Abstract
Chronic white matter structural injury is a risk factor for poor long-term outcomes after acute ischemic stroke (AIS). However, it is unclear how white matter structural injury predisposes to poor outcomes after AIS. To explore this question, in 42 AIS patients with moderate to severe white matter hyperintensity (WMH) burden, we characterized WMH and normal-appearing white matter (NAWM) diffusivity anisotropy metrics in the hemisphere contralateral to acute ischemia in relation to ischemic tissue and early functional outcomes. All patients underwent brain MRI with dynamic susceptibility contrast perfusion and diffusion tensor imaging within 12 h and at day 3–5 post stroke. Early neurological outcomes were measured as the change in NIH Stroke Scale score from admission to day 3–5 post stroke. Target mismatch profile, percent mismatch lost, infarct growth, and rates of good perfusion were measured to assess ischemic tissue outcomes. NAWM mean diffusivity was significantly lower in the group with early neurological improvement (ENI, 0.79 vs. 0.82 × 10−3, mm2/s; P = 0.02). In multivariable logistic regression, NAWM mean diffusivity was an independent radiographic predictor of ENI (β = − 17.6, P = 0.037). Median infarct growth was 118% (IQR 26.8–221.9%) despite good reperfusion being observed in 65.6% of the cohort. NAWM and WMH diffusivity metrics were not associated with target mismatch profile, percent mismatch lost, or infarct growth. Our results suggest that, in AIS patients, white matter structural integrity is associated with poor early neurological outcomes independent of ischemic tissue outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
White matter hyperintensity (WMH), or leukoaraiosis on T2 MRI, is thought to represent end-stage white matter disease and loss of structural integrity [1]. Importantly, patients with increased white matter structural injury have a greater risk of poor long-term functional outcomes after acute ischemic stroke (AIS) [2, 3]. Specifically, increasing WMH burden is predictive of poor long-term functional outcomes after AIS [2, 4]. At the microvascular level, decreased structural integrity and increased blood-brain barrier permeability (BBB-P) of normal-appearing white matter (NAWM) are also associated with poor long-term post-stroke outcomes [5, 6]. An unresolved question, however, is how white matter structural injury contributes to poor stroke outcomes.
There is some evidence to suggest that patients with increased WMH burden are at risk of infarct growth in the acute setting [7]. In select patient populations, WMH burden is also associated with early neurologic deterioration after AIS [8, 9]. These data suggest that patients with increasing WMH burden are at risk for infarct growth and poor early neurologic outcomes. An important consideration of these findings, however, is that visible WMH represents radiographic injury to only a small fraction of total brain white matter [10]. As a result, it is not known whether characterization of microstructural integrity of NAWM, representing the large majority of total white matter, will provide additional information on ischemic tissue and early clinical outcomes after AIS. Addressing this question could advance knowledge on the influence of NAWM structural integrity on the early trajectory after stroke, which has been shown to be a significant predictor of long-term outcomes [11], and provide insight into the mechanisms of white matter injury in post-stroke outcomes.
We hypothesize that decreased white matter structural integrity contributes to worse ischemic tissue and early clinical outcomes post stroke. In a population of AIS patients with moderate to severe WMH, at risk for infarct growth [7] and poor early neurologic outcomes, [8] we set out to characterize the clinical and radiographic variables associated with ischemic tissue and early clinical outcomes. Analysis of white matter structural integrity in the hemisphere contralateral to the acute infarct was performed to minimize any influence from acute cerebral ischemia and to investigate the effects of chronic white matter injury on early clinical outcomes. We used a prespecified definition of early neurological improvement (ENI) as part of a retrospective analysis of an ongoing prospective study of AIS patients with serial MRIs obtained in the acute (< 12 h from stroke onset) and subacute phases (3–5 days post stroke). Utilizing this radiographic approach, in the hemisphere contralateral to the acute infarct, we measured NAWM and WMH diffusivity anisotropy metrics in relation to ischemic tissue outcomes and ENI.
Methods
All aspects of this study have been approved by our Institutional Review Board. Informed consent was obtained from all individual participants included in the study or their surrogates.
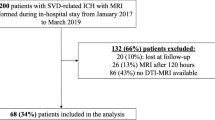
The current study was a retrospective analysis of an ongoing, prospective study, the Statins Augment smalL Vessel function and improve stroke Outcomes (SALVO, NIH 5R01NS082285) study of the effect of statin pretreatment in patients with AIS and moderate to severe WMH.
Participants, Inclusion/Exclusion Criteria
Between April 2014 and February 2017, all AIS subjects > 18 years presenting to our Emergency Department within 12 h from symptom onset were screened for eligibility and underwent a brain MRI. AIS was defined as (a) acute onset of focal neurological symptoms consistent with cerebrovascular syndrome, (b) MRI findings consistent with acute cerebral ischemia, and (c) no evidence of other neurological disorders to explain the symptoms. Subjects with moderate to severe WMH, as defined by Fazekas grade ≥ 2 in either category, [12] were eligible for enrollment in this study. Participants unable to obtain gadolinium-based contrast because of medical contraindications were excluded. Participants with premorbid functional status deemed by the investigator likely to interfere with study participation or follow-up were also excluded. All enrolled subjects had a repeat MRI at day 3–5 post stroke contemporaneous with clinical outcome assessment.
Clinical Variables
All participants were evaluated by a neurologist on admission and at day 3–5 post stroke, and the NIHSS score, as a measure of stroke severity, was determined. Age and past medical history (including atrial fibrillation, prior myocardial infarction, diabetes mellitus, hypertension, hyperlipidemia, and prior ischemic stroke) were obtained on admission from the patient or their surrogate, or abstracted from the medical record. Tobacco use was defined as patient reported current or any prior cigarette smoking. Admission systolic and diastolic blood pressures were abstracted from the first documented vital signs in the medical record. Treatment with intravenous thrombolysis was also recorded. Large-vessel occlusion of the anterior circulation was defined as occlusion of the internal carotid artery or proximal middle cerebral artery, M1 segment. AIS subtypes were categorized by a trained neurologist (M.R.E, N.S.R.) according to the criteria established by the Trial of Org 10172 in Acute Stroke Treatment [13]. ENI was defined as a reduction in the NIHSS of ≥ 2 points from the admission to day 3–5 assessment post stroke or a NIHSS score of 0 on follow-up assessment (ENI+).
Imaging Analysis
MRI Data Acquisition
Each participant underwent two separate brain MRIs with perfusion-weighted imaging (PWI): one (acute) within 12 h from stroke onset and the second (follow-up) at day 3–5 post stroke. Except for one participant, all acute MRIs were performed on a 1.5-T General Electric scanner. The follow-up MRI was performed using a 3-T Siemens Skyra scanner in all but five participants that could not undergo a dedicated 3-T MRI due to medical contraindications.
For the acute MRI, axial T2-weighted Fluid Attenuated Inversion Recovery (FLAIR) sequences were acquired, in most subjects, on a 1.5-T General Electric MRI system with TR/TE/TI = 9002/133/2200 ms, 220-mm field-of-view (FOV), 5-mm slice thickness with 1-mm gap, and in-plane resolution of 0.86 × 0.86 mm2. Diffusion-weighted (DWI)/diffusion tensor imaging (DTI) was obtained on the acute MRI with echo-planar imaging using the following acquisition parameters for most cases: TR/TE = 5000/92 ms, 240-mm FOV, 5-mm slice thickness with 1-mm gap, in-plane resolution of 0.94 × 0.94 mm2 (128 × 128 acquisition matrix up-sampled to 256 × 256), three 0 s/mm2 (b-zero) and 25 directions (1000 s/mm2 b-value). Eddy current distortion and motion correction was performed on DTI datasets as described previously [14]. Dynamic susceptibility contrast (DSC) PWI was acquired using gradient echo echo-planar imaging readout with the following parameters: TR/TE = 1500/40 ms, 220–240 ms FOV, 5 mm slice thickness with 1 mm gap, and 1.72 × 1.72 mm2 in-plane resolution and 80 time points. The time-to-maximum (Tmax, s) maps were calculated as described previously [6, 15, 16].
Follow-up FLAIR sequences were acquired with TR/TE/TI = 9000/119/2500 ms, 220-mm FOV, 5-mm slice thickness with 1-mm gap, and in-plane resolution of 0.86 × 0.86 mm2. The follow-up DSC PWI imaging protocol consisted of 80 acquisitions at a TR/TE = 1500/35 ms, 220 ms FOV, 5 mm slice thickness with 1 mm gap and 1.72 × 1.72 mm2 for most cases.
Volumetric Analysis
WMH and chronic strokes were outlined on the acute FLAIR sequence using a validated, semiautomated method utilizing MRIcro software (www.mricro.com) as described previously [5, 17]. Briefly, supratentorial WMH maps were derived in the ipsi- and contralesional hemispheres using automated signal intensity thresholding with subsequent manual editing to finalize the WMH maps. The acute DWI sequence was used for comparison to exclude any confounding due to acute cerebral ischemia. Total WMH volume (WMHv) was normalized to intracranial area [18]. Volumes of the acute infarct on DWI (DWIv), acute Tmax with a threshold > 6 s on DSC perfusion, and final infarct volume (FIV), defined as infarct volume on the follow-up FLAIR sequence, were determined. The PWI-DWI mismatch ratio was defined as acute Tmax/DWIv. Percent infarct growth was calculated as (FIV − DWIv)/FIV × 100. Good reperfusion was defined based on the criteria of a greater than 50% reduction in Tmax lesion volume between the baseline and day 3–5 follow-up MRI [19]. Percent mismatch lost was calculated as (FIV − DWIv)/(acute Tmax − DWIv) × 100 [7]. Target mismatch profile was defined as PWI-DWI mismatch ratio > 1.8 and mismatch volume ≥ 15 cm3 [19].
DTI Analysis
The DWI and FLAIR data were coregistered to one another in a semiautomated manner [20] to the ICBM-152 T1 Atlas [21]. Probabilistic NAWM masks were determined as described previously [6]. In brief, NAWM in the hemisphere contralateral to the acute infarct was segmented using the ICBM probabilistic atlas [22] with 95% WM probability and subtracting the WMH and chronic stroke masks. NAWM masks were further restricted by dilating the WMH masks three times (mincmorph, [23]) prior to subtraction and setting an ADC value threshold of less than 1500 × 10−6 mm2/s. Mean diffusivity (MD), radial diffusivity (RD), axial diffusivity (AD), and fractional anisotropy (FA) were subsequently measured in WMH and NAWM contralateral to the acute infarct. One participant was excluded from analysis because the 95% probability NAWM volume was less than 0.1 cm3.
Statistical Analysis
For statistical comparison of the ENI+ versus ENI− groups, Wilcoxon rank sum and Fisher’s exact test were used, as appropriate (RStudio version 1.0.153). Effect size was determined for statistically significant (P < 0.05) and selected additional variables. Univariable logistic regression was performed to assess the association of ENI with clinical and radiographic variables. Stepwise, backward elimination logistic regression analysis was performed using minimization of Akaike information criterion to determine predictors of ENI. To avoid the influence of collinearity between the diffusivity anisotropy metrics on the regression analysis [24], three models were run including (1) AD and RD, (2) MD, and (3) FA. Statistical significance was set at P < 0.05.
Results
Clinical and Radiographic Variables Associated with Early Neurological Outcomes
Forty-two participants were enrolled in our study. The acute and follow-up MRIs were obtained at a mean time ± standard deviation of 6.15 ± 2.78 h and 65.03 ± 26.5 h from last known well time, respectively. 52.3% of participants met criteria for ENI and eight (19.1%) had a worsening of NIHSS by 2 or more points from admission to day 3–5. We observed no difference in age, sex, pre-stroke disability, history of ischemic stroke, stroke secondary to large-vessel occlusion, or administration of intravenous tPA between the groups with and without ENI (Table 1). The ENI+ group, however, had decreased rates of diabetes, hyperlipidemia, hypertension, and strokes attributed to a small-vessel occlusive etiology (Table 1). Admission NIHSS scores were higher in the ENI+ group than the ENI− group; however, the ENI− group had higher follow-up NIHSS scores (Table 1).
No difference in total WMHv was observed between groups; however, the ENI+ group had a lower burden of periventricular WMH compared with the ENI− group (Table 2). There was no difference in the amount of deep WMH between groups. The PWI-DWI mismatch ratio, percent infarct growth, percent mismatch lost, and FIV were also not different between groups (Table 2). A large, but nonsignificant, difference in the rate of good reperfusion was observed between groups (ENI+, 77.8%; ENI−, 46.7%; P = 0.08).
NAWM RD and MD values were lower in the ENI+ group, as compared with the ENI− group (Table 3). Furthermore, effect size calculations suggested a medium practical significance for RD (r = 0.29) and MD (r = 0.31). No difference in WMH diffusivity anisotropy metrics was observed between ENI groups (Table 3).
In univariate regression analysis for predictors of ENI, hypertension, hyperlipidemia, diabetes, and increased admission NIHSS score were all predictors of ENI (Table 4). Increasing periventricular, but not deep, WMH burden was also negatively associated with ENI in univariable analysis. In addition, analysis of NAWM and WMH diffusivity anisotropy metrics showed that increasing NAWM RD (β = − 17.64, P = 0.037) and MD (β = − 16.17, P = 0.037) decreased the likelihood of ENI (Table 4). In multivariable, backward elimination stepwise logistic regression, diabetes and admission NIHSS score were associated with decreased and increased likelihood of ENI, respectively.
In backward elimination, stepwise logistic regression analyses for radiographic markers of ENI, NAWM MD (β = − 17.64, P = 0.037) was an independent predictor of ENI (Table 5).
Clinical Variables Associated with Ischemic Tissue Outcomes
Fifteen patients (34.0%) had a target mismatch profile present. Admission systolic blood pressure (β = − 0.035, P = 0.023) was negatively associated with presence of target mismatch profile on univariable logistic regression. On multivariable logistic regression analysis adjusting for WMHv, admission systolic blood pressure was an independent predictor for presence of a target mismatch profile (β = − 0.16, P = 0.04).
The median percent infarct growth in our cohort was 118% (IQR 26.8–221.9) excluding patients with strokes attributed to small-vessel occlusive disease. WMHv, age, sex, and WMH and NAWM diffusivity anisotropy metrics were not predictive of percent infarct growth (data not shown). In our population, 65.6% achieved good reperfusion on follow-up imaging. There was no association between WMHv or NAWM diffusivity anisotropy metrics and reperfusion status.
Discussion
In this study, we report that in individuals with moderate to severe WMH, preserved NAWM microstructural integrity is associated with ENI. We also demonstrate that clinical variables suspected as inciting factors for intrinsic small-vessel disease, namely diabetes, hypertension, and hyperlipidemia, [1] diminish the odds of ENI. Lastly, we show that in patients with moderate to severe WMH, target mismatch profile and infarct growth are common in the early stage of AIS. As the early trajectory of the NIHSS has been shown to predict long-term outcomes, [11] our observations that infarct growth and the lack of ENI are common in patients with severe WMH burden emphasize the vulnerabilities of this population for poor outcomes and advance our understanding of how white matter structural integrity contributes to poor long-term post-stroke outcomes.
In comparison with the ENI+ group, we observed that NAWM diffusivity, specifically RD and MD, was significantly increased in the ENI− group. Decreased NAWM structural integrity, reflected by higher NAWM RD and MD values, was also associated with decreased odds of ENI. These observations were further supported in the multivariable logistic regression analysis for radiographic predictors of ENI which demonstrated that NAWM MD was an independent predictor of ENI in models including DWIv, PWI-DWI mismatch ratio, and periventricular WMH burden. The multivariable model suggests that decreased NAWM structural integrity, reflected as increased MD, is an independent radiographic predictor of ENI. This observation suggests a role of white matter microstructural integrity in early clinical recovery after AIS. Furthermore, by restricting our DTI analysis to the contralesional hemisphere, we minimized any contribution of acute cerebral ischemia and were able to investigate the effects of chronic white matter injury on ENI.
The observation that diffusivity anisotropy values in WMH did not correlate with ENI is likely due to WMH, as a reflection of end-stage white matter disease, imparting a relative ceiling/floor effect on the respective diffusivity anisotropy analyses within these regions [25]. Accordingly, we observed no significant difference in the WMH diffusivity anisotropy values between ENI groups. Based on this reasoning, the DTI analysis of contralesional NAWM represents a broader spectrum of chronic white matter pathology, which we have previously shown influences long-term stroke outcomes [5].
We also show that patients with moderate to severe WMH burden are at high risk for poor early clinical outcomes. In part, this is likely due to the association between increased WMH burden and infarct growth [7]. In our population, the median percent infarct growth was 118%. We also observed that 34% of our population had a target mismatch profile present despite only 14.3% with a confirmed large-vessel occlusion. An explanation for this discrepancy could be that patients with severe WMH have hemodynamic impairment of the distal arteries/terminal arterioles and that this produces a tendency for poor ischemic tissue outcomes. This hypothesis is supported by prior work showing region-specific differences in cerebral blood flow in patients with WMH [26] and reduced cerebrovascular reactivity contributing to WMH progression [27].
Collectively, our findings confirm that individuals with advanced WMH burden are at high risk of poor ischemic tissue and early functional outcomes and that decreased NAWM microstructural integrity is associated with poor early post-stroke recovery. This is of clinical importance because the early trajectory of neurological improvement, as defined by the 2-day longitudinal NIHSS, has been shown to be a predictor of 90-day outcomes [11]. These observations highlight the influence of white matter structural integrity on stroke outcomes and agree with prior reports demonstrating a negative relationship between WMH burden and both early [8, 9] and long-term functional outcomes after AIS [2, 4, 28].
The design and patient population of this study offer several strengths including (1) a study of thoroughly ascertained, AIS patients including standardized measures of functional outcomes; (2) sequential MRIs obtained in the acute and subacute setting with PWI and DTI; (3) a standardized approach to MRI processing and analysis; and (4) utilizing acute clinical imaging sequences to identify early markers of ENI.
There are several limitations of this study that are important to consider in the overall interpretation and generalizability of our findings. First, while our sample size was large enough to detect significant differences in diffusivity anisotropy metrics relative to ENI with medium effect size (r = 0.3), the small study size could contribute to the lack of statistical power to detect smaller influences from other clinical or radiographic variables. Secondly, this was a study of patients with severe WMH and relatively small strokes (median DWIv 4.1 cm3), which could limit the overall generalizability. How our results translate to patients with different clinical demographics such as ethnicity or prevalence of vascular risk factors, large infarcts, or different stroke subtypes is unclear. We maintain, however, that this focused study of AIS patients at risk for poor outcomes demonstrates the added utility of characterizing NAWM structural integrity to inform on the clinical trajectory. The difference in initial stroke severity between groups, with the ENI− group having a lower admission NIHSS, could also suggest a floor effect to the lack of improvement in this group. This seems unlikely given that this group actually deteriorated from admission to day 3–5 as evidenced by the median NIHSS (ENI− NIHSS, admission 3.5 versus day 3–5, 6.0). Specifically, 60% (12 patients) of patients in the ENI− group had a worse NIHSS score on follow-up and an additional 20% (4 patients) had no change in NIHSS score. This observation suggests that the ENI− group, despite the low admission NIHSS, was in fact at risk for poor early neurologic outcomes. In addition, we have selected an NIHSS score cut-off for detection of ENI at a conservative, previously referenced margin (≥ 2) [8, 9] to capture small variation in the neurological status. Therefore, our results suggest that the clinical and radiographic characteristics of the ENI− cohort are indicative of a vulnerable stroke population. An additional limitation of our approach was the utilization of the acute MRI scans for characterization of NAWM diffusivity anisotropy metrics. As these were clinical scans, nonisotropic voxels were used for diffusivity anisotropy analysis and thus could have introduced some bias due to partial volume averaging [29]. We would maintain, however, that utilizing clinical scans to identify predictors of ENI functions is a clinically pragmatic approach for translation to patient care.
In summary, we report the association of NAWM diffusivity anisotropy metrics with ENI after acute cerebral ischemia. Our findings strengthen the line of evidence for a relationship between white matter structural integrity and post-stroke outcomes with new evidence for a role in the early trajectory of recovery after AIS. Furthermore, these findings suggest that characterizing white matter structural integrity in the acute stages of ischemic stroke is feasible and can potentially identify susceptible populations at risk for early clinical improvement or deterioration. Overall, these findings merit a prospective, large-scale investigation of the impact of NAWM diffusivity anisotropy metrics on early neurologic outcomes after AIS.
References
Wardlaw JM, Smith C, Dichgans M. Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol. 2013;12(5):483–97. https://doi.org/10.1016/S1474-4422(13)70060-7.
Onteddu SR, Goddeau RP Jr, Minaeian A, Henninger N. Clinical impact of leukoaraiosis burden and chronological age on neurological deficit recovery and 90-day outcome after minor ischemic stroke. J Neurol Sci. 2015;359(1–2):418–23. https://doi.org/10.1016/j.jns.2015.10.005.
Giurgiutiu DV, Yoo AJ, Fitzpatrick K, Chaudhry Z, Leslie-Mazwi T, Schwamm LH, et al. Severity of leukoaraiosis, leptomeningeal collaterals, and clinical outcomes after intra-arterial therapy in patients with acute ischemic stroke. J Neurointerv Surg. 2015;7(5):326–30. https://doi.org/10.1136/neurintsurg-2013-011083.
Arsava EM, Rahman R, Rosand J, Lu J, Smith EE, Rost NS, et al. Severity of leukoaraiosis correlates with clinical outcome after ischemic stroke. Neurology. 2009;72(16):1403–10. https://doi.org/10.1212/WNL.0b013e3181a18823.
Etherton MR, Wu O, Cougo P, Giese AK, Cloonan L, Fitzpatrick KM, et al. Integrity of normal-appearing white matter and functional outcomes after acute ischemic stroke. Neurology. 2017;88(18):1701–8. https://doi.org/10.1212/WNL.0000000000003890.
Rost NS, Cougo P, Lorenzano S, Li H, Cloonan L, Bouts MJ, et al. Diffuse microvascular dysfunction and loss of white matter integrity predict poor outcomes in patients with acute ischemic stroke. J Cereb Blood Flow Metab. 2017. https://doi.org/10.1177/0271678X17706449.
Ay H, Arsava EM, Rosand J, Furie KL, Singhal AB, Schaefer PW, et al. Severity of leukoaraiosis and susceptibility to infarct growth in acute stroke. Stroke. 2008;39(5):1409–13. https://doi.org/10.1161/STROKEAHA.107.501932.
Nam KW, Lim JS, Kang DW, Lee YS, Han MK, Kwon HM. Severe white matter hyperintensity is associated with early neurological deterioration in patients with isolated pontine infarction. Eur Neurol. 2016;76(3–4):117–22. https://doi.org/10.1159/000448888.
Feng C, Tan Y, Wu YF, Xu Y, Hua T, Huang J, et al. Leukoaraiosis correlates with the neurologic deterioration after small subcortical infarction. J Stroke Cerebrovasc Dis. 2014;23(6):1513–8. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.12.032.
Espeland MA, Erickson K, Neiberg RH, Jakicic JM, Wadden TA, Wing RR, et al. Brain and white matter hyperintensity volumes after 10 years of random assignment to lifestyle intervention. Diabetes Care. 2016;39(5):764–71. https://doi.org/10.2337/dc15-2230.
Sajobi TT, Menon BK, Wang M, Lawal O, Shuaib A, Williams D, et al. Early trajectory of stroke severity predicts long-term functional outcomes in ischemic stroke subjects: results from the ESCAPE trial (endovascular treatment for small core and anterior circulation proximal occlusion with emphasis on minimizing CT to recanalization times). Stroke. 2017;48(1):105–10. https://doi.org/10.1161/STROKEAHA.116.014456.
Fazekas F, Barkhof F, Wahlund LO, Pantoni L, Erkinjuntti T, Scheltens P, et al. CT and MRI rating of white matter lesions. Cerebrovasc Dis. 2002;13(Suppl 2):31–6.
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24(1):35–41.
Sorensen AG, Wu O, Copen WA, Davis TL, Gonzalez RG, Koroshetz WJ, et al. Human acute cerebral ischemia: detection of changes in water diffusion anisotropy by using MR imaging. Radiology. 1999;212(3):785–92. https://doi.org/10.1148/radiology.212.3.r99se24785.
Wu O, Ostergaard L, Weisskoff RM, Benner T, Rosen BR, Sorensen AG. Tracer arrival timing-insensitive technique for estimating flow in MR perfusion-weighted imaging using singular value decomposition with a block-circulant deconvolution matrix. Magn Reson Med. 2003;50(1):164–74. https://doi.org/10.1002/mrm.10522.
Boxerman JL, Schmainda KM, Weisskoff RM. Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol. 2006;27(4):859–67.
Rost NS, Sadaghiani S, Biffi A, Fitzpatrick KM, Cloonan L, Rosand J, et al. Setting a gold standard for quantification of leukoaraiosis burden in patients with ischemic stroke: the Atherosclerosis Risk in Communities Study. J Neurosci Methods. 2014;221:196–201. https://doi.org/10.1016/j.jneumeth.2013.10.009.
Ferguson KJ, Wardlaw JM, Edmond CL, Deary IJ, Maclullich AM. Intracranial area: a validated method for estimating intracranial volume. J Neuroimaging. 2005;15(1):76–8. https://doi.org/10.1177/1051228404270243.
Lansberg MG, Straka M, Kemp S, Mlynash M, Wechsler LR, Jovin TG, et al. MRI profile and response to endovascular reperfusion after stroke (DEFUSE 2): a prospective cohort study. Lancet Neurol. 2012;11(10):860–7. https://doi.org/10.1016/S1474-4422(12)70203-X.
Collins DL, Neelin P, Peters TM, Evans AC. Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J Comput Assist Tomogr. 1994;18(2):192–205.
Mori S, Oishi K, Jiang H, Jiang L, Li X, Akhter K, et al. Stereotaxic white matter atlas based on diffusion tensor imaging in an ICBM template. NeuroImage. 2008;40(2):570–82. https://doi.org/10.1016/j.neuroimage.2007.12.035.
Mazziotta J, Toga A, Evans A, Fox P, Lancaster J, Zilles K, et al. A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM). Philos Trans R Soc Lond Ser B Biol Sci. 2001;356(1412):1293–322. https://doi.org/10.1098/rstb.2001.0915.
McConnell Brain Imaging Centre. BIC - The McConnell Brain Imaging Centre: home page. 2015. 2006.
Basser PJ, Jones DK. Diffusion-tensor MRI: theory, experimental design and data analysis - a technical review. NMR Biomed. 2002;15(7–8):456–67. https://doi.org/10.1002/nbm.783.
Wardlaw JM, Valdes Hernandez MC, Munoz-Maniega S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment. J Am Heart Assoc. 2015;4(6):001140. https://doi.org/10.1161/JAHA.114.001140.
O'Sullivan M, Lythgoe DJ, Pereira AC, Summers PE, Jarosz JM, Williams SC, et al. Patterns of cerebral blood flow reduction in patients with ischemic leukoaraiosis. Neurology. 2002;59(3):321–6.
Sam K, Crawley AP, Conklin J, Poublanc J, Sobczyk O, Mandell DM, et al. Development of white matter hyperintensity is preceded by reduced cerebrovascular reactivity. Ann Neurol. 2016;80(2):277–85. https://doi.org/10.1002/ana.24712.
Henninger N, Lin E, Baker SP, Wakhloo AK, Takhtani D, Moonis M. Leukoaraiosis predicts poor 90-day outcome after acute large cerebral artery occlusion. Cerebrovasc Dis. 2012;33(6):525–31. https://doi.org/10.1159/000337335.
Vos SB, Jones DK, Viergever MA, Leemans A. Partial volume effect as a hidden covariate in DTI analyses. NeuroImage. 2011;55(4):1566–76. https://doi.org/10.1016/j.neuroimage.2011.01.048.
Acknowledgements
This study is supported by the Statins Augment smalL Vessel function and improve stroke Outcomes (SALVO) study (NIH-NINDS 5R01NS082285).
Funding
The study was funded in part by the NIH-National Institute of Neurological Disorders and Stroke R01NS082285-01A1 (N.S.R.); National Institute of Biomedical Imaging and Bioengineering (P41EB015896); and American Heart Association 17CPOST33680102.
Author information
Authors and Affiliations
Contributions
Mark Etherton: study concept and design, acquisition of data, analysis and interpretation of data, drafting, and critical revision of the manuscript.
Ona Wu: study concept and design, analysis and interpretation of data, critical revision of the manuscript for intellectual content.
Anne-Katrin Giese: analysis and interpretation of data, critical revision of the manuscript for intellectual content.
Arne Lauer; acquisition of data, critical revision of the manuscript for intellectual content.
Gregoire Boulouis: acquisition of data, critical revision of the manuscript for intellectual content.
Brittany Mills: acquisition of data.
Lisa Cloonan: acquisition of data.
Kathleen L. Donahue: acquisition of data.
William Copen: study concept and design, critical revision of the manuscript for intellectual content.
Pamela Schaefer: study concept and design, critical revision of the manuscript for intellectual content.
Natalia S. Rost: study concept and design, analysis and interpretation of data, critical revision of the manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflict of Interest
Mark R. Etherton is in part supported by the American Heart Association (17CPOST33680102). Ona Wu is in part supported by NIH Health (P50NS051343, R01NS082285, R01NS086905) and NIBIB (P41EB015896). Anne-Katrin Giese reports no disclosures. Arne Lauer reports no disclosures. Gregoire Boulouis reports no disclosures. Brittany Mills reports no disclosures. Lisa Cloonan reports no disclosures. Kathleen L. Donahue reports no disclosures. William Copen reports no disclosures. Pamela Schaefer reports no disclosures. Natalia S. Rost is in part supported by the NIH-NINDS R01NS082285 and R01NS086905.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Etherton, M.R., Wu, O., Giese, AK. et al. White Matter Integrity and Early Outcomes After Acute Ischemic Stroke. Transl. Stroke Res. 10, 630–638 (2019). https://doi.org/10.1007/s12975-019-0689-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-019-0689-4