Abstract
MBSR(BC) is known to have a positive impact on psychological and physical symptoms among breast cancer survivors (BCS). The cognitive mechanisms of “how” MBSR(BC) works was addressed in a recent study that found that there was strong consistent evidence that reduced emotional reactivity is a mediator and moderate consistent evidence that mindfulness, rumination, and worry were mediators. The purpose of this study, as part of a larger R01 trial, was to test whether positive effects achieved from the MBSR(BC) program were mediated through changes in increased mindfulness, decreased fear of breast cancer recurrence, and perceived stress. Female BCS > 21 years diagnosed with Stage 0-III breast cancer were randomly assigned to a 6-week MBSR(BC) or a Usual Care (UC)regimen. Potential mediators of 6- and 12-week outcomes were identified by analysis of covariance (ANCOVA), followed by formal mediational analyses of main effects of MBSR(BC) on 6- and 12-week outcomes, including percentage of total effects explained. Among 322 BCS (167 MBSR(BC) and 155 UC), fear of recurrence and perceived stress, but not mindfulness, mediated reductions in anxiety and fatigue at weeks 6 and 12, partially supporting our hypothesis of cognitive mechanisms of MBSR(BC).
Trial Registration
Registration Number: NCT01177124 http://www.ClinicalTrials.gov
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most prevalent cancer among women, with 3.8 million cases reported in the United States for 2019 (DeSantis et al., 2019). Although 90% of breast cancer survivors (BCS) are surviving at least five years (American Cancer Society, 2020) after diagnosis due to new advanced treatments, they are often unprepared for the associated emotional trauma and multiple psychological and physical symptoms impacting their quality of life (QOL)(American Cancer Society, 2019; DeSantis et al., 2019; Lengacher et al., 2014). Evidence shows Mindfulness-based stress reduction (MBSR) programs offer a safe non-pharmacological approach for BCS providing multiple health benefits to reduce cancer symptom burden while also increasing their QOL (Lengacher et al., 2016). Specific evidence shows mindfulness-based programs are associated with improvements in psychological health, (stress, anxiety and depression) (Lengacher et al., 2012), and physical symptoms, (pain, fatigue and sleep) (Carlson et al., 2013; Garland et al., 2014; Johns et al., 2015; Lengacher et al., 2015, 2016), yet there is limited research examining the “mechanism of action” of mindfulness training to provide insight into the process by which this training impacts patient outcomes. Research utilizing mediation analyses may advance the scientific basis of how behavioral interventions work (Alan E Kazdin, 2006; Moyer et al., 2012), by also validating effective components on individualized patient benefits (Laurenceau et al., 2007).
The “healing power” of mindfulness is postulated to occur through two cognitive processes: awareness and attention (Brown & Cordon, 2009). Training in meditation is proposed to increase self-regulation of emotions and thoughts (Bishop, 2002), through use of moment-to-moment, non-judgmental/non-reactive awareness to internal and external experiences, resulting in reduced rumination and elaboration over past or future distressing experiences (Baer, 2003; Bishop et al., 2004; Brown et al., 2007; Kabat-Zinn, 1990, 2003). The mechanisms by which MBSR(BC) improves health outcomes/well-being remain largely unknown and mechanisms have not been validated (Moyer et al., 2012). Primary targets of mechanisms have been mindfulness, in addition to emotion regulation and cognitive control in the form of altering one’s perspective as a function of mindfulness practice.
For BCS, evidence shows MBSR significantly reduces perceived stress, anxiety and fatigue (Lengacher et al., 2016; Reich et al., 2017; Zainal et al., 2013). Mindfulness has been examined not just as an outcome measure, but as a mediator, and therefore a potential mechanism of MBSR among cancer survivors. A meta-analysis of mediators of 20 mindfulness-based interventions among all types of patients (Gu et al., 2015) examining the cognitive mechanisms of “how” MBSR(BC) works identified strong consistent evidence supporting reduced emotional reactivity as a mediator and moderate consistent evidence supporting mindfulness, rumination, and worry as mediators (Gu et al., 2015). Only 4 studies in this review included cancer survivors, one of which was Dr. Lengacher’ s (2014) mediation study, among 82 BCS receiving MBSR(BC) versus UC showing a reduction in fear of recurrence and improvement in physical functioning mediated improvements in perceived stress and anxiety. When examining mindfulness as a mediator of stress, improvements in perceived stress were found among survivors with a past diagnosis of cancer (Branstrom et al., 2010) and specifically among BCS (Boyle et al., 2017). While previous research investigated perceived stress as an outcome, there continues to be limited evidence investigating “stress” as a mechanism that modifies health outcomes. In a recent study among gastrointestinal cancer patients, perceived stress was found to mediate the relationship between dispositional mindfulness and psychological symptoms (anxiety, depression, social dysfunction, and loss of confidence) (Xu et al., 2017).
Fear of Cancer recurrence. In addition to mindfulness and perceived stress, fear of recurrence has been debated as a mechanism by which the MBSR intervention exerts positive outcomes on psychological and physical health among cancer survivors. The primary mechanism described in the R01 grant was biobehavioral therefore conceptually we postulated that the principal mechanism by which MBSR(BC) is effective was through increased mindfulness (e.g., awareness) and reduced fear of recurrence. We also postulate that to achieve maximum benefit from the MBSR(BC) program, practice and proficiency in mindfulness is a critically important element. By increasing mindfulness and reducing fear of recurrence, MBSR(BC) may modulate hypothalamic pituitary adrenal (HPA) axis and sympathetic (SNS) and parasympathetic nervous system (PNS) responses resulting in reduced physical, psychological, and biological markers of stress and increased quality of life and cellular immune function.
Although it is less clear about FOR as a mediator, our previous R21 and first mediator study did support FOR as a mediator among 82 breast cancer survivors who received MBSR(BC) versus UC (Lengacher et al., 2014). Results showed that a reduction in fear of recurrence and improvement in physical functioning mediated improvements in perceived stress and anxiety.
Often for breast cancer survivors, worry, rumination and uncertainty underlie the symptom expression of fear of cancer recurrence (Lee-Jones et al., 1997). Evidence is lacking in that fear of recurrence may also function as a mediator of reduced physical symptoms, such as fatigue, a common symptom reported by BCS transitioning off treatment.
Our first mediation study, among 82 breast cancer survivors who received MBSR(BC) versus UC (Lengacher et al., 2014), showed that a reduction in fear of recurrence and improvement in physical functioning mediated improvements in perceived stress and anxiety. These findings suggest that MBSR(BC) may impart “self-regulated” changes in cognitive and affective appraisals of one’s experiences and perspectives. Improved mindfulness and enhanced emotion regulation through MBSR have resulted in reduced mood disturbances (Laura E Labelle et al., 2015). In this study, we hypothesize cognitive mechanisms are mediators of the MBSR(BC) intervention for improving psychological health, through the processes of self-regulation of emotions to internal and external experiences. Our first mediation study (Lengacher et al., 2014), was limited to investigating fear of recurrence as a potential cognitive mechanism through which symptom improvements may have occurred. This current R01 investigated “mindfulness” and “perceived stress” as additional mediators of the MBSR(BC) intervention among BCS.
The aim of this study, as part of a larger R01 trial, was to “test whether positive effects from the MBSR(BC) program were mediated through changes in mindfulness and fear of recurrence of breast cancer. We hypothesized BCS in the MBSR(BC) program will report greater increases in mindfulness and larger reductions in fear of recurrence compared to BCS assigned to the UC regimen.
Methods
Sample and Setting
Female breast cancer survivors (BCS; n = 322) aged 21 and older were recruited from Moffitt Cancer Center, and the Carol and Frank Morsani Center for Advanced Healthcare between April 2009 through March 2014. BCS were included with a diagnosis of Stage 0-III breast cancer, lumpectomy and/or mastectomy and/or adjuvant radiation and/or chemotherapy. BCS with a diagnosis of Stage IV cancer, a severe mental disorder, and/or breast cancer recurrence were excluded. Recruitment commenced after patient completion of breast cancer surgery and near completion of treatment, up to 2 years off treatment. The Principal Investigator is a member of the Moffitt Breast Cancer and the Health Outcomes and Behavioral Program and has working relationships with physicians and nurses at Moffitt. Health practitioners assisted and were trained in screening for interest in enrollment and identified eligible patients during routine patient care. Flyers and brochures describing the study was distributed to patients via advertisements within the cancer center.
Study design and randomization
BCS were randomly assigned in a 1:1 ratio to either: (i) the formal (in-class) 6-week MBSR(BC) program tailored to BCS; or the (ii) usual care (UC) waitlisted regimen in which MBSR(BC) was offered within 6 months after study enrollment. Participants were stratified by type of surgery (lumpectomy versus mastectomy), breast cancer treatment (chemotherapy with or without radiation versus radiation alone), and stage of breast cancer (Stage 0/I versus II/III). This, along with the blocking mechanism, was done to enhance the likelihood of balanced distributions of baseline factors between the 2 study groups (e.g., pre-existing levels of anxiety, immune status, etc.). Participants assigned to MBSR(BC) were enrolled in a minimum of 5 to 6 participants, which is adequate for this type of research (per consultation Saki Santorelli). Baseline assessments will be done prior to randomization, hence all data collected at this time will be blinded to future assignment. Lab technicians were be blinded at each data point and scoring also was conducted blinded.
Procedures
The Institutional Review Board at the University of South Florida approved all procedures. BCS who met study inclusion criteria and expressed interest in the study were invited to an orientation session. At the orientation session, informed consent was obtained, blood sample, and baseline data were collected on measures of psychological, biological, and physical symptom status, QOL, demographic characteristics, and clinical history followed by randomization to either the MBSR(BC) program or the UC waitlisted group. BCS completed assessments at 6 weeks upon program completion and at 12 weeks, six weeks after program completion.
MBSR(BC) intervention procedures
BCS randomized to the MBSR(BC) intervention attended 6 weekly (2-h) sessions conducted by a trained psychologist in MBSR(BC). BCS received a training manual and 5 audio CD’s to guide their home practice of sitting meditation, body scan, gentle yoga, and walking meditation and recorded practice time in a diary during the 12 weeks of the study. The MBSR(BC) program is a 6-week program adapted by Dr. Lengacher for BCS from Jon Kabat-Zinn’s 8-week program (Kabat-Zinn et al., 1985, 1992). The intervention consists of (1) educational materials; (2) practice sessions of 4 formal and informal meditative techniques; and (3) group processes related to barriers to the practice, application in daily situations, and supportive group interaction. Participants receive meditative training (Kabat-Zinn et al., 1992) in 4 formal meditation techniques: (1) sitting meditation; (2) body scan meditation; (3) Gentle Hatha Yoga; and (4) walking meditation. BCS are taught to bring awareness to thoughts and emotions associated with symptoms such as pain, anxiety, sleep disturbances, and fear of recurrence and to then separate the emotional experience from the sensory experience. Through MBSR(BC), BCS learn to mitigate fears attached to physical and emotional distress by promoting self-regulation of attention through meditative practices. Informal techniques of mindfulness are learned by integrating attention and awareness into their daily activities (Hamilton et al., 2006). An example of self-regulation is the process of not getting caught up, or ruminating over something unpleasant, such as pain or anxiety, but focusing attention on the breath and the current activity. As one is immersed in the task, calmness occurs; this is called “present moment awareness,” a central concept of MBSR (Hamilton et al., 2006).
Usual Care Regimen
The Usual Care regimen consisted of standard post-treatment clinic visits and was not modified by study participation. UC participants were asked to not use or practice meditation or yoga techniques or participate in MBSR during the study. The UC group attended standard post-treatment clinic visits and were wait-listed to receive the MBSR(BC) program within 6 months after enrolling in the study.
Measures
Dependent variables
Physical symptoms
Physical symptoms included the following measurements. Pain. The Brief Pain Inventory (BPI) measures pain, including intensity and interference, and has reliability coefficients ranging from 0.82 to 0.95 (Keller et al., 2004). Fatigue. The Fatigue Symptom Inventory (FSI) is a 14-item self-report questionnaire that measures fatigue severity, frequency, daily pattern, and perceived interference with QOL (Hann et al., 1998). The FSI has a reliability alpha coefficient of 0.90, and a test–retest reliability ranging from r = 0.35-0.75 (Keller et al., 2004). Sleep. The Pittsburgh Sleep Quality Index (PSQI) is a 19 self-report sleep questionnaire with 5 questions rated by the bed partner to rate sleep quality of patients. Reliability is 0.80 for the global PSQI and ranges from 0.70 to 0.78 for sleep disturbance (Carpenter & Andrykowski, 1998).
Psychological symptoms
Psychological symptoms included the following measurements. Depression. The Center for Epidemiological Studies Depression Scale (CES-D), a four-point scale evaluated depression and has a reliability coefficient of 0.92 for breast cancer subjects (Radloff, 1977). State anxiety The State Trait Anxiety Inventory measured anxiety; internal consistency reliability is reported as 0.95 (Spielberger et al., 1983).
Quality of life (QOL)
The Medical Outcomes Study Short Form was used to assess mental and physical health as related to QOL; higher scores are demonstrative of better mental and physical health. Health-related quality of life was measured by the Medical Outcomes Studies Short-form (MOS SF-36), a 36-item questionnaire with Likert-type responses. Internal consistency reliability ranged from 0.62 to 0.94 (Ware et al., 1994). Test–retest reliability ranged from 0.43 to 0.90 (Ware et al., 1994).
Predictor variables
Perceived stress
The Perceived Stress Scale (PSS) measured participant stress; it is a 14-item Likert-type scale with an internal consistency reliability ranging from 0.84 to 0.86 (Cohen et al., 1983).
Fear of cancer recurrence
The Concerns about Recurrence Scale measured fear of recurrence (cancer) and includes the extent and nature of women’s fears about the possibility of breast cancer recurrence in two subscales: (1) overall FCR and (2) problem specific. The overall FCR is a 4 item, 1-to 6 scale (assesses overall fear of recurrence, scored as (1) ‘‘I don’t think about it at all’’ to (6) ‘‘I think about it all the time.” The second part includes 26 items assessing the nature of the fear of recurrence and extent to which they worry about each item, scored on a 5-point Likert scale ranging from (0) not at all, to (4) extremely. Overall, internal consistency reliability is 0.87 for BCS (Vickberg, 2003). Mindfulness was measured by 2 instruments. The Five Facet Mindfulness Questionnaire (FFMQ) (Baer et al., 2006), a 39-item instrument on a 1–5 Likert Scale evaluated five factors of mindfulness, observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience. Internal consistency ranges from 0.72 to 0.92 (Baer et al., 2008). The Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) (Feldman, 2007), is a 12-item 1–4 Likert-scale measuring 4 subscales of mindfulness (attention, present-focus, awareness, acceptance/non-judgment); internal consistency ranges from 0.74 to 0.77.
Demographic data/clinical history
Standard socio-economic demographic data were collected on age, gender, ethnicity, education completed, marital status, income status, and employment status at baseline and updated at 6 and 12 weeks. Standard clinical history data were collected at baseline, 6 and 12 weeks and included type of treatment, cancer diagnosis, and dates on treatment. As part of the clinical history form, data included a social history, lifestyle health behaviors, and medication use.
Statistical methods
Baseline demographic/clinical characteristics of outcomes and potential mediators were summarized as means and standard deviations for continuous variables and percentages for categorical variables. Patient characteristics were compared by random assignment by use of student t tests for continuous variables and chi-square tests for categorical variables. To evaluate whether positive effects achieved from the MBSR(BC) program were mediated through changes in mindfulness, perceived stress, and fear of recurrence of breast cancer: analysis of covariance (ANCOVA) was initially used to examine the relationships between the MBSR(BC) intervention and potential mediators and outcomes at both 6- and 12-weeks. The ANCOVA models included adjustment for baseline value of the mediator or outcome evaluated. Based on this analysis, outcome variables and potential mediating variables showing the strongest main effects associated with MBSR(BC) were selected for the mediational analyses. The meditational analyses were conducted using the SAS PROCESS macro and methods described by Preacher and Hayes (2004) and Imai et al. (2010) with p-values determined by use of bias corrected bootstrap confidence intervals. The percent of total effects explained by the mediator, were calculated as described by Hicks and Tingley (2011). With this method, estimates of total effects of MBSR(BC) on the primary outcomes of interest, and indirect effects attributed to a potential mediator, were estimated, and plotted. These analyses included change in mediators and outcomes at 6-weeks, as well as change in mediators at 6-week in relation to change in outcomes at 12-weeks (i.e., temporal relationship between initial change in mediator influencing longer-term outcome). The sequential assumption common in mediation analysis (Imai et al., 2010) was not tested because treatment was randomized. The SAS System, version 9.4 (Cary, NC) was used for analyses, with a 2-sided p-value of 0.05 used to define statistical significance.
Results
Participant characteristics
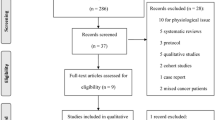
For recruitment, 1,647 participants were approached with 322 (167 MBSR(BC) and 155 UC) participants enrolled. Among the 322 BCS enrolled, 299 completed with 23 or 7% not completing the study. The mean age was 56 years and specially, 69.4% of the BCS were white, non-Hispanic, 11.6% Black non-Hispanic, 10.3% Hispanic, and 8.7% other. No statistically significant differences between groups were found at baseline demographic characteristics however a difference in clinical characteristics was found in use of anxiety medications for the MBSR(BC) group (Lengacher et al., 2016) for the CONSORT chart reporting number of participants screened, randomized, and retained, as well as demographic and clinical characteristics by random assignment. Results of the calculated baseline values of the primary outcome and potential mediators of interest by random assignment are presented in Table 1. In addition, the Cronbach Alpha internal consistency ranges are reported for the original measurements and updated for our current sample. In contrast to baseline demographic and clinical characteristics, several of the primary outcome and potential mediating variables were not fully balanced by random assignment. This included the MBSR(BC) intervention group compared to the UC group as having significantly higher state anxiety, fatigue, fear of recurrence overall, and fear of recurrence problems, and perceived stress at baseline, and lower QOL (emotional well-being). Mean scores for the two measures of mindfulness were similar by random assignment.
Early intervention effects
Mean change scores from baseline to 6-weeks and baseline to 12 weeks by random assignment are presented in Table 2 for a range of outcome variables and potential mediating variables, and adjustment for the baseline value of the variable of interest. From baseline to 6-weeks, the MBSR(BC) program was associated with greater reductions in state anxiety (p = 0.01) and fatigue (p = 0.006), as well as higher levels of emotional well-being (p = 0.04). Early Mediation effects at 6 weeks: For potential mediating variables, the ANCOVA revealed the MBSR(BC) program was associated with greater reduction in overall fear of recurrence (p = 0.03), problems stemming from fear of recurrence (p = 0.0003), and a trend towards lower perceived stress (p = 0.10) at 6 weeks. Mindfulness was not associated with MBSR(BC) at 6 weeks (p = 0.49 for CAMS-R scores; p = 0.27 for FFMQ scores). Of note, all but one baseline to 6-week outcome measure was in the expected direction of improved symptom status with MBSR(BC).
Late Intervention Effects
From baseline to 12-weeks, the MBSR(BC) program was associated with greater reductions in fatigue (p = 0.03), as well as trending reductions in state anxiety (p = 0.06) and QOL (p = 0.09). Later Mediation Effects. For potential mediating variables, the MBSR(BC) program was associated with greater reduction in fear of recurrence problems (p = 0.008) at 12 weeks and a trend towards lower perceived stress (p = 0.11). Mindfulness was trending for the FFMQ scores (p = 0.08) but was not significantly different for the CAMS-R scores (p = 0.32). Based on these results, state anxiety and fatigue were selected as primary outcome variables, and fear of recurrence (problems) and perceived stress were selected as potential mediating variables for mediational analyses. Although perceived stress was only trending for both early and late effects, mediation effects were nevertheless constant throughout the entire study period and perceived stress was therefore included for further mediation analyses.
Fear of recurrence as mediator
As seen in Fig. 1 (top half), a significant portion of the relationship between MBSR(BC) and state anxiety at both 6 (p = 0.03) and 12-weeks (p = 0.008) was mediated through reductions in fear of cancer recurrence that occurred at 6 weeks. At both time points, the 6-week reduction in fear of cancer recurrence associated with the MBSR(BC) program explained 37% of the total effects of MBSR(BC) on levels of state anxiety. Similarly, reductions in fear of recurrence associated with the MBSR(BC) program mediated reductions in fatigue at 12-weeks (p = 0.003), but not 6-weeks (p = 0.17) (Fig. 1, bottom half).
Perceived stress as mediator
Results were relatively similar when changes in perceived stress associated with the MBSR(BC) program (rather than changes in fear of recurrence) were examined in relation to levels of anxiety and fatigue at 6 and 12-weeks in a mediation analysis. Specifically, reduction in perceived stress at 6-weeks mediated the relationship between MBSR(BC) and state anxiety at 6 and 12-weeks (p = 0.003 and p = 0.02, respectively) (Fig. 2, top half). Of note, the reduction in perceived stress associated with the MBSR(BC) program explained 67% of the total effects of MBSR(BC) on lower levels of state anxiety at 6-weeks. Changes (reductions) in perceived stress associated with MBSR(BC) also mediated reductions in fatigue at 6 and 12-weeks (p = 0.009 and p = 0.04, respectively) (Fig. 2, bottom half). Thus, there was substantial overlap between MBSR(BC)-induced changes in fear of recurrence and changes in perceived stress mediating the relationships between MBSR(BC) and both state anxiety and fatigue at 6- and 12-weeks. Changes in mindfulness (CAMS-R) as a potential mediator were not associated with MBSR and its effects on anxiety or fatigue at either 6 or 12 weeks (p > 0.90 for all 4 models).
Subgroup analyses
At baseline, state anxiety was strongly correlated with fatigue (r = 0.53, p < 0.0001), and MBSR(BC) participants presented with higher baseline state anxiety values than UC participants (Table 1). Thus, subgroup analyses were conducted to examine the total effects of MBSR(BC) and mediating effects of fear of recurrence and perceived stress on 6- and 12-week outcome scores (anxiety and fatigue) among trial participants with baseline levels of anxiety and fatigue that were above the median (n = 111).
As seen in Table 3, a “large” total effect was observed for MBSR(BC) in relation to lower levels of fatigue at 6-weeks (effect size = 0.70, p = 0.0002) among participants who presented with high levels of anxiety and fatigue at study entry. “Medium” effect sizes were generally observed with respect to MBSR(BC) and lower levels of anxiety, fear of recurrence, and perceived stress at both 6 and 12-weeks. Only fear of recurrence was selected as a mediator in the subgroup analysis due to strong effects in the overall sample. In mediational analyses, there was an indication of reductions in fear of recurrence mediating the relationship between MBSR(BC) and state anxiety at 6 and 12-weeks (p = 0.09 and p = 0.01) among trial participants with high anxiety and fatigue at baseline (Fig. 3, top half). However, there was little to no evidence of change in fear of recurrence mediating the relationship between MBSR(BC) and fatigue at 6 and 12-weeks among trial participants with high anxiety and fatigue at baseline (Fig. 3, bottom half). Thus, we did not find evidence that fear of recurrence was a stronger mediator of the relationships between MBSR(BC) and state anxiety and fatigue at 6 and 12-weeks among the subset of participants who presented with high levels of anxiety and fatigue at study entry.
Plots of total and indirect effects of fear of recurrence as a potential mediator of state anxiety at 6 weeks (a) and 12 weeks (b), and fear of recurrence as a potential mediator of fatigue at 6 weeks (c) and 12 weeks (d). The analysis is restricted to participants who presented with levels of anxiety and fatigue above the median at study entry
In summary the results of this current study examining BCS (n = 322) in transition post-treatment suggest that the observed reductions in state anxiety and fatigue in the MBSR(BC) group are mediated by reductions in fear of recurrence and perceived stress.
Discussion
As part of a larger R01 clinical trial, results from these mediation analyses provide new knowledge and evidence identifying potential mechanisms of action for the MBSR(BC) intervention among breast cancer survivors (BCS) who are in transition off treatment. After initial analyses of early intervention effects of MBSR(BC) (baseline to 6 weeks), results pointed to fear of recurrence overall and fear of recurrence problems, and to a lesser extent perceived stress, as potential mediators of MBSR(BC) effects on state anxiety and fatigue. Mindfulness was not identified as a mediator of outcomes at 6 weeks. Late intervention effects from baseline to 12 weeks were observed with 6-week changes in fear of recurrence and trends toward perceived stress and mindfulness as potential mediators. These findings indicate that some mechanisms of action for MBSR(BC) may occur through the internal, cognitive perspectives of one’s affect (fear of recurrence/future uncertainties, self-perception of stress) to successfully reduce anxiety and fatigue. This evidence contributes to the scientific knowledge of MBSR by identifying specific cognitive mechanisms of action through which the MBSR(BC) program may positively influence health outcomes among BCS.
Mindfulness as a mediator. Multiple studies have proven the effects of mindfulness on tested outcomes and has proven effects as postulated over several years. In this study our team further postulated the additional premise to test mindfulness as a mediator or explaining the “through and by” which mindfulness is an identified mediator explaining how the mechanism works (Brown et. al., 2007). Although limited evidence exists examining the mechanism, or “mediators of effects” of a mindfulness intervention, our team further supports the need to identify significant specific and non-specific effects of mediators to maximize intervention treatment benefits of the “active components” (Gu et. al., 2015).
Hall and colleagues (2018) addressed the current discussion on what mechanisms of MBSR may improve health outcomes, with mindfulness possibly not playing a central role in the mechanism pathway of fear and stress to improve anxiety and fatigue. In this current study, mindfulness effects increased between 6 and 12 weeks, but never reached statistical significance, suggesting that cognitive changes specific to mindfulness may be a gradual process. Longer mindfulness meditation practice has been associated with improved optimism (Lengacher et al., 2009), improved psychological well-being (Baer et al., 2008; Josefsson et al., 2011), and reduced post-traumatic stress symptoms of avoidance (Bränström et al., 2012). These findings suggest that the effectiveness of the MBSR(BC) intervention may require a long-term commitment to practice attaining self-regulation of reactions to stress for psychological health improvements. Furthermore, in a waitlist control study of women with cancer, mindfulness did not mediate the effect of the MBSR intervention on depression (Labelle et al., 2010). Mindfulness therefore may not be the core mechanism determining MSBR’s effects on depression and fatigue (a correlated symptom of depression).
Additional explanations of why mindfulness did not appear as a mediator, are related to the concept of mindfulness or mechanism as defined may not be specifically assessed within each measurement survey, as conceptualized, and identified in the mechanistic process. For the future, it is recommended that two approaches be considered to assess the mechanism of intervention change: (1) dismantle studies to compare active ingredients; and (2) examine the central concept of mindfulness to determine if it is a single concept, or if there are different facets of mindfulness leading to change; therefore close examination of measures of mindfulness is vital to determine if it is a unidimensional concept or multifaceted construct (Kazdin et al., 2007; Boden et al., 2012).
Assessment of the concept of mindfulness, by the FFMQ and CAMSR indicate differential facets for mindfulness may possibly be contributing to mediation effects. Future examination of these facets, CAMSR, (acceptance, attention, awareness, and present focus) and the FFMQ (acting with awareness, describing, non-judging, non-reactivity, and observing) may provide insight into the mechanism of action. Currently, there may be other mechanisms, of how MBSR works, such as decreasing rumination in the meditation process, this concept is an important area for future consideration.
Stress and fear as mediators
Perceived stress and fear of recurrence were found to mediate the positive effects of MBSR(BC) on psychological health outcomes of anxiety and fatigue. Perceived stress mediated the effects of MBSR(BC) on state anxiety and fatigue. Prior to this study, reduced stress and fear have been evaluated as outcome measures of mindfulness (non-MBSR) interventions in non-cancer populations (Kim et al., 2016; O’Bryan et al., 2018), as well as MBSR interventions in cancer populations (Butow et al., 2017; Cheli et al., 2019; Compen et al., 2018; Crane-Okada et al., 2012; Lengacher et al., 2009, 2011, 2016). Examining stress as an underlying physiological-mechanistic process of how the MBSR intervention works, have largely remained unexplored. This study provides further evidence that “fear” and “perceived stress” are cognitive mechanisms for symptom improvement in anxiety and fatigue. These results further validate “fear of recurrence” as a mediator of the MBSR(BC) intervention on symptom improvement (Lengacher et al., 2014).
Related to the mechanism of stress and fear or recurrence as mediators, a further explanation of why mindfulness may not be a mediator is warranted. Evidence shows that continued cultivation of mindfulness, self regulates emotions, and decreases psychological stress (Hölzel et al., 2011). Additional considerations for considering mediators as an outcome, change in the outcome must precede and predict outcome effects through the intervention (Kraemer et al., 2002).
Mediation effects on fatigue
While perceived stress was found to be a mediator of fatigue, “fear of recurrence” did not mediate fatigue. Furthermore, despite a large effect size in the subgroup analysis for MBSR(BC) reducing fatigue (0.7), the effects explained by the mediators were minimal. MBSR(BC) seems to be most effective among BCS experiencing high anxiety and fatigue (Lengacher et al., 2016), i.e., individuals who may benefit most from the intervention. Since fatigue is one of the most distressing symptoms identified for BCS, understanding how the MBSR(BC) reduces fatigue is vital to future research. One could hypothesize that if MBSR(BC) self regulates reactions to emotional distress, this in turn may decrease emotional fatigue. Future research may also test if decreased rumination may be the process through which fatigue is decreased.
Future research may also examine cognitive and neurobiological mechanisms underlying self-compassion in relation to MBSR(BC) as an intervention to improve well-being. In the same vein, MBSR has shown promising results in reducing rumination in cancer populations (Campbell et al., 2012; Jain et al., 2007), but this has yet to be examined as a possible mechanism of MBSR in lowering stress and anxiety. A limitation of this current study is that self-reported fear and stress are naturally intertwined with self-reported anxiety, and therefore require further investigations utilizing objective measures of how these mediators are functionally changing during and after the MBSR(BC) intervention period.
Conclusions and limitations
This study contributes to the advancement of new knowledge and the scientific understanding of how the MBSR(BC) program may work through the proposed mechanisms practiced by participants as part of the intervention. Specifically, the effectiveness of MBSR(BC) is believed to occur by participants incorporating greater emotional and cognitive control through self-regulation of reactions to internal and external experiences. With a paucity of researchers investigating these mechanisms, this current study provides support for cognitive mechanisms being central to the success of the MBSR(BC) intervention. Ultimately, the goal of this work is to increase the QOL and improve distressing symptoms among BCS transitioning off treatment. The major benefits of performing the mediation analyses for this study are to advance clinical treatment research for cancer survivors thus providing evidence for intervention components (Moyer et al., 2012). Testing the mechanisms of action advances intervention research by “optimizing” the therapeutic active benefits and tailoring interventions more specifically for BCS (Alan E. Kazdin, 2007). Results of this mediation analyses may contribute to advancement of symptom science and theory development (Alan E. Kazdin, 2007), through a more meaningful understanding of mindfulness (Brown et al., 2007).
We postulated that to achieve the maximum benefit from the MBSR(BC) program, “practice and proficiency” in mindfulness are critically important elements through reducing fear of recurrence and perceived stress. MBSR(BC) may result in cognitive adaptations that in turn result in reduced physical and psychological symptoms and increased well-being. To advance the science of empirical investigations of intervention strategies, it is essential within larger clinical trials to validate MBSR intervention mechanisms that are specifically tailored for cancer survivors.
A limitation to this analysis was related to the selection of mediators and outcomes that guided by our proposed mechanisms of how we proposed MBSR(BC) would work; the actual variables identified were revised slightly based on the empirical results obtained. Thus, since perceived stress was not specified a priori as a potential mediator, results should be cautiously interpreted.
Data availability
Data will be archived in accordance with the NIH Data Sharing Plan, a national data repository.
References
American Cancer Society (2019). Cancer Facts & Figures. In American Cancer Society (Ed.). Atlanta.
American Cancer Society (2020). Survival Rates for Breast Cancer Retrieved from https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html
Baer, R. A. (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science and Practice, 10(2), 125–143. https://doi.org/10.1093/clipsy/bpg015
Baer, R. A., Lykins, E., & Peters, J. R. (2012). Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. The Journal of Positive Psychology, 7, 230–238.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45.
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., & Williams, J. M. (2008). Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment, 15, 329–342.
Bishop, S. R. (2002). What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine 64(1), 71–83. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11818588
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology Science and Practice, 11, 230–241.
Boden, M. T., Bernstein, A., Walser, R. D., Bui, L., Alvarez, J., & Bonn-Miller, M. O. (2012). Changes in facets of mindfulness and posttraumatic stress disorder treatment outcome. Psychiatry Research, 200(2–3), 609–613.
Boyle, C. C., Stanton, A. L., Ganz, P. A., Crespi, C. M., & Bower, J. E. (2017). Improvements in emotion regulation following mindfulness meditation: Effects on depressive symptoms and perceived stress in younger breast cancer survivors. Journal of Consulting and Clinical Psychology, 85, 397.
Bränström, R., Kvillemo, P., Brandberg, Y., & Moskowitz, J. T. (2010). Self-report mindfulness as a mediator of psychological well-being in a stress reduction intervention for cancer patients- A randomized study. Annals of Behavioral Medicine, 39, 151–161.
Bränström, R., Kvillemo, P., & Moskowitz, J. T. (2012). A randomized study of the effects of mindfulness training on psychological well-being and symptoms of stress in patients treated for cancer at 6-month follow-up. International journal of behavioral medicine, 19, 535–542.
Brown, K. W., & Cordon, S. (2009). Toward a Phenomenology of Mindfulness: Subjective Experience and Emotional Correlates. In F. Didonna (Ed.), Clinical Handbook of Mindfulness. New York: Springer Science.
Brown, K. W., Ryan, R. A., & Creswell, J. D. (2007). Mindfulness: Theoretical foundations and evidence for its salutary effects. Psychological Inquiry, 18(4), 211–237. Retrieved from <Go to ISI>://000250865000001
Butow, P. N., Turner, J., Gilchrist, J., Sharpe, L., Smith, A. B., Fardell, J. E., & Gebski, V. J. (2017). Randomized trial of ConquerFear: A novel, theoretically based psychosocial intervention for fear of cancer recurrence. Journal of Clinical Oncology, 35, 4066–4077.
Campbell, T. S., Labelle, L. E., Bacon, S. L., Faris, P., & Carlson, L. E. (2012). Impact of mindfulness-based stress reduction (MBSR) on attention, rumination and resting blood pressure in women with cancer: A waitlist-controlled study. Journal of Behavioral Medicine, 35, 262–271.
Carlson, L. E., Doll, R., Stephen, J., Faris, P., Tamagawa, R., Drysdale, E., & Speca, M. (2013). Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer (MINDSET). Journal of Clinical Oncology, 31, 3119–3126. https://doi.org/10.1200/jco.2012.47.5210.
Carpenter, J. S., & Andrykowski, M. A. (1998). Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research, 45(1 Spec No), 5–13. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=9720850
Cheli, S., Caligiani, L., Martella, F., De Bartolo, P., Mancini, F., & Fioretto, L. (2019). Mindfulness and metacognition in facing with fear of recurrence: A proof-of-concept study with breast-cancer women. Psycho-oncology, 28, 600–606.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/6668417
Compen, F., Bisseling, E., Schellekens, M., Donders, R., Carlson, L., van der Lee, M., & Speckens, A. (2018). Face-to-face and internet-based mindfulness-based cognitive therapy compared with treatment as usual in reducing psychological distress in patients with cancer: A multicenter randomized controlled trial. Journal of Clinical Oncology, 36, 2413–2421.
Crane-Okada, R., Kiger, H., Sugerman, F., Uman, G. C., Shapiro, S. L., Wyman-McGinty, W., & Anderson, N. L. (2012). Mindful movement program for older breast cancer survivors: A pilot study. Cancer Nursing, 35, E1–E13.
DeSantis, C. E., Ma, J., Gaudet, M. M., Newman, L. A., Miller, K. D., Goding Sauer, A., & Siegel, R. L. (2019). Breast cancer statistics. CA A Cancer J Clin, 69, 438–451.
Feldman, G., Hayes, A., Kumar, S., Greeson, J., & Laurenceau, J. (2007). Mindfulness and emotion regulation: The development and initial validation of the cognitive and affective mindfulness scale-revised (CAMS-R). Journal of Psychopathology and Behavioral Assessment, 29, 177–190.
Garland, S. N., Carlson, L. E., Stephens, A. J., Antle, M. C., Samuels, C., & Campbell, T. S. (2014). Mindfulness-based stress reduction compared with cognitive behavioral therapy for the treatment of insomnia comorbid with cancer: a randomized, partially blinded, noninferiority trial. Journal of Clinical Oncology, 32, 449–457.
Gu, J., Strauss, C., Bond, R., & Cavanagh, K. (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12.
Hall, D. L., Luberto, C. M., Philpotts, L. L., Song, R., Park, E. R., & Yeh, G. Y. (2018). Mind-body interventions for fear of cancer recurrence: A systematic review and meta-analysis. Psycho-oncology, 27, 2546–2558.
Hamilton, N. A., Kitzman, H., & Guyotte, S. (2006). Enhancing health and emotion: Mindfulness as a missing link between cognitive therapy and positive psychology. Journal of Cognitive Psychotherapy, 20, 123–134.
Hann, D. M., Jacobsen, P., Martin, S., Azzarello, L., & Greenberg, H. (1998). Fatigue and quality of life following radiotherapy for breast cancer: A comparative study. Journal of Clinical Psychology in Medical Settings, 5, 19–33.
Hayes, S., Luoma, J., Bond, F., Masuda, A., & Lillis, J. (2006). Behaviour research and therapy. Behaviour Research and Therapy, 44, 1–25.
Hicks, R., & Tingley, D. (2011). Causal mediation analysis. Stata J, 11, 605.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6, 537–559.
Imai, K., Keele, L., & Tingley, D. (2010). A general approach to causal mediation analysis. Psychological Methods, 15, 309–334. https://doi.org/10.1037/a0020761.
Jain, S., Shapiro, S. L., Swanick, S., Roesch, S. C., Mills, P. J., Bell, I., & Schwartz, G. E. (2007). A randomized controlled trial of mindfulness meditation versus relaxation training: Effects on distress, positive states of mind, rumination, and distraction. Annuals of Behavioral Medicine, 33, 11–21. https://doi.org/10.1207/s15324796abm3301_2.
Johns, S. A., Brown, L. F., Beck-Coon, K., Monahan, P. O., Tong, Y., & Kroenke, K. (2015). Randomized controlled pilot study of mindfulness-based stress reduction for persistently fatigued cancer survivors. Psycho-Oncology, 24, 885–893.
Josefsson, T., Larsman, P., Broberg, A., & Lundh, L.-G. (2011). Self-reported mindfulness mediates the relation between meditation experience and psychological well-being. Mindfulness, 2, 49–58.
Kabat-Zinn, J. (1990). Full-catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. . Bantam Doubleday Dell Publishing.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology-Science and Practice, 10, 144–156.
Kabat-Zinn, J., Lipworth, L., & Burney, R. (1985). The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine, 8(2), 163–190. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=3897551
Kabat-Zinn, J., Massion, A. O., Kristeller, J., Peterson, L. G., Fletcher, K. E., Pbert, L., . . . Santorelli, S. F. (1992). Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry, 149(7), 936–943. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1609875
Kazdin, A. E. (2006). Mechanisms of Change in Psychotherapy: Advances, Breakthroughs, and Cutting-Edge Research (Do Not Yet Exist).
Kazdin, A. E. (2007). Mediators and Mechanisms of Change in Psychotherapy Research. Annual Review of Clinical Psychology, 3(1), 1. Retrieved from http://ezproxy.lib.usf.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edb&AN=53344843&site=eds-live
Keller, S., Bann, C. M., Dodd, S. L., Schein, J., Mendoza, T. R., & Cleeland, C. S. (2004). Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clinical Journal of Pain, 20(5), 309–318. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15322437
Kim, M. K., Lee, K. S., Kim, B., Choi, T. K., & Lee, S.-H. (2016). Impact of mindfulness-based cognitive therapy on intolerance of uncertainty in patients with panic disorder. Psychiatry investigation, 13, 196.
Kraemer, H., Wilson, T., Fairburn, C. C. G., & Agras, W. S. (2002). Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry, 59, 877–883.
Labelle, L. E., Campbell, T. S., & Carlson, L. E. (2010). Mindfulness-based stress reduction in oncology: Evaluating mindfulness and rumination as mediators of change in depressive symptoms. Mindfulness, 1, 28–40.
Labelle, L. E., Lawlor-Savage, L., Campbell, T. S., Faris, P., & Carlson, L. E. (2015). Does self-report mindfulness mediate the effect of Mindfulness-Based Stress Reduction (MBSR) on spirituality and posttraumatic growth in cancer patients? The Journal of Positive Psychology, 10, 153–166.
Laurenceau, J.-P., Hayes, A. M., & Feldman, G. C. (2007). Some methodological and statistical issues in the study of change processes in psychotherapy. Clinical Psychology Review, 27, 682–695.
Lee-Jones, C., Humphris, G., Dixon, R., & Hatcher, M. B. (1997). Fear of cancer recurrence--a literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psycho-Oncology, 6(2), 95–105. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9205967
Lengacher, C. A., Johnson-Mallard, V., Barta, M., Fitzgerald, S., Moscoso, M. S., Post-White, J., & Kip, K. E. (2011). Feasibility of a mindfulness-based stress reduction program for early-stage breast cancer survivors. Journal of Holistic Nursing, 29, 107–117.
Lengacher, C. A., Johnson-Mallard, V., Post-White, J., Moscoso, M. S., Jacobsen, P. B., Klein, T. W., & Kip, K. E. (2009). Randomized controlled trial of mindfulness-based stress reduction (MBSR) for survivors of breast cancer. Psycho-Oncology, 18, 1261–1272.
Lengacher, C. A., Reich, R., Post-White, J., Moscoso, M., Shelton, M., Barta, M., & Budhrani, P. (2012). Mindfulness based stress reduction in post-treatment breast cancer patients: An examination of symptoms and symptom clusters. Journal of Behavioral Medicine, 35, 86–94.
Lengacher, C. A., Reich, R. R., Paterson, C. L., Jim, H. S., Ramesar, S., Alinat, C. B., & Kip, K. E. (2015). The effects of mindfulness-based stress reduction on objective and subjective sleep parameters in women with breast cancer: A randomized controlled trial. Psycho-Oncology, 24, 424–43.
Lengacher, C. A., Reich, R. R., Paterson, C. L., Ramesar, S., Park, J. Y., Alinat, C. B., & Kip, K. E. (2016). Examination of broad symptom improvement due to mindfulness-based stress reduction for breast cancer survivors: A randomized controlled trial. Journal of Clinical Oncology, 37, 2827–2834.
Lengacher, C. A., Shelton, M. M., Reich, R. R., Barta, M. K., Johnson-Mallard, V., Moscoso, M. S., & Kip, K. E. (2014). Mindfulness based stress reduction (MBSR(BC)) in breast cancer: Evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). Journal of Behavioral Medicine, 37, 185–195.
Moyer, A., Goldenberg, M., Hall, M. A., Knapp-Oliver, S. K., Sohl, S. J., Sarma, E. A., & Schneider, S. (2012). Mediators of change in psychosocial interventions for cancer patients: A systematic review. Behavioral Medicine, 38, 90–114.
O’Bryan, E. M., Luberto, C. M., Kraemer, K. M., & McLeish, A. C. (2018). An examination of mindfulness skills in terms of affect tolerance among individuals with elevated levels of health anxiety. Anxiety, Stress, & Coping, 31, 702–713.
Preacher, K. J., & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731.
Radloff, L. (1977). The CES-D scale: A self-report depression scale for researching the general population. Application of Psychological Measures, 1, 385–401.
Reich, R. R., Lengacher, C. A., Alinat, C. B., Kip, K. E., Paterson, C., Ramesar, S., & Moscoso, M. (2017). Mindfulness-based stress reduction in post-treatment breast cancer patients: Immediate and sustained effects across multiple symptom clusters. Journal of Pain and Symptom Management, 53, 85–95.
Spielberger, C., Gorsuch, R., & Luschene, R. (1983). Manual for the State-Trait Anxiety Inventory. . Consulting Psychologists.
Vickberg, S. M. (2003). The Concerns About Recurrence Scale (CARS): a systematic measure of women's fears about the possibility of breast cancer recurrence. Annuals of Behavioral Medicine, 25(1), 16–24. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12581932
Ware, J. H., Kosinski, M., & Keller, M. (1994). SF-36 physical and mental health summary scales, a user’s manual. (2nd ed.). The Health Institute.
Xu, W., Zhou, Y., Fu, Z., & Rodriguez, M. (2017). Relationships between dispositional mindfulness, self-acceptance, perceived stress, and psychological symptoms in advanced gastrointestinal cancer patients. Psycho-oncology, 26, 2157–2161.
Zainal, N. Z., Booth, S., & Huppert, F. A. (2013). The efficacy of mindfulness-based stress reduction on mental health of breast cancer patients: A meta-analysis. Psycho-Oncology, 22, 1457–1465.
Funding
This study was supported by the National Cancer Institute (Award Number 1R01 CA131080-01A2). This work also has been supported in part by the Biostatistics and Bioinformatics Shared Resource at the H. Lee Moffitt Cancer Center & Research Institute, an NCI designated Comprehensive Cancer Center (P30-CA076292). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health. This study protocol was approved by the Institutional Review Board at the University of South Florida to ensure the ethical treatment of participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declares that they have no conflicts of interest.
Human and animal rights and informed consent
At orientation for MBSR(BC), BCES, and UC, all participants signed informed consents prior to enrolling in the study. The USF institutional review board at the University of South Florida serves as the University of South Florida's Ethics committee and gave approval, in addition to the Moffitt Cancer Center Scientific Review Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data repository: data will be archived in accordance with the NIH Data Sharing Plan, a national data repository.
Rights and permissions
About this article
Cite this article
Lengacher, C.A., Gruss, L.F., Kip, K.E. et al. Mindfulness-based stress reduction for breast cancer survivors (MBSR(BC)): evaluating mediators of psychological and physical outcomes in a large randomized controlled trial. J Behav Med 44, 591–604 (2021). https://doi.org/10.1007/s10865-021-00214-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-021-00214-0