Abstract
While various techniques for analyses of the bone/implant interface are developed, most of them do not show the osseointegration process in details. In this article, we present a new inverted approach to explore the osseointegration of the dental implants, based on the chemical deep etching of titanium implants. An approach was tested on 18 implants inserted in 6 dogs. Bone/implant blocks were taken after 1, 3, and 6 months after implantation. The titanium was chemically removed from the interface, leaving the bone tissue intact. Once metal was removed, bone tissue was analyzed macroscopically and with a scanning electron microscope, afterwards decalcified and used for histological analysis. The clear patterns of implant integration into the bone tissue were obtained after 1, 3, and 6 months after implantation. After 1 month, the bone/implant interface was still very immature. After 3 months, the bone was already quite mature and organized. After 6 months, the external bone layer on the bone/implant interface appeared in its final osseointegrated form. The presented inverted method for the osseointegration analysis offers new insight into the healing process of the bone/implant interface after implantation, as well as integrative processes occurring around implants with different surfaces and designs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The integration of the dental implants into the bone tissue and characteristics of the interface between bone and implant is one of the biggest challenges in dental and orthopedic implant research. Several different approaches to characterize the morphology of the implant osseointegration are known [1,2,3]. The first approach supposes to derive the intact bone-implant interface and prepare the cuts (lengthwise and transverse) of the “implant-bone” border zone [4,5,6]. The second technique is based on mechanical removal of the implant from the bone tissue, thereby damaging the interface [4, 7]. Each approach has its own disadvantages [8, 9]. For example, the bone tissue on the border with the implant is often damaged when obtaining bone sections with the implant and preparing cuts of teeth. This is also difficult to maintain the integrity of bone associated with the implant during their mechanical separation. As stronger the implant/bone connection is, as more damages of bone tissue will be occurred. Furthermore, it is impossible to save intact the shape and size of the bone contacting with the implant surface. Therefore, this method cannot be used for detailed investigation of the processes of bone formation around threaded implants [8, 9] and approaches should be improved. An advantageous approach is the computed tomography of the implant-bone interface [10].
Here, we suggest the deep etching approach based on the chemical removal of the implant from the bone leaving the shape and size of the bone tissue intact.
2 Materials and Methods
2.1 Experimental Animals
Six male mongrel dogs (> 2 years), weighting between 15 and 20 kg, were used in this study. The animals were kept in purpose-designed rooms and were fed and watered ad libitum with a standard diet. The study was approved by local research ethics committee (protocol 6, 07/26/2012) [4]. All surgery was performed in an operating room at the Kazan State Academy of Veterinary Medicine, Kazan, Russia.
2.2 The Experimental Model and Implants
The model of bone defect was developed 6 months prior of implants insertion. The dogs were anesthetized with an intramuscular injection of aminazine (1 ml) and xylazine hydrochloride 5 mg/kg, then propofole (0.6 ml/kg) was injected intravenously. A preoperative antibiotic (amoxicillin) was administered intramuscularly, and 1.8 ml of artikaine at 2% was used in the surgical area for conduction anesthesia. Two mandibular premolars were bilaterally extracted, the tooth cavities were left for healing and filling with the bone tissue for 6 months. Then, the implants were inserted into the bone bed of the removed premolars by using traditional technique.
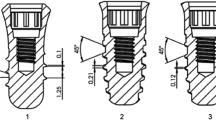
After 6 months after surgery, 18 dental implants of 3.25-mm diameter and 8.5-mm length (produced specially for the dogs from nanostructured titanium on Kazan medical instruments factory, Kazan, Russia) were inserted in the jaw sites with atrophied bone and analyzed after 1, 3, and 6 months of healing [11]. The animals were divided into three groups with 2 dogs in each according to the time between initial surgery and the bone-implant blocks removal. The bone blocks with the integrated implants were cut out after 1, 3, and 6 months (Fig. 1) and subjected to the deep etching. The jaw was recovered by using osseoconductive and asseoinductive materials and tooth implant establishment to provide normal life of the dog (see Fig. 2).
2.3 The Non-traumatic Removal of Implant from the Bone
The method consists in titanium removal without damaging of the bone. Each bone block containing an osseointegrated titanium implant was washed in phosphate buffer saline (PBS, рН 7.4) and placed into an etching solution (19.6% hydrofluoric acid, 8.9% metallic zinc, 71.5% ethylene glycol). The composition of the solution provides the complete removal of titanium from the bone tissue and implants. Titanium reacts readily with weak acids in the presence of complexing agents and become dissolved in 30 days. As a result, the implant disappears while the surrounding bone tissue remains intact [11]. The remaining bone tissue was further processed to remove the bone mineral component (decalcification) and used for long-term histological analysis.
2.4 Sample Processing and Analysis
After etching, the obtained bone samples were kept back for macroscopic evaluation and scanning electron microscopy (SEM). For the histological examination of the bone, samples were submerged in 10% formol solution for 24 h and then washed in running water for a further 24 h. After that, the samples were dehydrated in graded ethanol solutions from 70 to 100%, embedded in paraffin, and stained with hematoxylin/eosin solution or according to Van Gieson’s protocol [12].
3 Results
Healing of all surgeries went uneventful. Initially placed implants were clinically integrated with normal peri-implant tissue appearance until the bone-implant blocks were cut out. The implants were removed by the chemical etching and analyzed as described in Section 2.
The macroscopic examination after the removal of the implant using the method of deep etching by Mirgazizov [12] allowed characterizing the contours, surface, and volume of the bone tissue that contacted with the implant surface. A clear imprint of the implant screw in the bone tissue was observed on the third month (Fig. 3a), which is a characteristic feature of its osseointegration.
The macroscopic and scanning electron microscopy (SEM) analysis of the bone surface after etching and removal of the implant. The shape of the implant screw threads was clearly visible on the walls of the bone block, which indicated the osseointegration of the interface (a). SEM analysis of the bone tissue 1 (b), 3 (c), and 6 (d) months after the implantation
Then, the scanning electron microscopy of the bone blocks obtained after 1, 3, and 6 months of implantation was performed (Fig. 3b–d, respectively). One month after the implantation, the bone tissue started to follow the shape of implant threads. However, the “bone carving” at this time was still incomplete. In 3 months, the bone regeneration at the surface of the implant following the imprint of the screw pattern was observed (Fig. 3c), and in 6 months after the implantation, the bone tissue in the osseointegrated interfaces was homogenous and the bone interface was an exact imprint of the screw threads of implants.
The histological analysis of the samples demonstrated bone remodeling around the implant (Fig. 4 a). During the first month, there was a mature and fibrous connective tissue in the upper and middle segments of the implant (Fig. 4a). In the lower segment, a connective tissue and separate bone beams were observed (Fig. 4b). Three months after the implantation, a fibrous bone tissue similar to the screw threads was identified (Fig. 4c). Six months after the implantation, the bone tissue around the implant was organized as a mature lamellar bone with the clearly visible ridges on the upper margin along the entire surface of the implant (Fig. 4d).
Histological analysis of the bone tissue samples after 1, 3, and 6 months after the implantation, magnification × 400. (a) A mature fibrous connective tissue (Van Gieson staining). Upper and middle segments of the implant after 1 month of the experiment. b A connective tissue and separate bone beams. Lower segment of the implant after 1 month of the experiment (Van Gieson staining). c A fibrous bone tissue following the implant surface after 3 months of the experiment (Hematoxylin and eosin staining). d A mature lamellar bone with clear ridges on the inner line along the entire surface of the implant after 6 months of the experiment (hematoxylin and eosin staining)
4 Discussion
Despite of success in the clinical use of dental implants made of titanium and its alloys, the materials and designs of implants need to be improved [1, 14]. An important step is the optimization of the bone-implant interface and development of new surfaces and macrodesigns of implants that could enhance the process of osseointegration [1, 2, 15, 16]. In a broad sense, an interface is a border between interacting independent objects. From this perspective, this term “interface” is appropriate to describe dental implants interacting with the jaw bone, oral mucosa, abutments, prosthetic structures, as well as teeth surrounding the implant-supported rehabilitations, suggesting them to be more complex than the single implant/bone interface.
Since the development of the new implant surfaces and designs is an urgent problem in stomatology, the evaluation of the bone-implant interface parameters is widely describe [1,2,3]. While many methods to characterize their interfaces are already known including the in vitro analysis [1, 17,18,19], however, there are very few methods to evaluate this interface in vivo [1,2,3]. This is mainly implant torque removal (biomechanical evaluation of the bone/implant interface strength) [20] and histology with the help of undecalcified specific histological procedures [21]. Both systems are incomplete and need to be combined to achieve relevant conclusions [2]. On the other hand, the torque removal provides interesting data on the biomechanical characteristics of the interface, but the results are too statistically insignificant and the method does not allow investigating and understanding the reasons of the observed results [20]. The bone/implant undecalcified histological analysis is also limited by analytical relevance: the histological method for bone cutting allows obtaining 1 or 2 good histological slides for each analyzed implant [20]. This means that researchers can only observe one axis of the osseointegrated implants, while the osseointegration process may differ considerably from the implant periphery.
In order to analyze the osseointegration of the whole implant periphery, some researchers suggest using of non-destructive physical methods, such as synchrotron radiation [21] and microtomography [10, 22], to reconstruct the whole osseointegrated interface around the implant. However, these methods have their own limits related to the physical behavior of the implant material (in particular, its optical density). The artifacts are numerous and make it difficult to accurately analyze the whole interface [23].
It is always recommended to combine these various methods in order to improve the significance of any study on the bone/implant interface. Even if the dental surfaces of implants are widely covered in the literature, these data remain contradictory and difficult to interpret due to these technical limitations to investigation of the interface with quantitative analysis. However, even with the existing limits, these methods are needed to explore the characteristics of the interface parameters and to evaluate the reliability and efficiency. Studying these interfaces is also very important when making implants suitable for difficult clinical cases [24,25,26].
In this article, we introduce a new approach to studying the osseointegration of dental implants. This approach is based on deep etching of titanium-made implants [8, 12]. In this approach, titanium is chemically removed from the interface with the bone left intact. As the metal is removed, the decalcified bone tissue can be used for microscopic study. Using this method, we studied the integration of implants in the bone tissue for up to 6 months.
The results of this study illustrate the stages of osseointegration of threaded implants, as well as a new approach to analysis of this process. In this method of osseointegration, a threaded implant can be identified as at the stage when the entire space between the implant and the bone wall (in particular, the space between the threads) is filled with newly formed mature bone tissue, as well as when the bone tissue accurately imitates the geometry of the implant as the mirror image of the implant shape [26]. When osseointegration is achieved, an exact imprint of the implant design and continuous and compact external bone surface is observed.
Osseointegration was initially defined as an experimental observation of titanium ankylosis in bone [1]. In this study, we present a new concept for osseointegration of threaded implants as an experimental observation of the complete growth of bones and reconstruction along the bone/implant border. This approach remains relatively theoretical, since the most important parameter is clinical evaluation of the implant stability, which allows to load the implant with a crown and to make it fulfill its function.
In this study, the samples needed 6 months for complete osseointegration, i.e., for formation of a mature compact bone all over the implant during the osseointegration process. In this conceptual study, we used a simple threaded implant made of titanium to verify the main mechanisms of the analytical protocols, which was of interest for various shapes of surfaces [27], since all the available evaluations have been based on measurements of the rotational moment and analysis of the undecalcified bone integrated with the implant [21].
5 Conclusions
The experimental and morphological study of the integration of implants by the method of deep chemical etching by Mirgazizov [11] revealed the features of regeneration around the threaded implants and proved the fact of formation of a mature compact bone in the lower segment after 3 months of osseointegration and along the entire length of the implant after 6 months of this process. Furthermore, the investigations allowed considering the osseointegration of a threaded implant as a complete mirror image of the implant surface at the bone surface appearing as a result of the processes of bone formation. The proposed approach can be used for the clinical and morphological studies of any new materials used for implantation and offers new opportunities for researchers with regard to the use of other implant designs in both stomatology and other fields of medicine.
References
Dohan Ehrenfest, D. M., Coelho, P. G., Kang, B. S., Sul, Y. T., & Albrektsson, T. (2010). Classification of osseointegrated implant surfaces: materials, chemistry and topography. Trends in Biotechnology, 28(4), 198–206.
Coelho, P. G., Granjeiro, J. M., Romanos, G. E., Suzuki, M., Silva, N. R., Cardaropoli, G., Thompson, V. P., & Lemons, J. E. (2009). Basic research methods and current trends of dental implant surfaces. Journal of Biomedical Materials Research. Part B, Applied Biomaterials, 88(2), 579–596.
Coelho, P. G., Suzuki, M., Marin, C., Granato, R., Gil, L. F., Tovar, N., Jimbo, R., Neiva, R., & Bonfante, E. A. (2015). Osseointegration of plateau root form implants: unique healing pathway leading to Haversian-like long-term morphology. Advances in Experimental Medicine and Biology, 881, 111–128.
Mirgazizov, M. Z., Khafizov, R. G., Mirgazizov, R. M., Kolobov, I. R., Tsyplakov, D. E., Mirgazizov, A. M., & Khafizova, F. A. (2013). Experimental base for internal connection dental implants for two-step implantation. Stomatologiia (Mosk), 92(3), 4–8.
Calvo-Guirado, J. L., Satorres-Nieto, M., Aguilar-Salvatierra, A., Delgado-Ruiz, R. A., Maté-Sánchez de Val, J. E., Gargallo-Albiol, J., Gómez-Moreno, G., & Romanos, G. E. (2015). Influence of surface treatment on osseointegration of dental implants: histological, histomorphometric and radiological analysis in vivo. Clinical Oral Investigations, 19(2), 509–517.
Du, Z., Ivanovski, S., Hamlet, S. M., Feng, J. Q., & Xiao, Y. (2016). The ultrastructural relationship between osteocytes and dental implants following osseointegration. Clinical Implant Dentistry and Related Research, 18(2), 270–280.
Eroglu, C. N., Ertugrul, A. S., Eskitascioglu, M., & Eskitascioglu, G. (2016). Changes in the surface of bone and acid-etched and sandblasted implants following implantation and removal. European Journal of Dentistry, 10(1), 77–81.
Mirgazizov MZ, Hafizov RG, Mirgazizov AM, Mirgazizov RM, Hafizova FA, Zyplakov DE. (2013) Interfaces in osseointegrated dental implants and a new inverted approach to their microscopic and histological study. Inverted approach for implant interface analysis. POSEIDO, 1(3), 141–147
Mirgazizov MZ, Hafizov RG, Mirgazizov М. (1996) Endosseous implant and its installation. RF Patent 2135117.
Cai, W. X., Ma, L., Zheng, L. W., Kruse-Gujer, A., Stübinger, S., Lang, N. P., & Zwahlen, R. A. (2015). Influence of non-steroidal anti-inflammatory drugs (NSAIDs) on osseointegration of dental implants in rabbit calvaria. Clinical Oral Implants Research, 26(4), 478–483.
Payer, M., Lohberger, B., Strunk, D., Reich, K. M., Acham, S., & Jakse, N. (2014). Effects of directly autotransplanted tibial bone marrow aspirates on bone regeneration and osseointegration of dental implants. Clinical Oral Implants Research, 25, 468–474.
Mirgazizov MZ, Mirgazizov RM, Hafizova FA, Hafizov RG, Khairullin FA, Gunter VE, Zyplakov DE, Kozlova AK. (2009) The method of deep etching. RF Patent 2464646.
Bancroft, J. D., & Stevens, A. (1996). Theory and practice of histotechnological techniques (4th ed.). New York(NY): Churchill Livingstone.
Hafizov RG, Mirgazizov MZ, Hafizova FA, Khairullin FA, Aripov RA, Kozlova AK. (2009) Surgical punch-conductor for gingival regeneration around dental implants. RF Patent 92608.
Mirgazizov MZ, Hafizov RG, Mirgazizov RM. (1996) Dental implant and method of its installation. RF Patent 2135118.
Hafizov RG., Mirgazizov MZ, Hafizova FA, Zhitko AK, Hafizov RG, Mirgazizov RM. (2009) Single-phased mechanical active implant. RF Patent 86449.
Kang, B. S., Sul, Y. T., Oh, S. J., Lee, H. J., & Albrektsson, T. (2009). XPS, AES and SEM analysis of recent dental implants. Acta Biomaterialia, 5(6), 2222–2229.
Morra, M., Cassinelli, C., Bruzzone, G., Carpi, A., Di Santi, G., Giardino, R., & Fini, M. (2003). Surface chemistry effects of topographic modification of titanium dental implant surfaces: 1. Surface analysis. The International Journal of Oral & Maxillofacial Implants, 18(1), 40–45.
Cassinelli, C., Morra, M., Bruzzone, G., Carpi, A., Di Santi, G., Giardin, R., & Fini, M. (2003). Surface chemistry effects oftopographic modification of titanium dental implant surfaces: 2. In vitro experiments. The International Journal of Oral & Maxillofacial Implants, 18(1), 46–52.
Marin, C., Bonfante, E. A., Jeong, R., Granato, R., Giro, G., Suzuki, M., Heitz, C., & Coelho, P. G. (2013). Histologic and biomechanical evaluation of 2 resorbable-blasting media implant surfaces at early implantation times. The Journal of Oral Implantology, 39(4), 445–453.
Kang, B. S., Sul, Y. T., Johansson, C. B., Oh, S. J., Lee, H. J., & Albrektsson, T. (2012). The effect of calcium ion concentration on the bone response to oxidized titanium implants. Clinical Oral Implants Research, 23(6), 690–697.
Jung, H., Kim, H. J., Hong, S., Kim, K. D., Moon, H. S., Je, J. H., & Hwu, Y. (2003). Osseointegration assessment of dental implants using a synchrotron radiation imaging technique: a preliminary study. The International Journal of Oral & Maxillofacial Implants, 18(1), 121–126.
Park, Y. S., Yi, K. Y., Lee, I. S., & Jung, Y. C. (2005). Correlation between microtomography and histomorphometry for assessment of implant osseointegration. Clinical Oral Implants Research, 16(2), 156–160.
Song, J. W., Cha, J. Y., Bechtold, T. E., & Park, Y. C. (2013). Influence of peri-implant artifacts on bone morphometric analysis with micro-computed tomography. The International Journal of Oral & Maxillofacial Implants, 28(2), 519–525.
Bartov, M. S., Karyagina, A. S., Gromov, A. V., Mishina, D. M., Trunova, G. I., Sidorova, E. I., Andreeva, E. V., Donchenko, S. V., Mukhametov, F. F., Mukhametov, U. F., Mirgazizov, M. Z., Mirgazizov, A. M., Hafizov, R. G., Lunin, V. G., Filippova, N. E., & Ginsburg, A. P. (2012). Osteoplastic preparations of the new generation “GAMALANT” containing growth regeneration factors of bone tissue. Department of Traumatology and Orthopedics, 2, 21–25.
Mirgazizov MZ, Mirgazizov AM, Mirgazizov RM, Hafizov RG, Lunin VG, Karyagina-Zhulina AS, Kotnova AP, Sharapova NE, Tkachuk AP, Bartov MS, Ginsburg AP. (2012) The method of address delivery of the osteoplastic materials containing growth and regeneration factors of the bone tissue. RF Patent 2469676.
Dohan Ehrenfest, D. M., Vazquez, L., Park, Y. J., Sammartino, G., & Bernard, J. P. (2011). Identification card and codification of the chemical and morphological characteristics of 14 dental implant surfaces. The Journal of Oral Implantology, 37(5), 525–542.
Funding
We like to acknowledge the support of this work by the Russian Science Foundation (project No. 15-14-00046) and subsidy of the Russian Government to support the Program of competitive development of Kazan Federal University.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hafizova, F.A., Mirgazizov, R.M., Hafizov, R.G. et al. Exploring the Integration of Threaded Implants: the Chemical Deep Etching Approach. BioNanoSci. 8, 313–318 (2018). https://doi.org/10.1007/s12668-017-0468-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-017-0468-1