Abstract
Effective and scalable lifestyle interventions are needed to address high rates of obesity in people with serious mental illness (SMI). This pilot study evaluated the feasibility of a behavioral weight loss intervention enhanced with peer support and mobile health (mHealth) technology for obese individuals with SMI. The Diabetes Prevention Program Group Lifestyle Balance intervention enhanced with peer support and mHealth technology was implemented in a community mental health setting. Thirteen obese individuals with SMI participated in a pre-post pilot study of the 24-week intervention. Feasibility was assessed by program attendance, and participant satisfaction and suggestions for improving the model. Descriptive changes in weight and fitness were also explored. Overall attendance amounted to approximately half (56 %) of weekly sessions. At 6-month follow-up, 45 % of participants had lost weight, and 45 % showed improved fitness by increasing their walking distance. Participants suggested a number of modifications to increase the relevance of the intervention for people with SMI, including less didactic instruction and more active learning, a simplified dietary component, more in depth technology training, and greater attention to mental health. The principles of standard behavioral weight loss treatment provide a useful starting point for promoting weight loss in people with SMI. However, adaptions to standard weight loss curricula are needed to enhance engagement, participation, and outcomes to respond to the unique challenges of individuals with SMI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The epidemic of obesity is affecting individuals with serious mental illness (SMI), including schizophrenia, schizoaffective disorder, major depressive disorder, and bipolar disorder, at alarming levels. Obesity rates are nearly twice as high in people with SMI compared to the general population; nearly 60 % of individuals with SMI are classified as obese (BMI ≥ 30) [1]. Psychiatric medications are frequently cited as the cause of weight gain [2], but lifestyle behaviors are also a major contributor to obesity in this population [3]. Many individuals with SMI want to eat more healthily and be more physically active, and there is evidence that lifestyle interventions lead to modest weight loss in people with SMI [4, 5]. However, individuals with SMI encounter considerable barriers to weight loss, including the impact of psychiatric symptoms on motivation, difficulty finding affordable healthy foods and supported exercise options, and a lack of social support for lifestyle change [6, 7]. In addition, widespread dissemination and implementation of evidence-based practices for healthy lifestyle change has not yet happened in mental health settings. There is a critical need for pragmatic and scalable behavioral interventions that effectively address obesity in individuals with SMI.
Successful behavioral weight loss programs for people without mental illness have been translated from clinical trials to community settings and implemented across diverse populations [8]. The Diabetes Prevention Program (DPP) trial is considered a gold standard in behavioral weight management research in the general population. In a large randomized trial, half of participants receiving this lifestyle intervention achieved over 7 % weight loss [9]. The DPP curriculum, which focuses on goal setting, problem solving, and persistence of weight loss efforts is the most widely replicated model for behavioral weight loss in the United States [10].
Adapting existing evidenced-based weight loss interventions such as the DPP could be a successful and scalable strategy for meeting the needs of individuals with SMI and obesity. However, there are substantial challenges that need to be addressed in any adaptation for this high-risk group. First, individuals with SMI are likely to require intensive behavioral measures and additional support to achieve sustainable and clinically significant health behavior change. In contrast, the intensity and time typically allotted for behavioral weight loss interventions is likely to be inadequate to provide the emotional and informational support needed to help individuals with SMI change lifelong health habits [6]. Engaging peer support in lifestyle interventions could be an adaptation that might increase the intensity and relevance of lifestyle interventions for persons with SMI and obesity. Peer support, defined as support from people with the same health conditions who share their own experiences and coping strategies to support others, is an effective strategy for managing chronic conditions [11–13], and recent research indicates its potential for promoting weight loss in the general population [14–16]. Many of the core principles of peer support in mental health recovery (e.g., instilling hope, expressing empathy, social modeling) have direct relevance for helping to motivate and empower obese individuals with SMI to better manage their weight. Peer support could be a potentially potent adjunct to behavioral weight loss treatment for individuals with SMI.
A second feature of behavioral interventions for persons with SMI is the need to provide frequent prompting, reminders, self-monitoring, and positive motivation to achieve sustained health behavior change. Mobile health (mHealth) technology using sensors, smartphones, and text messaging has the potential to enhance the daily presence and reach of time-limited behavioral weight loss treatment sessions. Professionals and peers could potentially help participants sustain motivation and address challenges to healthy eating and exercise in their natural environments through smart devices and wearable technologies. Approximately 72 % of individuals with SMI report owning a mobile phone [17], and mobile phones with internet connection (smartphones) are being used to help people with SMI monitor and self-manage their psychiatric symptoms [18, 19]. Recent reviews of the literature have highlighted that various mobile and web-based platforms, including social media websites and smartphone applications, are acceptable for targeting people with SMI [20, 21]. There is also evidence that popular wearable activity tracking devices are feasible and desirable among people with SMI [22]. The progressively reduced costs and increasingly widespread accessibility to mHealth technologies opens up the possibility of using existing technologies to augment standard behavioral weight loss treatment for people with SMI.
The objective of this pilot study was to evaluate the feasibility of adapting a standard behavioral weight loss treatment (DPP) for obese persons with SMI by increasing the intensity, accessibility, and presence of lifestyle interventions through peer support and mHealth technology. Feasibility was assessed by program participation, and by examining participant satisfaction with the program and suggestions for improving the model. Descriptive changes in weight and fitness were also explored. Consistent with the National Institutes of Health (NIH) Stage Model for behavioral intervention development this small-scale feasibility study was a first step in treatment generation and refinement [23]. The overall goal of this stage of research was to identify any modifications needed to further adapt components of the intervention for people with SMI in preparation for a larger pilot study exploring its potential efficacy.
Methods
Participants
This study was conducted in collaboration with an urban community mental health center located in southern New Hampshire. Thirteen obese individuals with SMI participated in this study. Participants were age 21 or older; had SMI defined by an axis I diagnosis of schizophrenia, schizoaffective disorder, major depressive disorder, or bipolar disorder (based on the Structured Clinical Interview for DSM–IV); and had obesity defined as body mass index (BMI) ≥30. Participants received medical clearance from a primary care provider to participate in the exercise component of the program. Participants were required to be on stable pharmacological treatment defined as receiving the same psychiatric medications over the prior 2 months. Exclusion criteria were: residing in a nursing home or other institution; primary diagnosis of dementia or significant cognitive impairment defined as a Mini Mental Status Exam [24] score <24; inability to walk one city block; pregnant or planning to become pregnant within the next 18 months; inability to speak English; terminal illness with mortality expected within 1 year; or current diagnosis of an active substance dependence disorder.
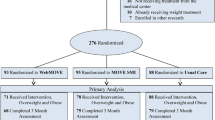
Study Procedures
Recruitment occurred between July and October 2014. Clinical staff identified 29 people who were appropriate candidates and who agreed to be contacted for research. Eight of those contacted were not interested. Two individuals were excluded from the study because they did not have reliable transportation, two were excluded due to enrollment in another weight management and fitness study, two were excluded for medical reasons, one was excluded because he did not meet the BMI criteria, and one individual moved before the program began. Committees for the Protection of Human Subjects at Dartmouth College and the New Hampshire Department of Health and Human Services approved all study procedures. Informed consent was obtained from all participants. Participants were paid for completing pre- and post-intervention assessments, but not for enrolling in the behavioral weight loss program. We used a mixed-method exploratory design with quantitative and qualitative data collected concurrently to inform future enhancements to the intervention design [25]. Quantitative assessments of participant satisfaction and pre-post descriptive outcomes of weight and fitness were conducted at baseline and 6-month follow-up. In-depth qualitative interviews exploring the acceptability of the intervention from participants’ perspective were also conducted at 6-month follow-up.
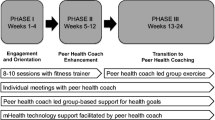
Intervention Design
The 24-week enhanced behavioral weight loss intervention consisted of the following: (a) once weekly 90-minute weight management group sessions taught by two lifestyle coaches and supported by a wellness peer; (b) twice weekly optional 1-hour group exercise sessions led by a certified fitness trainer; and (c) mHealth technology and social media to increase motivation and facilitate self-monitoring and peer support outside of treatment sessions. The weight management component was modeled on the evidence-based Diabetes Prevention Program Group Lifestyle Balance intervention (GLB) [26]. The goals of the GLB program are to achieve a 7 % weight reduction and to increase physical activity gradually to 150 min/week over a 6-month period. The GLB program focuses on weight loss through healthy eating and physical activity and was originally designed for individuals at risk for diabetes and cardiovascular disease in the general population. Our study team agreed to make minimal changes to the GLB protocol rather than assume that some aspects of a standard behavioral weight loss treatment may be inappropriate or too difficult for individuals with SMI. We added content addressing the impact of mood on health behaviors and strategies for overcoming barriers to change for people with SMI.
Participants were taught standard behavioral weight loss techniques, including goal setting, problem solving, and strategies for preventing lapses such as temporary or small slips in weight loss efforts. Self-monitoring dietary intake and physical activity were the primary strategies for behavior change. Participants were weighed privately at the start of every session and were encouraged to weigh themselves at home daily. A major focus of the GLB curriculum is on calorie balance and the need to restrict calories as well as reduce fat intake. At the beginning of the program every participant was given a calorie goal calculated by estimating the daily calories needed to maintain their starting weight and subtracting 500–1000 calories/day to achieve a 1–2 pound per week weight loss. The fat goals, given in grams of fat per day, were based on consuming only 25 % of total daily calories from fat. Participants were taught to track fat and calorie intake each day using a nutrient counter with the fat gram and calorie content of household portions and restaurant items, and a pocket sized booklet with spaces for recording 7 days of food intake with fat and calorie values.
Two mental health counseling graduate students delivered the weight management sessions as certified GLB lifestyle coaches. The lifestyle coaches participated in a 2-day GLB Lifestyle Coach training workshop where they received instruction on healthy eating and nutrition and skills training to implement and deliver the GLB curriculum. Throughout the study, the lifestyle coaches received 1-h weekly supervision from a mental health nurse practitioner and ongoing consultation from a registered dietician who provided dietary counseling during several group sessions. Fidelity to the GLB protocol was monitored through observation at each session by the study principal investigator (KA) who also received training and certification to deliver the program and was also involved in the supervision of the lifestyle coaches.
The intervention included support from a wellness peer who was an individual with SMI who had previously participated in a healthy lifestyle intervention and was highly recommended by the community mental health center. The role of the wellness peer was to help facilitate activities and small group discussions, and to engage as a co-learner to enhance peer-participant collaboration. The wellness peer was encouraged to share her own experiences with dietary change and increasing physical activity, including challenges as well as successes. The wellness peer’s role was designed to complement and extend professional weight management instruction by facilitating emotional (e.g., praise and encouragement), appraisal (e.g., feedback and social comparison), and informational (e.g., advice and suggestions) support to help participants change lifelong health habits.
A certified personal trainer led twice weekly group exercise sessions. Group exercise started at a level appropriate for sedentary persons, with gradual increases in duration and intensity. The group exercise sessions were an optional adjunct to the required core weight management sessions and intended to provide participants with an opportunity to reach their weekly physical activity goals.
Technology Support
As part of the mHealth support component, participants were provided Fitbit wearable activity tracking devices and Apple iPhone smartphones to use for the duration of the study. The primary purpose of the mHealth technologies were to keep participants engaged in the intervention, promote adherence to the intervention, facilitate self-monitoring, and provide ongoing motivation and support outside regular treatment sessions towards reaching the program weight loss and physical activity goals. The Fitbit wearable activity tracking devices (Fitbit Zip) were intended to facilitate self-monitoring of unstructured physical activity throughout the day and motivate participants to be more active in their daily routines. The Fitbit Zip device is a compact wearable accelerometer that easily clips onto participants’ clothing, and tracks number of steps and distance in miles, and syncs wirelessly with a free companion smartphone application available on the iPhone. The Fitbit rewards milestones such as reaching daily step goals with colorful trophies or animations, and allows users to compare steps and progress with others through the smartphone application interface. We elected to use Fitbit wearable activity tracking devices because in our previous research we found that these devices are feasible for use in this population, and that participants find them motivational and fun to use [22].
To promote program attendance, participants were sent regular text messages from research staff as reminders to attend the weekly weight management group sessions and the two optional exercise classes each week. Additional text messages were also sent to remind and encourage participants to be more active as part of their daily routines, and to support participants in reaching the program physical activity goal of 150 min of physical activity each week. Participants attended two brief 30-min training sessions with a member of the research staff (JN) for instruction in using the Fitbit wearable activity tracking devices, syncing the Fitbit with the companion mobile application, and sending and receiving text messages using the smartphone.
At week 10 of the program, participants were introduced to a Facebook group. The Facebook group was aimed at promoting the GLB program content, keeping participants interested in the program, and providing participants with a way to interact and share personal successes and healthy eating and exercise tips outside of regular group sessions. The Facebook group was accessible only to participants enrolled in this study, and was monitored for safety and appropriate content daily by a member of the research team (JN). We also regularly posted content supporting the weekly lessons from the GLB group weight management classes onto to the Facebook group. Participants received additional instruction about how to access and post content to the Facebook page through a mobile application downloaded to their study smartphones. Additional details regarding the feasibility and acceptability of using Facebook to support this intervention are reported elsewhere [27]. Technical support for using the Fitbits or smartphones was provided to participants on an as needed basis by a member of the research team (JN) over the duration of the program.
Study Measures
Quantitative measures of feasibility included program attendance, participant satisfaction, and descriptive outcomes including weight and cardiorespiratory fitness. A research assistant tracked attendance during weekly weight management and exercise sessions throughout the 24-week program. Participant satisfaction with the program was assessed using a participant satisfaction questionnaire adapted from a prior feasibility study of a psychosocial intervention for individuals with SMI [28], which was designed to measure perceived satisfaction, usefulness, and ease of learning. Participants rated their level of satisfaction for 17-questions referring to various program components (“The exercise groups were useful”, “The peer leaders in the program were helpful”) using a 5-point Likert rating scale (1 = “strongly disagree” to 3 = “strongly agree”). At each visit, weight was measured in pounds (lbs) on a flat, even surface with the use of a high-quality, calibrated digital scale, with the participant wearing indoor clothing and no shoes. Cardiorespiratory fitness was assessed by the 6-min Walk Test (6-MWT), which measures the distance an individual can walk in 6 min [29]. In obese adults, the 6-MWT is a reliable and valid measure of cardiovascular fitness with favorable test-retest and discriminant validity, and has been used in adults with a variety of chronic health conditions [30, 31]. An increase in distance of >50 meters is associated with clinically significant reduction in risk for cardiovascular disease [32]. Clinically significant cardiovascular risk reduction was assessed by either a ≥5 % weight loss or >50 m increase on the 6-min Walk Test.
Participant Feedback Interviews
We conducted in-depth qualitative interviews with each participant to further explore their experiences with the program, including perceived benefits and challenges of participation, and suggested modifications to improve specific components of the intervention (e.g., dietary self-monitoring, exercise sessions, group-based activities, wellness peer support). A research interviewer who was not involved in delivering the intervention was trained and supervised by the study principal investigator (KA), an experienced qualitative researcher, to conduct the 1-h in-depth participant feedback interviews. All interviews were audiotaped and transcribed verbatim for thematic analysis.
Data Analysis
Descriptive statistics, including means and frequencies, were used to summarize program attendance, participant satisfaction ratings, and descriptive outcomes including weight and cardiorespiratory fitness. Statistical analyses were performed using SPSS software, version 20.0. We analyzed text message transcripts using thematic analysis, which is a method for identifying, analyzing, and reporting key themes within data [33]. Two members of our research team (KA & JN) used a template with primary domains from the qualitative interview guide to independently review each of the transcripts. We then created a table of key findings by respondent and domain that allowed us to synthesize important findings by noting similarities, differences, and trends across respondents. The researchers summarized key participant feedback within each domain. A targeted and explanatory approach to qualitative analysis is particularly useful when there is a pragmatic need for data, as is the case with formative research used to develop and refine an intervention prior to a larger trial [34, 35].
Results
The 13 participants were individuals with SMI (n = 3 schizophrenia; n = 3 bipolar disorder; n = 7 major depression) ranging in age from 21 to 58 years (mean 48.8; SD = 10.6) with a mean weight of 243.5 lbs (SD = 53.1 lbs) and mean body mass index of 41.5 kg/m2 (SD = 11.5 kg/m2). The majority of participants (77 %) were dual eligible beneficiaries covered by both Medicaid and Medicare. The complete list of participant background characteristics is presented in Table 1. Follow-up data was completed for 85 % of participants (N=11) at 6 months. One participant conducted the baseline assessment but never attended one session, and another left the study after attending one session citing scheduling conflicts with family and work obligations. The average number of weight management sessions attended was 13.5 (SD = 4.6) out of 24. The overall attendance rate was 56 %, with a 79 % attendance rate during the first 12 weeks and dropping to 33 % during weeks 13–24. The average number of optional exercise group sessions attended was 10 (SD = 10.6) out of 45.
There were no overall significant changes in mean weight or fitness. At 6-month follow-up, nearly half (45 %) of participants were below their baseline weight and 45 % improved their cardiorespiratory fitness by increasing their walking distance on the 6-MWT. One-third (36 %) of participants met the criteria for clinically significant cardiovascular risk reduction (defined as ≥5 % weight loss or >50 m increase on the 6-MWT). The majority of participants (89 %) reported satisfaction with the program (Table 2), the majority agreed that the activities were useful (89 %), and over three-quarters (78 %) reported that the program helped them make progress toward their health goals.
Participant Feedback Interviews
The primary themes from the participant feedback interviews are summarized in Table 3. Perceived program benefits included nutrition education and strategies for healthy eating, self-monitoring dietary intake to help with portion control, fun and reinforcing group exercise sessions, group support for motivating health behavior change, and positive role modeling and support by the wellness peer. Perceived challenges included too much didactic instruction with little opportunity for participants to interact with one another, intensive dietary tracking that was complex, inconvenient and unsustainable in daily life, weekly self-weighing that often felt more discouraging than helpful, and mental health symptoms that interfered with behavior change.
Many of the participants’ suggested modifications to the program were closely aligned with the challenges they identified with participating in the program. Participants suggested we include more active and engaging learning activities and opportunities for participants to interact with each another. They suggested we focus more on overall positive changes to dietary behavior (e.g., “more balanced meals”) and less on counting calories and fat. Several participants suggested we add grocery shopping tips and cooking skills training to the program. Many participants also commented that the program should address in more depth how mental health symptoms relate to and impact lifestyle change, and how to cope with symptoms that interfere with the change process. Finally, several participants felt it would be helpful if wellness peers could share more of their personal challenges and successes with weight loss and focus less on giving participants’ advice for behavior change.
Discussion
The objective of this pilot study was to evaluate the feasibility of a standard behavioral weight loss treatment enhanced with peer support and mHealth technology for obese individuals with SMI. The results of this early stage research suggest that the principles of standard behavioral weight loss treatment provide a useful starting point for promoting weight loss in people with SMI. However, adaptions to treatment curricula developed for the general population appear to be necessary to address the unique challenges of individuals with SMI who are trying to lose weight. Participants reported a number of perceived benefits from the program, including group support for motivating health behavior change and role modeling and support by the wellness peer. At 6-months, 45 % of participants were below their baseline weight and 45 % improved their fitness through increased walking distance. The attendance rate (56 %) was poor for weekly weight management sessions. Participants suggested a number of modifications to improve the intervention, including greater attention to the impact of mental health symptoms on behavior change. Our results align with prior studies demonstrating the need to modify standard behavioral approaches to weight loss treatment to address the unique challenges of people with SMI who are trying to lose weight [36, 37].
Didactic instruction alone is highly unlikely to be a successful approach to increasing personal motivation and self-efficacy to change health behaviors, particularly for people with SMI who experience information processing challenges in attention, concentration, and memory [38]. Several participants commented that the weight management sessions involved a lot of “lectures” with little opportunity to interact with other participants. Future research should explore different approaches to engaging people with SMI in the learning process by incorporating more discussion, active learning, collaborative work, and problem-based learning. While both psychiatric rehabilitation and behavioral weight loss treatment frequently use group formats to deliver interventions, limited research has explicitly focused on evaluating the use of theories and principles to guide group instruction and social learning in healthy lifestyle interventions for people with SMI. Active and collaborative learning techniques that involve “learning by doing” may be particularly potent for people with SMI who are learning to change lifestyle habits over more traditional teaching methods where participants passively receive health information.
Social cognitive theory (SCT) is a relevant framework for studying the application of active and collaborative learning concepts to promote health behavior change in people with SMI. SCT focuses on increasing the personal self-efficacy needed to adopt new lifestyle habits in large part through social modeling and social support [39]. Behavioral weight loss interventions for people with SMI guided by a SCT framework could include group-based instructional methods where participants work together to discuss concepts, solve problems, and actively learn to change exercise and eating behaviors through new experiences introduced during group sessions. Participants in this pilot study wanted more opportunities to interact with each other, and several participants felt it would be helpful if wellness peers could share more of their own challenges and successes with weight loss and focus less on giving personal advice for behavior change. Both of these suggestions align well with SCT’s principle of social modeling where seeing people similar to oneself succeed is expected to raise participants’ beliefs that they too have the capability to successfully change lifestyle habits.
The challenges of self-monitoring dietary intake experienced by individuals with SMI have been reported elsewhere [36, 37], and continued to present problems in the present study. Several participants reported that intensive dietary tracking was complex, inconvenient, and not sustainable in daily life. While self-monitoring dietary intake is an evidence-based strategy for successful weight loss in people without mental illness [40], prior studies of healthy lifestyle interventions for people with SMI have demonstrated successful weight loss by focusing on other self-regulatory strategies to control eating (e.g., increasing fruit and vegetable consumption rather than a caloric restriction diet) [4, 41]. While self-monitoring dietary intake may be an effective skill for weight loss in highly motivated individuals [42], many people with SMI who are trying to lose weight may benefit more by learning strategies that empower them to make healthy food choices that are less cognitively taxing.
Participants in this pilot study also suggested that the intervention place greater attention on mental health and its impact on health behavior change. Numerous studies have shown that physical activity can improve depression [43] and has positive effects on anxiety [44]. However, mental health symptoms can also be a barrier to being more physically active in the first place and thus symptoms may need to be addressed before starting a new exercise routine, particularly for people who are prone to depression [45]. Teaching participants coping strategies for mental health symptoms that interfere with efforts to change eating and exercise behaviors may be key to increasing their self-efficacy to adopt these new lifestyle habits to lose weight. Future refinements to the intervention should include more in depth attention to the interconnectedness of health and mental health.
Participants were also generally satisfied with the mHealth support component of the intervention. As we report in more detail elsewhere [27, 46], participants expressed high satisfaction with using the Fitbit wearable devices to track their physical activity, and considered Facebook a useful platform for interacting and supporting each other outside regular group sessions. However, participants also agreed that more extensive training was necessary for learning how to use the more complex smartphone devices and mobile applications, for overcoming technical challenges, and for navigating the Facebook website.
The use of mHealth technologies could also effectively support health behavior change by increasing participants’ self-efficacy according to important principles of Social Cognitive Theory. For example, the Fitbit wearable activity tracking devices afford valuable opportunities for building self-confidence in being more physically activity through creating small and measurable tasks that can be easily mastered over time, referred to as “self-mastery” experiences [39], such as setting gradually more challenging daily step goals. We also learned that participants appreciated the text message reminders and found the text messages that encouraged being more physically activity to be particularly helpful and motivating. This is consistent with prior research, where personalized and encouraging text messages appeared beneficial for supporting individuals with psychiatric conditions [47]. Text messaging could also be used to further build self-efficacy according to the Social Cognitive Theory principle of verbal persuasion, by providing personalized encouragement and helping individuals realize they have the capability to make the necessary healthy lifestyle changes to lose weight.
Limitations
There are a number of limitations that are associated with the current study. First, the sample was small, involving only volunteers that were self-selected, and the study was implemented with an uncontrolled design consistent with the intent of a pilot feasibility study [48]. As such, the study was neither designed nor statistically powered to evaluate the effectiveness of the intervention. The primary purpose of this early stage developmental study was to get feedback from participants on the initial version of the behavioral intervention. Future studies with a larger sample size are needed to evaluate the potential of the intervention model in improving health outcomes for persons with SMI. Second, participants were representative of the regional population in New Hampshire, and our sample was limited by a lack of racial/ethnic diversity. Feasibility results do not necessarily generalize beyond the inclusion and exclusion criteria of the pilot design and should be interpreted with caution. Finally, the sample size and design of a pilot study does not allow for determining the feasibility and potential effectiveness of the adapted intervention with respect to the needs and responses of persons with different degrees of obesity and psychiatric diagnoses. Despite these limitations, a unique strength of this study was the exploration of feasibility from the perspective of participants. Using a mixed methods interventional framework allowed us to study in depth how participants experienced the multi-component intervention and explore their recommendations for future refinements to the model.
Conclusion
The results of this early stage research suggest that the principles of standard behavioral weight loss treatment provide a useful starting point for promoting weight loss in people with SMI. However, substantial adaptions to treatment curriculum developed for the general population will be needed in order to successfully address the unique challenges of individuals with SMI who are trying to lose weight. Future development of this model should focus on active and collaborative learning techniques, simplified self-regulatory skills to control eating, additional technology training, and greater attention to mental health and its impact on health behavior change. Principles of Social Cognitive Theory offer important insight for guiding future multi-component behavioral weight loss interventions combining peer support and mHealth technology for reaching and engaging this at-risk group.
References
Scott D, Happell B: The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues in Mental Health Nursing 32:589–597, 2011
Manu P, Dima L, Shulman M, Vancampfort D, De Hert M, Correll CU: Weight gain and obesity in schizophrenia: epidemiology, pathobiology, and management. Acta Psychiatrica Scandinavica, 2015. doi:10.1111/acps.12445.
Laursen TM, Nordentoft M, Mortensen PB: Excess early mortality in schizophrenia. Annual Review of Clinical Psychology 10:425–448, 2014. doi:10.1146/annurev-clinpsy-032813-153657
Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Naslund JA, Wolfe R, et al.: Pragmatic replication trial of health promotion coaching for obesity in serious mental illness and maintenance of outcomes. The American Journal of Psychiatry 172:344–352, 2015. doi:10.1176/appi.ajp.2014.14030357
Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, et al: A behavioral weight-loss intervention in persons with serious mental illness. The New England Journal of Medicine 368:1594–1602, 2013. doi:10.1056/NEJMoa1214530
Yarborough BJ, Stumbo SP, Yarborough MT, Young TJ, Green CA. Improving Lifestyle Interventions for People With Serious Mental Illnesses: Qualitative Results From the STRIDE Study. Psychiatric Rehabilitation Journal, 2015. doi:10.1037/prj0000151.
Aschbrenner K, Carpenter-Song E, Mueser K, Kinney A, Pratt S, Bartels S: A qualitative study of social facilitators and barriers to health behavior change among persons with serious mental illness. Community Mental Health Journal 49:207–212, 2013. doi:10.1007/s10597-012-9552-8.
Venditti EM, Kramer MK: Diabetes Prevention Program Community Outreach Perspectives on Lifestyle Training and Translation. American Journal of Preventive Medicine 44:S339–S345, 2013. doi:10.1016/j.amepre.2012.12.014.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al.: Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine 346:393–403, 2002. doi:10.1056/NEJMoa012512.
Ali MK, Echouffo-Tcheugui J, Williamson DF: How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health affairs (Project Hope). 31:67–75, 2012. doi:10.1377/hlthaff.2011.1009.
Piette JD, Resnicow K, Choi H, Heisler M: A diabetes peer support intervention that improved glycemic control: mediators and moderators of intervention effectiveness. Chronic Illness 9:258–267, 2013. doi:10.1177/1742395313476522.
Moskowitz D, Thom DH, Hessler D, Ghorob A, Bodenheimer T: Peer coaching to improve diabetes self-management: which patients benefit most? Journal of General Internal Medicine 28:938–942, 2013. doi:10.1007/s11606-013-2367-7.
Druss BG, Zhao L, von Esenwein SA, Bona JR, Fricks L, Jenkins-Tucker S, et al.: The Health and Recovery Peer (HARP) Program: a peer-led intervention to improve medical self-management for persons with serious mental illness. Schizophrenia Research 118:264–270, 2010. doi:10.1016/j.schres.2010.01.026.
Leahey TM, Kumar R, Weinberg BM, Wing RR: Teammates and social influence affect weight loss outcomes in a team-based weight loss competition. Obesity (Silver Spring, Md) 20:1413–1418, 2012. doi:10.1038/oby.2012.18.
Leahey TM, Wing RR: A randomized controlled pilot study testing three types of health coaches for obesity treatment: Professional, peer, and mentor. Obesity (Silver Spring, Md) 21:928–934, 2013. doi:10.1002/oby.20271; 10.1038/oby.2012.179.
Aschbrenner K, Naslund J, Barre L, Mueser K, Kinney A, Bartels S. Peer health coaching for overweight and obese individuals with serious mental illness: intervention development and initial feasibility study. Translational Behavioral Medicine 1–8, 2015. doi:10.1007/s13142-015-0313-4.
Ben-Zeev D, Davis KE, Kaiser S, Krzsos I, Drake RE: Mobile technologies among people with serious mental illness: opportunities for future services. Administration and Policy in Mental Health 40:340–343, 2013. doi:10.1007/s10488-012-0424-x.
Hidalgo-Mazzei D, Mateu A, Reinares M, Undurraga J, Bonnin Cdel M, Sanchez-Moreno J. et al.: Self-monitoring and psychoeducation in bipolar patients with a smart-phone application (SIMPLe) project: Design, development and studies protocols. BMC Psychiatry 15:52, 2015. doi:10.1186/s12888-015-0437-6.
Faurholt-Jepsen M, Vinberg M, Frost M, Christensen EM, Bardram J, Kessing LV: Daily electronic monitoring of subjective and objective measures of illness activity in bipolar disorder using smartphones–the MONARCA II trial protocol: A randomized controlled single-blind parallel-group trial. BMC Psychiatry 14:309, 2014. doi:10.1186/s12888-014-0309-5.
Alvarez-Jimenez M, Alcazar-Corcoles MA, Gonzalez-Blanch C, Bendall S, McGorry PD, Gleeson JF: Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophrenia Research 156:96–106, 2014. doi:10.1016/j.schres.2014.03.021.
Naslund JA, Marsch LA, McHugo GJ, Bartels SJ: Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. Journal of Mental Health (Abingdon, England) 1–12, 2015. doi:10.3109/09638237.2015.1019054.
Naslund JA, Aschbrenner KA, Barre LK, Bartels SJ: Feasibility of popular m-Health technologies for activity tracking among individuals with serious mental illness. Telemedicine and e-Health 21:213–216, 2015. doi:10.1089/tmj.2014.0105.
Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M: Reenvisioning clinical science: Unifying the discipline to improve the public health. Clinical Psychological Science: A Journal of the Association for Psychological Science 2:22–34, 2014. doi:10.1177/2167702613497932.
Folstein MF, Folstein SE, McHugh PR: Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12:189–198, 1975.
Zhang W: Mixed methods application in health intervention research: A multiple case study. International Journal of Multiple Research Approaches 8:24–35, 2014. doi:10.5172/mra.2014.8.1.24.
Kramer MK, Kriska AM, Venditti EM, Miller RG, Brooks MM, Burke LE, et al.: Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. The American Journal of Preventive Medicine 37:505–511, 2009. doi:10.1016/j.amepre.2009.07.020.
Naslund JA, Aschbrenner K, Bartels S: Acceptability of Facebook for Health Promotion in People with Serious Mental Illness. Under Review.
Meyer PS, Johnson DP, Parks A, Iwanski C, Penn DL: Positive living: A pilot study of group positive psychotherapy for people with schizophrenia. The Journal of Positive Psychology 7:239–248, 2012. doi:10.1080/17439760.2012.677467.
Balke B. A SIMPLE FIELD TEST FOR THE ASSESSMENT OF PHYSICAL FITNESS. REP 63-6. [Report] Civil Aeromedical Research Institute (US) 1–8, 1963.
Larsson UE, Reynisdottir S: The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiotherapy Research International : The Journal for Researchers and Clinicians in Physical Therapy 13:84–93, 2008. doi:10.1002/pri.398.
Beriault K, Carpentier AC, Gagnon C, Menard J, Baillargeon JP, Ardilouze JL, et al: Reproducibility of the 6-minute walk test in obese adults. International Journal of Sports Medicine 30:725–727, 2009. doi:10.1055/s-0029-1231043.
Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, et al.: Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. JAMA 270:1702–1707, 1993.
Braun V, Clarke V: Using thematic analysis in psychology. Qualitative Research in Psychology 3:77–101, 2006. doi:10.1191/1478088706qp063oa.
Solomon P: Rapid assessment of existing HIV prevention programming in a community mental health center. Journal of Prevention & Intervention in the Community 33:137–151, 2007.
Beebe J: Rapid Assessment Process. Walnut Cree, Altamira Press, 2001.
Schneider KL, Sullivan JC, Pagoto SL: Translation of the diabetes prevention program into a community mental health organization for individuals with severe mental illness: a case study. Translational behavioral medicine 1:453–460, 2011. doi:10.1007/s13142-011-0053-z.
Srebnik D, Chwastiak LA, Russo J, Sylla L: A pilot study of the diabetes prevention program on weight loss for adults at community mental health centers. Psychiatric Services (Wash, DC) 66:200-203, 2015. doi:10.1176/appi.ps.201300576.
Trivedi JK: Cognitive deficits in psychiatric disorders: Current status. Indian Journal of Psychiatry 48:10–20, 2006. doi:10.4103/0019-5545.31613.
Bandura A: Health promotion from the perspective of social cognitive theory. Psychology and health 13:623–649, 1998.
Teixeira PJ, Carraca EV, Marques MM, Rutter H, Oppert JM, De Bourdeaudhuij I, et al.: Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Medicine 13:84, 2015. doi:10.1186/s12916-015-0323-6.
Bartels SJ, Pratt SI, Aschbrenner KA, Barre LK, Jue K, Wolfe RS, et al.: Clinically significant improved fitness and weight loss among overweight persons with serious mental illness. Psychiatric services (Wash, DC) 64:729–736, 2013. doi:10.1176/appi.ps.003622012.
Burke LE, Wang J, Sevick MA: Self-monitoring in weight loss: A systematic review of the literature. Journal of the American Dietetic Association 111:92–102, 2011. doi:10.1016/j.jada.2010.10.008.
Mead GE, Morley W, Campbell P, Greig CA, McMurdo M, Lawlor DA. Exercise for depression. The Cochrane Database of Systematic Reviews 4:Cd004366, 2008. doi:10.1002/14651858.CD004366.pub3.
Anderson E, Shivakumar G: Effects of exercise and physical activity on anxiety. Frontiers in Psychiatry 4:27, 2013
Pinto Pereira SM, Geoffroy MC, Power C: Depressive symptoms and physical activity during 3 decades in adult life: bidirectional associations in a prospective cohort study. JAMA Psychiatry 71:1373–1380, 2014.
Naslund JA, Aschbrenner K, Bartels S: Wearable mHealth Activity Tracking for Health Promotion in People with Serious Mental Illness: Using Participant Feedback to Inform Future Interventions. Under Review.
Ben-Zeev D, Kaiser SM, Krzos I: Remote “hovering” with individuals with psychotic disorders and substance use: feasibility, engagement, and therapeutic alliance with a text-messaging mobile interventionist. Journal of Dual Diagnosis 10:197–203, 2014. doi:10.1080/15504263.2014.962336
Leon AC, Davis LL, Kraemer HC: The Role and Interpretation of Pilot Studies in Clinical Research. Journal of Psychiatric Research 45:626–629, 2011. doi:10.1016/j.jpsychires.2010.10.008
Acknowledgments
The authors wish to think Stacey Zawacki, DrPH, RDN, for expert consultation on the nutrition component of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflict of interest as it relates to the subject of this manuscript.
Funding
This study was supported by an AHRQ funded K12 Career Development Fellowship for Patient-Centered Outcomes Research awarded to the first author (K12 HS021695-01, PI: Bartels). Additional support was received from the United States Centers for Disease Control and Prevention Health Promotion and Disease Prevention Research Center (Cooperative Agreement Number U48DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Rights and permissions
About this article
Cite this article
Aschbrenner, K.A., Naslund, J.A., Shevenell, M. et al. Feasibility of Behavioral Weight Loss Treatment Enhanced with Peer Support and Mobile Health Technology for Individuals with Serious Mental Illness. Psychiatr Q 87, 401–415 (2016). https://doi.org/10.1007/s11126-015-9395-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-015-9395-x