Abstract
The Five Facet Mindfulness Questionnaire (FFMQ), a widely used and comprehensive assessment of mindfulness, has demonstrated promising psychometric properties among non-clinical and clinical samples and among diverse international samples. Yet, to date, no studies have examined its factor structure, reliability, and validity in a clinical sample of United States (USA) underrepresented minorities. The current study addressed this by investigating the factor structure, internal consistency, test-retest reliability, and construct validity of the FFMQ among 283 low-income African American adults with a recent suicide attempt. Exploratory factor analysis revealed a 20-item, five-factor measure: acting with awareness, describing, non-judging, observing, and non-reacting. Confirmatory factor analysis supported this reduced item five-factor structure. Internal consistency coefficients ranged from 60–86, but test-retest reliability coefficients did not support the temporal stability. Construct validity was supported; FFMQ facets were correlated with theoretically related constructs, such as self-compassion and self-criticism. Several facets were negatively associated with depressive symptoms and suicidal ideation, and the describing facet demonstrated unique predictive validity for depressive symptoms. These findings support the cultural relevance and utility of the FFMQ with African Americans with significant psychological distress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mindfulness has garnered increasing attention in the behavioral health community in recent years. Derived from Buddhist spiritual traditions, mindfulness involves meditative practices that cultivate “paying attention on purpose, in the present moment, and non-judgmentally to the unfolding of experience moment by moment” (p.145) (Kabat-Zinn 2003). This practice has been associated with psychological well-being and self-compassion (Astin et al. 2003; Carmody and Baer 2008) and reduced levels of anxiety, depression, and substance use (Chiesa and Serreti 2009; Grossman et al. 2004). It has been incorporated into several widely used interventions, like mindfulness-based stress reduction (MBSR), dialectical behavior therapy (DBT), mindfulness-based cognitive therapy (MBCT), and acceptance and commitment therapy (ACT) (Hayes et al. 2006; Kabat-Zinn 2003; Linehan 2015; Segal et al. 2002).
Given the growing interest in mindfulness, there has been a desire for a shared operational definition of the construct and corresponding psychometrically sound metrics that would facilitate the investigation of underlying mechanisms and associations with health outcomes. Five primary scales have been used to assess mindfulness: Mindful Attention Awareness Scale (MAAS) (Brown and Ryan 2003), Freiburg Mindfulness Inventory (FMI) (Walach et al. 2006), Kentucky Inventory of Mindfulness Skills (KIMS) (Baer et al. 2004), Cognitive and Affective Mindfulness Scale (CAMS) (Feldman et al. 2006; Hayes and Feldman 2004), and the Mindfulness Questionnaire (MQ) (Chadwick et al. 2008). Despite the strengths of these measures, they have been critiqued for only assessing a subset of the mindfulness dimensions (Tran et al. 2013). For instance, the MAAS included attentional and awareness aspects of mindfulness, but not acceptance and non-judging (Baer 2003). Moreover, although the CAMS measured four mindfulness facets (attention, present focus, awareness, acceptance/non-judging), the subscales did not demonstrate acceptable levels of internal consistency (Feldman et al. 2006).
These limitations were addressed by collating these five questionnaires into a single, comprehensive measure, the Five Facet Mindfulness Questionnaire (FFMQ), which assesses five mindfulness facets: (1) acting with awareness—attending to present-moment experiences without being distracted; (2) describing—expressing thoughts, feelings, beliefs, and other internal experiences in words; (3) non-judging—accepting inner experience without judgment or self-criticism; (4) observing—noticing internal and external experiences; and (5) non-reacting—refraining from impulsive reactions to inner experiences (Baer et al. 2006). Among predominantly European American samples, these facets have demonstrated good internal consistency (alphas from 0.75 to 0.91) and construct validity, as evidenced by their correlations with several variables (Baer et al. 2006; Baer et al. 2008). All facets, except for observing, have demonstrated incremental validity with regard to predicting psychological symptom levels and assessing mindfulness (Aguado et al. 2015; Baer et al. 2006).
The factor structure, reliability, and validity of the FFMQ have been supported in non-meditators and experienced meditators as well as in non-clinical samples (Baer et al. 2008; Bohlmeijer et al. 2011; Christopher et al. 2012). To date, only one study has examined the FFMQ in a US clinical sample of individuals diagnosed with mood disorders (e.g., depression) and/or anxiety disorders (e.g., panic disorder) (Curtiss and Klemanski 2014). Although both a five-factor model and a four-factor model, excluding observing, were tested via confirmatory factor analysis (CFA), results supported a four-factor hierarchical solution that included acting with awareness, describing, non-judging, and non-reacting. This suggests that mindfulness is a multidimensional construct with a factor structure that differs in the context of psychopathology; observing may be inconsistent with mindfulness in the context of severe psychopathology (Curtiss and Klemanski 2014). In this clinical sample, the measure demonstrated good internal consistency: acting with awareness (α = .90), describing (α = .90), non-judging (α = .92), and non-reacting (α = .80). Convergent validity was also supported; the facets were inversely associated with emotion dysregulation, emotional avoidance, and psychological distress.
Although these findings extend our understanding of the psychometric properties of the FFMQ in US clinical samples, the sample was majority European American (79.5%). In addition, several studies have adapted and translated the FFMQ for international samples (e.g., Italian, Dutch, Chinese) (Deng et al. 2011; Giovannini et al. 2014; Veehof et al. 2011), but only one study investigated the psychometrics of a non-translated FFMQ among a Spanish sample (Cebolla et al. 2012). Results confirmed a hierarchical five-factor model, and internal consistency for the five facets ranged from acceptable to excellent (α’s ranged from .75–.91). Convergent validity was supported via inverse associations among the facets and psychological symptoms (depression, anxiety, and somatization). However, observing was unrelated to psychological symptoms. Collectively, these findings support the measure’s use across clinical and diverse samples, yet highlight the value of additional examination in diverse populations.
To date, no studies have investigated the factor structure or reliability and validity of the FFMQ among US racial and ethnic minority clinical samples. This is concerning given efforts to utilize mindfulness-based interventions to address psychological and physical health disparities experienced by US racial and ethnic minorities (Abercrombie et al. 2007; Dutton et al. 2013; Vallejo and Amaro 2009; Witkiewitz et al. 2013; Woods-Giscombé and Black 2010). The current study is an effort to expand our knowledge base by examining the FFMQ’s psychometric properties in low-income African Americans with a history of a suicide attempt. Because different factor structures have emerged across samples and no psychometric studies have included substantial racial and ethnic minority participants, we had no a priori hypotheses about the FFMQ’s factor structure in our sample. Thus, prior to conducting a CFA, we conducted an exploratory factor analysis (EFA) to investigate which factor structure would emerge. We then hypothesized that (1) CFA results would replicate the factor structure revealed by the EFA; (2) FFMQ facets would exhibit adequate internal consistency and temporal stability; and (3) FFMQ facets would be positively related to the self-kindness and mindfulness dimensions of self-compassion; negatively related to the self-judgment and over-identification dimensions of self-compassion; inversely related to self-criticism, depressive symptoms, and suicidal ideation; and predictive of depressive symptoms and suicidal ideation.
Method
Participants
The sample included 283 men and women who met the following criteria for study inclusion: self-identified as African American, made a suicide attempt with significant intent within the past year (determined by the 20-item Suicide Intent Scale (Beck et al. 1974)), displayed adequate cognitive functioning (measured by the Mini-Mental State Exam (Folstein et al. 2001)), reported minimal psychotic symptoms (measured by the 10-item Nia Psychotic Screen), and did not have a life-threatening medical condition (self-reported). The sample included individuals aged 18–62 years (M = 37.24, SD = 12.24), most of whom were female (52%), unemployed (82%), and had no health insurance (64%). Nearly half of the sample reported having three or more suicide attempts (44%), being homeless (46%), and being single/never married (49%; Table 1).
Procedure
The study used data gathered at the pre- and post-intervention assessment associated with a longitudinal randomized controlled trial examining the relative effectiveness of a compassion-based group therapy versus treatment as usual for African Americans with a recent suicide attempt. Participants were recruited from the emergency unit, inpatient wards, and outpatient clinics associated with an urban public hospital that serves predominately low-income patients. They provided written consent, completed a 2-hour pre-intervention and post-intervention assessment, and received $20 remuneration for each assessment they completed.
Measures
Participants completed 12 measures at the pre- and post-intervention assessment. All measures were read aloud, given the low levels of healthcare literacy in the sample. Only the measures used in this study are described below.
Demographic Questionnaire (DQ)
Participants provided information regarding age, socioeconomic status, marital status, caregiver status, and psychiatric history.
Five Facet Mindfulness Questionnaire (FFMQ)
This 39-item inventory assesses five facets of mindfulness: observing, describing, acting with awareness, non-judging, and non-reacting (Baer et al. 2006). Items are rated on a 5-point Likert scale ranging from 1 (never or very rarely true) to 5 (very often or always true); higher scores represent higher levels of mindfulness. Descriptive and psychometric information is presented in the background above.
Self-compassion Scale (SCS)
This 26-item questionnaire taps six aspects of self-compassion: self-kindness (e.g., “I try to be understanding and patient toward aspects of my personality I don’t like”), self-judgment (e.g., “I’m disapproving and judgmental about my own flaws and inadequacies”), common humanity (e.g., “I try to see my failings as part of the human condition”), isolation (e.g., “When I think about my inadequacies it tends to make me feel more separate and cut off from the rest of the world”), mindfulness (e.g., “When something painful happens I try to take a balanced view of the situation”), and over-identification (e.g., “When I’m feeling down I tend to obsess and fixate on everything that’s wrong”). Scoring is based on a 5-point Likert scale that ranges from 1 (almost never) to 5 (almost always). The SCS has good psychometric properties across diverse samples in terms of internal consistency and test-retest reliability, as well as construct, content, and convergent validity (Deniz et al. 2008; Neff 2003). The self-kindness, self-judgment, mindfulness, and over-identification subscales were used in the current study to examine convergent validity. The following internal consistency coefficients were obtained in the current sample: self-kindness (α = .73), self-judgment (α = .78), mindfulness (α = .70), and over-identification (α = .72).
Levels of Self-criticism Scale (LOSC)
The 22-item LOSC assess comparative and internalized self-criticism (Thompson and Zuroff 2004). Comparative self-criticism is defined as negative self-perception in relation to others, and it encompasses feelings of inferiority. Internalized self-criticism is defined as negative self-perception based on internally held standards, and it includes feelings of failure and inability to reach personal standards. Sample items include: “I fear that if people get to know me too well, they will not respect me” (comparative self-criticism) and “I often get very angry with myself when I fail” (internalized self-criticism). Statements are rated on a 7-point Likert scale ranging from 1 (not at all) to 7 (very well). Good internal consistency and convergent validity with depressive symptoms, psychological distress, self-esteem, and perfectionism have been demonstrated for this measure. However, there are no data on the LOSC’s reliability and validity among a demographically comparable sample. It demonstrated good internal consistency in the current sample (α = .81).
Beck Depression Inventory-II (BDI-II)
The 21-item BDI-II measures depressive symptoms (Beck et al. 1996). Participants rate their symptom severity during the past 2 weeks, ranging from 0 (no experience of the symptom) to 3 (high experience of the symptom). A final score, ranging from 0 to 63, is calculated by summing all scores, and higher scores indicate more severe depressive symptoms. One item includes: “Loss of pleasure: (0) I get as much pleasure as I ever did from the things that I enjoy, (1) I don’t enjoy things as much as I used to, (2) I get very little pleasure from the things I used to enjoy, (3) I can’t get any pleasure from the things I used to enjoy.” Previous research has supported the BDI-II’s use for African American, low-income, and suicidal populations (Carr et al. 2013; Grothe et al. 2005; Joe et al. 2008). Excellent internal consistency was found in the current sample (α = .90).
Beck Scale for Suicidal Ideation (BSS)
The 21-item BSS examines the desire to die, reasons for living, and suicidal intent (Beck and Steer 1991). Items are on a scale from 0 to 2; total scores range from 0 to 42, with higher scores suggesting higher levels of suicidal ideation. An example item is as follows: “(0) I would try to save my life if I found myself in a life-threatening situation; (1) I would take a chance on life or death if I found myself in a life-threatening situation; (2) I would not take the steps necessary to avoid death if I found myself in a life-threatening situation.” The BSS has good internal consistency in African Americans (Houry et al. 2006), including the current sample (α = .85).
Data Analytic Plan
SPSS 23 was used to conduct descriptive statistics, EFA, and correlation analysis. CFA and structural equation modeling (SEM) were conducted in Mplus Version 7.2 (Muthen and Muthen 2012). The current study sought to establish and validate the factor structure of the FFMQ among a clinical sample of African Americans via EFA and CFA; thus, we used split data analysis in which pre- and post-data were combined and then split to create both EFA and CFA samples (Cudeck and Browne 1983). The EFA sample consisted solely of pre-intervention data for 187 participants. The CFA sample consisted of pre- and post-intervention data from 139 participants, resulting in 200 data points. We used the “CLUSTER” option in Mplus to adjust for data from two time points for some individuals. Data were clustered by participant, which adjusts the standard error and chi-squared test of model fit to account for the non-independence in the data.
Results
EFA
Consistent with the approach from Baer et al. (2006), the factor structure of the FFMQ was examined via EFAs that were conducted using principal axis factoring, with an oblique (promax) rotation given that factors were presumed to be correlated. First, to determine the factorability of the correlation matrix, the Bartlett’s test of sphericity (i.e., probability that correlations in a matrix are 0) was examined; it was statistically significant (p < .001), indicating that the data were appropriate for factor analysis. Second, the Kaiser-Meyer-Olkin (KMO) was examined, and a value of .79 was found (i.e., values greater than .60 are desired) (Tabachnick and Fidel 2007), supporting the sampling adequacy for factor analysis. Third, we examined eigenvalues and scree plots to determine the factor structure. Results of the initial EFA revealed that there were eleven factors with eigenvalues greater than one; yet, the scree plot supported five factors. Relying solely on eigenvalues greater than 1.0 can contribute to an overestimation of the number of meaningful factors; thus, it has been argued that the scree plot provides more useful information regarding how many factors should be retained (Floyd and Widaman 1995). Therefore, we conducted a second factor analysis specifying five factors.
The five-factor solution was also conducted using principal axis factoring, with an oblique (promax) rotation. Similar to Baer et al. (2006), we deleted items with a factor loading of less than .40 and with cross-loadings of less than a .20 difference from an item’s highest factor loading. Consistent with test development best practices, we also deleted items with extracted communalities lower than .40, although this criterion was not used in the original scale development process (Tabachnick and Fidel 2007; Worthington and Whittaker 2006). Based on these criteria, 20 of the original 39 items were retained. A final EFA was conducted on the 20-item scale to ensure the factor structure remained the same after deleting poor items (Table 2).
The EFA five-factor solution retained key features of the original FFMQ. Factor 1, acting with awareness, contained four of the original eight items and accounted for 19.69% of the variance. Similarly, factor 2, describing, included five items from the original eight-item subscale and accounted for 17.89% of the variance. Factor 3, non-judging, consisted of four of the original eight items and accounted for 8.58% of the variance. Factor 4, observing, contained four items from the original eight-item subscale, and it accounted for 7.54% of the variance. Lastly, factor 5, non-reacting, contained three of the original items from the seven-item subscale, and it accounted for 6.19% of the variance. Collectively, these facets accounted for 59.89% of the variance.
In addition, the facets demonstrated modest, but significant intercorrelations, supporting their relatedness yet distinctiveness (See Table 3). Some correlations were in unexpected directions; non-judging was inversely correlated with observing and non-reacting. This suggests that although these FFMQ facets are related, they may differentially function in a psychiatric sample of low-income African Americans. Moreover, acting with awareness was not correlated with observing or non-reacting, and describing was not associated with non-judging. This indicates that there also are non-overlapping aspects of mindfulness being measured by the FFMQ in this sample.
CFA
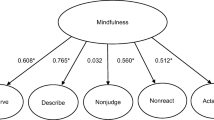
We conducted a CFA with the 20-item FFMQ five-factor solution revealed in the current study’s EFA. CFA analysis was conducted using SEM with the Maximum Likelihood Robust (MLR) estimator, accounting for non-normality in the data. Consistent with existing research (Baer et al. 2006), we compared two models: a five-factor solution consistent with our EFA results and a five-factor hierarchical model with a mindfulness latent variable that underlies the five facets. However, unlike the original FFMQ validation study, we did not use item parceling; individual items were used as indicators, providing an item-level test of the FFMQ model fit (Christopher et al. 2012). Although the five-factor hierarchical model has outperformed a general five-factor model in previous research (Baer et al. 2006; Baer et al. 2008; Christopher et al. 2012), this was not the case in the current study. Rather, the five-factor model had a better fit than the five-factor hierarchical model, as evidenced by all calculated fit statistics (Kline 2010). With regard to the chi-squared test, values closer to 0 indicate a better fit; the five-factor model was 226.58 whereas the five-factor hierarchical model was 266.39. In terms of the RMSEA, scores range from 0 to 1, and a value of .06 or less represents an acceptable model fit. The RMSEA for the five-factor model was .05 (acceptable), and it was .06 for the five-factor hierarchical model (acceptable). In terms of the CFI, values closer to 1 indicate a better fit, with a value of .90 generally suggesting an acceptable model fit. The CFI for the five-factor model was .93 compared to the CFI value of .89 for five-factor hierarchical model. Finally, SRMR values can range from 0 to 1, with a value of .08 or less indicating an acceptable model. The five-factor model SRMR was .06, whereas the five-factor hierarchical model SRMR was .09 (Table 4). All items loaded significantly onto the appropriate facet (See Table 5).
Reliability
Internal Consistency
To test the hypothesis that the FFMQ facets would have good internal consistency, Cronbach’s alphas (α) were calculated. The following reliability coefficients were obtained for the reduced-item subscales based on the EFA: acting with awareness (α = .87), describing, (α = .82), non-judging (α = .69), observing (α = .71), and non-reacting (α = .60). Although these alpha coefficients are lower than those obtained in the original sample for some subscales (Table 6), three of the facet scales exhibited acceptable to good levels of internal consistency and two facets, non-judging and non-reacting, demonstrated poor internal consistency (Cronbach 1951).
Test-Retest
To evaluate the hypothesis that the FFMQ facets would have good temporal stability, we obtained the test-retest reliabilities of the EFA reduced-item facets by conducting bivariate correlations between two time points, pre-intervention and 6-week follow up, for all participants. The following 6-week test-retest reliability correlations were obtained: acting with awareness (r = 0.48, p = .00), describing (r = 0.22, p = .05), non-judging (r = .32, p = .00), observing (r = 0.54, p = .00), and non-reacting (r = .24, p = .03). These scores are within the unacceptable to poor range. Thus, the hypothesis that the FFMQ would have good temporal stability was not supported (Cronbach 1947; Schmidt et al. 2003).
Validity
Pre-intervention data were used for convergent validity analyses. Convergent validity was assessed by testing if the reduced-item FFMQ facet scores were associated with self-compassion, levels of self-criticism, depressive symptoms, and suicidal ideation (Table 7). First, we expected all five mindfulness facets to be positively related to the SCS subscales of self-kindness and mindfulness and to the total SCS score. As expected, describing, non-reacting, and observing were positively related to self-kindness and mindfulness. Although acting with awareness was related to self-kindness, it was not related to mindfulness. Surprisingly, non-judging was not associated with self-kindness and was negatively associated with mindfulness. All facets were positively associated with the total SCS score. Also related to self-compassion, we hypothesized that the five facets would be negatively related to the self-judgment and over-identification subscales of the SCS. As expected, acting with awareness, describing, non-judging, and non-reacting were negatively related to self-judgment and over-identification. Taken together, the FFMQ facets show good, albeit not excellent, convergent validity with dimensions of self-compassion.
Second, it was hypothesized that levels of self-criticism would be negatively related to the five facets. As expected, level of self-criticism was negatively associated with acting with awareness and non-judging. However, it was not significantly associated with describing, observing, and non-reacting. Thus, our hypothesis that higher levels of self-criticism were related to lower levels of mindfulness was partially supported.
Third, we expected that the five facets would be negatively related to depressive symptoms and suicidal ideation. This was partially supported; all facets, except for observing, were negatively related to depressive symptoms. Moreover, two facets (acting with awareness and describing) were negatively related to suicidal ideation. Thus, individuals who endorsed higher levels of certain aspects of mindfulness reported lower levels of depressive symptoms and suicidal ideation.
Fourth, consistent with existing FFMQ psychometric evaluations, we examined if each facet added to the prediction of behavioral health beyond that attributable to other facets. We expected each facet to add to the prediction of depressive symptoms and suicidal ideation (observing was excluded as it did not correlate with depressive symptoms or suicidal ideation). SEM analysis was conducted using Mplus. To account for non-normality in the data, we used the MLR estimator in the analyses. All variables were treated as latent variables, and to scale each latent variable, the paths to the indicators with the highest loading were set to 1. The variables were allowed to covary in the analysis. We reported standardized parameter estimates and regression coefficients. Our hypotheses were partially supported. Only describing (β = −.18, p = .01) was negatively associated with depressive symptoms in the context of other facets, whereas no facets were associated with suicidal ideation in the context of the other facets (Fig. 1). These findings provide partial support for the unique contributions of each facet in understanding the association between mindfulness and behavioral health outcomes.
Discussion
Building upon efforts to examine the performance of mindfulness assessments in diverse samples, this study investigated the FFMQ’s psychometric properties in low-income African Americans with significant distress. The results that emerged were promising in terms of the relevance of the measure for this sample. Exploratory factor analyses revealed a five-factor structure that was similar to but shorter than the original five facet structure (Baer et al. 2006), and CFA using this 20-item FFMQ demonstrated its superiority over a hierarchical five-factor structure. This suggests that the five facets, although related, may not adequately represent a higher order mindfulness construct in a clinical sample of African Americans. This was underscored by the unexpected negative associations among some facets. With regard to the measure’s reliability in this sample, the 20-item FFMQ had adequate to good internal consistency, but its temporal stability was not supported. In terms of validity, this measure in this sample demonstrated strong convergent validity as most of the scores correlated in the expected direction with theoretically-related constructs. In addition, the describing facet uniquely predicted reduction in depressive symptoms in the context of other facets. These findings highlight the multidimensional nature of the mindfulness construct with facets that differentially function in a severely distressed clinical sample of African Americans.
Despite the promising findings, mixed findings emerged regarding the FFMQ’s reliability in this sample. Internal consistency coefficients were adequate to good for most facets, indicating that facet items measured the same general construct (Baer et al. 2006). However, test-retest reliability correlations were poor for all facets. In this sample, the facets may reflect state mindfulness rather than individual differences in trait mindfulness. Prior data suggest that increased practice of state mindfulness via meditative practices increases trait mindfulness. However, in a clinical sample of non-meditators where engagement in state mindfulness is variable, trait mindfulness may be variable over time (Kiken et al. 2015). Moreover, it is unclear if our findings differ from the original sample, as test-retest reliability correlations were not reported (Baer et al. 2006). Test-retest reliabilities have only been reported for some translated versions of the FFMQ (e.g., Chinese, Italian, Brazilian) (de Barros et al. 2014; Deng et al. 2011; Giovannini et al. 2014), which are not comparable to the English version. Thus, although this study uniquely reports the test-retest reliabilities, more research is needed to understand if facet test-retest reliabilities reflect scale measurement qualities or differential stability of the facets across diverse samples.
Surprisingly, some facets were negatively associated with each other. Non-judging was inversely associated with observing and non-reacting. Other studies have found the greatest variance in scale correlations between non-judging and observing, which has been attributed to the fact that difficulties maintaining a non-judgmental attitude and problems with attention/observation can impede the development of mindfulness skills and may occur in different categories of individuals (Lilja et al. 2013). A negative correlation between these constructs has been found in other samples (Lilja et al. 2011) and on other mindfulness measures (Baer et al. 2004). This negative association is consistent with evidence that non-judging of inner experience is akin to metacognitive processes (Solem et al. 2015), whereas observing and non-reacting to inner experience are more associated with mindfulness. The counterintuitive relation between non-judging and non-reacting suggests that these facets serve different functions among low-income African Americans with past suicide attempts. An example non-judging item is, “I tell myself I shouldn’t be feeling the way that I’m feeling” (R). Higher endorsement of this item is suggestive of greater self-judgment, and in our sample, is associated with less reactivity. It could be that among individuals with past suicide attempts, telling themselves that they should not feel suicidal or hopeless may protect against reactive, and potentially harmful, behaviors. Acting with awareness was not associated with observing or non-reacting. It has been unrelated to observing in previous research with clinical samples (Curtiss and Klemanski 2014). People with low scores on acting with awareness, but not on observing or any other facet, often are diagnosed with attention deficit hyperactivity disorder (Smalley et al. 2009). With regard to the lack of association between acting with awareness and non-reactivity, it has been presumed that acting with awareness involves mindfully attending to everyday activities whereas non-reactivity measures more complex applications of mindfulness skills involving extensive meditation practice (Lilja et al. 2013). Given that our study largely included pre-intervention data, it could be that participants possess rudimentary mindfulness skills, but have yet to acquire more sophisticated skills. Future studies need to examine the psychological profiles of individuals with unusual patterns of scores and changes on FFMQ facets over time (Lilja et al. 2013).
With regard to convergent validity, all facets of mindfulness were positively related to self-compassion overall. This suggests a robust association between mindfulness and self-compassion in this sample. This is in keeping with existing research including meditators and non-mediators (Baer et al. 2012). Despite the apparent overlap in these constructs, there is mounting evidence that mindfulness and self-compassion differentially predict psychological well-being and thus are distinct, albeit related constructs (Baer et al. 2012).
Also related to construct validity, this study uniquely found that acting with awareness and non-judging were negatively associated with self-criticism. The link between self-criticism and psychopathology has been established (Cox et al. 2004; Fazaa and Page 2003; Lerman et al. 2012) and research has shown an association between mindfulness and enhanced well-being (Astin et al. 2003; Carmody and Baer 2008). Yet, few studies have examined the link between mindfulness and self-criticism, especially among US samples. Among Chinese adults living in Hong Kong, the mindfulness subscale of the SCS was negatively associated with self-criticism (Wong & Mak 2013). Among Portuguese adolescents, mindfulness measured by the CAMS was negatively related to two components of self-criticism: feelings of inadequacy and feelings of self-loath/hate (Cunha & Paiva, 2012). Mindfulness’ emphasis on noticing unpleasant feelings in a non-judgmental manner may reduce tendencies to disparage personal shortcomings. Additional research is needed on the link between mindfulness and self-criticism among diverse samples, but these preliminary findings suggest that promoting certain aspects of mindfulness may be beneficial for people with high levels of self-criticism.
The data in support of the predictive validity of the facets in terms of both depressive symptoms and suicidal ideation advance the literature. Although limited attention has been paid to the unique variance attributable to the mindfulness facets vis-à-vis depressive symptoms, prior research has documented a link between mindfulness facets and depressive symptoms. For example, among college students, acting with awareness, non-reactivity, and non-judging were inversely related to depressive symptoms and observing was positively related to depressive symptoms (Barnes and Lynn 2010). Among Italian participants, non-judging was the only predictor of depressive symptoms after a 2-year period, even when controlling for sex and baseline levels of depressive symptoms (Petrocchi and Ottaviani 2016). Our study with low-income African Americans with past suicide attempts found that most facets were inversely correlated with depressive symptoms, and describing was associated with reduced depressive symptoms in the context of the other facets. Exploring the relation between mindfulness and depressive symptoms in this sample is necessary given that African Americans have more severe, disabling, and untreated depression than individuals from other ethnoracial groups (Williams et al. 2007), and depression is a leading cause of disease-related disability worldwide (Bromet et al. 2011).
Our study is one of few to examine the mindfulness-suicidal ideation link, despite that fact that mindfulness has been incorporated into treatments that target suicidal behavior (Serpa et al. 2014; Williams et al. 2008). Mindfulness has been associated with strong predictors of suicide, like depressive symptoms and anger, and has been found to weaken the association between neuroticism and suicidal ideation (Tucker et al. 2014). Our results enhance these findings demonstrating the relation between mindfulness facets and suicidal ideation in low-income African Americans. Although no facets were predictive of suicidal ideation in the presence of other mindfulness facets, additional research is needed to investigate how mindfulness relates to suicidal ideation and other outcomes, especially among those at risk for suicide attempts.
Of note, the observing facet did not perform in a manner consistent with existing literature. Among experienced mediators, observing positively correlated with adaptive outcomes (openness to experience, emotional intelligence), whereas among healthy non-meditators and in clinical samples, it correlated positively with maladaptive variables (experiential avoidance, depression) (Baer et al. 2006; Baer et al. 2008). In our clinical sample of non-meditators, observing was not associated with maladaptive outcomes (self-criticism, depressive symptoms, suicidal ideation) and it was positively associated with two mindfulness facets, describing and non-reacting. This further supports the notion that mindfulness is multifaceted and its structure is influenced by differences in meditation expertise, psychopathology, and culture (Barnes and Lynn 2010; Curtiss and Klemanski 2014). The observing facet warrants additional examination with regard to its conceptual relevance to mindfulness and its association with outcomes across diverse samples.
The findings need to be considered in light of study limitations. The sample consisted entirely of African American men and women facing socioeconomic barriers (high poverty, homelessness). These results may not generalize to socioeconomically diverse samples of African Americans or to samples that differ with regard to race/ethnicity and/or social class. Further, all participants had suicide attempt histories. Given the low base rate of death by suicide in African Americans (Kochanek et al. 2013), sample participants are not nationally representative of African Americans. The fact that the current results show that the FFMQ factor structure is not invariant in this sample may be due to the sample being African American, the sample being in extreme distress, some interaction of these variables, or additional variable/s not recognized in this study. Thus, these results are preliminary, and they require replication and further exploration. The majority of the data were cross-sectional, which limits the conclusions that can be drawn about predictive validity in terms of depressive symptoms and suicidal ideation. There is mounting evidence that mindfulness also has neurophysiological correlates (Chiesa et al. 2013; Zeidan et al. 2014) and these were not examined. Lastly, although the current results contribute to the extant literature, it is not clear what facets account for psychometric differences, and additional examinations are warranted. One recommendation to address this issue is to test the psychometric properties of the proposed 20-item FFMQ version with diverse samples using both classical test theory (CCT) and item response theory (IRT) methods.
Despite these limitations, the results further substantiate the psychometric soundness of the FFMQ. They suggest that the FFMQ is a culturally relevant assessment tool for African Americans in research and clinical settings, with attention to how its facets function in this sample. The results add to the burgeoning evidence that mindfulness can reduce the presence and severity of deleterious psychological symptoms. Finally, the data suggest that increasing mindfulness facets through mindfulness-based interventions may reduce depressive symptoms and suicidal ideation in low-income African American suicide attempters. The implementation of such interventions can move the field closer to eliminating the health disparities experienced by this population (Woods-Giscombé and Black 2010; Woods-Giscombé & Gaylord 2014).
References
Abercrombie, P. D., Zamora, A., & Korn, A. P. (2007). Lessons learned providing a Minfdulness-based stress reduction program for low-income multiethnic women with abnormal pap smears. Holistic Nursing Practice, 21, 26–34. doi:10.1097/00004650-200701000-00006.
Aguado, J., Luciano, J. V., Cebolla, A., Serrano-Blanco, A., Soler, J., & Garcia-Campayo, J. (2015). Bifactor analysis and construct validity of the Five Facet Mindfulness Questionnaire (FFMQ) in non-clinical Spanish samples. Froniters in Psychology, 6. doi:10.3389/fpsyg.2015.00404.
Astin, J. A., Shapiro, S. L., Eisenberg, D. M., & Forys, K. L. (2003). Mind-body medicine: state of the science implications for practice. The Journal of the American Board of Family Practice, 16, 131–147. doi:10.3122/jabfm.16.2.131.
Baer, R. A. (2003). Mindfulness training as a clinical intervention: a conceptual and empirical review. Clinical Psychology: Science and Practice, 10, 125–143. doi:10.1093/clipsy.bpg015.
Baer, R. A., Smith, G. T., & Allen, K. B. (2004). Assessment of mindfulness by self-report: the Kentucky Inventory of Mindfulness Skills. Assessment, 11, 191–206. doi:10.1177/1073191104268029.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment in Education, 13, 27–45. doi:10.1177/1083191105283504.
Baer, R. A., Smith, G. T., Lykins, E. L. B., Button, D., Krietemeyer, J., Sauer, S., et al. (2008). Construct validity of the Five Facet Mindfulness Questionnaire in meditating and nonmeditating samples. Assessment, 15, 329–342. doi:10.1177/1073191107313003.
Baer, R. A., Lykins, E. L. B., & Peters, J. R. (2012). Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. The Journal of Positive Psychology, 7, 230–238. doi:10.1080/17439760.2012.674548.
Barnes, S. M., & Lynn, S. J. (2010). Mindfulness skills and depressive symptoms: a longitudinal study. Imagination, Cognition, and Personality, 30, 77–91. doi:10.2190/IC.30.1.e.
Beck, A. T., & Steer, R. (1991). Beck Scale for Suicide Ideation manual. San Antonio: Harcourt Brace.
Beck, A. T., Schuyler, D., & Herman, I. (1974). The development of suicide intent scales. In A. T. Beck, H. L. Resnick, & D. J. Littieri (Eds.), Prediction of suicide (pp. 45–56). Bowie: Charles Press.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory manual (2nd ed.). San Antonio: Psychological Corporation.
Bohlmeijer, E. T., ten Klooster, P. M., Fledderus, M., Veehof, M., & Baer, R. A. (2011). Psychometric properties of the Five Facet Mindfulness Questionnaire in depressed adults and development of a short form. Assessment, 18, 308–320. doi:10.1177/1073191111408231.
Bromet, E., Andrade, L. H., Hwang, I., Sampson, N. A., Alonso, J., De Girolamo, G., et al. (2011). Cross-national epidemiology of DSM-IV major depressive episode. BMC Medicine, 9. doi:10.1186/1741-7015-9-90.
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. doi:10.1037/0022-3514. 84.4.822.
Carmody, J., & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31, 23–33. doi:10.1007/s10865-007-9130-7.
Carr, E. R., Woods, A. M., Vahabzadeh, A., Sutton, C., Witteneaur, J., & Kaslow, N. J. (2013). PTSD, depressive symptoms, and suicidal ideation in African American women: a mediated model. Journal of Clinical Psychology in Medical Settings, 20, 37–45. doi:10.1007/s10880-012-9316-1.
Cebolla, A., García-Palacios, A., Soler, J., Guillen, V., Baños, R., & Botella, C. (2012). Psychometrics properties of the Spanish validation of the Five Facets of Mindfulness Questionnaire. European Journal of Psychiatry, 26, 118–126. doi:10.4321/S0213-61632012000200005.
Chadwick, P., Hember, M., Symes, J., Peters, E., Kuipers, E., & Dagnan, D. (2008). Responding mindfully to unpleasant thoughts and images: reliability and validity of the Southampton Mindfulness Questionnaire (SMQ). British Journal of Clinical Psychology, 47, 451–455. doi:10.1348/014466508X314891.
Chiesa, A., & Serreti, A. (2009). Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. Journal of Alternative & Complementary Medicine, 15, 593–600. doi:10.1089/acm.2008.0495.
Chiesa, A., Serreti, A., & Jakobsen, J. C. (2013). Mindfulness: top-down or bottom-up emotion regulation strategy? Clinical Psychology Review, 33, 82–96. doi:10.1016/j.cpr.2012.10.006.
Christopher, M. S., Neuser, N. J., Michael, P. G., & Baitmangalkar, A. (2012). Exploring the psychometric properties of the Five Facet Mindfulness Questionnaire. Mindfulness, 3, 124–131. doi:10.1007/s12671-011-0086-x.
Cox, B. J., Enns, M. W., & Clara, I. P. (2004). Psychological dimensions associated with suicidal ideation and attempts in the National Comorbidity Survey. Suicide and Life-threatening Behavior, 34, 209–219 Retrieved from http://www.guilford.com/cgi-bin/cartscript.cgi?page=pr/jnsl.htm&dir=periodicals/per_psych&cart_id=.
Cronbach, L. J. (1947). Test reliability: Its meaning and determination. Psychometrika, 12, 1–16. doi:10.1007/BF02289289.
Cronbach, L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16, 297–334. doi:10.1007/BF02310555.
Cudeck, R., & Browne, M. W. (1983). Cross-validation of covariance structures. Multivariate Behavioral Research, 18, 147–167. doi:10.1207/s15327906mbr1802_2.
Cunha, M. & Paiva, M.J. (2012). Text anxiety in adolescents: The role of self-criticism and acceptance and mindfulness skills. The Spanish Journal of Psychology, 15(2), 533-543. doi: 10.5209/rev_SJOP.2012.v15.n2.38864
Curtiss, J., & Klemanski, D. H. (2014). Factor analysis of the Five Facet Mindfulness Questionnaire in a heterogeneous clinical sample. Journal of Psychopathology and Behavioral Assessment, 36, 683–694. doi:10.1007/s10862-014-9429-y.
de Barros, V. V., Kozasa, E. H., de Souza, I. C. W., & Ronzani, T. M. (2014). Validity evidence of the Brazilian version of the Five Facet Mindfulness Questionnaire (FFMG). Psicologia: Teoria e Pesquisa, 30, 317–327. doi:10.1590/S0102-37722014000300009.
Deng, Y.-Q., Liu, X.-H., Rodriguez, M. A., & Xia, C.-Y. (2011). The Five Facet Mindfulness Questionnaire: psychometric properties of the Chinese version. Mindfulness, 2, 123–128. doi:10.1007/s12671-011-0050-9.
Deniz, M., Kesici, S., & Sumer, A. S. (2008). The validity and reliability of the Turkish version of the Self-compassion Scale. Social Behavior and Personality: An International Journal, 36, 1151–1160. doi:10.2224/sbp.2008.36.9.1151.
Dutton, M. A., Bermudez, D., Matas, A., Majid, H., & Myers, N. L. (2013). Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cognitive and Behavioral Practice, 20, 23–32. doi:10.1016/j.cbpra.2011.08.003.
Fazaa, N., & Page, S. (2003). Dependency and self-criticism as predictors of suicidal behavior. Suicide and Life-threatening Behavior, 33, 172–185. doi:10.1521/suli.33.2.172.22777.
Feldman, G., Hayes, A. F., Kumar, S., Greeson, J., & Laurenceau, J.-P. (2006). Mindfulness and emotion regulation: the development and initial validation of the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R). Journal of Psychopathology and Behavioral Assessment, 29, 177–190. doi:10.1007/s10862-006-9035-8.
Floyd, F. J., & Widaman, K. F. (1995). Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment, 7, 286–299. doi:10.1037/1040-3590.7.3.286.
Folstein, M. F., Folstein, S. E., McHugh, P. R., & Fanjiang, G. (2001). Mini-mental state examination. Odessa: Psychological Assessment Resources.
Giovannini, C., Giromini, L., Bonalume, L., Tagini, A., Lang, M., & Amadei, G. (2014). The Italian Five Facet Mindfulness Questionnaire: a contribution to its validity and reliability. Journal of Psychopathology and Behavioral Assessment, 36, 415–423. doi:10.1007/s10862-013-9403-0.
Grossman, P., Niemann, L., Schmidt, S., & Walach, H. (2004). Mindfulness-based stress reduction and health benefits: a meta-analysis. Journal of Psychosomatic Research, 57, 35–43. doi:10.1016/S0022-3999(03)00573-7.
Grothe, K. B., Dutton, G. R., Jones, G. N., Bodenlos, J., Ancona, M., & Brantely, P. J. (2005). Validation of the Beck Depression Inventory-II in a low-income African American sample of medical outpatients. Psychological Assessment, 17, 110–114. doi:10.1037/1040-3590.17.1.110.
Hayes, A. M., & Feldman, G. (2004). Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice, 11, 255–262. doi:10.1093/clipsy.bph080.
Hayes, S. C., Luoma, J. B., Bond, F. W., Masuda, A., & Lillis, J. (2006). Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy, 44, 1–25. doi:10.1016/j.brat.2005.06.006.
Houry, D., Kemball, R., Rhodes, K. V., & Kaslow, N. J. (2006). Intimate partner violence and mental health symptoms in African American female ED patients. American Journal of Emergency Medicine, 24, 444–450. doi:10.1016/j.ajem.2005.12.026.
Joe, S., Woolley, M. E., Brown, G. K., Ghahramanlou-Holloway, M., & Beck, A. T. (2008). Psychometric properties of the Beck Depression Inventory-II in low-income African American suicide attempters. Journal of Personality Assessment, 90, 521–523. doi:10.1080/00223890802248919.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice, 10, 144–156. doi:10.1093/clipsy.bpg016.
Kiken, L. G., Garland, E. L., Bluth, K., Palsson, O. S., & Gaylord, S. A. (2015). From a state to a trait: trajectories of state mindfulness in meditation during intervention predict changes in trait mindfulness. Personality and Individual Differences, 81, 41–46. doi:10.1016/j.paid.2014.12.044.
Kline, R. B. (2010). Principles and practice of structural equation modeling (3rd ed.). New York: Guilford.
Kochanek, K. D., Arias, E., & Anderson, R. N. (2013). How did cause of death contribute to racial differences in life expectancy in the United States in 2010? (NCHS data brief, no 125). Hyattsville: National Center for Health Statistics.
Lerman, S. F., Shahar, G., & Rudich, Z. (2012). Self-criticism interacts with the affective component of pain to predict depressive symptoms in female patients. European Journal of Pain, 16, 115–122. doi:10.1016/j.ejpain.2011.05.007.
Lilja, J. L., Frodi-Lundgren, A., Hanse, J. J., Josefsson, T., Lundh, L.-G., Skold, C., et al. (2011). Five Facet Mindfulness Questionnaire—reliability and factor structure: a Swedish version. Cognitive Behaviour Therapy, 40, 291–303. doi:10.1080/16506073.2011.580367.
Lilja, J. L., Lundh, L.-G., Josefsson, T., & Falkenstrom, F. (2013). Observing as an essential facet of mindfulness: a comparison of FFMQ patterns in meditating and non-meditating individuals. Mindfulness, 4, 203–212. doi:10.1007/s12671-012-0111-8.
Linehan, M. M. (2015). DBT skills training manual (Second ed.). New York: The Guilford Press.
Muthen, L. K., & Muthen, B. O. (2012). Mplus user guide (7th ed.). Los Angeles: Muthen & Muthen.
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2, 223–250. doi:10.1080/15298860390209035.
Petrocchi, N., & Ottaviani, C. (2016). Mindfulness facets distinctively predict depressive symptoms after two years: the mediating role of rumination. Personality and Individual Differences, 83, 92–96. doi:10.1016/j.paid.2015.08.017.
Schmidt, F. L., Le, H., & Ilies, R. (2003). Beyond alpha: an empirical examination of the effects of different sources of measurement error on reliability estimates for measures of individual differences constructs. Psychological Methods, 8, 206–224. doi:10.1037/1082-989X.8.2.206.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford.
Serpa, J. G., Taylor, S. L., & Tillisch, K. (2014). Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Medical Care, 52, S19–S24. doi:10.1097/MLR.0000000000000202.
Smalley, S. L., Loo, S. K., Hale, S. H., Shrestha, A., & McGough, J. J. (2009). Mindfulness and attention deficit hyperactivity disorder. Journal of Clinical Psychology, 65, 1087–1098. doi:10.1002/jclp.20618.
Solem, S., Thunes, S. S., Hjemdal, O., Hagen, R., & Wells, A. (2015). A metacognitive perspective on mindfulness: an empirical investigation. BMC Psychology. doi:10.1186/s40359-015-0081-4.
Tabachnick, B. G., & Fidel, L. S. (2007). Using multivariate statistics (5th ed.). Boston: Pearson Education.
Thompson, R. S., & Zuroff, D. C. (2004). The Levels of Self-criticism Scale: comparative self-criticism and internalized self-criticism. Personality and Individual Differences, 36, 419–430. doi:10.1016/s0191-8869(03)00106-5.
Tucker, R.P., O’Keefe, V.M, Cole, A.B., Rhoades-Kerswill, S., Hollingsworth, D.W., Helle, A.C., et al., (2014). Mindfulness tempers the impact of personality on suicidal ideation. Personality and Individual Differences, 68, 229–233. doi:10.1016/j.paid.2014.05.001
Tran, U.S., Gluk, T.M, & Nader, I.W. (2013). Investigating the Five Facet Mindfulness Questionnaire (FFMQ): Construction of a short form and evidence of a two-factor higher order structure of mindfulness. Journal of Clinical Psychology, 69(9), 951–965. doi:10.1002/jclp.21996
Vallejo, Z., & Amaro, H. (2009). Adaptation of mindfulness based stress reduction program for addiction relapse prevention. The Humanistic Psychologist, 37, 192–206. doi:10.1080/08873260902892287.
Veehof, M. M., ten Klooster, P. M., Taal, E., Westerhof, G. J., & Bohlmeijer, E. T. (2011). Psychometric properties of the Dutch Five Facet Mindfulness Questionnaire (FFMQ) in patients with fibromyalgia. Clinical Rheumatology, 30, 1045–1054. doi:10.1007/s10067-011-1690-9.
Walach, H., Buchheld, N., Buttenmuller, V., Kleinknecht, N., & Schmidt, S. (2006). Measuring mindfulness—the Freiburg Mindfulness Inventory (FMI). Personality and Individual Differences, 40, 1543–1555. doi:10.1016/j.paid.2005.11.025.
Williams, D. R., Gonzalez, H. M., Neighbors, H. W., Nesse, R. M., Abelson, J. M., Sweetman, J., et al. (2007). Prevalence and distribution of major depressive disorder in African Americans, Carribean Blacks, and Non-Hispanic Whites: results from the National Survey of American Life. JAMA Psychiatry, 64, 305–315. doi:10.1001/archpsyc.64.3.305.
Williams, J. M. G., Duggan, D. S., Crane, C., & Fennell, J. V. (2008). Mindfulness-based cognitive therapy for prevention of recurrence of suicidal behavior. Journal of Clinical Psychology: In Session, 62, 201–210. doi:10.1002/jclp.20223.
Witkiewitz, K., Bowen, S., Douglas, H., & Hsu, S. H. (2013). Mindfulness-based relapse prevention for substance craving. Addictive Behaviors, 38, 1563–1571. doi:10.1016/j.addbeh.2012.04.001.
Wong, C.C.Y. & Mak, W.W.S. (2013). Differentiating the role of three self-compassion components in buffering cognitive-personality vulnerability to depression among Chinese in Hong Kong. Journal of Counseling Psychology, 60(1), 162–169. doi:10.1037/a0030451
Woods-Giscombé, C. L., & Black, A. R. (2010). Mind-body interventions to reduce risk for health disparities related to stress and strength among African American women: The potential of mindfulness-based stress reduction, loving-kindness, and the NTU therapeutic framework. Complementary Health Practice Review, 15, 115–131. doi:10.1177/1533210110386776.
Woods-Giscombé, C.L., & Gaylord, S.A. (2014). The cultural relevance of mindfulness meditation as a health intervention for African Americans: Implications for reducing stress-related health disparities. Journal of Holistic Nursing, 32(3), 147–160. doi:10.1177/0898010113519010
Worthington, R. L., & Whittaker, T. (2006). Scale development research: a content analysis and recommendations for best practices. The Counseling Psychologist, 34, 806–838. doi:10.1177/0011000006288127.
Zeidan, F., Martucci, K. T., Kraft, R. A., McHaffie, J. G., & Cognill, R. C. (2014). Neural correlates of mindfulness meditation-related anxiety relief. SCAN, 9, 751–759. doi:10.1093/scan/nst041.
Acknowledgments
This research was supported by a grant from the Emory University Research Council (Group interventions for Suicidal African American men and women)awarded to the last author. We appreciate the contributions of Bradley Goodnight and Martha Calamaras to this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
None of the authors have any conflicts of interest to report.
Rights and permissions
About this article
Cite this article
Watson-Singleton, N.N., Walker, J.H., LoParo, D. et al. Psychometric Evaluation of the Five Facet Mindfulness Questionnaire in a Clinical Sample of African Americans. Mindfulness 9, 312–324 (2018). https://doi.org/10.1007/s12671-017-0776-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-017-0776-0