Abstract
Objectives
Prior research has found that self-compassion is associated with a range of health and well-being outcomes, but the specific association between self-compassion and sleep quality remains poorly understood. The purpose of this study is to respond to this issue through conducting a meta-analysis to quantify the relationship between self-compassion and sleep quality.
Methods
Systematic literature searches were conducted using the PsychInfo, Embase and Medline electronic databases to identify studies reporting on the relationship between self-compassion and sleep quality. Random effects meta-analysis was used to synthesise results.
Results
Seventeen independent studies from 15 publications met criteria for inclusion in this review. All studies included self-reported sleep quality measures. No study reported objective measurements of sleep quality. Meta-analysis revealed evidence of a significant association whereby those with higher self-compassion reported fewer sleep problems r = − 0.32, 95%CI [− .36, − .28]. In a subgroup (n = 6) of studies that delineated the positively and negatively worded items of the self-compassion scale (termed positive self-compassion and self-coldness, respectively), self-coldness was more strongly associated with poor sleep quality r = 0.36, 95%CI [.18, .52] than positive self-compassion r = − 0.15, 95%CI [− .24, − .05].
Conclusions
Our meta-analysis found that self-compassion is associated with self-reported sleep quality. Future research is needed to investigate directions of causality and to consider if self-compassion-based interventions might be effective in improving sleep quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Up to 50% of people experience persistent sleep disturbances, including difficulties initiating and maintaining sleep (LeBlanc et al. 2007; Walsh and Üstün 1999). Sleep disturbances are associated with a range of poor health outcomes, including increased systemic inflammation (Irwin et al. 2016), cognitive impairment (Banks and Dinges 2007), obesity (Cappuccio et al. 2008) and increased risk of death (Parthasarathy et al. 2015). Poor sleep quality also compromises psychological health, impacting daytime functioning (Morin and Benca 2012) and increasing the risk of developing mental disorders including depression, anxiety and substance use disorders (Hertenstein et al. 2019). While there is evidence that pharmacological treatments can be efficacious in treating sleep problems, they come with significant side effects, including risk of addiction and daytime drowsiness (Qaseem et al. 2016). Thus, there is a need to better understand modifiable psychological factors associated with a good night’s sleep, indexed by sleep quality.
Subjective appraisals of sleep quality (such as sleep diaries and self-report questionnaires) do not correlate strongly with objective measures (such as actigraphy and polysomnography), with the former more strongly linked to psychological well-being and quality of life (Baker et al. 2018; Bei et al. 2015). Although numerous validated measures of subjective sleep quality exist, one frequently used scale is the Pittsburgh Sleep Quality Index (PSQI; Buysse et al. 1989).
Self-compassion is a promising psychological resource associated with a range of health behaviours, and emerging work shows that it is also relevant to sleep quality (Hu et al. 2018; Sirois et al. 2015). Self-compassion can be defined as a healthy way of relating towards the self that is based on self-kindness, mindful awareness and awareness of common humanity as opposed to self-criticism, over-identification with experiences and a sense of isolation (Neff 2003a). Self-compassion becomes salient during difficulties and shapes how an individual relates towards their suffering (Neff 2003a). Self-compassion is positively associated with a number of healthy behaviours including physical activity, healthy diet and medical adherence (Sirois and Hirsch 2019; Sirois et al. 2015; Terry and Leary 2011). Emotion regulation, defined as the process by which an individual shapes the emotions they experience, as well as when and how they express these emotions (Gross 1998), is thought to be a key mechanism by which self-compassion facilitates healthy behaviours, as self-compassion both ameliorates negative and enhances positive emotional states (Sirois et al. 2015; Terry and Leary 2011).
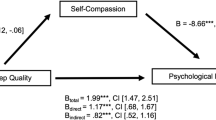
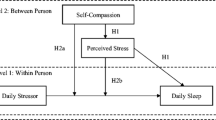
In the context of sleep, self-compassion might shape how an individual relates to a sleep disturbance, daily life stressors or ruminative thoughts. For example, while self-compassion might support night-time relaxation, self-critical thoughts could fuel restlessness and agitation and thus perpetuate an even poorer night’s sleep (Butz and Stahlberg 2018; Hu et al. 2018). In support of this hypothesis, a number of recent studies have investigated the association between self-compassion and sleep quality and found a significant association (Butz and Stahlberg 2018; Hu et al. 2018; Kemper et al. 2015). For instance, Kemper and colleagues surveyed 213 trainee and professional health clinicians and found that self-compassion was associated with lower ratings of sleep disturbance, as measured by the Patient Reported Outcomes Measurement Information System (PROMIS), though the relationship was weaker than the association between sleep quality and psychological symptoms of distress (Kemper et al. 2015). Emerging work shows that self-compassion may play a protective role in ameliorating the negative effect of stressors on sleep quality (Butz and Stahlberg 2018; Hu et al. 2018). Thus, self-compassion may have a direct relationship with sleep quality, and concurrently dampen the impact that other important factors such as perceived stress, rumination and anxiety have on sleep quality.
Importantly, emerging research also indicates that brief self-compassion-based activities might lead to improvements in sleep quality. For example, in an experiment conducted by Butz and Stahlberg (2018), 143 college students were asked to think about personal problems for 3 min and were then randomised to complete either (i) a 20-min brief self-compassion meditation, (ii) a self-compassionate writing task or (iii) no instruction control (Butz and Stahlberg 2018). Participants then reported on their sleep quality the following day via the Sleep Problems Questionnaire (Jenkins et al. 1988). The authors found that those randomised to either of the self-compassion conditions reported significantly better sleep quality than the control condition, indicating that a brief self-compassion induction can contribute to improved sleep quality. This finding is important, because it shows that self-compassion is amenable to change and that improved self-compassion may facilitate better subjective sleep quality.
It is also possible that a bidirectional relationship exists between self-compassion and sleep quality. Sleep has been shown to have a complex and bidirectional relationship with other psychological factors such as depression (Baker et al. 2018). For instance, a recent observational study found that maladaptive emotion regulation (represented by worry and rumination scores) partially accounted for the relationship between sleep quality and subsequent depressive symptoms (O'Leary et al. 2017). Thus, it is conceivable that poor sleep quality may also reduce levels of self-compassion over time.
A distinction has been made between the positively and negatively worded items of the self-compassion scale (Brenner et al. 2017). Factor analyses have revealed that these items represent discrete latent factors, termed self-compassion and self-coldness, respectively (Brenner et al. 2017; Brown et al. 2016; Körner et al. 2015). Self-coldness entails being aggressive or harsh towards oneself in moments of failure or suffering (Brenner et al. 2017) (e.g. measured with the item: “I’m disapproving and judgmental about my own flaws and inadequacies”). Self-coldness appears to have more robust associations with psychological symptom measures such as depression and anxiety (Brenner et al. 2017; Körner et al. 2015), whereas positive self-compassion may be more strongly related to indices of positive well-being such as ego integrity (Phillips and Ferguson 2013). Since the majority of self-reported sleep measures, such as the Pittsburgh Sleep Quality Index (PSQI), measure symptoms of sleep disturbance, it is plausible that self-coldness may be a stronger predictor than self-compassion.
Despite emerging research associating self-compassion with less sleep disturbance, no meta-analysis has synthesised results to estimate the overall strength and direction of the relationship between self-compassion and sleep quality. The extent to which self-compassion and self-coldness distinctly relate to sleep disturbances likewise remains unclear. Hence, we aimed to review and quantitatively synthesise the research that reports on the association between self-compassion and sleep quality.
Method
Search Strategy and Selection Criteria
This review was guided by the PRISMA guidelines and pre-registered on the PROSPERO database (registration # CRD42019142128). Comprehensive searches were conducted using three electronic databases: PsycInfo, EMBASE and Medline. As self-compassion and sleep quality are a relatively new field of research, we aimed to be broad in our search strategy to identify all published studies in the area. Thus, the search term “self-compassion” was paired with the word “sleep”, and no limits were placed on search results at the database search phase. Both peer-review published and grey literature (dissertations and conference abstracts) were eligible, to reduce the risk of publication bias in results. After removing duplicates, all results were then screened manually by two independent reviewers (LB and EH) to identify studies published in English that report data on both self-compassion and sleep quality.
Studies were considered for inclusion if they reported quantitative data on both sleep (either self-report or objective physiological data) and self-compassion (self-report) measured with psychometrically validated scales. Studies were eligible for inclusion if their sample had a mean age 18 or over, and studies of children or adolescent samples with a mean age under 18 were excluded. Because this review focused on the relationship between sleep quality and self-compassion, an inclusion criterion was that the association was reported either as a correlation coefficient (e.g. Pearson’s r) or in-text description. To be eligible for inclusion in the meta-analysis, a reported correlation coefficient and the corresponding sample size was required. Authors were contacted to obtain this information if it was not reported. Both cross-sectional and interventional studies were eligible for inclusion. For the intervention studies, we obtained the overall baseline correlation between self-compassion and sleep quality pooled across conditions (e.g. pooled across intervention and control groups).
Data Extraction
Data on the year, place of publication, sample size, study design (cross-sectional or intervention), participant characteristics (study setting, proportion female and mean age) and outcome measures were extracted for all studies by two independent judges (LB and EH) with excellent reliability (κ = .98). Disagreements were resolved by consensus.
Study Quality Assessment
A modified version of the Agency for Healthcare Research and Quality (AHRQ) methodology checklist was used to assess study quality, in accordance with current recommendations (Zeng et al. 2015). The full AHRQ includes a checklist of 11 items, where each is rated as being present (1/1), absent (0/1) or unclear (.5/1). In our study, three items were removed because they were deemed not relevant to cross-sectional analyses (e.g. “clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained”). Quality was rated independently by two authors (LB and CB) with good inter-rater reliability (κ = .93) and disagreements were resolved by consensus. Recent work has recommended reporting study quality as a domain matrix rather than aggregating a numerical value of study quality for each included study (O’Connor et al. 2015). While this approach prohibits an analysis modelling between-study variance in outcome based on a numerical value of study quality, the matrix approach is recommended as it offers a more precise representation of the quality of included studies (Losilla et al. 2018).
Statistical Analyses
To synthesise the quantitative data, we performed a random effects meta-analysis using the Metafor package in R (Viechtbauer 2010). The correlation coefficient Pearson’s r was chosen as the effect size measure of the relationship between self-compassion and sleep due to its interpretability and good statistical properties (Rosenthal and DiMatteo 2001).
Most self-reported sleep quality scales (e.g. PSQI) are organised such that a higher score indicates poorer sleep quality. Poor sleep quality incorporates a range of sleep problems, including difficulties getting to sleep (sleep onset latency), night-time awakenings and early rising (Buysse et al. 1989). Only one included study (study 2 of Butz and Stahlberg 2018) used a sleep measure scored in the reverse direction. For uniformity, this was reverse-scored so that in all cases, a higher sleep score indicates a greater level of sleep disturbance.
Pearson’s r is not normally distributed, and so, all r values were transformed to Fisher’s z to compute an aggregate effect size estimate across studies and were then reconverted back to r for interpretation of the final result (Rosenthal and DiMatteo 2001). To investigate inter-study differences in results, heterogeneity was measured using the Q and I2 statistics. A non-significant Q statistic supports the null hypothesis that the pooled effect size represents a unitary effect. The I2 statistic describes the percentage of variation between studies due to heterogeneity rather than chance and values of 25%, 50% and 75% representing low, medium and high levels of heterogeneity, respectively (Higgins et al. 2003). Heterogeneity was modelled using a priori determined potential moderators including self-compassion measure (SCS vrs SCS-SF), sleep quality measure and participant mean age. Publication bias was assessed via inspection of the funnel plot, Egger regression and the Kendall rank correlation test.
Results
Study Characteristics
After removing duplicates, our search yielded a total of 69 results and ultimately 17 of these met criteria for inclusion in this meta-analysis (see PRISMA flow diagram in Fig. 1), with a combined sample size of 1830 participants. Data were derived from 14 peer-reviewed journal articles and one dissertation (Bricklin-Small 2017). Three of the included studies were independent samples reported within one larger journal article (Butz and Stahlberg 2018). Eight studies used a cross-sectional design (Bricklin-Small 2017; Butz and Stahlberg 2018; Hu et al. 2018; Jeste et al. 2019; Kemper et al. 2015; Kim and Ko 2018; Sirois et al. 2019; Vaillancourt and Wasylkiw 2019) and the remaining nine were intervention studies where baseline correlations between self-compassion and sleep quality were analysed (Butz and Stahlberg 2018; Christopher et al. 2018; Dvorakova et al. 2017; Frank et al. 2015; Hwang et al. 2019; Trent et al. 2018, Trent et al. 2019a, b). All studies included only self-reported sleep quality measures, including the Pittsburgh Sleep Quality Index (seven studies), the Insomnia Severity Index (three studies), the Patient Reported Outcomes Measurement Information System (three studies), the Lifestyle Questionnaire (three studies) and the Sleep Problem Scale (one study). Interestingly, 12 of the 15 publications (80%) were published in the past 2 years, demonstrating the rapid and recent expansion of the field. The mean of included study mean ages was 38.70, and the mean percentage of females across included studies was high (66.5%). A summary of included study characteristics can be found in Table 1.
Quantitative Synthesis of Results
A random effects meta-analysis indicated an overall significant association between self-compassion and sleep quality whereby higher self-compassion was associated with fewer disturbing sleep symptoms, r = − .32, 95%CI [− .36, − .28], as seen in the forest plot in Fig. 2.
Cochrane’s Q revealed no evidence of heterogeneity in effect sizes across studies q (16) = 16.81, p = 0.40. The I2 statistic was 3.2 (95%CI: [0.00, 68.52]), indicating that an estimated 3.2% of observed variation in effect sizes could be due to heterogeneity rather than chance. Since there was no significant between-study variance in effect sizes, moderator and subgroup analyses were not conducted.
Moderators of Overall Result
Non-significant heterogeneity can still be modelled using meta-regression (Field and Gillett 2010), so we considered if between-study differences in results could be explained by measures and participant age. Self-compassion measure (SCS versus SCS-SF) was not a significant moderator of results QM (1) = 3.25, p = .07. The non-significant trend favoured the full-length self-compassion scale. Likewise, measure of sleep quality was not a significant moderator QM (4) = 7.00, p = .14. Mean age also did not moderate results QM (1) = 2.70, p = .10.
Positive Self-compassion Versus Self-coldness
Six studies included information on the distinct effects of positive self-compassion and self-coldness (negative self-compassion). There was a small, significant association between positive self-compassion and sleep quality, r = − .15, 95%CI [− .24, − .05]. There was a stronger association between self-coldness and sleep quality, r = .36, 95%CI [.18, .52].
Study Quality
The reporting quality of included studies was relatively high (see Table 1). The most common domain that studies failed to report on was discussing participant exclusions from analysis, with only 5 of the 17 included studies providing this information. Another area of concern was that nearly half (8/17) of the studies failed to report on their strategy for handling missing data. Other domains, such as participant response rates (reported by 14/17 studies) and scale reliability coefficients (reported by 15/17 studies), were well documented by the majority of studies.
Risk of Publication Bias
Egger regression and rank correlation test for funnel plot asymmetry were both non-significant in the primary analysis, indicating no evidence of publication bias (Z = − .45, p = .65; Kendall τ = − .09, p = .66).
Discussion
This meta-analysis investigates the association between self-compassion and sleep quality. In a synthesis of 17 studies, we found evidence of a significant association between self-compassion and subjective sleep quality, whereby high self-compassion is associated with better sleep quality. Our overall effect size estimate (r = − .32) indicates that self-compassion and self-reported sleep quality share 32% (i.e. approximately one third) of common variance. When investigating the distinct associations between positive self-compassion and self-coldness and sleep quality, we found that self-coldness was a stronger predictor of sleep quality than positive self-compassion, although both associations were significant.
Self-compassion has been identified as being an emotional regulation strategy that can self-soothe distressing symptoms and reduce general suffering (Diedrich et al. 2016; Finlay-Jones et al. 2015). Sleep disturbances constitute a specific form of distress and can have a substantial negative impact on daily life functioning and overall health (Hertenstein et al. 2019; Morin and Benca 2012). While our findings are correlational and do not point to directions of causality, self-compassion may be a psychological resource that might facilitate greater subjective sleep quality and potentially enable people to relax and downregulate self-critical thoughts and emotions that interfere with good quality sleep. Indeed, early experimental work supports this hypothesis, whereby brief self-compassion exercises before bedtime have been found to lead to improved sleep quality, as measured by the Sleep Problems Questionnaire (Butz and Stahlberg 2018). It is also possible that the relationship between self-compassion and sleep quality is mediated by other psychological factors such as perceived stress (Hu et al. 2018; Kemper et al. 2015) or rumination (Butz and Stahlberg 2018). In addition, self-compassion has been shown to be linked to an important sleep-related behaviour, bedtime procrastination, partly through the use of cognitive reappraisal, which is itself an adaptive emotion regulation strategy (Sirois et al. 2019).
A growing number of research groups have found that self-coldness exhibits stronger associations with psychopathology, including symptoms of depression, anxiety and stress than positive self-compassion (Brenner et al. 2017; Körner et al. 2015; Muris et al. 2018). Our finding that self-coldness is more strongly associated with sleep quality than positive self-compassion echoes this idea, but the result should be interpreted with caution. First, data on the distinct association between sleep quality and positive self-compassion and self-coldness was only available for a subset of six of our included studies (combined n = 536). Within this subset, three studies used validated measures of sleep disturbance (Frank et al. 2015; Kim and Ko 2018; Vaillancourt and Wasylkiw 2019), whereas the remaining studies—conducted by a single research group—used a single-item measure of positive sleep quality (Trent et al. 2018, 2019a, b). Thus, data on the relationship between sleep quality and positive self-compassion compared with self-coldness is quite limited and based on heterogeneous measures of self-reported sleep quality. More research using validated measures of sleep quality is needed to help clarify this issue.
While all studies included in this meta-analysis measured self-compassion with either the 26- or 12-item Self Compassion Scale, there was heterogeneity in measures of sleep quality. The most widely used sleep scale was the 19-item PSQI, used in seven studies. Other scales utilised include the eight-item sleep subscale of the Patient-Reported Outcomes Measurement Information System (PROMIS; k = 3), the Insomnia Severity Index (ISI; k = 3) and a single-item measure of sleep quality, rated on a four-point scale (k = 3). While we found no evidence of between-study heterogeneity in effect sizes, it should be noted that these measures vary in quality and depth. The PSQI is a gold-standard measure incorporating seven components of sleep quality (Buysse et al. 1989). It is validated for both community and clinical populations and has good psychometric properties (Carpenter and Andrykowski 1998). While the PSQI’s length could be problematic in intervention-based research where sleep quality is one of a number of secondary outcomes, where feasible, we recommend its use in future studies investigating self-compassion and sleep quality. This will facilitate cross-study comparisons and enable higher quality research in the emerging field of self-compassion and sleep quality.
Limitations and Future Research
We included both cross-sectional and interventional studies in this meta-analysis to estimate the strength of the relationship between self-compassion and sleep quality. However, our study does not investigate directions of causality, and the interesting question of whether self-compassion-related interventions might lead to improvements in sleep quality, meditated through enhanced self-compassion, is a question that remains unanswered. The potential influence of sleep quality on self-compassion also cannot be excluded. We recommend that future randomised controlled trials of self-compassion-based interventions consider including sleep quality as an outcome measure. A recent meta-analysis of mindfulness meditation on sleep quality found evidence of moderate salutary effects of mindfulness compared with nonspecific active controls (Rusch et al. 2019). The construct of self-compassion overlaps with the construct of mindfulness, but it is distinct in that it explicitly includes the facets of common humanity and self-kindness (Neff and Dahm 2015). While the construct of mindfulness and mindfulness-based training programs such as mindfulness-based stress reduction often implicitly include coverage of relating to compassion and self-kindness (Neff and Dahm 2015; Rosch 2007), an explicit focus on self-compassion might be helpful in downregulating distressing thoughts and emotions relating to sleep symptoms. Thus, it would be interesting to consider the relative effects of self-compassion-based training on sleep compared with established effects reported for mindfulness meditation.
Notably, no studies examined the relationship between self-compassion and sleep quality using objective assessments of sleep such as polysomnography or actigraphy. As there tend to be discrepancies between objectively and subjectively measured sleep quality (Bei et al. 2015), it would be interesting to see if the relationship between self-compassion and sleep holds using objective sleep quality measures. While the field of self-compassion research is dominated by use of the self-report SCS (Neff 2003b) or SCS-SF (Raes et al. 2011), to improve validity, it could be useful to consider other ways of measuring the construct, for instance through direct measurement of observed self-compassionate responses or observational ratings (Strauss et al. 2016).
We found evidence of a small to medium-strength correlation between self-compassion and sleep problems (r = − 0.32), and prior research has found stronger relationships between sleep quality and psychopathology such as symptoms of depression, anxiety and stress (Benca et al. 1992; Kim and Ko 2018). Sleep disturbance is a key feature of many clinical disorders, including depression and anxiety, which helps explain these stronger associations. This also indicates that it is important to consider other psychological factors in addition to self-compassion when understanding an individual’s sleep (Calkins et al. 2013).
As research is still emerging, any clinical implications are largely speculative at this stage. Future research examining a potential causal relationship between self-compassion and sleep quality, or any difference in the relationship between positive self-compassion, self-coldness and sleep quality may provide useful clinical directions. For example, an important consideration would be whether decreasing self-coldness (as opposed to increasing positive self-compassion) would be a useful clinical intervention for improving subjective sleep quality or whether addressing both positive and negative facets of self-compassion would be equally useful when designing clinical interventions to improve sleep quality. Furthermore, studies investigating relationships between self-compassion and sleep quality in child and adolescent samples would be a valuable avenue to pursue in future research.
In sum, our meta-analysis of 17 studies found evidence of a significant association between self-compassion and self-reported sleep quality. Future research is needed to expand on these early results, and specifically to investigate directions of causality in order to better understand the nature of the relationship between self-compassion and sleep quality. Investigating the potential role of self-compassion-based therapies in enhancing sleep quality is also worth considering in future research.
References
Baker, F. C., de Zambotti, M., Colrain, I. M., & Bei, B. (2018). Sleep problems during the menopausal transition: prevalence, impact, and management challenges. Nature and Science of Sleep, 10, 73–95. https://doi.org/10.2147/NSS.S125807.
Banks, S., & Dinges, D. F. (2007). Behavioral and physiological consequences of sleep restriction. Journal of Clinical Sleep Medicine, 3(5), 519–528. https://doi.org/10.5664/jcsm.26918.
Bei, B., Coo, S., Baker, F. C., & Trinder, J. (2015). Sleep in women: a review. Australian Psychologist, 50(1), 14–24. https://doi.org/10.1111/ap.1209.
Benca, R. M., Obermeyer, W. H., Thisted, R. A., & Gillin, J. C. (1992). Sleep and psychiatric disorders: a meta-analysis. Archives of General Psychiatry, 49(8), 651–668. https://doi.org/10.1001/archpsyc.1992.01820080059010.
Brenner, R. E., Heath, P. J., Vogel, D. L., & Credé, M. (2017). Two is more valid than one: examining the factor structure of the self-compassion scale (SCS). Journal of Counseling Psychology, 64(6), 696–707. https://doi.org/10.1037/cou0000211.
Bricklin-Small, D. (2017). The relationship between self-compassion and sleep in the college population (Publication No. 10268331) [Doctoral dissertation, William James College]. ProQuest Dissertations and Theses.
Brown, L., Bryant, C., Brown, V., Bei, B., & Judd, F. (2016). Self-compassion, attitudes to ageing and indicators of health and well-being among midlife women. Aging & Mental Health, 20(10), 1035–1043. https://doi.org/10.1080/13607863.2015.1060946.
Butz, S., & Stahlberg, D. (2018). Can self-compassion improve sleep quality via reduced rumination? Self and Identity, 17(6), 666–686. https://doi.org/10.1080/15298868.2018.1456482.
Buysse, D. J., Reynolds III, C. F., Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213. https://doi.org/10.1016/0165-1781(89)90047-4.
Calkins, A. W., Hearon, B. A., Capozzoli, M. C., & Otto, M. W. (2013). Psychosocial predictors of sleep dysfunction: the role of anxiety sensitivity, dysfunctional beliefs, and neuroticism. Behavioral Sleep Medicine, 11(2), 133–143. https://doi.org/10.1080/15402002.2011.643968.
Cappuccio, F. P., Taggart, F. M., Kandala, N.-B., Currie, A., Peile, E., Stranges, S., & Miller, M. A. (2008). Meta-analysis of short sleep duration and obesity in children and adults. Sleep, 31(5), 619–626. https://doi.org/10.1093/sleep/31.5.619.
Carpenter, J. S., & Andrykowski, M. A. (1998). Psychometric evaluation of the Pittsburgh sleep quality index. Journal of Psychosomatic Research, 45(1), 5–13. https://doi.org/10.1016/S0022-3999(97)00298-5.
Christopher, M. S., Hunsinger, M., Goerling, L., Bowen, S., Rogers, B. S., Gross, C. R., Dapolonia, E., & Pruessner, J. C. (2018). Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: a feasibility and preliminary efficacy trial. Psychiatry Research, 264, 104–115. https://doi.org/10.1016/j.psychres.2018.03.059.
Diedrich, A., Hofmann, S. G., Cuijpers, P., & Berking, M. (2016). Self-compassion enhances the efficacy of explicit cognitive reappraisal as an emotion regulation strategy in individuals with major depressive disorder. Behaviour Research and Therapy, 82, 1–10. https://doi.org/10.1016/j.brat.2016.04.003.
Dvorakova, K., Kishida, M., Li, J., Elavsky, S., Broderick, P. C., Agrusti, M. R., & Greenberg, M. T. (2017). Promoting healthy transition to college through mindfulness training with first-year college students: pilot randomized controlled trial. Journal of American College Health, 65(4), 259–267. https://doi.org/10.1080/07448481.2017.1278605.
Field, A. P., & Gillett, R. (2010). How to do a meta-analysis. British Journal of Mathematical and Statistical Psychology, 63(3), 665–694. https://doi.org/10.1348/000711010X502733.
Finlay-Jones, A. L., Rees, C. S., & Kane, R. T. (2015). Self-compassion, emotion regulation and stress among Australian psychologists: testing an emotion regulation model of self-compassion using structural equation modeling. PLoS One, 10(7), e0133481. https://doi.org/10.1371/journal.pone.0133481.
Frank, J. L., Reibel, D., Broderick, P., Cantrell, T., & Metz, S. (2015). The effectiveness of mindfulness-based stress reduction on educator stress and well-being: results from a pilot study. Mindfulness, 6(2), 208–216. https://doi.org/10.1007/s12671-013-0246-2.
Gross, J. J. (1998). Antecedent-and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology, 74(1), 224–237. https://doi.org/10.1037/0022-3514.74.1.224.
Hertenstein, E., Feige, B., Gmeiner, T., Kienzler, C., Spiegelhalder, K., Johann, A., Jansson-Fröjmark, M., Palagini, L., Rücker, G., Riemann, D., & Baglioni, C. (2019). Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Medicine Reviews, 43, 96–105. https://doi.org/10.1016/j.smrv.2018.10.006.
Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. https://doi.org/10.1136/bmj.327.7414.557.
Hu, Y., Wang, Y., Sun, Y., Arteta-Garcia, J., & Purol, S. (2018). Diary study: the protective role of self-compassion on stress-related poor sleep quality. Mindfulness, 9(6), 1931–1940. https://doi.org/10.1007/s12671-018-0939-7.
Hwang, Y.-S., Goldstein, H., Medvedev, O. N., Singh, N. N., Noh, J.-E., & Hand, K. (2019). Mindfulness-based intervention for educators: effects of a school-based cluster randomized controlled study. Mindfulness, 10(7), 1417–1436. https://doi.org/10.1007/s12671-019-01147-1.
Irwin, M. R., Olmstead, R., & Carroll, J. E. (2016). Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biological Psychiatry, 80(1), 40–52. https://doi.org/10.1016/j.biopsych.2015.05.014.
Jenkins, C. D., Stanton, B.-A., Niemcryk, S. J., & Rose, R. M. (1988). A scale for the estimation of sleep problems in clinical research. Journal of Clinical Epidemiology, 41(4), 313–321. https://doi.org/10.1016/0895-4356(88)90138-2.
Jeste, D. V., Glorioso, D., Lee, E. E., Daly, R., Graham, S., Liu, J., Paredes, A. M., Nebeker, C., Tu, X. M., Twamley, E. W., Van Patten, R., Yamada, Y., Depp, C., & Kim, H.-C. (2019). Study of independent living residents of a continuing care senior housing community: sociodemographic and clinical associations of cognitive, physical, and mental health. American Journal of Geriatric Psychiatry, 27(9), 895–907. https://doi.org/10.1016/j.jagp.2019.04.002.
Kemper, K. J., Mo, X., & Khayat, R. (2015). Are mindfulness and self-compassion associated with sleep and resilience in health professionals? The Journal of Alternative and Complementary Medicine, 21(8), 496–503. https://doi.org/10.1089/acm.2014.0281.
Kim, C., & Ko, H. (2018). The impact of self-compassion on mental health, sleep, quality of life and life satisfaction among older adults. Geriatric Nursing, 39(6), 623–628. https://doi.org/10.1016/j.gerinurse.2018.06.005.
Körner, A., Coroiu, A., Copeland, L., Gomez-Garibello, C., Albani, C., Zenger, M., & Brähler, E. (2015). The role of self-compassion in buffering symptoms of depression in the general population. PLoS One, 10(10), e0142027. https://doi.org/10.1371/journal.pone.0136598.
LeBlanc, M., Beaulieu-Bonneau, S., Mérette, C., Savard, J., Ivers, H., & Morin, C. M. (2007). Psychological and health-related quality of life factors associated with insomnia in a population-based sample. Journal of Psychosomatic Research, 63(2), 157–166. https://doi.org/10.1016/j.jpsychores.2007.03.004.
Losilla, J.-M., Oliveras, I., Marin-Garcia, J. A., & Vives, J. (2018). Three risk of bias tools lead to opposite conclusions in observational research synthesis. Journal of Clinical Epidemiology, 101, 61–72. https://doi.org/10.1016/j.jclinepi.2018.05.021.
Morin, C. M., & Benca, R. (2012). Chronic insomnia. The Lancet, 379(9821), 1129–1141. https://doi.org/10.1016/S0140-6736(11)60750-2.
Muris, P., van den Broek, M., Otgaar, H., Oudenhoven, I., & Lennartz, J. (2018). Good and bad sides of self-compassion: a face validity check of the self-compassion scale and an investigation of its relations to coping and emotional symptoms in non-clinical adolescents. Journal of Child and Family Studies, 27(8), 2411–2421. https://doi.org/10.1007/s10826-018-1099-z.
Neff, K. D. (2003a). Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032.
Neff, K. D. (2003b). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860309027.
Neff, K. D., & Dahm, K. A. (2015). Self-compassion: what it is, what it does, and how it relates to mindfulness. In B. Ostafin, M. Robinson, & B. Meier (Eds.), Handbook of mindfulness and self-regulation (pp. 121–137). Springer. https://doi.org/10.1007/978-1-4939-2263-5_10.
O’Connor, S. R., Tully, M. A., Ryan, B., Bradley, J. M., Baxter, G. D., & McDonough, S. M. (2015). Failure of a numerical quality assessment scale to identify potential risk of bias in a systematic review: a comparison study. BMC Research Notes, 8(1), 224. https://doi.org/10.1186/s13104-015-1181-1.
O'Leary, K., Bylsma, L. M., & Rottenberg, J. (2017). Why might poor sleep quality lead to depression? A role for emotion regulation. Cognition and Emotion, 31(8), 1698–1706. https://doi.org/10.1080/02699931.2016.1247035.
Parthasarathy, S., Vasquez, M. M., Halonen, M., Bootzin, R., Quan, S. F., Martinez, F. D., & Guerra, S. (2015). Persistent insomnia is associated with mortality risk. The American Journal of Medicine, 128(3), 268–275. https://doi.org/10.1016/j.amjmed.2014.10.015.
Phillips, W. J., & Ferguson, S. J. (2013). Self-compassion: a resource for positive aging. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 68(4), 529–539. https://doi.org/10.1093/geronb/gbs091.
Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016). Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Annals of Internal Medicine, 165(2), 125–133. https://doi.org/10.7326/M15-2175.
Raes, F., Pommier, E., Neff, K. D., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702.
Rosch, E. (2007). More than mindfulness: when you have a tiger by the tail, let it eat you. Psychological Inquiry, 18(4), 258–264. https://doi.org/10.1080/10478400701598371.
Rosenthal, R., & DiMatteo, M. (2001). Meta-analysis: recent developments in quantitative methods for literature reviews. Annual Review of Psychology, 52, 59–82. https://doi.org/10.1146/annurev.psych.52.1.59.
Rusch, H. L., Rosario, M., Levison, L. M., Olivera, A., Livingston, W. S., Wu, T., & Gill, J. M. (2019). The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences, 1445(1), 5–16. https://doi.org/10.1111/nyas.13996.
Sirois, F. M., & Hirsch, J. K. (2019). Self-compassion and adherence in five medical samples: the role of stress. Mindfulness, 10(1), 46–54. https://doi.org/10.1007/s12671-018-0945-9.
Sirois, F. M., Kitner, R., & Hirsch, J. K. (2015). Self-compassion, affect, and health-promoting behaviors. Health Psychology, 34(6), 661–669. https://doi.org/10.1037/hea0000158.
Sirois, F. M., Nauts, S., & Molnar, D. S. (2019). Self-compassion and bedtime procrastination: an emotion regulation perspective. Mindfulness, 10(3), 434–445. https://doi.org/10.1007/s12671-018-0983-3.
Strauss, C., Taylor, B. L., Gu, J., Kuyken, W., Baer, R., Jones, F., & Cavanagh, K. (2016). What is compassion and how can we measure it? A review of definitions and measures. Clinical Psychology Review, 47, 15–27. https://doi.org/10.1016/j.cpr.2016.05.004.
Terry, M. L., & Leary, M. R. (2011). Self-compassion, self-regulation, and health. Self and Identity, 10(3), 352–362. https://doi.org/10.1080/15298868.2011.558404.
Trent, N. L., Borden, S., Miraglia, M., Pasalis, E., Dusek, J. A., & Khalsa, S. B. S. (2019a). Improvements in psychological and occupational well-being following a brief yoga-based program for education professionals. Global Advances in Health and Medicine, 8, 1–11. https://doi.org/10.1177/2164956119856856.
Trent, N. L., Borden, S., Miraglia, M., Pasalis, E., Dusek, J. A., & Khalsa, S. B. S. (2019b). Improvements in psychological and occupational well-being in a pragmatic controlled trial of a yoga-based program for professionals. The Journal of Alternative and Complementary Medicine., 25(6), 593–605. https://doi.org/10.1089/acm.2018.0526.
Trent, N. L., Miraglia, M., Dusek, J. A., Pasalis, E., & Khalsa, S. B. S. (2018). Improvements in psychological health following a residential yoga-based program for frontline professionals. Journal of Occupational and Environmental Medicine, 60(4), 357–367. https://doi.org/10.1097/JOM.0000000000001216.
Vaillancourt, E. S., & Wasylkiw, L. (2019). The intermediary role of burnout in the relationship between self-compassion and job satisfaction among nurses. Canadian Journal of Nursing Research. https://doi.org/10.1177/0844562119846274.
Viechtbauer, W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. https://doi.org/10.18637/jss.v036.i03.
Walsh, J. K., & Üstün, T. B. (1999). Prevalence and health consequences of insomnia. Sleep., 22, S427–S436.
Zeng, X., Zhang, Y., Kwong, J. S. W., Zhang, C., Li, S., Sun, F., Niu, Y., & Du, L. (2015). The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. Journal of Evidence-Based Medicine, 8(1), 2–10. https://doi.org/10.1111/jebm.12141.
Author information
Authors and Affiliations
Contributions
LB: collaborated in study design, conducted the literature search and data analysis and wrote the first draft of the paper. EH: collaborated with the study design, assisted with the literature search and writing of the paper. HL: collaborated with the design and writing of the study.
CB: collaborated in study design and writing and editing of the final manuscript. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brown, L., Houston, E.E., Amonoo, H.L. et al. Is Self-compassion Associated with Sleep Quality? A Meta-analysis. Mindfulness 12, 82–91 (2021). https://doi.org/10.1007/s12671-020-01498-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-020-01498-0