focused on exercise and healthy eating education and activities. Participants met weekly with a fitness trainer for supported exercise sessions at a local gym, while peer health coaching focused on activities to help participants make healthy changes in diet and exercise in their daily lives. During individual sessions, participants chose an activity from a menu of healthy eating activities, including meal planning, eating out, budgeting, and grocery shopping. Additionally, peers encouraged participants to join them in physical activity at the gym or in the community.
Peer health coaches also led weekly 1-h group meetings to inspire, guide, and support participants through the process of setting specific and measurable health goals, establishing and following a weekly action plan to create new health habits, and incorporating healthy changes into their everyday lives. The group-based curriculum was adapted from the Whole Health Action Management (WHAM) training program and peer support model developed by the SAMHSA-HSRA Center for Integrated Health Solutions [23]. Our modified curriculum added healthy eating education and skills training activities to supplement the curriculum’s focus on fitness and wellness.
Phase III (weeks 13–24) focused on the transition from one-on-one sessions with a fitness trainer to peer health coaching. Participants met one-on-one with peer health coaches, every other week, to continue peer modeling and integration of health behaviors into daily life. Peer-led exercise groups met once per week for 1-h and involved a variety of low-impact cardio exercises and team sports. Weekly peer-led groups also met once per week to reinforce healthy behaviors through peer support and accountability for goals. Finally, participants met with their fitness trainers and peer coaches together once per month for 1-h to review progress and make modifications to health goals and activities.
Mobile health technology support
Mobile health technology in the form of wearable activity tracking devices (FitBit or Nike FuelBand) and smartphones (Apple iPhone 4S) for accessing the mobile applications for the tracking devices and for sending and receiving text messages were provided to participants at the start of the program. The mobile technology was intended to enhance peer health coaching and promote health behavior change in daily contexts. The FitBit and FuelBand are both accelerometers that track steps, distance, and calories burned and sync wirelessly with smartphone applications available for the iPhone 4S. Both devices reward milestones such as reaching 10,000 steps with colorful trophies or animations, and allow users to compare steps and progress with others through the smartphone application. A complete description of the mobile health technology component is available elsewhere [24].
Participant recruitment
Ten participants were recruited for the study from a community mental health center in Keene, NH. Inclusion criteria were as follows: age 21 or older; axis I diagnosis of major depression, bipolar disorder, schizoaffective disorder, or schizophrenia; body mass index (BMI) ≥25; and able and willing to provide informed consent for participation. Individuals who met any of the following exclusion criteria were not eligible for the study: currently residing in a nursing home or group home; terminal physical illness; primary diagnosis of dementia, co-morbid diagnosis of dementia, or significant cognitive impairment as indicated by an MMSE score <24; inability to speak and understand English; and pregnant or planning a pregnancy within the next 6 months. Participants were recruited through referrals from clinic staff, case managers, and mental health clinicians. Twenty-four people were referred to the study. Ten of those contacted were not interested in the study, two did not meet the study criteria for BMI, one participant was unable to reach after initial contact, and one participant who was eligible and interested in the study moved before starting the program. Committees for the Protection of Human Subjects at Dartmouth College and the New Hampshire Department of Health and Human Services approved all study procedures.
Study design
We used an intervention mixed-methods study design involving quantitative assessments, in-depth interviews, and focus groups to assess feasibility from the perspective of three stakeholder groups: participants, fitness trainers, and peer health coaches. Using multiple methods allows for a more complete and thorough understanding of feasibility issues in the target population [25, 26]. Feasibility was assessed by program participation and perceived benefit and satisfaction with the program. A major objective of the pilot study was to determine whether modifications and refinements were necessary before conducting further research to evaluate the potential effectiveness of the intervention [27].
Study measures
Quantitative measures of feasibility included attendance and participant satisfaction. Fitness trainers and peer coaches tracked attendance during phases II and III of the program. These data were used to calculate individual and overall participation rates for each intervention component. Program satisfaction and feedback was assessed using a form completed by participants at the end of the intervention.
Qualitative interviews
Semi-structured interviews explored participants’ satisfaction, perceived benefits, and recommended modifications for each intervention component: peer coaches, fitness trainers, group activities, and mobile health technology. We used an interview topic guide that followed a “funnel structure” in which broad questions were asked first, with the interviewer gradually proceeding to more specific questions within each domain [28]. Qualitative interviews lasted 45–60 min for which participants were compensated $20. Focus group interviews covering the same domains were conducted with peer health coaches and personal fitness trainers. Focus group interviews lasted 60–90 min for which participants were compensated with a $25 gift card. All interviews were audiotaped and transcribed verbatim.
The methodology for the qualitative assessment involved a rapid assessment process described by Beebe [29] as an intensive, team-based qualitative inquiry using triangulation and iterative data analysis. In contrast to traditional qualitative methods that tend to be long-term, descriptive and broad-based, rapid qualitative methods are time-limited, targeted, and often more explanatory in nature. This technique is particularly useful when there is a pragmatic need for qualitative data to inform services and intervention development [30].
Data analysis
Descriptive statistics, including means and frequencies, were used to summarize program attendance and satisfaction. Statistical analyses were performed using SPSS software, version 19.0. The qualitative data analysis involved data reduction [31] and matrix analysis techniques [32]. Four members of the research team independently reviewed interview transcripts and noted key themes within each domain. Our objective was to generate primary feasibility findings within each domain for each type of respondent (i.e., participant, peer health coach, fitness trainer) and across respondents.
RESULTS
The 10 participants were individuals with SMI (n = 2 schizophrenia; n = 1 schizoaffective disorder; n = 1 bipolar disorder; n = 6 major depression) ranging in age from 30 to 57 years (mean = 46.6; SD = 8.7) with a mean body mass index of 42.3 kg/m2 (SD = 15.3) and mean weight of 108.8 kg (SD = 37.6). Participants were predominantly white (90 %) and most were women (90 %). All participants were single or never married. One participant dropped out after 4 weeks because of a medical concern unrelated to the study. Attendance rates for each of the components of the program are listed in Table 1.
There was no overall significant change in mean weight; however, over half (56 %) of participants lost weight by the end of the intervention with mean weight loss 2.7 ± 2.1 kg. Participants reported a favorable response to the intervention on the satisfaction questionnaire administered at the end the program (Table 2). The majority of completers reported that the program was useful and convenient and helped them reach their goals. Interestingly, 33 % (n = 3) of completers reported that the groups were not helpful. The majority of completers reported that they would recommend the program to a friend.
Key stakeholder interviews
From the perspective of all stakeholder groups, the combination of fitness trainers, peer health coaching, and mobile health technology created a “system of support” for health behavior change. Participants reported benefits from both the structured workouts with a fitness trainer and peer health coaching for healthy eating and exercise. They learned to set and work towards health goals and benefited from opportunities to socialize with each other during peer-led group sessions. Many participants adopted a new exercise or increased the amount or intensity of exercise. Increasing fruit and vegetable intake and cutting back on high-calorie snacks and sugar-sweetened beverages were the most common types of nutritional changes reported by participants. Wearable activity monitoring devices motivated participants to increase their physical activity, while text messages from peer health coaches encouraged them to make healthy changes on a daily basis.
Peer health coaching complemented the gym-based fitness trainer model by providing emotional support and modeling exercise and healthier food choices in home and social environments. Peer health coaches felt they could relate to participants on a personal level and believed that peer sessions were the most “natural” component of the program. Fitness trainers reported that the peers were particularly helpful at addressing participants’ barriers and challenges to healthy eating (e.g., perceived cost, lack of time, and cooking skills).
Major feedback from peer health coaches was that they were uncomfortable as “coaches” and “instructors” and they expressed a strong desire to engage in mutual peer support in which the focus of sessions is negotiated between the peer and participant and co-learning is emphasized. They were reluctant to use many of the coaching techniques outlined in the study protocol due to concerns that doing so would create a power imbalance in their relationships with participants. In contrast, participants reported that a major strength of the program was peer instruction, modeling, and assistance with planning weekly exercise activities, and sharing “what works.” Participants did not express a desire for reciprocal relationships with peer health coaches; however, many participants wanted more opportunities to cultivate relationships with other participants in the program.
The final phase of PeerFIT included a transition from individual sessions with a trainer to peer-led group exercise. Participants reported that they enjoyed the “fun” aspect of peer-led group exercise and interacting with other participants. They also liked having a variety of activities to choose from. Participants noted several barriers to participating in the group exercise, including schedule conflicts and concerns about physical limitations. Peer health coaches recommended that exercise groups be introduced at the beginning of the program at the same time as individual fitness training sessions to increase engagement and attendance. Fitness trainers agreed that 8–10 training sessions was sufficient time to learn how to exercise, but they commented that it was “difficult” for them to disengage with participants once the series of sessions were over. However, neither peer health coaches nor participants expressed a desire for more involvement by the fitness trainer during the final phase of the program.
DISCUSSION
The PeerFIT program appeared to be feasible as evidenced by participation rates, perceived benefit, and satisfaction with the program. Participation rates were high or satisfactory for most intervention components with the exception of peer-led exercise groups. Attendance rates at one-on-one sessions with fitness trainers and peer health coaches were similar (81 vs. 79 %, respectively), and the majority of participants attended weekly peer-led nutrition sessions and one-on-one meetings with peer health coaches during the final phase of the program. PeerFIT was feasible to implement as a collaborative effort between a community mental health center and a peer support agency and showed promise for improving healthy eating, exercise, and weight loss among individuals with SMI.
Our study contributes to the growing body of research indicating a promising role for peers in health promotion for individuals with SMI [17, 18, 20, 33]. Research on peer support to date has primarily focused on the peer’s role in improving recovery-oriented outcomes such as quality of life, self-esteem, and life satisfaction [34–36]. However, peers in mental health recovery may be just as well suited to address health behavior change. Our study involved peers who were trained to guide participants towards health behavior change and use self-disclosure to inspire hope and support—a technique also used for peer health coaching in non-mental health contexts—while also attending to the challenges associated with mental illness.
An important finding from our qualitative interviews with the peer health coaches was their strong preference for more mutuality in their relationships with participants and their desire for co-learning opportunities. They did not feel comfortable in the role of “instructor” or “coach,” because they believed this created a hierarchy that interfered with their ability to establish reciprocal relationships. Of note, the peers in this pilot study were from a peer support agency that trains peers to provide “Intentional Peer Support” in which all participants are seen to benefit from learning from each other [37]. The role of a teacher or coach is seen as contradicting this core value when peers are viewed as more skilled or experienced than participants. Interestingly, although the peer health coaches reported feeling uncomfortable providing “coaching” (as opposed to support), participants did not express concerns about the peers’ role in the program and instead noted the benefits of the peer modeling healthy behaviors and providing ideas for getting more exercise and improving eating habits.
These contrasting perspectives may reflect a long-standing debate among peer support advocates about the appropriate role for peers, particularly as peers have assumed paid roles within the mental health system as service providers where patient outcomes are routinely monitored [34, 38]. This issue has been characterized as weighing the comparative merits of complete reciprocity in contrast to asymmetrical relationships that are professionally oriented (presenting the advantage of eligibility for Medicaid reimbursement) in which there is a designated peer service provider and a designated client who is a service recipient. A hybrid variation of this professionalized peer role proposed by Swarbrick and colleagues consists of “wellness coaching” role that assumes that most peers in recovery will need to develop specialized health-related knowledge and coaching skills in order to adopt the role of a paid wellness coach [39]. Based on our initial feasibility study, a collaborative coaching and learning model may occupy a middle ground where peers help guide participants to develop and obtain healthy lifestyle goals while leading activities that offer direct experiences in healthy eating (e.g., grocery shopping, cooking) and exercise (e.g., walking, group fitness classes). This hybrid role consisting of coaching and peer support may provide the right combination of reciprocity and targeted support to achieve clinically significant cardiovascular risk reduction in individuals with SMI.
A possible explanation for the observed low attendance in the peer-led groups may reflect an unintentional consequence of the sequential design of the PeerFIT program. The group-based exercise activities were introduced during the final phase, at the conclusion of the series of individual fitness trainer sessions. It is possible that participants perceived the shift to peer-led group exercise as a loss (rather than a gain) following a significant period of receiving one-on-one coaching with a professional fitness trainer. In a prior qualitative study of In SHAPE, participants reported that a personal connection with a fitness trainer was a major incentive to exercise [40]. Future modifications to the PeerFIT intervention will explore introducing peer-led group exercise at the beginning of the program as a complementary component, rather than as a replacement for activities with a fitness trainer. A prior study of group-based behavioral weight management for adults with SMI reported low participation rates in exercise groups, with participation decreasing over the course of the intervention [5]. Alternative physical activity interventions could focus on increasing the amount of planned activity and exercise in participants’ setting of choice (e.g., home, neighborhood, gym), using activity tracking devices to increase motivation and facilitate social support for individual and group goals.
As we have reported previously, the mobile health technology component of the PeerFIT program emerged as feasible and highly acceptable to participants [24]. This was reflected by the sustained use of the wearable activity tracking devices and smartphones over the entire duration of the intervention as well as participants’ high satisfaction with using the devices and comments that the devices were both motivating and helped facilitate goal setting [24]. Consistent with prior studies highlighting the benefits of supportive and tailored text messages [41–43], participants found that the personalized text messages from their peer health coaches were useful and motivating. Through the smartphone applications for each device, peer health coaches could check on participants’ exercise progress remotely and at any time of the day, and then tailor supportive text messages according to participants’ individual needs. Similar peer-to-peer communication techniques involving real-time data collected using mobile devices and shared through a smartphone application interface are currently being evaluated in a weight loss intervention in the early stages of development [44]. Mobile health technology facilitates interactions among peers and promotes positive health behavior change without relying on face-to-face encounters. We found that mobile health technologies designed for the general population are not only feasible for use among this high-risk patient group [24], but appear to be useful tools for facilitating peer support activities towards positive health behavior change.
Limitations
This was an initial pilot study of the feasibility to examine the feasibility of a novel approach to be further studied in a larger scale trial. Consistent with the intent of a pilot feasibility study, our study was not designed to evaluate the potential efficacy of the PeerFIT intervention. The primary purpose was to understand the user’s experience with the intervention in order to identify areas for future refinement. The sample size was small, involving volunteers that were self-selected. In addition, the peer coaches and participants were representative of the regional population in rural New Hampshire, and our sample was limited by a lack of racial/ethnic diversity. Feasibility results do not necessarily generalize beyond the inclusion and exclusion criteria of the pilot design and should be interpreted with caution. Despite these limitations, a unique strength of this study was the exploration of feasibility from the perspective of stakeholder groups. Using a mixed methods intervention framework allowed us to study in depth how participants and providers experienced the multi-component intervention and explore their recommendations for refinements to the model.
CONCLUSION
Peer support and mobile health technologies are promising strategies for increasing the effectiveness of health promotion interventions for individuals with SMI. This study provides preliminary evidence that peer health coaching and mobile health technology is not only feasible in individuals with SMI but also that participants found the program to be useful and helpful in supporting their behavior change process. Qualitative reports noted several successful changes participants had made in exercise and healthy eating. Future refinements to the model should include a greater emphasis on mutuality and reciprocal learning among peers and additional opportunities for participants to support one another’s exercise goals with the introduction of peer-led group exercise at the beginning of the intervention.
References
Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006; 3(2): A42.
Scott D, Happell B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Ment Health Nurs. 2011; 32(9): 589-597.
Bartels SJ, Pratt SI, Aschbrenner KA, et al. Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatr Serv. 2013; 64(8): 729-736.
Cabassa LJ, Ezell JM, Lewis-Fernandez R. Lifestyle interventions for adults with serious mental illness: a systematic literature review. Psychiatr Serv. 2010; 61(8): 774-782.
Daumit GL, Dickerson FB, Wang NY, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013; 368(17): 1594-1602.
Cohn T, Grant S, Faulkner GE. Schizophrenia and obesity: addressing obesogenic environments in mental health settings. Schizophr Res. 2010; 121(1–3): 277-278.
Sazlina SG, Browning C, Yasin S. Interventions to promote physical activity in older people with type 2 diabetes mellitus: a systematic review. Front Public Health. 2013; 1: 71.
Baksi AK. Experiences in peer-to-peer training in diabetes mellitus: challenges and implications. Fam Pract. 2010; 27(Suppl 1): i40-i45.
Moskowitz D, Thom DH, Hessler D, Ghorob A, Bodenheimer T. Peer coaching to improve diabetes self-management: which patients benefit most? J Gen Intern Med. 2013; 28(7): 938-942.
Clark AM, Munday C, McLaughlin D, Catto S, McLaren A, Macintyre PD. Peer support to promote physical activity after completion of centre-based cardiac rehabilitation: evaluation of access and effects. Eur J Cardiovasc Nurs. 2012; 11(4): 388-395.
Thom DH, Ghorob A, Hessler D, De Vore D, Chen E, Bodenheimer TA. Impact of peer health coaching on glycemic control in low-income patients with diabetes: a randomized controlled trial. Ann Fam Med. 2013; 11(2): 137-144.
Ginis KAM, Nigg CR, Smith AL. Peer-delivered physical activity interventions: an overlooked opportunity for physical activity promotion. Transl Behav Med. 2013; 3(4): 434-443.
Imanaka M, Ando M, Kitamura T, Kawamura T. Effectiveness of web-based self-disclosure peer-to-peer support for weight loss: randomized controlled trial. J Med Internet Res. 2013; 15(7): e136.
Leahey TM, Wing RR. A randomized controlled pilot study testing three types of health coaches for obesity treatment: professional, peer, and mentor. Obesity. 2013; 21(5): 928-934.
Gray CM, Hunt K, Mutrie N, et al. Football fans in training: the development and optimization of an intervention delivered through professional sports clubs to help men lose weight, become more active and adopt healthier eating habits. BMC Public Health. 2013; 13: 232.
Wong-Rieger D, Rieger FP. Health coaching in diabetes: empowering patients to self-manage. Can J Diabetes. 2013; 37(1): 41-44.
Druss BG, Zhao L, von Esenwein SA, et al. The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophr Res. 2010; 118(1–3): 264-270.
Goldberg RW, Dickerson F, Lucksted A, et al. Living well: an intervention to improve self-management of medical illness for individuals with serious mental illness. Psychiatr Serv. 2013; 64(1): 51-57.
Bartels SJ, Aschbrenner KA, Rolin SA, Hendrick DC, Naslund JA, Faber MJ. Activating older adults with serious mental illness for collaborative primary care visits. Psychiatr Rehabil J. 2013; 36(4): 278-288.
Kelly E, Fulginiti A, Pahwa R, Tallen L, Duan L, Brekke JS. A pilot test of a peer navigator intervention for improving the health of individuals with serious mental illness. Community Ment Health J. 2014; 50(4): 435-446.
Van Citters AD, Pratt SI, Jue K, et al. A pilot evaluation of the In SHAPE individualized health promotion intervention for adults with mental illness. Community Ment Health J. 2010; 46(6): 540-552.
Bartels SJ, Pratt SI, Aschbrenner KA, et al. Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. Am J Psychiatry. In Press.
SAMHSA-HRSA Center for Integrated Health Solutions. WHAM: Whole Health Action Management: peer support training participant guide. http://www.integration.samhsa.gov.
Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ. Feasibility of popular mHealth technologies for activity tracking among individuals with serious mental illness. Telemed e-Health. In Press.
Eyles C, Leydon G, Hoffman C, Copson E, Prescott P, Lewith G. Mindfulness for the fatigue, anxiety and depression in women with metastatic breast cancer: a mixed method feasibility study. J Altern Complement Med. 2014; 20(5): A60.
Smith JD, Baillie J, Baglin T, et al. A feasibility study to inform the design of a randomized controlled trial to identify the most clinically and cost effective anticoagulation length with low molecular weight heparin in the treatment of cancer associated thrombosis (ALICAT): study protocol for a mixed-methods study. Trials. 2014; 15: 122.
Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009; 36(5): 452-457.
Krueger RA. Focus groups: a practical guide for applied research. Thousand Oaks, CA: Sage; 1994.
Beebe J. Rapid assessment process: an introduction. Walnut Creek, CA: Altamira Press; 2001.
Solomon P. Rapid assessment of existing HIV prevention programming in a community mental health center. J Prev Interv Commun. 2007; 33(1–2): 137-151.
Miles M, Huberman M. Qualitative data analysis: an expanded sourcebook. 2nd ed. Thousand Oaks, CA: Sage; 1994.
Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002; 12(6): 855-866.
Williams JM, Dwyer M, Verna M, et al. Evaluation of the CHOICES program of peer-to-peer tobacco education and advocacy. Community Ment Health J. 2011; 47(3): 243-251.
Davidson L, Chinman M, Sells D, Rowe M. Peer support among adults with serious mental illness: a report from the field. Schizophr Bull. 2006; 32(3): 443-450.
Davidson L, Bellamy C, Guy K, Miller R. Peer support among persons with severe mental illnesses: a review of evidence and experience. World Psychiatry Off J World Psychiatr Assoc (WPA). 2012; 11(2): 123-128.
Chinman M, George P, Dougherty RH, et al. Peer support services for individuals with serious mental illnesses: assessing the evidence. Psychiatr Serv. 2014; 65(4): 429-441.
Mead S, Hilton D, Curtis L. Peer support: a theoretical perspective. Psychiatr Rehabil J. 2001; 25(2): 134-141.
Davidson L, O'Connell M, Tondora J, Styron T, Kangas K. The top ten concerns about recovery encountered in mental health system transformation. Psychiatr Serv. 2006; 57(5): 640-645.
Swarbrick M, Murphy AA, Zechner M, Spagnolo AB, Gill KJ. Wellness coaching: a new role for peers. Psychiatr Rehabil J. 2011; 34(4): 328-331.
Shiner B, Whitley R, Van Citters AD, Pratt SI, Bartels SJ. Learning what matters for patients: qualitative evaluation of a health promotion program for those with serious mental illness. Health Promot Int. 2008; 23(3): 275-282.
Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev. 2010; 32(1): 56-69.
Woolford SJ, Barr KL, Derry HA, et al. OMG do not say LOL: obese adolescents' perspectives on the content of text messages to enhance weight loss efforts. Obesity. 2011; 19(12): 2382-2387.
Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013; 21(1): 25-31.
Pellegrini CA, Duncan JM, Moller AC, et al. A smartphone-supported weight loss program: design of the ENGAGED randomized controlled trial. BMC Public Health. 2012; 12(1): 1041.
Acknowledgments
This study was funded by grants from the National Institute of Mental Health (Grant number NIMH R01 MH089811) and the Agency for Healthcare Quality and Research (Grant number K12 HS021695-01). SB and KA were supported by the Health Promotion Research Center at Dartmouth supported by Cooperative Agreement Number U48DP005018 from the Centers for Disease Control and Prevention. The funders played no role in the design, conduct, or analysis of the study nor in the interpretation and reporting of the study findings.
Conflict of interest
All authors declare that they have no conflict of interest.
Adherence to ethical principles
All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice: Peer health coaching is a promising model for supporting health behavior change among individuals with serious mental illness.
Policy: Peer-led health promotion may offer innovative, cost-effective, and scalable interventions that require less intensive resources while delivering effective behavior change strategies that reach a greater proportion of at-risk individuals with serious mental illness
Research: Research is needed to evaluate the potential effectiveness of peer health coaching interventions for promoting fitness and weight loss among individuals with serious mental illness.
About this article
Cite this article
Aschbrenner, K.A., Naslund, J.A., Barre, L.K. et al. Peer health coaching for overweight and obese individuals with serious mental illness: intervention development and initial feasibility study. Behav. Med. Pract. Policy Res. 5, 277–284 (2015). https://doi.org/10.1007/s13142-015-0313-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-015-0313-4