Abstract
Background
Confocal laser endomicroscopy (CLE) has a potential to make optical diagnosis of neoplastic polypoidal lesions and may replace traditional histology in the proposed “diagnose and discard approach”. The present study was planned to assess the accuracy of probe-based CLE in predicting histology of polypoidal lesions of gastrointestinal (GI) tract in vivo before their removal.
Methods
In this prospective single-centre study, patients with upper and/or lower GI polypoidal lesions were enrolled. After detection of polypoidal lesions with white light endoscopy, probe-based CLE examination was performed. Real-time and offline presumptive CLE diagnosis of polypoidal lesions was made as per Miami classification and was compared with histopathology as the gold standard.
Results
A total of 50 GI polyps from 50 patients (28 males) were assessed. The mean (±SD) size of polyps was 13.7 (± 8.5) mm. Most polyps were located at the cecum (24.0%) or stomach (24.0%). On histological examination, hyperplastic and adenomatous polyps, adenocarcinoma, and lipoma were seen in 54%, 26%, 18% and 2% patients, respectively. On comparison of real-time CLE examination with histopathology, 40 (83.3%) and 8 patients (16.7%) had concordant and discordant results, respectively. Two polyps were inconclusively diagnosed on CLE. On offline examination, concordance with histopathology was observed in 85.4% (n = 41) of polyps, which was marginally better than online examination, though the difference was not statistically significant (p = 0.45). On comparing the real-time and offline findings of CLE, concordance was found in 91.7% of the cases. Accuracy, sensitivity, specificity, positive and negative predictive values on real-time evaluation were 83.3%, 87.5%, 79.1%, 80.7%, and 86.3%, respectively.
Conclusion
CLE is a useful tool for prediction of histology to assess the polypoidal lesions of the GI tract, and it may avoid polypectomy at least in some patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.

Introduction
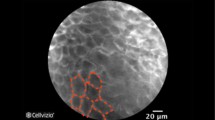
Recently, there has been an evolution in endoscopy from high-definition white light endoscopy and color enhancement methods to the novel optical technology known as “virtual biopsy”. Color enhancement methods include chromoendoscopy with topical dyes, narrow-band imaging (NBI) and similar technologies, autofluorescence endoscopy, Raman spectroscopy probes, and trimodal spectroscopy [1]. Some of these endoscopic techniques may predict histology (e.g. NBI can provide in vivo differentiation between neoplastic and non-neoplastic lesions and between low-grade and high-grade dysplasia on the basis of pit and vascular pattern characterization) [2,3,4,5,6,7]. Confocal laser endomicroscopy (CLE) is one of the recently emerging novel endoscopic modalities providing the endoscopist with a greater diagnostic option for optimizing the role of biopsy during gastrointestinal (GI) endoscopy. CLE obtains a very high magnification of the mucosal layer of the GI tract, and it has the potential to enable the histological diagnosis in real time at approximately 1000-fold magnification and a resolution of approximately 1 μm [8, 9]. At this level of resolution, visualization of GI mucosa including lamina propria, as well as individual cell is achievable with real-time acquisition speeds [10]. CLE has the potential to make optical diagnosis of neoplastic polypoidal lesions and may replace traditional histology in proposed “diagnose and discard approach”. In this proposed new approach, small polyps may be imaged, removed and then discarded without histological evaluation. It is also possible to leave non-neoplastic polyp in situ with consequent reduction in polypectomy-related costs and complications.
The present study was planned to assess the accuracy of probe-based CLE in predicting histology and to assess its ability to make an accurate and reliable histological diagnosis of polypoidal lesions of the GI tract in vivo before their removal.
Methods
This was a prospective observational single-centre study done from July 2015 to December 2016. This study was approved by the institutional review board. Adult patients (>18 years old) attending the outpatient clinic or admitted and undergoing upper and/or lower GI endoscopy and detected to have polypoidal lesions were enrolled in this study. Patients having bleeding diathesis, on antiplatelet or anticoagulants, pregnancy, and with history of allergy to fluorescein dye were excluded from the study. Before each procedure, informed consent was obtained. The patients undergoing upper GI endoscopy were made to fast for at least 6 h, whereas those for colonoscopy were prepared with standard doses of polyethylene glycol.
All examinations and procedures were performed by one experienced endoscopist. The white light high-definition endoscopy was used as the primary screening method. After the detection of lesion in the GI tract, its anatomical location was determined and its size was estimated based on comparison with a biopsy forceps (closed, 5 mm, or open, 9 mm). The morphological characteristics of the polypoidal lesions were recorded in accordance with the Paris classification system [11]. The CLE examination was performed by administering 2.5–5.0 mL of 10% fluorescein sodium, intravenously. Immediately after the fluorescein injection, the confocal probe was passed through the scope and confocal video images of the polypoidal lesion were obtained and recorded.
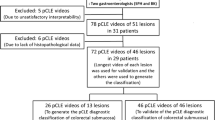
Good quality CLE videos of 2–5-min duration were acquired and subsequently, snare or biopsy forceps polypectomy of the lesion was performed. Polyp was sent for histopathological examination by an expert pathologist. The presumptive confocal diagnosis was made in real time during the procedure based on the established Miami classification [12]. Histopathological diagnosis was made according to the modified Vienna criteria [13, 14]. The pathologist was blinded to the CLE examination report . The CLE videos recorded during the procedure were then randomly distributed and reviewed “offline” by the same endoscopist at least 1 month after the procedure, to ensure blinding to histological diagnosis and endoscopic information recorded during the procedure. The histopathology diagnosis was used as a reference standard.
Statistical methods
Statistical analysis was performed with the help of Epi Info (Centres for Disease Control and Prevention, Atlanta, Georgia, USA). Descriptive analysis was performed to get a brief summary of the data. Chi-square test was used to find a significant association between categorical variables. Sensitivity, specificity, positive predictive values (PPV) and negative predictive values (NPV) were calculated. P-value less than 0.05 was considered statistically significant.
Results
From July 2015 to December 2016, 50 patients (28 males, 56%) with 50 GI polyps were recruited in this study. The median age of patients was 58 years (range 30–79 years). Abdominal discomfort (40%) was the commonest symptom, followed by flatulence (28.0%), bleeding per rectum (22%) and dyspepsia (10%). Family history of GI cancer was present in 6 patients (12%). The mean (±SD) size of polyps was 13.7 ± 8.5 mm with a median value of 10 mm (range 5–45 mm). Polyp size of ≥ 10 mm was found in 62.0% of the polyps, and the rest were between 5 and 9 mm. Table 1 shows the location and histological diagnosis of the polyps. None of the patients experienced any complication either due to endoscopic polypectomy or sedation.
On CLE examination, hyperplastic polyp (Fig. 1), adenomatous polyp (Fig. 2) and adenocarcinoma (Fig. 3) were noted in 56%, 26% and 14% of polyps, respectively. Two polyps (4%) showed inconclusive results on CLE examination, one of these turned out to be a lipoma and the other an adenoma. CLE images were not optimum in the second case. Table 2 shows the comparison of real-time and offline CLE examination with histopathology. On offline examination, concordance with histopathology was observed in 85.4% (n = 41) of polyps, which was marginally better than online examination though the difference was not statistically significant. On comparing the real-time and offline findings of CLE, concordance was found in 91.7% (n = 44) of the polyps. Table 3 shows the comparison of sensitivity, specificity, PPV, NPV and accuracy of real-time and offline CLE examinations with histopathology as the gold standard.
Discussion
In this single-centre study, we compared histology assessed by probe-based CLE of GI polypoidal lesions with gold standard histopathology. In the present study, when real-time CLE classification of polypoidal lesions was compared with histopathology, we found that 83.3% polyps had concordant results with histopathology with an overall sensitivity of 87.5%, specificity of 79.1% and overall diagnostic accuracy of 83.3%. Our results are comparable to those in the study by Shahid et al. [15] who used probe-based CLE that had a sensitivity of 86%, specificity of 78% and overall accuracy of 82% for the prediction of histopathology. Kiesslich et al. [16] published the use of CLE during ongoing colonoscopy in which they found endoscopy-based confocal endomicroscopy (eCLE) had an accuracy of 99% with a sensitivity of 97% and specificity of 99% in diagnosing intra-epithelial neoplasia and colorectal carcinoma. Similarly, Hurlstone et al. [17] demonstrated a sensitivity of 97.4%, specificity of 97.4% and overall accuracy of 99% in diagnosing intra-epithelial neoplasia using eCLE. A relatively lower sensitivity, specificity and diagnostic accuracy were observed in our study as compared with the previous studies by Kiesslich et al. [16] and Hurlstone et al. [17] in predicting neoplastic and non-neoplastic polypoidal lesions. This difference might be attributed to different systems of CLE used (endoscopic vs. probe-based). There are several advantages and disadvantages between the two confocal systems. eCLE has slightly higher lateral resolution (7 vs.1 μm) and higher ability to scan in the vertical axis perpendicular to the surface. On the other hand, probe-based CLE has the ability to acquire images more rapidly (12 per second vs. 0.8 per second) and is more easily adapted to practice since the probe can be passed through the accessory channel of any standard endoscope.
In present study, we also did an offline CLE analysis of GI polypoidal lesions, which showed a sensitivity of 85%, specificity of 85.7% and diagnostic accuracy of 85.4% as compared with histopathology, which is in accordance with the result of a previous study [15]. In present study, the specificity and diagnostic accuracy increased from 79.1% to 85.7% and 83.3% to 85.4% when analysis was done offline. This can be explained by the fact that in offline analysis the reviewer can scroll back and can freeze the images and also review individual frames which is difficult in real-time analysis because of time constraints and relative difficulty in holding the CLE probe at the proper position on small polyps. The classification of polypoidal lesions into neoplastic and non-neoplastic polyps by Miami classification both by real-time and offline CLE analysis were concordant in 91.7% as compared with histopathology. It indicates that endoscopist can do in vivo analysis of the polypoidal lesions of the GI tract with a high degree of accuracy and may take decision about whether to resect or leave the polyp in situ on the table. Our study was limited by the relatively small sample size and heterogeneity of data as it included polyps from both upper and lower GI systems. Also, two polyps were excluded from our analysis. One of these turned out to be a lipoma for which no standard CLE classification exists, and the other was an adenoma whose CLE images were not optimum.
Our study demonstrated that CLE can be a useful tool to evaluate GI polypoidal lesions during esophagogastroduodenoscopy or colonoscopy and can allow the endoscopist to do in vivo histological examination of the GI polypoidal lesions. CLE system has high sensitivity and specificity to differentiate polypoidal lesions into neoplastic and non-neoplastic types by analyzing the cellular and architectural features with magnification and resolution similar to that of ex vivo histopathology. CLE evaluation can be a very effective tool during ongoing upper GI endoscopy and colonoscopy to decide about whether to resect and discard a neoplastic polyp without sending it for histopathological examination. This strategy, if validated, can decrease the burden on pathologist and likely to result in cost saving. It is also possible to leave the non-neoplastic polyp in situ to circumvent the complications of polypectomy as proposed by the American Society for Gastrointestinal Endoscopy (ASGE) for the management of diminutive polyps [18]. However, in the future, CLE needs further studies on large number of patients in order to replace histopathology as a diagnostic tool for the evaluation of GI polypoidal lesions.
We conclude that CLE is a useful tool for the prediction of histology during ongoing esophagoduodenoscopy and colonoscopy and should be used to assess the polypoidal lesions of the GI tract. It may avoid polypectomy wherever possible. In vivo CLE evaluation of polypoidal lesions of the GI tract may help endoscopist to take on table decisions whether to resect and discard the polyp or to leave the polyp in situ.
References
Meining A, Saur D, Bajbouj M, et al. In vivo histopathology for detection of gastrointestinal neoplasia with a portable, confocal miniprobe an examiner blinded analysis. Clin Gastroenterol Hepatol. 2007;5:1261–7.
Pohl J, Nguyen-Tat M, Pech O, May A, Rabenstein T, Ell C. Computed virtual chromoendoscopy for classification of small colorectal lesions: a prospective comparative study. Am J Gastroenterol. 2008;10:562–9.
Rex DK. Narrow-band imaging without optical magnification for histologic analysis of colorectal polyps. Gastroenterology. 2009;136:1174–81.
Rex DK, Helbig CC. High yields of small and flat adenomas with high-definition colonoscopes using either white light or narrow band imaging. Gastroenterology. 2007;133:42–7.
Togashi K, Konishi F, Ishizuka T, Sato T, Senba S, Kanazawa K. Efficacy of magnifying endoscopy in the differential diagnosis of neoplastic and non-neoplastic polyps of the large bowel. Dis Colon Rectum. 1999;42:1602–8.
Tung SY, Wu CS, Su MY. Magnifying colonoscopy in differentiating neoplastic from non-neoplastic colorectal lesions. Am J Gastroenterol. 2001;96:2628–32.
Ignjatovic A, East JE, Suzuki N, Vance M, Guenther T, Saunders BP. Optical diagnosis of small colorectal polyps at routine colonoscopy (Detect InSpect ChAracterise Resect and Discard; DISCARD trial): a prospective cohort study. Lancet Oncol. 2009;10:1171–8.
Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy. 2004;36:1094–8.
Chauhan SS, Dayyeh BK, Bhat YM, Gottlieb KT, Hwang JH, Komanduri S. Confocal laser endomicroscopy. Gastrointest Endosc. 2014;80:928–38.
Shieh FK, Drumm H, Nathanson MH, Jamidar PA. High-definition confocal endomicroscopy of the common bile duct. J Clin Gastroenterol. 2012;46:401–6.
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December1, 2002. Gastrointest Endosc 2003;58 Suppl:S3–43.
Wallace M, Lauwers GY, Chen Y, et al. Miami classification for probe-based confocal laser endomicroscopy. Endoscopy. 2011 43:882–91.
Schlemper RJ, Riddell RH, Kato Y, et al. The Vienna classification of gastrointestinal epithelial neoplasia. Gut. 2000;47:251–5.
Rubio CA, Nesi G, Messerini L, et al. The Vienna classification applied to colorectal adenomas. J Gastroenterol Hepatol. 2006;21:1697–703.
Shahid MW, Buchner AM, Heckman MG, et al. Diagnostic accuracy of probe-based confocal laser endomicroscopy and narrow band imaging for small colorectal polyps: a feasibility study. Am J Gastroenterol. 2012;107:231–9.
Kiesslich R, Burg J, Vieth M, et al. Confocal laser endoscopy for diagnosing intraepithelial neoplasias and colorectal cancer in vivo. Gastroenterology. 2004;127:706–13.
Hurlstone DP, Baraza W, Brown S, Thomson M, Tiffin N, Cross SS. In vivo real-time confocal laser scanning endomicroscopic colonoscopy for the detection and characterization of colorectal neoplasia. Br J Surg. 2008;95:636–45.
Rex DK, Kahi C, O’Brien M, et al. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2011;7:419–22.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PAS, BBS, VKR, EK, and MKG declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shah, P.A., Shah, B.B., Rai, V.K. et al. A study on confocal endomicroscopy in comparison with histopathology for polypoidal lesions of the gastrointestinal tract: A prospective single-centre experience. Indian J Gastroenterol 38, 332–337 (2019). https://doi.org/10.1007/s12664-019-00973-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-019-00973-4