Abstract
Background
Though pathogenesis of non-alcoholic steatohepatitis (NASH) is unclear, association with small intestinal bacterial overgrowth [SIBO] and fecal dysbiosis is suggested. We evaluated SIBO in NASH using quantitative jejunal aspirate culture (conventional criteria: ≥ 105 colony forming unit (CFU)/mL and newer cutoff ≥ 103 CFU/mL) and glucose hydrogen breath test.
Methods
Thirty-eight patients with NASH (age 37.5 years, range 20–54, 9, 24% female), diagnosed by ultrasonography, alanine aminotransferase >1.5 times normal and liver biopsy (in 27/38, 71%) and exclusion of other causes and 12 constipation-predominant irritable bowel syndrome as historical controls (age 39.5-y, 26–44; 3, 25% female) without fatty liver were studied.
Results
Jejunal aspirates, obtained in 35/38 patients, were sterile in 14/35 (40%) and bacteria isolated in 21 (60%) (all aerobic, in one anaerobe also; Gram positive 5, negative 13, both 3). In contrast, bacteria (two Gram negative) were isolated in 3/12 (25%) controls (odds ratio 4.5, 95% CI 1.0–19.5; p = 0.04); colony counts were higher in NASH than controls (median 380 CFU/mL, 0–200,000 vs. 0 CFU/mL, 0–1000; p = 0.02). Gram negative bacteria tended to be commoner in NASH than controls (16/35 vs. 2/12; p = 0.07). Seven out of 35 (20%) patients with NASH (≥ 105 CFU/mL in 5 and 2 other on glucose hydrogen breath test) and no control had SIBO (p = ns); low-grade SIBO (≥103 CFU/mL) was commoner in NASH than controls (14/35, 40%, vs. 1/12, 8.3%; p = 0.04). There was no correlation between bacterial colony count and bacterial type and anthropometric and biochemical parameters.
Conclusion
Low-grade bacterial overgrowth, particularly with Gram negative bacteria, was commoner in NASH than controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic steatohepatitis (NASH) is common all over the world [1, 2]. It has potential clinical significance in causing cirrhosis of liver both among children and adults in the long-run [1, 3,4,5]. Pathogenesis of NASH is largely unresolved yet. Though it is associated with obesity, hyperlipidemia, and diabetes mellitus [2, 3, 6,7,8], these factors are not found universally [9].
Gut dysbiosis (small intestinal bacterial overgrowth [SIBO] and qualitative change in fecal microbiota) have been found to be associated with NASH in a few animal and human studies [8, 10,11,12,13,14]. However, diagnosis of SIBO in most of these studies was not based on the gold standard method (quantitative jejunal aspirate culture), but on d-xylose, glucose, and lactulose hydrogen breath tests, sensitivity and specificity of which are somewhat low [15]. There are scanty data on SIBO in patients with NASH using quantitative bacterial culture of jejunal aspirate, which, though not perfect, is accepted as the gold standard for the diagnosis [15].
Non-alcoholic steatohepatitis-like changes are known in patients with morbid obesity and jejunoileal bypass [6, 16, 17], which are often associated with SIBO; such changes are known to improve after gut microbiota modulating treatment such as that with metronidazole, rifaximin, and probiotics [18,19,20]. Therefore, if SIBO is found to be a factor contributing to NASH, antibiotic therapy may have potential role in its treatment in addition to weight reduction and control of diabetes mellitus. It has also been demonstrated that NASH patients, even in the absence of alcohol consumption, have increased alcohol level in the portal vein due to bacterial fermentation of ingested carbohydrates in the gut [21]. Accordingly, we undertook a prospective study to evaluate the association between SIBO and NASH using quantitative jejunal aspirate culture and glucose hydrogen breath test (GHBT).
Methods
Participants
Consecutively, patients diagnosed having NASH based on high aminotransaminase values (> 1.5 times above the upper limit of normal) for at least 3 months, fatty liver on abdominal ultrasonography (USG), and histological features on liver biopsy (in 27/38, 71% patients) were evaluated clinically, and for SIBO using quantitative culture of jejunal aspirate and GHBT using standard techniques [15, 22]. Patients having one or more of the following were excluded from the study: (1) alcohol intake greater than 20 g/day, (2) positive tests for HBsAg or anti-HCV antibody in serum, (3) positive autoimmune markers (ANA, ASMA, AMA, and ALKM) by standard techniques, (4) abnormally high serum transferrin saturation and ferritin more than 50% and 200 ng/mL, respectively, (5) history of ingestion of hepato-toxic drugs like corticosteroids, nifedipine, amiodarone, and isoniazid during the previous 6 months, (6) advanced liver disease, and (7) receiving any antibiotic in the past 4 weeks.
Data of 12 patients with constipation-predominant irritable bowel syndrome (IBS) studied as historical controls were used for comparison [23]. None of these controls had clinical, biochemical, and ultrasonographic (USG) evidence of liver disease.
Anthropometry
Anthropometric measurements included weight, height, body mass index (BMI), waist and hip circumferences, and waist-hip ratio. Weight was measured to the nearest half-kilogram and height to the nearest 2 mm. BMI was calculated using the formula Kg/m2. Waist circumference was measured at the level of the umbilicus. Hip circumference in centimeters was noted at the widest portion of buttocks. Waist-hip ratio was calculated by dividing waist circumference by hip circumference. The Indian cutoff to define obesity was used [24].
Investigations
Biochemical investigations like serum albumin, alanine aminotransferase (ALT), aspartate aminotransferase (AST), fasting blood glucose, complete lipid profile, serum transferrin saturation, and ferritin were obtained in all patients. Abdominal USG was performed in all patients for evidence of fatty liver and to look for any evidence of portal hypertension. Fatty liver on USG was graded as described previously [25] as follows: grade 0, normal echogenicity; grade I, slight, diffuse increase in fine echoes in liver parenchyma with normal visualization of diaphragm and intrahepatic vessel borders; grade II, moderate, diffuse increase in fine echoes with slightly impaired visualization of intrahepatic vessels and diaphragm; grade III, marked increase in fine echoes with poor or non-visualization of the intrahepatic vessel borders, diaphragm and posterior right lobe of the liver. Investigations to exclude other causes of chronic hepatitis were undertaken.
Liver biopsy
Percutaneous liver biopsy was done in consenting patients. Biopsy tissues were evaluated by a single pathologists and were scored using Brunt’s criteria [26]. Grading was done as follows: (a) steatosis was graded as 0 (no steatosis), 1 (< 33% of biopsy), 2 (33% to 66%), and 3 (> 66% of biopsy); (b) necro-inflammation was graded as 1–3; and (c) fibrosis was graded as 1 (zone 3 fibrosis, focally or extensively present), 2 (zone 3 fibrosis with periportal fibrosis), 3 (zone 3 fibrosis with bridging fibrosis), and 4 (cirrhosis).
Jejunal aspiration
Jejunal aspirate was collected during upper gastrointestinal endoscopy done under light sedation using a pediatric colonoscope and a double lumen catheter described by us previously with some modifications [23, 27]. Briefly, the catheter assembly had an inner tube that was 3 cm longer than the outer tube. An obturator blocked the mouth of the outer tube. The assembly was sterilized by autoclaving. On reaching the jejunum, the catheter assembly was introduced through the biopsy channel of a sterilized pediatric colonoscope. The inner tube was then pushed beyond the tip of the outer tube once the outer tube was 4–5 cm ahead of the tip of the endoscope. This led to dislodgement of the obturator from the tip of the outer tube. Jejunal aspirate, collected through the inner tube with a sterile syringe, was used for aerobic and anaerobic bacterial culture (transported in Robertson’s cooked meat medium for the latter) and colonies counted by serial dilution technique [23, 27].
Bacteriological studies
Bacterial species were cultured and identified using standard techniques [28]. Briefly, for aerobic culture, samples were homogenized and then diluted serially. Aliquots of non-diluted sample and each dilution (100 μL each) were plated on blood agar and MacConkey agar. After incubation, colonies were counted and bacterial species identified using standard techniques [28, 29]. For anaerobic culture, Robertson’s cooked meat broth was used. Undiluted sample and serial dilutions (100 μL each) were sub-cultured on Wilkins-Chalgren agar. For anaerobic culture, anaerobic jars (McIntosh) were used. The standard anaerobic recipe has 3 evacuation replacement cycles. Strains of Clostridium difficile, Clostridium perfringens, Bacteroides fragilis, and Gram-negative cocci were used as positive control with each batch. Pseudomonas aeruginosa was used as negative control. Cultures were examined for bacterial growth after incubation for 48 h and, if negative, after 5 days at 37 °C in an anaerobic chamber. In case of bacterial growth, colonies were counted and bacterial species identified using standard techniques [15, 27]. Rogosa agar was used for lactobacilli and was incubated in anaerobic conditions [28]. Bacterial counts were expressed as logarithm of colony forming units per milliliter of jejunal fluid. Total bacterial colonies and count of each species were obtained.
Glucose hydrogen breath test
Glucose hydrogen breath test was performed after adequate preparation using standard technique [22] within 1 week of conducting bacteriological studies. Standard criteria described previously (> 12 parts per million above basal in breath hydrogen on at least two consecutive reading) were used for diagnosis of SIBO on GHBT [22].
Ethics clearance
The study protocol was approved by the Ethics Committee of the Institute. Informed consent was obtained from each subject.
Statistical analysis
Sample size was calculated based on Indian studies showing frequency of SIBO among NASH to be 37% [12] and that among controls to be 1% [30,31,32], two-sided confidence interval (CI) of 90% and power of 80%, and ratio of controls to cases of 0.3; 31 cases and 10 controls were estimated. For calculation of sample size, EpiInfo software version 7 (Center for Disease Control and Prevention, Atlanta, Georgia, USA) was used.
Data were expressed as median and range. Comparison between continuous and categorical data in various groups was done using Mann-Whitney U and Chi-square tests with Yates’ correction, if applicable, respectively. Two continuous variables were correlated using Spearman’s correlation. Differences were considered statistically significant at p<0.05. Data were analyzed by SPSS version 15 (SPSS, Inc., Chicago, IL, USA), R, Epicalc and R-studio software (R development core team, Vienna, Austria) and MedCalc version 14 (Warandeberg 3, 1000 Brussels, Belgium).
Results
Demographic, clinical, and biochemical parameters
Since adequate jejunal aspirate could not be obtained in 3 patients with NASH, they were excluded from the analysis. Thirty-five patients with NASH whose data were finally analyzed (median age 37.0 years, range 20–54, 7, 20% female) were comparable to 12 controls (age 39.5 years, 26–44; 3, 25% female) in age and gender. Table 1 presents the demographic, clinical, and laboratory data of patients and the controls. Anthropometric parameters in patients with NASH were median (range), weight 70 kg (55–115), height 1.7 m (1.5–1.8), BMI 25.4 kg/m2 (20.4–37.5), and waist-hip ratio 0.97 (0.84–1.09). Twenty of 35 (57.1%) patients with NASH had BMI >25 kg/m2 that has been defined as obesity in India. Three patients with NASH were diabetic. None of the control was obese (median BMI 21 kg/m2, range 19–22.9) or diabetic.
Ultrasonography revealed grade 1, 2, and 3 fatty liver in 14 (40.0%), 16 (45.7%), and 5 (14.2%) patients, respectively. Median alanine and aspartate aminotransferases (ALT and AST) values were 90 IU/L (29–349) and 62.5 IU/L (17–292), respectively. Of 27/35 (77%) patients undergoing liver biopsy, histology revealed steatosis (none in 1, grade 1 in 17, grade 2 in 8, and grade 3 in 1), necro-inflammation (stage 1 in 19, stage 2 in 6, and stage 3 in 2), and fibrosis (stage 1 in 13, stage 2 in 8, stage 3 in 2, and stage 4 in 4).
Patients with NASH who underwent or did not undergo liver biopsy were comparable in demographic, clinical, and laboratory parameters (Table 2).
Glucose hydrogen breath test result
GHBT was done in 25 patients, 2 of whom were positive for SIBO. None of the controls had SIBO on GHBT.
Result of jejunal aspirate culture
Jejunal aspiration procedure was safe and well tolerated by all the patients. Of 35 patients with NASH in whom adequate jejunal aspirate could be obtained, culture was sterile in 14 (40%) and aerobic bacteria were isolated in 21 (60%), one of whom also grew anaerobes. In contrast, bacteria were isolated in 3/12 (25%) controls (odds ratio 4.5, 95% CI 1.0–19.5; p=0.04; Acinetobacter baumannii, which is Gram negative, in two). Gram negative bacteria tended to be commoner in NASH than controls (16/35 vs. 2/12; odds ratio 4.2, 95% CI 0.8–22; p=0.07). Patients with NASH had higher colony counts of bacteria in jejunal aspirate than controls (median 330 CFU/mL, range 0–200,000 vs. median 0 CFU/mL, 0–1000; p=0.02; Fig. 1). The colony counts in whom the organisms were grown on cultures was less than 103 CFU/mL in 7, between 103 and 105 CFU/mL in 9, and ≥ 105 CFU/mL in five. Both the patients with positive result on GHBT did not grow any bacteria on jejunal aspirate culture.
Table 3 shows the nature of bacteria isolated. Gram positive, negative, and both Gram positive and negative bacteria were grown in jejunal aspirate of 5 (38%), 13 (62%), and 3 (14%) of 21 patients with NASH, respectively. Though the colony counts among patients having growth of Gram negative and both Gram negative and positive bacteria were higher than those having Gram positive bacteria, there was no relationship between the colony counts and the type of bacteria and BMI, and degree of transaminase elevation (Figs. 2 and 3a–d).
SIBO was present in 7/35 (20%) patients with NASH (≥ 105 CFU/mL on jejunal aspirate culture in 5 and on GHBT in 2 other) and no control (p=ns); however, low grade bacterial overgrowth (≥103 CFU/mL) was detected more often among patients with NASH than controls (14/35, 40%, vs. 1/12, 8.3%; odds ratio 7.3, 95% CI 0.8–63; p=0.04). Even after excluding patients with NASH not undergoing liver biopsy, conclusion did not change (Table 2).
Comparison of patients with and without SIBO
Demographic, anthropometric, and laboratory parameters of patients with or without SIBO (based on the conventional definition of ≥ 105 CFU/mL on jejunal aspirate culture) were comparable (Table 4).
Discussion
In the present study, we found that (i) though according to conventional definition (jejunal aspirate colony count ≥105 CFU/mL) frequency of SIBO was comparable among patients with NASH and controls, low-grade SIBO (≥103 CFU/mL) was commoner among patients with NASH; (ii) Gram negative bacteria was commonly isolated in NASH and their frequency tended to be higher than among controls; and (iii) there was no relationship between the colony counts and the type of bacteria and demographic and biochemical parameters.
The finding of the present study is important as it is being realized currently that low grade bacterial overgrowth (≥ 103 CFU/mL) may be significant in other gastrointestinal disorders such as IBS and tropical sprue and may contribute to the pathogenesis of these conditions [15, 23, 33, 34]. In a recent study in patients with IBS, it was shown that treatment with norfloxacin, directed against SIBO, resulted in symptom improvement more often in patients with high- (≥ 105) and low-grade (≥ 103 but ≤ 105) SIBO than those without SIBO (either low- or high-grade) suggesting the importance of low-grade SIBO [34]. In another study, there were 9/13 patients with tropical sprue with bacterial contamination of small bowel, which was more than controls [23]. Growth of ≥ 103 CFU/mL of colonic type flora was regarded as significant bacterial contamination of the small bowel [23]. Hence, a colony count in jejunal aspirate of ≥ 103 CFU/mL has been defined as low grade SIBO recently [15]. Role of the gut microbiota in metabolic disorders including obesity, diabetes mellitus, atherosclerosis, and coronary artery disease, broadly considered as metabolic syndrome, is being understood in the recent years [35,36,37]. NASH is also included in metabolic syndrome, which is often associated with the other metabolic disorders [38]. Hence, quantitative (SIBO) and qualitative alteration in gut microbiota is quite expected to be associated with NASH. However, there is scarcity of the data on this issue in the literature. In an earlier study by Riordan et al. using jejunal aspirate culture, the incidence of liver injury was not common in patients with SIBO [39]. The findings in our study are somewhat different than those reported earlier by Wigg et al. who found that SIBO was present more often in patients with NASH (50%) than controls (22%) [13]. Though we found SIBO as defined by colony count of ≥ 105 CFU/mL was comparable between patients with NASH and controls, a low-grade SIBO was commoner among the patients. One reason for lower frequency of high-grade SIBO in our patient population may be because of lower BMI of our patients (26.6 ± 4.0 kg/m2) when compared to the earlier study (30 ± 6 kg/m2) as obesity itself has shown to be associated with SIBO [14].
Recently, based on animal studies, gut microbiota have been suggested to play important role in pathogenesis of different spectrum of non-alcoholic fatty liver diseases (NAFLD) ranging between steatosis, NASH, fibrosis, and liver cancer [40]. To make our study population homogeneous, we included patients with NASH only. Though liver biopsy is considered important to diagnose NASH [41], it could not be done in 23% of non-consenting patients and none of the controls due to its invasive nature with potential risk of complication and ethical issues. However, the demographic, clinical, and laboratory parameters of patients undergoing and not undergoing liver biopsy were comparable (Table 2), suggesting that this limitation might not be a major limitation. A practice guideline published by American Association for the Study of Liver suggested that liver biopsy should be performed in those who would benefit the most from diagnostic, therapeutic guidance, and prognostic perspectives [41].
Several human studies also showed that fecal microbial dysbiosis studied using 16S ribonucleic acid gene sequencing was commoner among patients with NASH than controls [42]. A few studies even showed that some specific species of microbial metagenome were associated with specific liver lesion such as Bacterioides with NASH and Ruminococcus with fibrosis [10]. In another study, Escherichia, Anaerobacter, Lactobacillus, and Streptococcus metagenome in feces were associated with NAFLD [43]. In yet another study, the presence of Gram negative bacterial metagenome was associated with NAFLD [44]. This observation is somewhat in line with the result of our study showing that Gram negative bacteria tended to be commoner in patients with NASH than controls. However, in the earlier study [44], altered fecal microbiota correlated with liver biochemistry in patients with NAFLD, which is different than the results of the present study. A few specific microbes being associated with NASH can be explained based on the fact that different gut microbes produce different metabolites and hence, immune function [40, 42, 43]. Moreover, some specific microbes such as E. coli, Bacteroides, Bifidobacteria, Clostridia, and Ruminococcus are known to produce alcohol from dietary carbohydrates, and portal vein alcohol has been shown to be elevated in these patients even in the absence of alcohol ingestion [21].
Diabetes and hypothyroidism are known to cause SIBO [45]. In our study, diabetes mellitus or impaired glucose tolerance was present in three patients and in only one of them the jejunal aspirate culture was positive. In this patient, the culture grew Enterococcus with <105 CFU/mL. Hypothyroidism was present in only one patient in whom the culture, as well as GHBT, was negative.
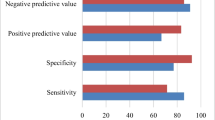
We used the quantitative culture of jejunal aspirate, the gold standard test for the diagnosis of SIBO [15]. In our study, we performed GHBT in spite of its low sensitivity to diagnose SIBO due to its non-invasive nature and high specificity [15, 22]. It helped us to pick up two additional patients with SIBO in whom jejunal aspirate cultures were negative. This might have resulted from SIBO in location beyond the reach of endoscopic aspirating catheter. Moreover, GHBT, being non-invasive, could also be performed among controls. It was shown in earlier studies that jejunal culture is more sensitive than hydrogen breath tests [33]. In a study by Corazza et al., the sensitivity and specificity of glucose breath test were 62% and 83%, respectively [46]. Limited data available on the d-xylose breath test to diagnose SIBO also suggests a low specificity of this investigation [47]. Therefore, most human studies on SIBO in patients with NASH had limitations [11,12,13]. The present study is the second study in which quantitative culture of jejunal aspirate, the currently accepted gold standard method for diagnosis of SIBO, though not perfect, has been used. The only other study that used aspirate culture found 37% frequency of SIBO among patients with NAFLD; however, in that study, no control was included [12].
Our study had a few limitations. The control group included previously reported patients with constipation-predominant IBS rather than healthy subjects. Though ideal controls could have been socioeconomically comparable healthy subjects, we could not include them for endoscopic jejunal aspiration due to ethical issue. Though a fourth of patients with IBS are known to have SIBO, it usually occurs in patients with diarrhea- rather than constipation-predominant IBS [33, 48]. Moreover, our results showed that even in comparison with patients with IBS, NASH patients more often had low-grade SIBO suggesting that inclusion of healthy subjects as controls would not refute our conclusion. The ratio of patients to controls were kept as 3:1 as the control group included previously reported patients and it is difficult to get consent of control population for endoscopic jejunal aspiration due to the degree of discomfort associated with it. Though we excluded the presence of NASH by liver function test and USG, liver biopsy or non-invasive magnetic resonance spectroscopy were not done. However, as shown in Table 2, even after excluding the patients who did not undergo liver biopsy, the conclusions remain valid. This is an association study. Cause and effect relation cannot be concluded from this study.
In conclusion, low-grade SIBO was commoner among patients with NASH as compared to controls.
References
Bellentani S. The epidemiology of non-alcoholic fatty liver disease. Liver Int. 2017;37 Suppl 1:81–4.
Agrawal S, Duseja AK. Non-alcoholic fatty liver disease: east versus west. J Clin Exp Hepatol. 2012;2:122–34.
Angulo P, Keach JC, Batts KP, Lindor KD. Independent predictors of liver fibrosis in patients with nonalcoholic steatohepatitis. Hepatology. 1999;30:1356–62.
Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149. 389-97:e10.
Feldstein AE, Charatcharoenwitthaya P, Treeprasertsuk S, Benson JT, Enders FB, Angulo P. The natural history of non-alcoholic fatty liver disease in children: a follow-up study for up to 20 years. Gut. 2009;58:1538–44.
Ratziu V, Giral P, Charlotte F, et al. Liver fibrosis in overweight patients. Gastroenterology. 2000;118:1117–23.
Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and obesity: an autopsy study with analysis of risk factors. Hepatology. 1990;12:1106–10.
Wiest R, Albillos A, Trauner M, Bajaj J, Jalan R. Targeting the gut-liver axis in liver disease. J Hepatol. 2017; pii: S0168-8278(17)32016-0.
Sreenivasa Baba C, Alexander G, Kalyani B, et al. Effect of exercise and dietary modification on serum aminotransferase levels in patients with nonalcoholic steatohepatitis. J Gastroenterol Hepatol. 2006;21:191–8.
Boursier J, Mueller O, Barret M, et al. The severity of nonalcoholic fatty liver disease is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63:764–75.
Fialho A, Thota P, McCullough AJ, Shen B. Small intestinal bacterial overgrowth is associated with non-alcoholic fatty liver disease. J Gastrointestin Liver Dis. 2016;25:159–65.
Kapil S, Duseja A, Sharma BK, et al. Small intestinal bacterial overgrowth and toll-like receptor signaling in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2016;31:213–21.
Wigg AJ, Roberts-Thomson IC, Dymock RB, McCarthy PJ, Grose RH, Cummins AG. The role of small intestinal bacterial overgrowth, intestinal permeability, endotoxaemia, and tumour necrosis factor alpha in the pathogenesis of non-alcoholic steatohepatitis. Gut. 2001;48:206–11.
Sabate JM, Jouet P, Harnois F, et al. High prevalence of small intestinal bacterial overgrowth in patients with morbid obesity: a contributor to severe hepatic steatosis. Obes Surg. 2008;18:371–7.
Ghoshal UC, Ghoshal U. Small intestinal bacterial overgrowth and other intestinal disorders. Gastroenterol Clin N Am. 2017;46:103–20.
Hocking MP, Duerson MC, O'Leary JP, Woodward ER. Jejunoileal bypass for morbid obesity. Late follow-up in 100 cases. N Engl J Med. 1983;308:995–9.
Li L, Liu DW, Yan HY, Wang ZY, Zhao SH, Wang B. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016;17:510–9.
Drenick EJ, Fisler J, Johnson D. Hepatic steatosis after intestinal bypass--prevention and reversal by metronidazole, irrespective of protein-calorie malnutrition. Gastroenterology. 1982;82:535–48.
Gangarapu V, Ince AT, Baysal B, et al. Efficacy of rifaximin on circulating endotoxins and cytokines in patients with nonalcoholic fatty liver disease. Eur J Gastroenterol Hepatol. 2015;27:840–5.
Ma YY, Li L, Yu CH, Shen Z, Chen LH, Li YM. Effects of probiotics on nonalcoholic fatty liver disease: a meta-analysis. World J Gastroenterol. 2013;19:6911–8.
Duseja A, Chawla YK. Obesity and NAFLD: the role of bacteria and microbiota. Clin Liver Dis. 2014;18:59–71.
Ghoshal UC. How to interpret hydrogen breath tests. J Neurogastroenterol Motil. 2011;17:312–7.
Ghoshal UC, Ghoshal U, Ayyagari A, et al. Tropical sprue is associated with contamination of small bowel with aerobic bacteria and reversible prolongation of orocecal transit time. J Gastroenterol Hepatol. 2003;18:540–7.
Misra A, Chowbey P, Makkar BM, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70.
Scatarige JC, Scott WW, Donovan PJ, Siegelman SS, Sanders RC. Fatty infiltration of the liver: ultrasonographic and computed tomographic correlation. J Ultrasound Med. 1984;3:9–14.
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–74.
Ghoshal U, Ghoshal UC, Ranjan P, Naik SR, Ayyagari A. Spectrum and antibiotic sensitivity of bacteria contaminating the upper gut in patients with malabsorption syndrome from the tropics. BMC Gastroenterol. 2003;3:9.
Collee JG, Miles RS, Walt B. Tests for the identification of bacteria. In: Collee JG, Fraser AG, Marmion BP, Simmons A, editors. Mackie and McCartney Practical Medical Microbiology. New York: Churchill Livingstone; 1996. p. 131–49.
Anonymous. Processing clinical specimens for anaerobic bacteria: Isolation and identification procedures. In: Baron EJ, Peterson LR, Finegold SM, editors. Bailey and Scott’s Diagnostic Microbiology. Philadelphia: Mosby; 1994. p. 474–503.
Bardhan PK, Gyr K, Beglinger C, Vogtlin J, Frey R, Vischer W. Diagnosis of bacterial overgrowth after culturing proximal small-bowel aspirate obtained during routine upper gastrointestinal endoscopy. Scand J Gastroenterol. 1992;27:253–6.
Bala L, Ghoshal UC, Ghoshal U, et al. Malabsorption syndrome with and without small intestinal bacterial overgrowth: a study on upper-gut aspirate using 1H NMR spectroscopy. Magn Reson Med. 2006;56:738–44.
Lakshmi CP, Ghoshal UC, Kumar S, et al. Frequency and factors associated with small intestinal bacterial overgrowth in patients with cirrhosis of the liver and extra hepatic portal venous obstruction. Dig Dis Sci. 2009;55:1142–8.
Ghoshal UC, Srivastava D, Ghoshal U, Misra A. Breath tests in the diagnosis of small intestinal bacterial overgrowth in patients with irritable bowel syndrome in comparison with quantitative upper gut aspirate culture. Eur J Gastroenterol Hepatol. 2014;26:753–60.
Ghoshal UC, Srivastava D, Misra A, Ghoshal U. A proof-of-concept study showing antibiotics to be more effective in irritable bowel syndrome with than without small-intestinal bacterial overgrowth: a randomized, double-blind, placebo-controlled trial. Eur J Gastroenterol Hepatol. 2016;28:281–9.
Goel A, Gupta M, Aggarwal R. Gut microbiota and liver disease. J Gastroenterol Hepatol. 2014;29:1139–48.
Festi D, Schiumerini R, Eusebi LH, Marasco G, Taddia M, Colecchia A. Gut microbiota and metabolic syndrome. World J Gastroenterol. 2014;20:16079–94.
Greenhill C. Obesity: gut microbiota, host genetics and diet interact to affect the risk of developing obesity and the metabolic syndrome. Nat Rev Endocrinol. 2015;11:630.
Duseja A, Singh SP, Saraswat VA, et al. Non-alcoholic Fatty Liver Disease and Metabolic Syndrome-Position Paper of the Indian National Association for the Study of the Liver, Endocrine Society of India, Indian College of Cardiology and Indian Society of Gastroenterology. J Clin Exp Hepatol. 2015;5:51–68.
Riordan SM, McIver CJ, Williams R. Liver damage in human small intestinal bacterial overgrowth. Am J Gastroenterol. 1998;93:234–7.
Boursier J, Diehl AM. Implication of gut microbiota in nonalcoholic fatty liver disease. PLoS Pathog. 2015;11:e1004559.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Am J Gastroenterol. 2012;107:811–26.
Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146:1513–24.
Jiang W, Wu N, Wang X, et al. Dysbiosis gut microbiota associated with inflammation and impaired mucosal immune function in intestine of humans with non-alcoholic fatty liver disease. Sci Rep. 2015;5:8096.
Wang B, Jiang X, Cao M, et al. Altered fecal microbiota correlates with liver biochemistry in nonobese patients with non-alcoholic fatty liver disease. Sci Rep. 2016;6:32002.
Krajicek EJ, Hansel SL. Small intestinal bacterial overgrowth: A primary care review. Mayo Clin Proc. 2016;91:1828–33.
Corazza GR, Menozzi MG, Strocchi A, et al. The diagnosis of small bowel bacterial overgrowth. Reliability of jejunal culture and inadequacy of breath hydrogen testing. Gastroenterology. 1990;98:302–9.
Dellert SF, Nowicki MJ, Farrell MK, Delente J, Heubi JE. The 13C-xylose breath test for the diagnosis of small bowel bacterial overgrowth in children. J Pediatr Gastroenterol Nutr. 1997;25:153–8.
Ghoshal UC, Kumar S, Mehrotra M, Lakshmi C, Misra A. Frequency of small intestinal bacterial overgrowth in patients with irritable bowel syndrome and chronic non-specific diarrhea. J Neurogastroenterol Motil. 2010;16:40–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
UCG, CSB, UG, GA, AM, VAS, and GC declare that they have no conflict of interest.
Ethics statement
The authors declare that the study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning Human and Animal Rights. The protocol was approved by the Institutional Ethics Committee and informed consent was obtained from the study subjects.
Rights and permissions
About this article
Cite this article
Ghoshal, U.C., Baba, C.S., Ghoshal, U. et al. Low-grade small intestinal bacterial overgrowth is common in patients with non-alcoholic steatohepatitis on quantitative jejunal aspirate culture. Indian J Gastroenterol 36, 390–399 (2017). https://doi.org/10.1007/s12664-017-0797-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-017-0797-6