Abstract
Background
The aim of this pilot study is to investigate the diagnostic yield of probe-based confocal laser endomicroscopy (pCLE) in the evaluation of depth of invasion in colorectal lesions.
Methods
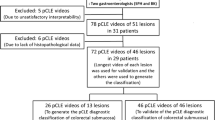
Patients with colorectal lesions eligible for either endoscopic treatment or surgery were enrolled in the study. Tumor’s depth of invasion was classified as mucosal or slight submucosal (M-SM1) and deep submucosal invasion or deeper (SM2 or deeper). White light endoscopy (WLE), magnifying narrow band imaging (M-NBI), and magnifying chromoendoscopy (M-CE) were used to assess colorectal lesions, and pCLE was used to identify tumor’s features related to SM2 or deeper. The diagnostic classification of depth of invasion was obtained by correlating pCLE findings with histology results (on-site diagnosis). All colorectal lesions were stratified by a second endoscopist who was blinded to any clinical and histological information with the use of WLE, M-NBI, M-CE, and pCLE (off-line review).
Results
A total of 22 colorectal lesions were analyzed: seven were adenoma, ten intramucosal cancer, and five SM2 or deeper cancer. With respect to pCLE findings, loss of crypt structure was seen in all SM2 or deeper cancers and only in one M-SM1 lesion. Sensitivity, specificity, and accuracy of WLE, M-NBI, and M-CE in off-line review were 60/94/86, 60/94/86, and 80/94/91%, respectively. Sensitivity/specificity/accuracy of pCLE in off-line review were 80/94/91%, respectively. The inter-observer agreement of pCLE between on-site diagnosis and off-line review was 0.64 (95%CI 0.27–1.0).
Conclusions
pCLE may represent a useful tool to evaluate the depth of invasion in colorectal lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endoscopic resection is commonly used to remove colorectal neoplasms with a negligible risk of lymph node metastasis. Specifically, endoscopic submucosal dissection (ESD) was developed in order to allow the en bloc resection of gastrointestinal (GI) lesions regardless of their shape and size. Because of such possibility to remove lesions in one piece, ESD has been shown to be associated to a low recurrence rate and to facilitate a precise histological assessment of the resected specimen [1,2,3]. It is well-known in literature that colorectal cancers confined to the intramucosal layer or invading less than 1000 μm of the submucosa, with no lymphovascular involvement or poor differentiated histology, have a negligible risk of lymph node metastasis [4]. Guidelines for the treatment of colorectal lesions suggested endoscopic resection as the treatment of choice for intramucosal carcinoma or carcinoma with slight submucosal invasion (≤ 1000 μm) (M-SM1) [2, 5, 6]. Surgery with lymph node dissection is instead recommended for submucosal deep invasive cancers (> 1000 μm) or deeper (SM2 or deeper), given the risk of lymph node metastasis. Therefore, the evaluation of tumor’s depth of invasion is of main importance to select the best treatment option.
In the last years, advanced imaging techniques have been developed to facilitate the evaluation of lesions’ depth of invasion [7]. In particular, magnifying crystal violet crhomoendoscopy (M-CE) with mucosal pit pattern diagnosis and magnifying narrow band imaging (M-NBI) have been shown to be very helpful in evaluating lesions’ depth of invasion [8,9,10]. However, such techniques, as well as full-zoom endoscopes, are not widely used yet, especially in Western countries.
Probe-based confocal laser endomicroscopy (pCLE) is a new technique for real-time, in vivo high-resolution evaluation of GI mucosa at a cellular level. There are a few data in literature on pCLE use and its feasibility, safety, and reliability in differentiating non-neoplastic from neoplastic colorectal lesions [11, 12]. We believe that pCLE may be helpful to predict tumor’s depth of invasion in colorectal lesions and an alternative modality of M-CE and M-NBI. For this reason, we carried on this pilot study with the aim to assess the diagnostic yield of pCLE for colorectal tumors (UMIN000016557).
Material and methods
Patients
Patients with colorectal lesions eligible for either endoscopic treatment or surgery and referred to two cancer centers were enrolled in the study. Inclusion criteria were as follows: age between 20 and 79 years, ECOG performance status 0–2, white blood cell ≥ 3000/mm3, hemoglobin ≥ 8.0 g/dl, platelet ≥ 100,000/μl, aspartate aminotransferase ≤ 100 IU/l, alanine aminotransferase ≤ 100 IU, creatinine ≤ 1.5 mg/dl. Patients allergic to fluorescein or with contraindications to its intravenous administration and patients who could not stop antithrombotic therapy according to Japanese guidelines on antithrombotic treatment were excluded from the study [13].
On-site diagnosis
Bowel preparation was obtained with 2–3 l of polyethylene glycol-electrolyte solution administered orally early morning on the day of the procedure.
Prior to examination, scopolamine butylbromide (10 mg) or glucagon (0.5 mg) was administered intravenously in patients with no contraindication to these drugs, in order to reduce bowel peristalsis. Expert endoscopists (Y.S. and Y.O.), who had performed > 5000 colonoscopies but with little experience in pCLE, as they had never used it before, carried out all the procedures. A video endoscope system (EVIS LUCERA SPECTRUM; Olympus, Optical Co., Ltd., Tokyo, Japan) and full-zoom colonoscopes (PCF-Q260AZI, CF-H260AZI, Olympus, Optical Co., Ltd., Tokyo, Japan) were used in this study. When a lesion was found, its depth of invasion was initially assessed with white light endoscopy (WLE) and classified as M-SM1 or SM2 or deeper, according to endoscopic features [9]. Regions of interest, such as depression, large nodules, or reddened areas, were accurately assessed as well [8]. M-NBI was subsequently used on the region of interest or the center of the lesion to evaluate blood vessel and surface pattern, in order to estimate the depth of invasion according to Sano’s classification (CP-I: non-neoplastic, CP-II: adenomatous polyp, CP-IIIA: intramucosal or superficial submucosal invasive cancer, CP-IIIB: deep submucosal invasive cancer). CP-II and IIIA lesions corresponded to M-SM1 and CP-IIIB to SM2 or deeper [10]. After M-NBI analysis, M-CE with crystal violet staining was used to evaluate pit pattern and to estimate the depth of invasion according to the clinical classification of pit pattern (non-invasive pattern: M-SM1; invasive pattern: SM2 or deeper) [8]. pCLE was used after WLE, M-NBI, and M-CE assessment. In particular, we used a pCLE system (Cellvizio; Mauna Kea Technologies, Paris, France) together with a 2.5-mm diameter (GastroFlex-UHD probe (Mauna Kea Technologies)). This probe can be used through the accessory channel of any standard colonoscope and has a field of view of 240 μm. The probe was advanced through the working channel and then fully apposed to the region of interest after intravenous administration of fluorescein. Image scans were obtained at a rate of 12 frames per second. As the endoscopists had never used pCLE before, prior to the start of this study, they completed a web-based diagnostic tutorial on pCLE image interpretation (http://www.cellvizio.net/learn/image-interpretation). In vivo pCLE analysis included an initial intravenous administration of 2.5 ml of 10% fluorescein sodium solution (Alcon Parma, Tokyo, Japan). Soon after fluorescein injection, the confocal probe was advanced through the working channel and then applied to the region of interest previously evaluated with M-NBI and M-CE. The pCLE examination was video-recorded. pCLE findings were divided into two categories—crypt findings (round/slit/stellate opening/villiform/irregular/lack of structure) and epithelial findings (uniform/irregular/dark/thickened; more than one finding could be found in the same lesion)—and were classified according to Miami classification [14]. Moreover, an expert endoscopist (Y.S.) proposed a diagnostic classification of tumor’s depth of invasion by correlating pCLE findings with histological results.
Off-line review
An off-line review was performed for all colorectal lesions by a second endoscopist, who was blinded to any clinical and histological information (S.A.). The endoscopist was not also informed which treatment was performed for any lesions. Prior to the start of the study, this endoscopist completed the web-based diagnostic tutorial on pCLE image interpretation, as mentioned before.
Lesions were assessed with WLE, M-NBI, and M-CE in the same order, and depth of invasion was evaluated by using each imaging technique. The video of pCLE analysis was available to be reviewed, in order to evaluate microsurface and microvascular pattern and, therefore, to estimate tumor’s depth of invasion according to diagnostic classification. The second endoscopist was allowed to watch the video as many times as needed.
Histology
All neoplastic lesions were removed either with endoscopic treatment or surgery according to the endoscopist’s decision during the on-site diagnosis. The resected specimens were retrieved, fixed in 10% buffered formalin solution and examined by expert pathologists with the use of hematoxylin and eosin staining. Lesions removed endoscopically were serially sectioned at 2–3-mm intervals, while lesions removed with surgery at 4–5-mm intervals. The histological classification was done according to the Japanese Classification of Colorectal Carcinoma [15]. According to depth of invasion, lesions were classified as adenoma, intramucosal carcinoma, or superficial submucosal invasive carcinoma (≤ 1000 μm from muscularis mucosae) (pM-SM1), or deep submucosal invasive carcinoma (> 1000 μm) or deeper (pSM2 or deeper). Depth of submucosal invasion was measured from the lowest part of muscularis mucosae to the deepest area of invasion [16]. If muscularis mucosae was difficult to identify because of tumor invasion, depth of invasion was measured starting from tumor’s surface. Pedunculated lesions were classified according to modified Haggitt’s classification [16]. Pedunculated lesions with head invasion were classified as SM1, and those with stalk invasion as SM2. Intramucosal cancer corresponds to high-grade dysplasia according to the Japanese classification and to mucosal high-grade neoplasia according to the World Health Organization and revised Vienna classification [17, 18].
Statistical analysis
Continuous variables were expressed as medians and ranges, and categorical variables were expressed as numbers and frequencies. This study evaluated the sensitivity, specificity, and accuracy of each of the aforesaid endoscopic imaging techniques in on-site diagnosis and off-line review for the evaluation of tumor’s depth of invasion. Inter-observer agreement for pCLE findings between on-site diagnosis and off-line review was analyzed by using the kappa test. Statistical analyses were performed with EZR version 1.27 (Saitama Medical Center, Jichi Medical University, Japan) [19].
Results
A total of 24 lesions found in 21 patients were analyzed. Histology showed that 22 out of 24 lesions had neoplastic features: 7 adenomas, 10 mucosal cancers, 4 deep submucosal invasive cancers, and 1 deeper cancer invading to muscularis propria. No superficial submucosal invasive cancer was found. Seventeen lesions were classified as pM-SM1 and five were pSM2 or deeper. The median size of the 22 neoplastic lesions was 25 mm (range 3–60 mm) (Table 1). The remaining two lesions were non-neoplastic polyps and were therefore excluded from the study.
With respect to the on-site diagnosis, the sensitivity, specificity, and accuracy of WLE, M-NBI, and M-CE were 100/94/95, 100/100/100, and 100/100/100%, respectively (Table 2). A score was assigned to each pCLE finding, according to histology examination (Table 3). Loss of crypt structure was common in SM2 or deeper (5/5) (Fig. 1) and rare in M-SM1 (1/17) (Fig. 2). There was little correlation between the epithelial pattern and histology. Epithelial thickening and loss of crypt structure were identified in three out of five SM2 or deeper cancers. Initially, we wanted to evaluate also blood vessels pattern, but as it was difficult to recognize and to interpret in many of the lesions, we decided not to consider it for tumor’s analysis. Therefore, loss of crypt structure was chosen as the pCLE finding indicative of SM2 or deeper in on-site diagnosis. For lesions with loss of crypt structure classified as SM2 or deeper according to histology classification, pCLE in on-site diagnosis showed a sensitivity, specificity, and accuracy of 100, 94, and 95%, respectively.
a WLE showing a reddish depressed lesion with thickened and elevated margins in the lower rectum. The depressed area was selected as region of interest. b M-NBI showing avascular surface, classified as Type IIIB according to Sano’s classification. c M-CE with crystal violet staining showing irregular and distorted pit pattern in the depressed area, which was classified as Vi invasive pattern. d pCLE showing loss of structure in the region of interest. e Histological analysis of the resected specimen (removed with surgery) showing deep submucosal invasive adenocarcinoma (2000 μm from the surface)
a Flat elevated lesion located in the rectosigmoid colon. The slightly depressed area on the distal side was selected as region of interest. b M-NBI showing irregular vascular pattern with mesh-like structures. These findings were classified as Type IIIA according to Sano’s classification. c M-CE with crystal violet staining showing irregular arrangement and size of pit pattern. These findings were classified as Vi non-invasive according to pit pattern classification. d pCLE analysis showing irregular structures with dark epithelium. e Histological analysis of the resected specimen (removed with ESD) showing well-differentiated tubular adenocarcinoma confined to mucosal layer
Sensitivity, specificity, and accuracy of WLE, M-NBI, and M-CE in off-line review were 60/94/86, 60/94/86, and 80/94/91%, respectively. Sensitivity, specificity, and accuracy of pCLE in off-line review were 80, 94, and 91%, respectively (Table 4). The inter-observer agreement of pCLE between on-site diagnosis and off-line review was 0.64 (95% confidence interval 0.27–1.0). No adverse event associated with intravenous fluorescein administration was reported.
Discussions
The aim of this pilot study was to describe our initial experience with pCLE for the diagnosis of depth of invasion in colorectal lesions. On-site analysis identified loss of crypt structure as the pCLE finding indicative of SM2 or deeper. Based on this finding, a simple pCLE classification for the diagnosis of tumor’s depth of invasion was proposed. Moreover, the diagnostic performance of pCLE for the evaluation of depth of invasion was validated by off-line review, with good inter-observer agreement (kappa value = 0.64). Even though the endoscopists who performed the procedures had little experience with pCLE in on-site diagnosis and off-line review, this study showed that pCLE could be useful to predict the depth of invasion in colorectal neoplasms and, thus, it may help in choosing the best treatment option.
Magnifying image-enhanced endoscopy was developed in order to allow an accurate evaluation of histology type and depth of invasion in colorectal tumors. M-NBI was shown to be able not only to differentiate between non-neoplastic and neoplastic lesions but also to estimate the depth of invasion in neoplastic polyps [20, 21]. NBI has been shown to have 84.8% sensitivity, 88.7% specificity, and 87.7% accuracy in differentiating between SM1 and SM2, according to Sano’s classification. Although there are many classifications based on M-NBI, the Japan NBI Expert Team (JNET) has recently proposed a universal classification for colorectal tumors (JNET classification), which was not published yet when we started this pilot study [10]. In our study, we were able to accurately estimate tumor’s depth of invasion through pit pattern analysis, as it has been already done in previous studies [22]. Matsuda et al. showed that sensitivity, specificity, and diagnostic accuracy of M-CE in differentiating between M-SM1 and SM2 lesions were 85.6, 99.4, and 98.8%, respectively [8]. In Japan, pit pattern analysis with CE is considered as a standard method to predict the depth of invasion, and M-NBI is an alternative option [10, 23, 24]. Both these diagnostic techniques require a full-zoom magnifying colonoscope, which has the capability to magnify the endoscopic view up to 100 times. In the Western countries, this kind of endoscope is rarely used and there are also technical limitations in the use of magnifying endoscopy, mainly with respect to the ability to focus on a target lesion and take pictures, as the majority of endoscopists did not have a specific training. Some studies in literature analyzed the learning curve for magnifying endoscopy in colorectal polyps assessment, but most of them were image interpretation studies using images taken by expert endoscopists [25].
pCLE is an advanced imaging technique which allows for the in vivo visualization of the mucosal layer and subcellular structures in the GI tract. The flexible miniprobe has a diameter of 2.5 mm and can be advanced through the working channel of any colonoscope. Moreover, the confocal system allows the in vivo visualization of microscopic cellular structure at 60 μm from the surface, without the need of adjusting the focus. This is done by simply apposing the probe to the epithelium, as the pinhole filter inside the probe cuts the fluorescent light out-of-the-focus. Some studies showed that pCLE is an easy-to-learn and promising diagnostic new method for in vivo analysis of colorectal polyps and inflammatory bowel diseases (IBD) [11, 26]. Our study supported the idea that the learning period for the use of pCLE was short.
In 2004, Kiesslich et al. classified colorectal tissue into normal, regenerative, and neoplastic, and compared these subtypes with the underlying pathological diagnosis [27]. However, this classification was not helpful in treatment strategy decision. A classification system for normal and pathological states in the GI tract using pCLE was proposed during a meeting held in Miami, Florida, in 2009 (Miami classification), and is now widely accepted [14]. Even though this classification could be very helpful to predict histology type of the lesion, since three to four pCLE findings per GI disease were proposed, it was unclear which one was the most indicative of tumor’s depth of invasion. With our study, we showed that loss of crypt structure was the most significant pCLE feature associated to SM2 or deeper cancer. We believe that loss of crypt structure may represent the atypia indicative of invasive cancer in pCLE analysis, similarly to VI or VN pit pattern in the pit pattern diagnosis. Endocytoscopy was recently developed to allow the analysis of mucosal structures at a cellular level. A target is stained with an absorptive contrast agent (methylene blue for cell nucleus, crystal violet for cell cytoplasm and glands ducts), and then particular lens are used to collect highly magnified images up to 450 times in order to visualize subcellular structures. Kudo et al. proposed an endocytoscopic (EC) classification and reported that the EC3b category, characterized by unclear gland formation and agglomeration of distorted nuclei, was indicative of SM2 or deeper invasive lesions [28]. Endocytoscopy allows the diagnosis of tumor’s depth of invasion through the evaluation of nuclear morphology, which is not possible with pCLE. However, endoscytoscopy requires a longer learning period in order to acquire the ability to focus on a target lesion and take pictures compared to pCLE.
To our best knowledge, there is only one study in literature on the evaluation of depth of invasion in colorectal lesions with pCLE. This study by Kim et al. classified colorectal submucosal findings as negative or indicative of carcinoma infiltration, and blood vessels pattern was rarely mentioned. In this study, submucosal carcinoma infiltration seen with pCLE was associated to dark and irregular nests of cells with irregular architecture and little or no mucin. Based on rates of correlation with pathological findings, the sensitivity, specificity, and accuracy of the submucosal carcinoma infiltration classification were 91.7, 86.8, and 88.0%, respectively [29]. However, it was not sure whether the aforesaid findings were really associated to submucosal invasion, as pCLE allows the visualization of cellular structure up to 60 μm from the epithelial surface, which means that confocal laser beam could not reach the submucosal layer.
As mentioned above, although the sufficient diagnostic performance of M-CE was already shown in several studies, these advanced image modalities were not commonly used due to the limited availability and use of a full-zoom endoscope and crystal violet staining, and the technical limitations in the use of magnifying endoscopy, especially in the West. Thus, it was hard to say that M-CE was a global standard method to predict the depth of invasion in colorectal neoplasms. In addition to C-CE, M-NBI could not also be an alternative modality due to the limited availability and use of a full-zoom colonoscope. On the other hand, pCLE is applicable for any colonoscope and allows for easier use without long training period compared with M-CE and M-NBI. Additionally, pCLE is more commonly available than full-zoom endoscope in the West. Therefore, we believed that pCLE was a good alternative option. Further randomized controlled trials are warranted to compare the diagnostic performance amongst M-CE, M-NBI, and pCLE. Furthermore, pCLE is applicable for functional imaging and molecular imaging of colorectal disease in future which we will not be able to develop using currently available magnifying endoscopy. Thus, we need to introduce standard pCLE use in Japan before the introduction of advanced imaging technology [30, 31].
Our study has some limitations. Firstly, there was a potential carryover effect due to other imaging techniques. Indeed, pCLE analysis was inevitably affected by WLE, M-NBI, and M-CE results. The region of interest was examined with WLE first, followed by M-CE and M-NBI; moreover, during pCLE examination, the probe was kept in contact with lesion’s surface, and this made the acquisition of good quality M-NBI and M-CE pictures difficult. Secondly, blood vessels architecture was not analyzed, as it was not visible many of the time. Loss of crypt structure alone may represent a helpful finding to predict the depth of invasion when analyzing target regions with pCLE, but the combination of blood vessels and cellular structures analysis may provide better diagnostic outcomes. Thirdly, SM1 lesions eligible for endoscopic treatment could not be included in the study.
In conclusion, pCLE may represent a useful tool for estimating the depth of invasion in colorectal lesions. Large-scale, multicenter, prospective clinical studies are needed to further evaluate the clinical impact of such technology for the assessment of GI lesions. We will continue to use pCLE analysis in order to collect more data, which could possibly support the use of intravenous fluorescein in Japan in the next future.
References
Saito Y, Uraoka T, Yamaguchi Y, Hotta K, Sakamoto N, Ikematsu H, Fukuzawa M, Kobayashi N, Nasu J, Michida T, Yoshida S, Ikehara H, Otake Y, Nakajima T, Matsuda T, Saito D (2010) A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 72:1217–1225. https://doi.org/10.1016/j.gie.2010.08.004
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH (2015) Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 47:829–854. https://doi.org/10.1055/s-0034-1392882
Oka S, Tanaka S, Saito Y, Iishi H, Kudo SE, Ikematsu H, Igarashi M, Saitoh Y, Inoue Y, Kobayashi K, Hisabe T, Tsuruta O, Sano Y, Yamano H, Shimizu S, Yahagi N, Watanabe T, Nakamura H, Fujii T, Ishikawa H, Sugihara K (2015) Local recurrence after endoscopic resection for large colorectal neoplasia: a multicenter prospective study in Japan. Am J Gastroenterol 110:697–707. https://doi.org/10.1038/ajg.2015.96
Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, Iwashita A, Ajioka Y, Watanabe H, Watanabe T, Muto T, Nagasako K (2004) Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol 39:534–543. https://doi.org/10.1007/s00535-004-1339-4
Tanaka S, Kashida H, Saito Y, Yahagi N, Yamano H, Saito S, Hisabe T, Yao T, Watanabe M, Yoshida M, Kudo SE, Tsuruta O, Sugihara K, Watanabe T, Saitoh Y, Igarashi M, Toyonaga T, Ajioka Y, Ichinose M, Matsui T, Sugita A, Sugano K, Fujimoto K, Tajiri H (2015) JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 27:417–434. https://doi.org/10.1111/den.12456
Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K (2017) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 23:1–34. https://doi.org/10.1007/s10147-017-1101-6
Hayashi N, Tanaka S, Hewett DG, Kaltenbach TR, Sano Y, Ponchon T, Saunders BP, Rex DK, Soetikno RM (2013) Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc 78:625–632. https://doi.org/10.1016/j.gie.2013.04.185
Matsuda T, Fujii T, Saito Y, Nakajima T, Uraoka T, Kobayashi N, Ikehara H, Ikematsu H, Fu KI, Emura F, Ono A, Sano Y, Shimoda T, Fujimori T (2008) Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am J Gastroenterol 103:2700–2706. https://doi.org/10.1111/j.1572-0241.2008.02190.x
Ikehara H, Saito Y, Matsuda T, Uraoka T, Murakami Y (2010) Diagnosis of depth of invasion for early colorectal cancer using magnifying colonoscopy. J Gastroenterol Hepatol 25:905–912. https://doi.org/10.1111/j.1440-1746.2010.06275.x
Sano Y, Tanaka S, Kudo SE, Saito S, Matsuda T, Wada Y, Fujii T, Ikematsu H, Uraoka T, Kobayashi N, Nakamura H, Hotta K, Horimatsu T, Sakamoto N, Fu KI, Tsuruta O, Kawano H, Kashida H, Takeuchi Y, Machida H, Kusaka T, Yoshida N, Hirata I, Terai T, Yamano HO, Kaneko K, Nakajima T, Sakamoto T, Yamaguchi Y, Tamai N, Nakano N, Hayashi N, Oka S, Iwatate M, Ishikawa H, Murakami Y, Yoshida S, Saito Y (2016) Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Digest Endosc Off J Jpn Gastroenterol Endosc Soc 28:526–533. https://doi.org/10.1111/den.12644
Buchner AM, Shahid MW, Heckman MG, Krishna M, Ghabril M, Hasan M, Crook JE, Gomez V, Raimondo M, Woodward T, Wolfsen HC, Wallace MB (2010) Comparison of probe-based confocal laser endomicroscopy with virtual chromoendoscopy for classification of colon polyps. Gastroenterology 138:834–842. https://doi.org/10.1053/j.gastro.2009.10.053
De Palma GD, Staibano S, Siciliano S, Persico M, Masone S, Maione F, Siano M, Mascolo M, Esposito D, Salvatori F, Persico G (2010) In vivo characterisation of superficial colorectal neoplastic lesions with high-resolution probe-based confocal laser endomicroscopy in combination with video-mosaicing: a feasibility study to enhance routine endoscopy. Dig Liver Dis Off J Italian Soc Gastroenterol Italian Assoc Stud Liver 42:791–797. https://doi.org/10.1016/j.dld.2010.03.009
Fujimoto K, Fujishiro M, Kato M, Higuchi K, Iwakiri R, Sakamoto C, Uchiyama S, Kashiwagi A, Ogawa H, Murakami K, Mine T, Yoshino J, Kinoshita Y, Ichinose M, Matsui T (2014) Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 26:1–14. https://doi.org/10.1111/den.12183
Wallace M, Lauwers GY, Chen Y, Dekker E, Fockens P, Sharma P, Meining A (2011) Miami classification for probe-based confocal laser endomicroscopy. Endoscopy 43:882–891. https://doi.org/10.1055/s-0030-1256632
Rectum JSfCotCa (2009) Japanese Society for Cancer of the Colon and Rectum. Japanese classification of colorectal carcinoma. 7th edn. Revised Version. Kanehara and Co Ltd, Tokyo
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishihara S, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Boku N, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20:207–239. https://doi.org/10.1007/s10147-015-0801-z
Hamilton SRBF, Boffetta P et al (2010) Carcinoma of the colon and rectum. In: Bosman FT, Carneiro F, Hruban RH et al (eds) WHO classification of tumours of the digestive system, 4th edn. IARC, Lyon, pp 134–146
Dixon MF (2002) Gastrointestinal epithelial neoplasia: Vienna revisited. Gut 51:130–131
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458. https://doi.org/10.1038/bmt.2012.244
Sano Y, Ikematsu H, Fu KI, Emura F, Katagiri A, Horimatsu T, Kaneko K, Soetikno R, Yoshida S (2009) Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Gastrointest Endosc 69:278–283. https://doi.org/10.1016/j.gie.2008.04.066
Ikematsu H, Matsuda T, Emura F, Saito Y, Uraoka T, Fu KI, Kaneko K, Ochiai A, Fujimori T, Sano Y (2010) Efficacy of capillary pattern type IIIA/IIIB by magnifying narrow band imaging for estimating depth of invasion of early colorectal neoplasms. BMC Gastroenterol 10:33. https://doi.org/10.1186/1471-230x-10-33
Kudo S, Hirota S, Nakajima T, Hosobe S, Kusaka H, Kobayashi T, Himori M, Yagyuu A (1994) Colorectal tumours and pit pattern. J Clin Pathol 47:880–885
Sakamoto T, Saito Y, Nakajima T, Matsuda T (2011) Comparison of magnifying chromoendoscopy and narrow-band imaging in estimation of early colorectal cancer invasion depth: a pilot study. Dig Endosc Off J Jpn Gastroenterol Endosc Soc 23:118–123. https://doi.org/10.1111/j.1443-1661.2010.01049.x
Sakamoto T, Nakajima T, Matsuda T, Murakami Y, Ishikawa H, Yao K, Saito Y (2018) Comparison of the diagnostic performance between magnifying chromoendoscopy and magnifying narrow-band imaging for superficial colorectal neoplasm: an online survey. Gastrointest Endosc 87:1318–1323. https://doi.org/10.1016/j.gie.2017.12.021
Higashi R, Uraoka T, Kato J, Kuwaki K, Ishikawa S, Saito Y, Matsuda T, Ikematsu H, Sano Y, Suzuki S, Murakami Y, Yamamoto K (2010) Diagnostic accuracy of narrow-band imaging and pit pattern analysis significantly improved for less-experienced endoscopists after an expanded training program. Gastrointest Endosc 72:127–135. https://doi.org/10.1016/j.gie.2010.01.054
Neumann H, Vieth M, Atreya R, Neurath MF, Mudter J (2011) Prospective evaluation of the learning curve of confocal laser endomicroscopy in patients with IBD. Histol Histopathol 26:867–872. https://doi.org/10.14670/hh-26.867
Kiesslich R, Burg J, Vieth M, Gnaendiger J, Enders M, Delaney P, Polglase A, McLaren W, Janell D, Thomas S, Nafe B, Galle PR, Neurath MF (2004) Confocal laser endoscopy for diagnosing intraepithelial neoplasias and colorectal cancer in vivo. Gastroenterology 127:706–713
Kudo SE, Wakamura K, Ikehara N, Mori Y, Inoue H, Hamatani S (2011) Diagnosis of colorectal lesions with a novel endocytoscopic classification—a pilot study. Endoscopy 43:869–875. https://doi.org/10.1055/s-0030-1256663
Kim B, Kim YH, Park SJ, Cheon JH, Kim TI, Kim WH, Kim H, Hong SP (2017) Probe-based confocal laser endomicroscopy for evaluating the submucosal invasion of colorectal neoplasms. Surg Endosc 31:594–601. https://doi.org/10.1007/s00464-016-5003-x
Goetz M, Wang TD (2010) Molecular imaging in gastrointestinal endoscopy. Gastroenterology 138:828–833.e821. https://doi.org/10.1053/j.gastro.2010.01.009
Kiesslich R, Duckworth CA, Moussata D, Gloeckner A, Lim LG, Goetz M, Pritchard DM, Galle PR, Neurath MF, Watson AJ (2012) Local barrier dysfunction identified by confocal laser endomicroscopy predicts relapse in inflammatory bowel disease. Gut 61:1146–1153. https://doi.org/10.1136/gutjnl-2011-300695
Acknowledgements
We would like to thank Dr. Hiyoyuki Takamaru and Masau Sekiguchi, Endoscopy Division, National Cancer Center Hospital, Tokyo, Japan, and Dr. Flaminia Purchiaroni, Wolfson Unit for Endoscopy, St Mark’s Hospital, London, UK, for her kind support to this paper. Moreover, we would like to thank the Japan Agency for Medical Research and Development (AMED), which supported this study under Grant Number 15ck0106028h0002.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was carried on according to the ethical principles included in the Declaration of Helsinki. As intravenous fluorescein for pCLE has not been approved yet for clinical use in Japan, prior to the start of the study, we obtained the approval from the institutional review board for off-label use of intravenous fluorescein. Written informed consent was obtained from all patients.
Conflict of interest
There was no conflict of interest to be disclosed in relation to this study.
Rights and permissions
About this article
Cite this article
Abe, S., Saito, Y., Oono, Y. et al. Pilot study on probe-based confocal laser endomicroscopy for colorectal neoplasms: an initial experience in Japan. Int J Colorectal Dis 33, 1071–1078 (2018). https://doi.org/10.1007/s00384-018-3059-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3059-x