Abstract
Objectives
Growing evidence supports the efficacy of mindfulness-based interventions for symptoms in cancer survivors. Identifying theory-based psychological processes underlying their effects on symptoms would inform research to enhance their efficacy and cost-effectiveness. We conducted secondary analyses examining the effect of mindfulness-based stress reduction (MBSR) for cancer-related fatigue on mindfulness facets, self-compassion, and psychological inflexibility. We also examined whether changes in these processes were associated with the symptom outcomes of fatigue interference, sleep disturbance, and emotional distress.
Methods
Thirty-five persistently fatigued cancer survivors (94% female, 77% breast cancer survivors) were randomized to either MBSR for cancer-related fatigue or a waitlist control (WC) condition. Self-report measures were administered at pre-intervention, post-intervention, and 1-month follow-up. Then the WC group received MBSR and completed a post-intervention follow-up.
Results
Linear mixed modeling analyses of the first three time points showed steady increases over time for certain mindfulness facets (observing, acting with awareness, and nonjudging) and self-compassion in favor of the MBSR group. When analyzing pre- and post-intervention data across study conditions, none of the psychological processes predicted change in fatigue interference. However, increased nonjudging was associated with decreased sleep disturbance (β = −.39, p = 0.003), and increased acting with awareness was associated with decreased emotional distress (β = − 0.36, p = 0.003). Self-compassion did not predict change in symptom outcomes.
Conclusions
Results point to specific psychological processes that may be targeted to maximize the efficacy of future MBSR interventions for cancer survivors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Advances in early detection and treatment of cancer have resulted in steady increases in the number of cancer survivors (Jemal et al. 2017). Although the growth in cancer survivorship is encouraging, survivors often experience debilitating symptoms for months or even years following treatment (Bower 2014; Jones et al. 2016; Noordman et al. 2018). Common symptoms include fatigue, sleep disturbance, depression, and anxiety (Cleeland et al. 2013). As many as 80% of patients have reported cancer-related fatigue (CRF) during treatment and 53% following completion of treatment (Henry et al. 2008; Jones et al. 2016; Wang et al. 2014). Furthermore, up to 34% reported experiencing CRF 5 to 10 years post-diagnosis (Bower et al. 2006; Jones et al. 2016). CRF has been strongly linked to increased depressive symptoms and anxiety, greater disability, and decreased work productivity and activity engagement (Berger, Gerber, and Mayer 2012; Dorland et al. 2018; Jones et al. 2016). Currently, pharmacological treatments for CRF have shown limited evidence of efficacy (Minton et al. 2011), whereas evidence for psychosocial interventions targeting CRF has been growing (Haller et al. 2017; Mustian et al. 2017).
Mindfulness-based interventions have been identified as a promising approach for managing common cancer-related symptoms (Zhang, Zhao, and Zheng 2019). Specifically, these interventions have led to improved sleep and decreased fatigue, emotional distress, and fear of cancer recurrence in cancer survivors (Hall et al. 2018; Zhang et al. 2019). Mindfulness-based interventions are hypothesized to reduce symptoms by targeting several psychological processes, including mindfulness, self-compassion, and psychological inflexibility (Gu, Strauss, Bond, and Cavanagh 2015; Kuyken et al. 2010). Mindfulness has been commonly defined as intentionally attending to the present moment with an open, nonjudgmental, and nonreactive stance (Kabat-Zinn 1994). One common conceptualization of mindfulness includes five key facets: (1) observing, which refers to noticing and attending to experiences in and outside of oneself, (2) describing, which refers to labeling internal experiences with words, (3) acting with awareness, which involves purposeful attention to one’s present activities, (4) nonjudging of inner experience, which refers to taking a nonevaluative stance toward thoughts and feelings, and (5) nonreactivity to inner experience, which refers to the tendency to allow thoughts and feelings to come and go without being caught up in them (Baer et al. 2008). Mindfulness-based interventions may also impact self-compassion, which is the ability to be kind to oneself when faced with personal suffering (Neff 2003a). Finally, these interventions may impact psychological inflexibility, which refers to behavior patterns driven by internal reactions (e.g., thoughts and feelings) rather than personal values, and is thought to be at the core of most human suffering (Hayes et al. 2013; Hayes et al. 1996).
Although growing evidence suggests that mindfulness-based interventions reduce cancer-related symptoms, including fatigue (Zhang et al. 2019), limited research has examined psychological processes that may be driving these effects. Studies exploring such processes are critical because they can inform optimization of interventions to maximize therapeutic effects (Kazdin 2007). One meta-analysis on primarily non-cancer populations examined potential mediators of the mental health effects of mindfulness-based interventions and found moderate evidence for mindfulness, rumination, and worry as mediators (Gu et al. 2015). Studies examining mediators of mindfulness-based interventions in cancer populations have also primarily focused on mental health outcomes (e.g., Boyle et al. 2017; Labelle et al. 2015). These studies have yielded mixed support for the potential mechanism of mindfulness and preliminary support for the potential mechanisms of self-kindness, fear of recurrence, and rumination (e.g., Boyle et al. 2017; Labelle et al. 2015). To date, only one study has examined processes underlying mindfulness-based intervention’s effects on fatigue and sleep disturbance, which were secondary outcomes of an online mindfulness course for work-related rumination (Querstret, Cropley, and Fife-Schaw 2017). In this trial, acting with awareness was the only mindfulness facet to significantly mediate the intervention’s effects on rumination, fatigue, and sleep disturbance.
The current study is a secondary data analysis of potential psychological mechanisms underlying the effects of a mindfulness-based stress reduction (MBSR) intervention for cancer-related fatigue. We examined several mechanisms (i.e., mindfulness, self-compassion, and psychological inflexibility) underlying our intervention’s effects on both physical and psychological symptoms. We hypothesized that (1) MBSR would lead to increases in facets of mindfulness (i.e., observing, describing, acting with awareness, nonjudging, and nonreactivity) and self-compassion and decreases in psychological inflexibility compared with the waitlist control (WC) condition, and that (2) changes in these processes following MBSR would be associated with reductions in symptoms (i.e., fatigue interference, sleep disturbance, and emotional distress).
Method
Participants
Thirty-five cancer survivors who had completed active treatment (average time since completion = 51.3 months [SD = 39.3 months]) participated in this pilot trial. Eligible individuals were adult cancer survivors (18 + years of age) who reported clinically significant CRF (score ≥ 4 on the Fatigue Symptom Inventory (FSI) severity composite (Hann et al. 1998)) for the past 8 weeks or longer. Individuals were excluded if they (1) had received cancer treatment, with the exception of hormonal therapy, in the previous 3 months; (2) were enrolled in hospice care; (3) had severe hearing impairment; (4) were experiencing severe depression (defined by a score ≥ 20 on the Patient Health Questionnaire-8 (PHQ-8; Kroenke et al. 2009); (5) had taken a mindfulness meditation course; or (6) lacked English fluency.
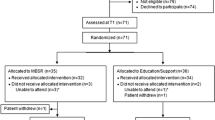
Procedure
Following institutional review board approval and registration with ClinicalTrials.gov (NCT01247532), participants were recruited from clinics affiliated with the Indiana University (IU) Simon Cancer Center, IU cancer research recruitment registries, or via self-referral from support or treatment facilities in Indianapolis. Descriptions of study procedures have been published in the primary outcome paper (Johns et al. 2015). Briefly, of the 159 people who were assessed for eligibility, 67 (42%) did not meet the CRF clinical cutoff, 7 (4%) had severe depression, 2 (1%) had previous mindfulness training, and 48 (30%) declined to participate. Primary reasons for refusal were time constraints and travel distance. The remaining 35 individuals provided informed consent, completed the baseline assessment during group enrollment sessions, and were randomized in blocks of four to either the MBSR class (n = 18) or the WC condition (n = 17).
The MBSR intervention was a series of 7 weekly classes, each 2 h in length, and included mindfulness practices, psychoeducation related to CRF, and home practice. The class was taught by a physician with extensive experience teaching MBSR. The MBSR course was adapted for cancer survivors but maintained fidelity to the standard MBSR program. Adaptations for cancer survivors included 2-h rather than 2.5-h classes, seven instead of eight classes, no extended day-long retreat, the addition of psychoeducation related to CRF, shortened inquiry at the end of practices, and shorter (20 min) home practice sessions. The curriculum was presented in the same sequence as the standard MBSR program, except that the mindful movement practice was introduced in session 2 rather than 3. Adaptations were supported by previous studies suggesting that reduction of class time does not decrease the effectiveness of MBSR and may reduce barriers to participation for populations with significant symptom burden (Carmody and Baer 2009). Psychoeducation on fatigue was added to tailor the material to the cancer experience, consistent with the National Comprehensive Cancer Network (NCCN) guidelines (Berger et al. 2015).
The first class session included an overview of the MBSR intervention followed by practice of mindful eating, mindful breathing, and a body scan. Participants were also introduced to guided meditations and other exercises on the CD for assigned home practice each week. In sessions 2 and 3, participants practiced the body scan, gentle hatha yoga, and awareness of breath meditation and learned about stress and sleep hygiene. In sessions 4, 5, and 6, participants deepened their practice and discussed full incorporation of the skills into their life. Finally, session 7 included further mindfulness practice, review of course topics, and strategies to maintain mindfulness practice. Throughout the course, participants were encouraged to practice daily mindfulness exercises and record this practice on a diary card. Additional intervention details are provided in the main study paper (Johns et al. 2015).
Outcomes were assessed at 3 or 4 time points, depending on the randomization arm. The first 3 time points, baseline prior to randomization (T1), post-intervention (T2), and 1-month follow-up (T3), were identical for both groups. Following assessment at T3, the WC group completed their respective MBSR course, followed by an assessment (T4). Two MBSR groups were held for each study condition, with 8–10 participants in each group.
All measures were administered in person on paper-based forms at T1 and T2, while at T3 and T4, participants had the option of completing measures in person or mailing them to the study team. Retention was excellent; all 35 participants completed assessments at T1, T2, and T3. Only one participant did not complete the assessment at T4.
Measures
Mindfulness
Mindfulness was measured with the Five Factor Mindfulness Questionnaire (FFMQ). The FFMQ is a 39-item measure with five subscales (observing, describing, acting with awareness, nonjudging of inner experience, and nonreactivity to inner experience) that are summed together to compute a total mindfulness score (Baer et al. 2006). Participants rated how true each item was for them (e.g., “I perceive my feelings and emotions without having to react to them”) on a scale from 1 (never or very rarely true) to 5 (very often or always true). Cronbach’s alpha coefficients have ranged from 0.75 to 0.91 for the total instrument and its five subscales (Baer et al. 2006). Construct validity also has been established, as four of the facets (all except for acting with awareness) have been associated with meditation experience (Baer et al. 2008). The FFMQ has been used with cancer populations, with excellent internal consistency (e.g., α = 0.92 for the total instrument) (Nakamura, Lipschitz, Kuhn, Kinney, and Donaldson 2013). In the present study, baseline internal consistency for the total instrument was 0.94, and baseline internal consistencies for the subscales were as follows: nonreactivity (α = 0.68), observing (α = 0.75), acting with awareness (α = 0.95), describing (α = 0.93), and nonjudging (α = 0.91).
Self-Compassion
Self-compassion was assessed with the 12-item Self-Compassion Scale-Short Form (SCS-SF; Neff 2003b). The measure contains three positive subscales (self-kindness, common humanity, and mindfulness) and three reverse-scored negative subscales (isolation, self-judgment, and over-identification), which are summed to create a composite score for self-compassion. Participants rated each item (e.g., “When I’m going through a very hard time, I give myself the caring and tenderness I need”) on a scale ranging from 1 (almost never) to 5 (almost always). The SCS-SF has shown good internal consistency with Cronbach’s alphas of 0.86 or higher and is highly correlated with the long form of the scale (rs ≥ 0.97 in all samples) (Raes, Pommier, Neff, and Van Gucht 2011). The SCS-SF also has demonstrated good discriminant validity, as it is not related to social desirability (Neff 2003b). In addition, the SCS-SF is negatively correlated with self-criticism and positively correlated with social connectedness, providing evidence of construct validity (Neff 2003b). Recent studies using the SCS with cancer populations found excellent internal consistency for both the full length scale (αs = 0.96 and 0.92) (Nakamura et al. 2013; Przezdziecki et al. 2013) and the short form (α = 0.91) (Sherman, Woon, French, and Elder 2017). In the present study, internal consistency for the SCS-SF at baseline was 0.90.
Psychological Inflexibility
Psychological inflexibility, which refers to an unwillingness to experience unwanted thoughts and feelings, was assessed using the 7-item Acceptance and Action Questionnaire-II (AAQ-II; Bond et al. 2011). Participants rated the items such as, “I’m afraid of my feelings,” on a scale from 1 (never true) to 7 (always true). The scale has demonstrated good internal consistency, with a mean alpha coefficient of 0.84 (Bond et al. 2011). Evidence of construct validity includes relationships between greater psychological inflexibility on the AAQ-II and higher levels of depressive symptoms, anxiety, stress, and other psychopathology (Bond et al. 2011). Recent studies with cancer patients have found the AAQ-II’s internal consistency to be acceptable (αs = 0.78 to 0.87) (Feros, Lane, Ciarrochi, and Blackledge 2013; Labelle et al. 2015). Baseline internal consistency for the AAQ-II in the current study was 0.91.
Fatigue Interference
The 7-item fatigue interference subscale of the Fatigue Symptom Inventory (FSI) assessed the degree to which fatigue disrupted cognition, mood, and activities in the past week (Hann et al. 1998). Each item is rated on an 11-point scale from 0 (no interference) to 10 (extreme interference). The FSI has been validated in patients with various cancers (Hann, Denniston, and Baker 2000). Construct validity was evidenced by negative correlations with life satisfaction and positive correlations with depressive symptoms (Hann et al. 2000). Additionally, patients undergoing cancer treatment showed higher FSI scores than those who were less than 1-year post-treatment. Convergent validity was evidenced by strong positive correlations of the FSI with an existing measure of fatigue. Internal consistency for the interference subscale was 0.94 in prior research (Hann et al. 2000) and 0.95 in the current study at baseline.
Sleep Disturbance
Insomnia severity and the impact of sleep difficulties on daily functioning over the past 2 weeks were assessed with the 7-item Insomnia Severity Index (ISI; Morin 1993). The ISI employs a 5-point scale from 0 (none) to 4 (very) with varying anchors (e.g., interference, satisfaction). A sample item asks for level of “difficulty falling asleep.” Construct validity for cancer patients was evidenced by positive correlations with other established measures of sleep and negative correlations with quality of life (Savard, Savard, Simard, and Ivers 2005). Internal consistency for the ISI was 0.90 in prior research with cancer patients (Savard et al. 2005) and the current research at baseline.
Emotional Distress
Emotional distress was calculated by summing the z-scores for the Patient Health Questionnaire-8 (PHQ-8), an 8-item measure of depressive symptoms, and the Generalized Anxiety Disorder Scale (GAD-7), a 7-item anxiety measure (Kroenke, Spitzer, Williams, Monahan, and Lowe 2007; Kroenke et al. 2009). Participants rated items such as how often they were bothered by “feeling down, depressed, or hopeless” (PHQ-8) and “not being able to stop or control worrying” (GAD-7) in the past 2 weeks on a Likert-type scale. Response options were 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day. Construct validity has been demonstrated for both measures in the general population (Kroenke et al. 2009; Löwe et al. 2008). Both measures have also been used in studies with cancer populations with evidence of good internal consistency (αs = 0.86–0.91) (Gonzalez et al. 2014; Kroenke et al. 2010). In the current sample, baseline internal consistency was 0.83 for the PHQ-8 and 0.85 for the GAD-7. Pre-treatment scores on the PHQ-8 and GAD-7 were highly correlated (r = 0.77); thus, the scores were combined to compute a total emotional distress score.
Data Analyses
Preliminary Analyses
Data analyses were conducted in SPSS version 23.0 (IBM Corp., Armonk, NY, USA). Baseline comparisons (t tests and chi-square analyses or Fisher’s exact tests) of demographic and medical characteristics and study variables between the MBSR and WC groups were first performed.
Hypothesis 1
A linear mixed modeling approach was employed to examine the impact of the MBSR intervention (n = 18) compared with the WC group (n = 17) on five facets of mindfulness (i.e., observing, describing, acting with awareness, nonjudging of inner experience, nonreactivity to inner experience), self-compassion, and psychological inflexibility. Each model included the main effects of time (T1, T2, and T3) and study group (MBSR or WC) and the time × group interaction. Both time and study group were treated as categorical variables in these models, focusing the analyses on average differences between groups and across time. A treatment effect was evidenced by a significant time × group interaction. However, given that this was a pilot study, our primary goal was to derive effect size estimates rather than test for statistical significance.
Hypothesis 2
After identifying psychological processes that significantly increased in the MBSR group, we used multiple linear regression to examine the extent to which these increases predicted change in symptom outcomes (fatigue interference, sleep disturbance, and emotional distress) pre- and post-MBSR. First, the WC group’s data at T3 were merged with the MBSR group’s data at T1; thus, the new variables included all data collected shortly before the MBSR courses for both groups (n = 35 across groups). The WC group’s data at T4 were merged with the MBSR group’s data at T2 to include all data collected immediately post-MBSR (n = 34 across groups). Following data reorganization, residualized change scores were computed by regressing the post-treatment value of each psychological process onto its pre-treatment value. The standardized residuals from these analyses were then used in our analyses for Hypothesis 2 (Cronbach and Furby 1970; MacKinnon 2008). Residualized change scores account for potential variability in pre-treatment scores, extracting out change predicted from regression toward the mean. Multiple linear regression analyses were conducted with the pre-treatment symptom level (fatigue interference, sleep disturbance, or emotional distress) in step 1, the residualized change score for the psychological process in step 2, and the post-treatment symptom level as the dependent variable. We chose to test one psychological process per model rather than entering all processes in the same model to avoid an insufficient case-to-independent variable ratio. Again, our primary goal was to compute effect size estimates for each analysis. A Bonferroni correction was used to limit the family-wise error rate, such that the significance threshold was adjusted from p < 0.05 to p < 0.00417.
Results
Preliminary Analyses
Table 1 presents participant characteristics by study group and group comparisons at baseline. Demographic and medical variables did not differ between groups, except for a higher rate of mental health treatment within the previous 6 months at baseline for WC participants compared with MBSR participants. There were significant bivariate correlations between history of mental health treatment and acting with awareness, self-compassion, and psychological inflexibility, though these processes did not significantly differ between groups at baseline. Mental health treatment was not significantly associated with any symptom outcomes at baseline.
Levels of observing and nonreactivity were significantly lower at baseline for WC participants compared with MBSR participants. All other study variables, including symptom outcomes, did not significantly differ between groups at baseline (see Table 1).
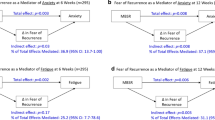
Intervention Effects on Psychological Processes
Seven linear mixed models were conducted to examine the impact of MBSR compared with WC on the five facets of mindfulness, self-compassion, and psychological inflexibility. These analyses revealed significant main effects of study group in favor of MBSR for all facets of mindfulness (observing, describing, acting with awareness, nonjudging, and nonreactivity), self-compassion, and psychological inflexibility (see Table 2). Analyses also showed significant group × time effects for observing, acting with awareness, nonjudging, and self-compassion (see Table 2). The interaction means displayed in Fig. 1–d show steady increases in each of these psychological processes for the MBSR group, whereas the means for the WC group remained relatively stable or slightly declined over time. Effect sizes (partial rs) ranged from 0.22 to 0.30 for significant group × time effects, compared with a range from 0.11 to 0.18 for nonsignificant group × time effects on describing, nonreactivity, and psychological inflexibility.
Associations Between Changes in Psychological Processes and Symptom Improvement
Multiple linear regression analyses were conducted to examine whether significant change in the psychological processes following MBSR were linked to reduced symptoms post-intervention. Models were constructed for each of the four predictors (i.e., observing, acting with awareness, nonjudging, and self-compassion) of the three symptoms (total = 12 models). As shown in Table 3, none of the predictors were significantly associated with fatigue interference, with effect sizes (βs) ranging from 0.02 for observing and nonjudging to − 0.24 for acting with awareness (p < 0.07). However, increases in nonjudging showed a significant, moderate association with lower levels of sleep disturbance (β = − 0.39, p = 0.003), and increases in acting with awareness showed a significant, moderate association with decreased emotional distress (β = − 0.36, p = 0.003). None of the other associations between changes in psychological processes and study outcomes were statistically significant.
Discussion
The present study provides new information regarding the impact of MBSR on theory-driven psychological processes and their relationships to symptom outcomes in cancer survivors. Consistent with our hypotheses, MBSR led to increases in mindfulness (i.e., observing, acting with awareness, nonjudging) and self-compassion as compared with the WC group. These processes were targeted in MBSR, as survivors practiced nonjudgmental awareness of the present moment and self-compassionate behaviors (e.g., grounding of breath during stressful experiences). Our results converge with prior research that found positive changes in cancer patients’ mindfulness and self-compassion following mindfulness-based interventions to improve their mental health (Bränström et al. 2010; Schellekens et al. 2017). Additionally, in our study, change in two of the four psychological processes predicted symptom outcomes. First, increases in nonjudging were linked to moderate decreases in sleep disturbance. Nonjudging has been associated with fewer ruminative thoughts, such as negative self-focused cognitions, that have been related to sleep disturbance (Carney, Harris, Falco, and Edinger 2013). Thus, a more nonjudgmental attitude toward these thoughts may help lessen their impact on sleep. Second, increases in acting with awareness were related to decreased emotional distress, consistent with findings with general population samples (Baer et al. 2006; Cash and Whittingham 2010) and cancer patients who completed MBSR (Garland, Tamagawa, Todd, Speca, and Carlson 2013). This relationship may be due to survivors’ increased ability to engage themselves in activities or find increased meaning in those activities by more fully attending to them.
Although MBSR led to increases in observing, this psychological process was not associated with changes in any of the measured symptoms. The null associations between changes in observing and symptoms may be related to the sample’s lack of training in mindfulness meditation at baseline. In a previous study, greater observing was associated with better psychological well-being in a sample of experienced meditators, but was unrelated to well-being in a meditation-naïve sample (Baer et al. 2008). It is possible that experienced meditators are able to notice a broader range of internal and external experiences with greater curiosity and compassion, leading to choices that promote greater well-being relative to nonmeditators. Furthermore, the effects of observing may be only be found when levels of other mindfulness facets are high. For example, greater observing and acting with awareness may provide more psychological benefits than elevated levels of either facet alone.
Self-compassion also did not predict changes in symptom outcomes. Conversely, in a mindfulness-based intervention trial with breast cancer survivors, self-kindness, a facet of self-compassion, mediated reductions in depressive symptoms (Boyle et al. 2017). Self-compassion has also been found to be associated with lower distress and greater quality of life in cancer patients, whereas few studies have examined its relationship to physical symptoms (Pinto-Gouveia, Duarte, Matos, and Fráguas 2014; Schellekens et al. 2017). In the general literature on mindfulness-based interventions, self-compassion has rarely been tested as a mediator of interventions’ effects on physical symptoms (Gu et al. 2015). Furthermore, although the SCS (and its short form) is the only measure of self-compassion with evidence of reliability and validity, recent studies have failed to replicate its original factor structure and have found inflated correlations between this measure and psychopathology (Brenner, Heath, Vogel, and Credé 2017; Muris 2016).
Although the MBSR intervention produced significant changes in four examined psychological processes, both the MBSR and WC groups showed relatively stable levels of the other three processes: describing, nonreactivity, and psychological inflexibility. These results contrast with previous findings suggesting that mindfulness-based interventions increase various facets of mindfulness and psychological flexibility in cancer and non-cancer samples (Bränström et al. 2010; Duarte and Pinto-Gouveia 2017; Heeren et al. 2015). The lack of change in describing in the current study may have been a function of relatively high scores at baseline, creating a ceiling effect. The measurement of nonreactivity and psychological inflexibility should also be considered. When examining the nonreactivity subscale of the FFMQ, five out of seven items require the endorsement of negative experiences (e.g., “When I have distressing thoughts or images, I am able to just notice them without reacting”). In addition, the items refer to what is “generally true” for the participant without specifying a time frame. Thus, participants were recalling their responses to challenges at varying time frames, which may have rendered the measure insensitive to intervention effects. The AAQ-II measure of psychological inflexibility also does not reference a time frame. Developing measures of psychological inflexibility and mindfulness facets that assess state psychological processes rather than traits is an important direction for future research.
Limitations and Future Research
Limitations of the present study should be considered. First, the sample size for this pilot study was relatively small, which prohibited formal mediation analyses and reduced statistical power for detecting effects and the ability of block randomization to achieve balance between groups on all variables. In addition, multiple comparisons were conducted, which increased the risk of type I error; however, we controlled the family-wise error rate for regression analyses. Sample homogeneity was another limitation, as participants were mostly Caucasian women diagnosed with early-stage breast cancer. Although established self-report measures were used, scholars have argued that “accurate” introspection or self-report is fostered through increased mindfulness practice; thus, behavioral measures or observer reports may be promising assessment alternatives, but are still under development (Davidson and Kaszniak 2015). Finally, residualized change scores for psychological processes rely on the assumption that the final observed data are a linear function of the initial observed data (Cronbach and Furby 1970), and these scores may be less reliable than their constituent parts (Rogosa et al. 1982).
The present pilot study highlights important links between theory-driven psychological processes and decreases in disabling symptoms in cancer populations. Findings also provide a foundation for research using formal mediation analyses to assess relationships between MBSR, psychological processes such as mindfulness, and cancer-related symptoms. Given mixed relations between mindfulness facets and symptoms, future research may explore interactive effects of these facets in predicting symptom improvement. For example, the mindfulness facet of observing may confer benefit only when accompanied by the practice of nonjudging. In addition, studies may include assessment time points during the intervention to gain a better understanding of the temporal patterns of these psychological processes and their relations to symptoms. Given the popularity of mindfulness-based interventions for cancer survivors, examining psychological mechanisms underlying their effects is a critical next step for enhancing their efficacy and cost-effectiveness.
References
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504.
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., et al. (2008). Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment, 15(3), 329–342. https://doi.org/10.1177/1073191107313003.
Berger, A. M., Gerber, L. H., & Mayer, D. K. (2012). Cancer-related fatigue: Implications for breast cancer survivors. Cancer, 118(SUPPL.8), 2261–2269. https://doi.org/10.1002/cncr.27475.
Berger, A. M., Mooney, K., Alvarez-Perez, A., Breitbart, W. S., Carpenter, K. M., Cella, D., et al. (2015). Cancer-related fatigue, version 2.2015. Journal of the National Comprehensive Cancer Network, 13(8), 1012–1039. https://doi.org/10.6004/jnccn.2015.0122.
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., et al. (2011). Preliminary psychometric properties of the acceptance and action questionnaire-II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42(4), 676–688. https://doi.org/10.1016/j.beth.2011.03.007.
Bower, J. E. (2014). Cancer-related fatigue—Mechanisms, risk factors, and treatments. Nature Reviews Clinical Oncology, 11(10), 597–609. https://doi.org/10.1038/nrclinonc.2014.127.
Bower, J. E., Ganz, P. A., Desmond, K. A., Bernaards, C., Rowland, J. H., Meyerowitz, B. E., & Belin, T. R. (2006). Fatigue in long-term breast carcinoma survivors: A longitudinal investigation. Cancer, 106(4), 751–758. https://doi.org/10.1002/cncr.21671.
Boyle, C. C., Stanton, A. L., Ganz, P. A., Crespi, C. M., Bower, J. E., Boyle, C. C., et al. (2017). Improvements in emotion regulation following mindfulness meditation: Effects on depressive symptoms and perceived stress in younger breast cancer survivors. Journal of Consulting and Clinical Psychology, 85(4), 397–402. https://doi.org/10.1037/ccp0000186.
Bränström, R., Kvillemo, P., Brandberg, Y., Moskowitz, J. T., Branstrom, R., Kvillemo, P., et al. (2010). Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients—A randomized study. Annals of Behavioral Medicine, 39(2), 151–161. https://doi.org/10.1007/s12160-010-9168-6.
Brenner, R. E., Heath, P. J., Vogel, D. L., & Credé, M. (2017). Two is more valid than one: Examining the factor structure of the self-compassion scale (SCS). Journal of Counseling Psychology, 64(6), 696–707. https://doi.org/10.1037/cou0000211.
Carmody, J., & Baer, R. A. (2009). How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology, 65(6), 627–638. https://doi.org/10.1002/jclp.20555.
Carney, C. E., Harris, A. L., Falco, A., & Edinger, J. D. (2013). The relation between insomnia symptoms, mood and rumination about insomnia symptoms. Journal of Clinical Sleep Medicine, 9(6), 567–575. https://doi.org/10.5664/jcsm.2752.
Cash, M., & Whittingham, K. (2010). What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness, 1(3), 177–182. https://doi.org/10.1007/s12671-010-0023-4.
Cleeland, C. S., Zhao, F., Chang, V. T., Sloan, J. A., O’Mara, A. M., Gilman, P. B., et al. (2013). The symptom burden of cancer: Evidence for a core set of cancer-related and treatment-related symptoms from the eastern cooperative oncology group symptom outcomes and practice patterns study. Cancer, 119(24), 4333–4340. https://doi.org/10.1002/cncr.28376.
Cronbach, L. J., & Furby, L. (1970). How we should measure “change”: Or should we? Psychological Bulletin, 74(1), 68–80. https://doi.org/10.1037/h0029382.
Davidson, R. J., & Kaszniak, A. W. (2015). Conceptual and methodological issues in research on mindfulness and meditation. American Psychologist, 70(7), 581–592. https://doi.org/10.1037/a0039512.
Dorland, H. F., Abma, F. I., Van Zon, S. K. R., Stewart, R. E., Amick, B. C., Ranchor, A. V., et al. (2018). Fatigue and depressive symptoms improve but remain negatively related to work functioning over 18 months after return to work in cancer patients. Journal of Cancer Survivorship, 12(3), 371–378. https://doi.org/10.1007/s11764-018-0676-x.
Duarte, J., & Pinto-Gouveia, J. (2017). Mindfulness, self-compassion and psychological inflexibility mediate the effects of a mindfulness-based intervention in a sample of oncology nurses. Journal of Contextual Behavioral Science, 6(2), 125–133. https://doi.org/10.1016/j.jcbs.2017.03.002.
Feros, D. L., Lane, L., Ciarrochi, J., & Blackledge, J. T. (2013). Acceptance and commitment therapy (ACT) for improving the lives of cancer patients: A preliminary study. Psycho-Oncology, 22(2), 459–464. https://doi.org/10.1002/pon.2083.
Garland, S. N., Tamagawa, R., Todd, S. C., Speca, M., & Carlson, L. E. (2013). Increased mindfulness is related to improved stress and mood following participation in a mindfulness-based stress reduction program in individuals with cancer. Integrative Cancer Therapies, 12(1), 31–40. https://doi.org/10.1177/1534735412442370.
Gonzalez, P., Castañeda, S. F., Dale, J., Medeiros, E. A., Buelna, C., Nuñez, A., et al. (2014). Spiritual well-being and depressive symptoms among cancer survivors. Supportive Care in Cancer, 22(9), 2393–2400. https://doi.org/10.1007/s00520-014-2207-2.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37(Apr), 1–12. https://doi.org/10.1016/j.cpr.2015.01.006.
Hall, D. L., Luberto, C. M., Philpotts, L. L., Song, R., Park, E. R., & Yeh, G. Y. (2018). Mind-body interventions for fear of cancer recurrence: A systematic review and meta-analysis. Psycho-Oncology, 27(11), 2546–2558. https://doi.org/10.1002/pon.4757.
Haller, H., Winkler, M. M. M., Klose, P., Dobos, G., Kümmel, S., Cramer, H., et al. (2017). Mindfulness-based interventions for women with breast cancer: An updated systematic review and meta-analysis. Acta Oncologica, 56(12), 1665–1676. https://doi.org/10.1080/0284186X.2017.1342862.
Hann, D. M., Denniston, M. M., & Baker, F. (2000). Measurement of fatigue in cancer patients: Further validation of the fatigue symptom inventory. Quality of Life Research, 9(7), 847–854. https://doi.org/10.1023/A:1008900413113.
Hann, D. M., Jacobsen, P. B., Azzarello, L. M., Martin, S. C., Curran, S. L., Fields, K. K., et al. (1998). Measurement of fatigue in cancer patients: Development and validation of the fatigue symptom inventory. Quality of Life Research, 7(4), 301–310. https://doi.org/10.1023/A:1024929829627.
Hayes, S. C., Levin, M. E., Plumb-Vilardaga, J., Villatte, J. L., & Pistorello, J. (2013). Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behavior Therapy, 44(2), 180–198. https://doi.org/10.1016/j.beth.2009.08.002.
Hayes, S. C., Wilson, K. G., Gifford, E. V., Follette, V. M., & Strosahl, K. (1996). Experimental avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152–1168. https://doi.org/10.1037/0022-006X.64.6.1152.
Heeren, A., Deplus, S., Peschard, V., Nef, F., Kotsou, I., Dierickx, C., et al. (2015). Does change in self-reported mindfulness mediate the clinical benefits of mindfulness training? A controlled study using the French translation of the five facet mindfulness questionnaire. Mindfulness, 6(3), 553–559. https://doi.org/10.1007/s12671-014-0287-1.
Henry, D. H., Viswanathan, H. N., Elkin, E. P., Traina, S., Wade, S., & Cella, D. (2008). Symptoms and treatment burden associated with cancer treatment: Results from a cross-sectional national survey in the U.S. Supportive Care in Cancer, 16(7), 791–801. https://doi.org/10.1007/s00520-007-0380-2.
Jemal, A., Ward, E. M., Johnson, C. J., Cronin, K. A., Ma, J., Ryerson, A. B., et al. (2017). Annual report to the nation on the status of cancer, 1975–2014, featuring survival. Journal of the National Cancer Institute, 109(9), 1–22. https://doi.org/10.1093/jnci/djx030.
Johns, S. A., Brown, L. F., Beck-Coon, K., Monahan, P. O., Tong, Y., & Kroenke, K. (2015). Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psycho-Oncology, 24(8), 885–893. https://doi.org/10.1002/pon.3648.
Jones, J. M., Olson, K., Catton, P., Catton, C. N., Fleshner, N. E., Krzyzanowska, M. K., et al. (2016). Cancer-related fatigue and associated disability in post-treatment cancer survivors. Journal of Cancer Survivorship, 10(1), 51–61. https://doi.org/10.1007/s11764-015-0450-2.
Kabat-Zinn, J. (1994). Wherever you go, there you are: Mindfulness meditation in everyday life. New York, NY: Hyperion.
Kazdin, A. E. (2007). Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3(1), 1–27. https://doi.org/10.1146/annurev.clinpsy.3.022806.091432.
Kroenke, K., Spitzer, R. L., Williams, J. B. W., Monahan, P. O., & Lowe, B. (2007). Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine, 146(5), 317–325. https://doi.org/10.7326/0003-4819-146-5-200703060-00004.
Kroenke, K., Strine, T. W., Spitzer, R. L., Williams, J. B. W., Berry, J. T., & Mokdad, A. H. (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. doi:https://doi.org/10.1016/j.jad.2008.06.026.
Kroenke, K., Zhong, X., Theobald, D., Wu, J., Tu, W., & Carpenter, J. S. (2010). Somatic symptoms in patients with cancer experiencing pain or depression. Archives of Internal Medicine, 170(18), 1686–1694. https://doi.org/10.1001/archinternmed.2010.337.
Kuyken, W., Watkins, E., Holden, E., White, K., Taylor, R. S., Byford, S., et al. (2010). How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy, 48(11), 1105–1112. https://doi.org/10.1016/j.brat.2010.08.003.
Labelle, L. E., Campbell, T. S., Faris, P., & Carlson, L. E. (2015). Mediators of mindfulness-based stress reduction (MBSR): Assessing the timing and sequence of change in cancer patients. Journal of Clinical Psychology, 71(1), 21–40. https://doi.org/10.1002/jclp.22117.
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. Y. (2008). Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. https://doi.org/10.1097/MLR.0b013e318160d093.
MacKinnon, D. P. (2008). Introduction to statistical mediation analysis. Mahwah, NJ: Erlbaum.
Minton, O., Richardson, A., Sharpe, M., Hotopf, M., & Stone, P. C. (2011). Psychostimulants for the management of cancer-related fatigue: A systematic review and meta-analysis. Journal of Pain and Symptom Management, 41(4), 761–767. https://doi.org/10.1016/j.jpainsymman.2010.06.020.
Morin, C. M. (1993). Insomnia: Psychological assessment and management. New York: Guilford Press.
Muris, P. (2016). A protective factor against mental health problems in youths? A critical note on the assessment of self-compassion. Journal of Child and Family Studies, 25(5), 1461–1465. https://doi.org/10.1007/s10826-015-0315-3.
Mustian, K. M., Alfano, C. M., Heckler, C., Kleckner, A. S., Kleckner, I. R., Leach, C. R., et al. (2017). Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: A meta-analysis. JAMA Oncology, 3(7), 961–968. https://doi.org/10.1001/jamaoncol.2016.6914.
Nakamura, Y., Lipschitz, D. L., Kuhn, R., Kinney, A. Y., & Donaldson, G. W. (2013). Investigating efficacy of two brief mind-body intervention programs for managing sleep disturbance in cancer survivors: A pilot randomized controlled trial. Journal of Cancer Survivorship, 7(2), 165–182. https://doi.org/10.1007/s11764-012-0252-8.
Neff, K. (2003a). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity, 2(3), 85–101. https://doi.org/10.1080/15298860390129863.
Neff, K. (2003b). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250. https://doi.org/10.1080/15298860390209035.
Noordman, B. J., Verdam, M. G. E., Lagarde, S. M., Shapiro, J., Hulshof, M. C. C. M., van Berge Henegouwen, M. I., . . . CROSS Study Group. (2018). Impact of neoadjuvant chemoradiotherapy on health-related quality of life in long-term survivors of esophageal or junctional cancer: Results from the randomized CROSS trial. Annals of Oncology, 29(2), 445–451. https://doi.org/10.1093/annonc/mdx726.
Pinto-Gouveia, J. J., Duarte, C., Matos, M., & Fráguas, S. (2014). The protective role of self-compassion in relation to psychopathology symptoms and quality of life in chronic and in cancer patients. Clinical Psychology and Psychotherapy, 21(4), 311–323. https://doi.org/10.1002/cpp.1838.
Przezdziecki, A., Sherman, K. A., Baillie, A., Taylor, A., Foley, E., & Stalgis-Bilinski, K. (2013). My changed body: Breast cancer, body image, distress and self-compassion. Psycho-Oncology, 22(8), 1872–1879. https://doi.org/10.1002/pon.3230.
Querstret, D., Cropley, M., & Fife-Schaw, C. (2017). Internet-based instructor-led mindfulness for work-related rumination, fatigue, and sleep: Assessing facets of mindfulness as mechanisms of change. A randomized waitlist control trial. Journal of Occupational Health Psychology, 22(2), 153–169. https://doi.org/10.1037/ocp0000028.
Raes, F., Pommier, E., Neff, K., & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self-compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. https://doi.org/10.1002/cpp.702.
Rogosa, D., Brandt, D., & Zimowski, M. (1982). A growth curve approach to the measurement of change. Quantitative Methods in Psychology, 92(3), 726–748. https://doi.org/10.1037/0033-2909.92.3.726.
Savard, M. H., Savard, J., Simard, S., & Ivers, H. (2005). Empirical validation of the insomnia severity index in cancer patients. Psycho-Oncology, 14(6), 429–441. https://doi.org/10.1002/pon.860.
Schellekens, M. P. J., van den Hurk, D. G. M., Prins, J. B., Donders, A. R. T., Molema, J., Dekhuijzen, R., . . . Speckens, A. E. M. (2017). Mindfulness-based stress reduction added to care as usual for lung cancer patients and/or their partners: A multicentre randomized controlled trial. Psycho-Oncology, 26(12), 2118–2126. https://doi.org/10.1002/pon.4430.
Sherman, K. A., Woon, S., French, J., & Elder, E. (2017). Body image and psychological distress in nipple-sparing mastectomy: The roles of self-compassion and appearance investment. Psycho-Oncology, 26(3), 337–345. https://doi.org/10.1002/pon.4138.
Wang, X. S., Zhao, F., Fisch, M. J., O’Mara, A. M., Cella, D., Mendoza, T. R., & Cleeland, C. S. (2014). Prevalence and characteristics of moderate to severe fatigue: A multicenter study in cancer patients and survivors. Cancer, 120(3), 425–432. https://doi.org/10.1002/cncr.28434.
Zhang, Q., Zhao, H., & Zheng, Y. (2019). Effectiveness of mindfulness-based stress reduction (MBSR) on symptom variables and health-related quality of life in breast cancer patients—A systematic review and meta-analysis. Supportive Care in Cancer, 27(3), 771–781. https://doi.org/10.1007/s00520-018-4570-x.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
Research reported in this publication was supported by grants from the Walther Cancer Foundation, Inc. and the National Cancer Institute (R25CA117865-01A11). This work was also supported by National Cancer Institute grant K05CA175048 (CEM and SAJ).
Author information
Authors and Affiliations
Contributions
KC designed and executed the study, completed data analyses, and wrote the paper. CEM assisted with the study design, study execution, and the writing of this paper. LFB and KAB delivered the intervention and assisted in the writing of this paper. KK assisted in the writing of this paper. SAJ designed the original trial that generated data analyzed in this paper and assisted in the writing of this paper. All authors approved the final version of the manuscript for submission.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Indiana University Institutional Review Board and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Walther Cancer Foundation or the National Institutes of Health. Research reported in this paper is based on a master’s thesis completed by KC.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chinh, K., Mosher, C.E., Brown, L.F. et al. Psychological Processes and Symptom Outcomes in Mindfulness-Based Stress Reduction for Cancer Survivors: A Pilot Study. Mindfulness 11, 905–916 (2020). https://doi.org/10.1007/s12671-019-01299-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-019-01299-0