Abstract
Background
Hepatic venous outflow tract obstruction (HVOTO) and extrahepatic portal venous obstruction (EHPVO) are important causes of portal hypertension and related complications in India. Both these conditions result from splanchnic venous thrombosis. In recent years, a V617F somatic mutation in Janus kinase 2 (JAK2) gene which is highly specific for myeloproliferative disorders has been detected in 40 % to 50 % and 30 % to 35 % of Western patients with HVOTO and EHPVO, respectively. However, data on this mutation in these conditions from Asian countries are limited.
Methods
We looked for JAK2 V617F mutation in Indian patients with HVOTO (n = 40, median age 31 [range 17–51] years, 21 female) and EHPVO (n = 50, median age 23 [15–70] years, 25 female) by using two separate methods. Both the methods involved polymerase chain reaction using allele-specific primers. Positive results on one or both of these techniques were confirmed using DNA sequencing.
Results
None of the 40 patients with HVOTO and only 1 of 50 patients with EHPVO was found to have JAK2 V617F mutation. In the one patient who was found to have this mutation, both the PCR methods and DNA sequencing showed positive results.
Conclusion
Hypercoagulability associated with JAK2 V617F mutation and associated chronic myeloproliferative disorders was not a major cause of HVOTO and EHPVO in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatic venous outflow tract obstruction (HVOTO) and extrahepatic portal venous obstruction (EHPVO) are important causes of portal hypertension in the Indian subcontinent [1, 2]. These conditions are related to blockage of the hepatic veins and/or inferior vena cava (IVC) in HVOTO and of the portal vein in EHPVO. This blockage is most often due to venous thrombosis, though occasionally, other causes such as congenital anomalies or tumors may be responsible. Thrombotic EHPVO in the absence of inflammatory diseases such as pancreatitis is essentially an Asian disease, being reported primarily from the Indian subcontinent and Japan. In these areas, it is the commonest cause of portal hypertension in children and young adults [1]. In comparison, in Europe or North America, EHPVO is very rare, being observed occasionally among elderly persons [1]. Similarly, HVOTO in Asian patients appears to be a different disease from that in the West because of an earlier age of onset, a subacute or insidious onset, and a longer survival [2].
In Western countries, “Philadelphia chromosome”-negative myeloproliferative disorders, namely polycythemia vera, essential thrombocythemia, and myelofibrosis, are a major cause for both HVOTO and EHPVO, being responsible for 33 % to 78 % and 23 % to 48 % of cases with these conditions, respectively [3–6]. These myeloproliferative disorders are related to a defect in multipotent hematopoietic stem cells which leads to an increased production of mature blood cells. The increased and autonomous production of these cells, important for the diagnosis of myeloproliferative disorders, is however difficult to establish in patients with HVOTO or EHPVO because of the frequent presence of hemodilution, occult bleeding, and hypersplenism [7–10].
In 2005, an acquired mutation in the Janus kinase 2 (JAK2) gene located on the short arm of chromosome 9 was identified in patients with polycythemia vera, essential thrombocythemia, and idiopathic myelofibrosis [11–15]. In this mutation, a guanidine-to-thymidine change at nucleotide 1849 in exon 12 leads to substitution of valine by phenylalanine at amino acid position 617 (V617F) of the JAK2 protein. This change, located in the JH2 pseudokinase domain, is associated with a gain of function and makes the JAK2 protein constitutively active even in the absence of erythropoietin, leading to an increased proliferation of hematopoietic stem cells. Several studies from the West have reported the presence of this mutation in 20 % to 45 % and 35 % of patients with HVOTO and EHPVO, respectively [16–18].
However, data on the role of myeloproliferative disorders and of this mutation in Indian patients with HVOTO and EHPVO are limited. In view of the onset at young age and relatively benign long-term course of these conditions in this geographical area, it is possible that myeloproliferative disorders contribute much less to the causation of these conditions in India. To clarify this issue, we studied the frequency of JAK2 V617F mutation in Indian patients with HVOTO and EHPVO.
Methods
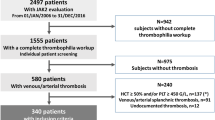
Subjects
Patients with HVOTO or EHPVO attending the outpatient or inpatient services of our department between January and October 2011 were invited to participate in the study. The study protocol was approved by the Ethics Committee of our institution, and all subjects provided an informed consent.
All the patients had clinical and/or endoscopic evidence of portal hypertension. Diagnosis of HVOTO was based on radiological evidence of obstruction of the main hepatic veins, inferior vena cava, or both. Diagnosis of EHPVO was based on evidence of obstruction of the extrahepatic portal vein, with or without its tributaries, along with demonstration of a portal cavernoma either at Doppler ultrasound or at magnetic resonance portovenography. Patients with identifiable causes of splanchnic venous thrombosis (i.e. liver tumors, pancreatitis, liver cirrhosis, previous laparotomy, recent pregnancy, or use of oral contraceptives) were excluded.
Detection of JAK2 V617F mutation
From each patient, 2 mL of peripheral blood was collected in EDTA. DNA was extracted using a standard spin column technique (QIAmp DNA Mini Kit; Qiagen, Valencia, CA, USA) as per the manufacturer’s instructions. Two separate DNA amplification methods were used for detection of JAK2 V617F mutation in DNA from each patient. DNA from one healthy person and from two patients with polycythemia rubra vera previously shown to have the V617F mutation were used as negative and positive controls, respectively.
Method A
This PCR-based method used three primers (two forward and one common reverse; Table 1) [12]. The common forward and common reverse primers amplify both wild-type and mutant DNA to produce a 364-base pair (bp) long amplicon. The third primer binds only to mutant DNA and amplifies an additional PCR product of 203 bp along with the common reverse primer. In the absence of JAK2 V617F mutation, this shorter amplicon is not generated. The generation of longer amplicon serves as an internal control to confirm that the amplification worked (Fig. 1).
Principle of method A. The primers 1 and 2 are common forward and reverse primers, respectively, that can bind to both wild-type and mutant DNA. Primer 3 is a forward primer that is specific for the mutant DNA sequence. Wild-type DNA produces only one amplicon (364 bp), whereas the presence of mutant DNA leads to production of two amplification products (364 and 203 bp)
Method B
This method used four primers: two forward and two reverse (Table 1) [19]. The outer primers bind to both wild-type and mutant DNA generating a 463-bp product, whose production serves as an internal reaction control. The two internal primers, one forward and one reverse, are located in the middle and are specific for wild-type and mutant DNA, respectively. The former generates a 229-bp PCR product with the wild-type DNA but not with the mutant DNA, and the latter generates a 279 bp long with the mutant DNA and not with the wild-type DNA. On electrophoresis of PCR product, a mixture of wild-type and mutant DNA would be expected to provide three bands (i.e. 463, 229, and 279 bp), whereas pure wild-type DNA would provide only two bands (463 and 229 bp; Fig. 2).
Principle of method B. The outer primers 1 and 2 are common forward and reverse primers, respectively, that can bind to both wild-type and mutant DNA. Primer 3 is a forward primer that is specific for the wild-type DNA sequence and in association with the common reverse primer produces a 229-bp product. Primer 4 is a reverse primer that is specific for the mutant DNA sequence and in association with the common forward primer produces a 279-bp product. Thus, wild-type DNA produces only two amplification product of 463 and 229-bp length, whereas the mutant DNA produces two amplification products of 463 and 279-bp length
Confirmation of mutation using DNA sequencing
For any specimen showing JAK2 V617F mutation using either of the above methods, the PCR products generated using external primers for method B above were sequenced using the dideoxynucleotide chain termination method (ABI 3130 genetic analyzer; Applied Biosystems, Foster City, CA, USA).
Results
A total of 90 patients, including 40 with HVOTO and 50 with EHPVO, were studied. Clinical and laboratory profiles of these patients are shown in Table 2. Among patients with HVOTO, venous obstruction was restricted to one or more hepatic veins in 23 (57.5 %), involved the hepatic veins as well as the IVC in 15 (37.5 %) patients, and only the IVC in 2 (5 %) patients. In one patient with combined hepatic and IVC venous obstruction, the IVC occlusion was caused by a membranous lesion.
Using both methods, 1 of the 50 patients with EHPVO and none of 40 patients with HVOTO tested positive for JAK2 V617F mutation (Figs. 3 and 4). DNA sequencing confirmed the existence of a guanidine-to-thymidine change at nucleotide 1849 in exon 12 of the JAK2 gene in this patient.
Gel electrophoresis for method A. The 364-bp band is expected with both wild-type and mutant DNA. In contrast, the 203-bp product is expected only with mutant DNA, as shown in lane 1 (positive control). None of the patient specimens shown in this picture yielded the 203-bp product, indicating the absence of JAK2 V617F mutation in these patients
Gel electrophoresis for method B. The 463-bp band is expected with both wild-type and mutant DNA; the 229-bp band is expected only with wild-type DNA, and the 279-bp band is expected only with mutant DNA. None of the patient specimens included in this picture yielded the 279-bp product, suggesting the absence of mutation. Positive control sample yielded only 279-bp product (but no 229-bp product), indicating homozygous JAK2 V617F mutation
The patient with JAK2 V617F mutation was a 24-year-old man with non-specific abdominal pain along with dragging sensation in the left upper abdomen for 3-year duration. His investigations revealed hemoglobin 10.9 g/dL, total leukocyte count 9000/μL, platelet count 251,000/μL, bilirubin 3.7 mg/dL, alanine aminotransferase 25 IU/mL (normal <40), aspartate aminotransferase 53 IU/mL (normal <40), alkaline phosphatase 129 IU/mL (normal <150), and prothrombin time 15.2 s (control 11.8 s). Upper gastrointestinal endoscopy revealed grade II esophageal varices. HBsAg and anti-HCV tested negative. Bone marrow biopsy revealed a hypercellular bone marrow (cellularity 80 % to 90 %), with moderately increased and pleomorphic megakaryocytes, normal maturation of erythroid cells, and increased eosinophilic cells, suggesting the presence of myeloproliferative disorder. The number of blasts, plasma cells, and lymphocytes were within normal limits.
Discussion
In this study that employed two separate techniques for detection of V617F mutation in the JAK2 gene, only 1 of 50 patients with EHPVO and none of 40 patients with HVOTO was found to have this mutation. These rates are much lower than those reported in studies from Western countries.
Some previous studies from India have looked for the presence of one of the myeloproliferative disorders as underlying cause for HVOTO. The first such Indian study used bone marrow culture technique and looked for the formation of endogenous erythrocyte colonies, and 21 (69 %) of the 32 patients with HVOTO studied tested positive [20]. The presence of such colonies was taken as evidence of a latent myeloproliferative disorder, which thus appeared quite frequent. In addition, individual case reports of HVOTO associated with myeloproliferative syndrome and JAK2 V617F mutation have been reported. [21, 22]. However, in two recent studies, myeloproliferative disorder was detected in only 8.5 % and 8.8 % of Indian patients with HVOTO [23, 24]. In one of these studies, JAK2 V617F mutation was also looked for, and 12 of 137 HVOTO patients were found to be positive for this mutation. These data suggest that JAK2 V617F mutation and hence myeloproliferative disorders are not a predominant cause of HVOTO among Indian patients. This is in contrast to the Western reports in which myeloproliferative disorders accounted for more than 50 % of all cases with HVOTO and a known cause. Our study is in agreement with the previous Indian data. However, in one other study, JAK2 V617F mutation was observed in 6 of 32 patients with portal vein thrombosis and in 4 of 20 patients with hepatic vein thrombosis [25]. But, this report is from a hematology unit and hence possibly preferentially included patients with myeloproliferative disease. Similarly, another Indian report showed JAK2 V617F mutation in 40 % of Indian patients with HVOTO and 15 % of those with EHPVO [26]. However, this study included a large number of patients who were already known to have a myeloproliferative condition or acute venous thrombosis. The results of these studies cannot be compared to those of our study, since the latter included only patients with idiopathic HVOTO or EHPVO.
The clinical presentation of HVOTO in Asian patients is also different from that of patients with this disease in Western countries. Whereas in Western countries, the disease is associated with a female preponderance and relative acute presentation, Asian patients with this disease are often characterized by a long duration of symptoms and signs and a higher prevalence of liver cirrhosis. It has been suggested that these geographical differences are related to differences in the location of the venous blockage, with pure hepatic vein block accounting for 62 % of HVOTO cases from Western countries [27], but only 6 % of Japan cases and 24 % of those in India; in the latter regions, obstruction of the IVC is more common [2, 28]. However, this explanation may not be true since in recent years, an increasing proportion of Asian patients with HVOTO have been reported to have only hepatic vein block. For instance, in our study, more than half of the patients with HVOTO had obstruction limited to hepatic veins. Similar predominance of hepatic vein involvement has been reported in another Indian study, wherein obstruction was present in the hepatic vein in 59 % of patients [23]. This is contrary to most of previous studies from India where combined hepatic plus IVC obstruction was the predominant site, in frequency of 56 % to 57.5 % [23, 29, 30]. Even in comparing those Asian HVOTO patients who have only hepatic vein block, differences from Western patients with HVOTO are apparent.
EHPVO is a condition that predominantly occurs in children and adolescents in Asian countries. The precise reason for the development of EHPVO in children has not been identified. Data that are available on JAK2 mutation in Asian patients with EHPVO are limited. We found that only 1 (2 %) of our 50 patients had the JAK2 mutation. A previous Indian study had found JAK2 V617F mutation in only 4 of 76 (5 %) patients with portal vein thrombosis [24]. In contrast, most of the Western studies have shown the presence of JAK2 mutation in nearly one third of cases with portal venous thrombosis. Interestingly, a study from UK showed that none of 30 EHPVO patients studied there had JAK2 V617F mutation [31]; it was found that a large proportion of these patients were of Asian origin.
Apart from myeloproliferative disorders, several other inherited and acquired prothrombotic disorders have been found to be associated with splanchnic venous thrombosis. Thus, HVOTO is a multifactorial disease, which can be caused by several prothrombotic disorders, occurring alone or simultaneously [3, 32]. Among various inherited prothrombotic conditions, factor V Leiden mutation and protein C and S deficiency have been shown to associate with HVOTO in around 25 %, 12 %, and 7 %, respectively, in Indian studies [33, 34], similar to data from the West [3, 35, 36]. However, a study from our center had failed to find an association between HVOTO and factor V Leiden and prothrombin gene G20210A mutations [29].
Similarly, no cause can be found for most of the cases with EHPVO. Various hypotheses have included omphalitis, neonatal umbilical sepsis and umbilical vein cannulation [37], congenital defects of portal vein [38], and inherited prothrombotic disorders [33, 39]. However, no cause can be found in a large majority of patients with EHPVO. Previous studies have failed to show a strong association of inherited thrombotic disorders, factor V Leiden mutation, prothrombin gene G20210A mutation, and protein C and S deficiency with EHPVO among Indian children [40–42]. Our data show that even the common JAK2 mutation is unlikely to be responsible for this condition in most of the patients. This suggests the need for further etiological studies to identify the cause of HVOTO and EHPVO in Asian patients.
In conclusion, our data indicate that JAK2 V617F gain-of-function mutation, which is a marker of myeloproliferative disorders, was noted as a major etiological factor for HVOTO and EHPVO in our patients. Further studies are needed to identify the cause(s) underlying these diseases related to venous thrombosis, which appear to be particularly common as causes of portal hypertension in India and neighboring countries.
References
Wani ZA, Bhat RA, Bhadoria AS, Maiwall R. Extrahepatic portal vein obstruction and portal vein thrombosis in special situations: need for a new classification. Saudi J Gastroenterol. 2015;21:129–38.
Okuda H, Yamagata H, Obata H, et al. Epidemiological and clinical features of Budd-Chiari syndrome in Japan. J Hepatol. 1995;22:1–9.
Denninger MH, Chait Y, Casadevall N, et al. Cause of portal or hepatic venous thrombosis in adults: the role of multiple concurrent factors. Hepatology. 2000;31:587–91.
De Stefano V, Teofili L, Leone G, Michiels JJ. Spontaneous erythroid colony formation as the clue to an underlying myeloproliferative disorder in patients with Budd-Chiari syndrome or portal vein thrombosis. Semin Thromb Hemost. 1997;23:411–8.
Chait Y, Condat B, Cazals-Hatem D, et al. Relevance of the criteria commonly used to diagnose myeloproliferative disorder in patients with splanchnic vein thrombosis. Br J Haematol. 2005;129:553–60.
Primignani M, Martinelli I, Bucciarelli P. Risk factors for thrombophilia in extrahepatic protal vein obstruction. Hepatology. 2005;41:603–8.
Chung RT, Iafrate AJ, Amrein PC, Sahani DV, Misdraji J. Case records of the Massachusetts General Hospital. Case 15–2006: a 46-year-old woman with sudden onset of abdominal distension. N Engl J Med. 2006;354:2166–75.
Menon KV, Shah V, Kamath PS. The Budd-Chiari syndrome. N Engl J Med. 2004;350:578–85.
Valla D, Casadevall N, Huisse MG, et al. Etiology of portal vein thrombosis in adults: a prospective evaluation of primary myeloproliferative disorders. Gastroenterology. 1988;94:1063–9.
Valla D, Casadevall N, Lacombe C, et al. Primary myeloproliferative disorder and hepatic vein thrombosis: a prospective study of erythroid colony formation in vitro in 20 patients with Budd-Chiari syndrome. Ann Intern Med. 1985;103:329–34.
Kralovics R, Passamonti F, Buser AS, et al. A gain of function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352:1779–90.
Baxter EJ, Scott LM, Campbell PJ, et al. Cancer genome project. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365:1054–61.
Levine RL, Wadleigh M, Cools J, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7:387–97.
Steensma DP, Dewald GW, Lasho TL, et al. The JAK2 V617F activating tyrosine kinase mutation is an infrequent event in both “atypical” myeloproliferative disorders and myelodysplastic syndromes. Blood. 2005;106:1207–9.
Jelinek J, Oki Y, Gharibyan V, et al. JAK2 mutation 1849GT is rare in acute leukemias but can be found in CMML, Philadelphia chromosome negative CML, and megakaryocytic leukemia. Blood. 2005;106:3370–3.
Primignani M, Barosi G, Bergamaschi G, et al. Role of the JAK2 mutation in the diagnosis of chronic myeloproliferative disorders in splanchnic vein thrombosis. Hepatology. 2006;44:1528–34.
Colaizzo D, Amitrano L, Tiscia GL, et al. Occurrence of the JAK2 V617F mutation in the Budd-Chiari syndrome. Blood Coagul Fibrinol. 2008;19:459–62.
Kiladjian JJ, Cervantes F, Leebeek FW, et al. The impact of JAK2 and MPL mutations on diagnosis and prognosis of splanchnic vein thrombosis: a report on 241 cases. Blood. 2008;111:4922–9.
Jones AV, Kreil S, Zoi K, et al. Widespread occurrence of the JAK2 V617F mutation in chronic myeloproliferative disorders. Blood. 2005;106:2162–8.
Dayal S, Pati HP, Pande GK, Sharma MP, Saraya AK. Multilineage hemopoietic stem cell defects in Budd–Chiari syndrome. J Hepatol. 1997;26:293–7.
Dhiman P, Saxena P. JAK2V617F: is it sufficient as a single player in splanchnic venous thrombosis? Case Rep Hematol. 2015;2015:373490.
Dasari S, Naha K, Hande M, Vivek G. A novel subtype of myeloproliferative disorder? JAK2V617F-associated hypereosinophilia with hepatic venous thrombosis. BMJ Case Rep. 2013; 2013.
Amarapurkar DN, Punamiya SJ, Patel ND. Changing spectrum of Budd-Chiari syndrome in India with special reference to non-surgical treatment. World J Gastroenterol. 2008;14:278–85.
Shetty S, Kulkarni B, Pai N, Mukundan P, Kasatkar P, Ghosh K. JAK2 mutations across a spectrum of venous thrombosis cases. Am J Clin Pathol. 2010;134:82–5.
Sazawal S, Rathi S, Chikkara S, et al. JAK2 mutation in patients with splanchnic venous thrombosis: a pilot study from India. Indian J Med Res. 2012;135:429–31.
Deepak A, Punamiya S, Patel N, Parekh S, Mehta S, Shah N. Prevalence of JAK2-V617F mutation in intra-abdominal venous thrombosis. Trop Gastroenterol. 2011;32:279–84.
Murad SD, Valla DC, de Groen PC, et al. Determinants of survival and the effect of portosystemic shunting in patients with Budd–Chiari syndrome. Hepatology. 2004;39:500–8.
Dilawari JB, Bambery P, Chawla Y, et al. Hepatic outflow obstruction (Budd-Chiari syndrome): experience with177 patients and review of the literature. Medicine (Baltimore). 1994;73:21–36.
Kumar SI, Kumar A, Srivastava S, Saraswat VA, Aggarwal R. Low frequency of factor V Leiden and prothrombin G20210 A mutations in patients with hepatic venous outflow tract obstruction in northern India: a case-control study. Indian J Gastroenterol. 2005;24:211–5.
Singh V, Sinha SK, Nain CK, et al. Budd-Chiari syndrome: our experience of 71 patients. J Gastroenterol Hepatol. 2000;15:550–4.
Abd-El-Hamid N, Taylor RM, Marinello D, et al. Aetiology and management of extrahepatic portal vein obstruction in children: King’s College Hospital experience. J Pediatr Gastroenterol Nutr. 2008;47:630–4.
Janssen HL, Meinardi JR, Vleggaar FP, et al. Factor V Leiden mutation prothrombin gene mutation, and deficiencies in coagulation inhibitors associated with Budd-Chiari syndrome and portal vein thrombosis: results of a case-control study. Blood. 2000;96:2364–8.
Bhattacharyya M, Makharia G, Kannan M, Ahmed RP, Gupta PK, Saxena R. Inherited prothrombotic defects in Budd–Chiari syndrome and portal vein thrombosis: a study from North India. Am J Clin Pathol. 2004;121:844–7.
Mohanty D, Shetty S, Ghosh K, Pawar A, Abraham P. Hereditary thrombophilia as a cause of Budd–Chiari syndrome: a study from western India. Hepatology. 2001;34:666–70.
Deltenre P, Denninger MH, Hillaire S, et al. Factor V Leiden related Budd–Chiari syndrome. Gut. 2001;48:264–8.
Mahmoud AE, Elias E, Beauchamp N, Wilde JT. Prevalence of the factor V Leiden mutation in hepatic and portal vein thrombosis. Gut. 1997;40:798–800.
Yadav S, Dutta AK, Sarin SK. Do umbilical vein catheterization and sepsis lead to portal vein thrombosis? A prospective, clinical and sonographic evaluation. J Pediatr Gastroenterol Nutr. 1993;17:392–6.
Odievre M, Pige G, Alagille D. Congenital abnormalities associated with extraheptic portal hypertension. Arch Dis Child. 1977;52:383–5.
Pinto RB, Silveira TR, Bandenilli E, Rohsig L. Portal vein thrombosis in children and adolescents: the low prevalence of hereditary thrombophilic disorders. J Pediatr Surg. 2004;39:1356–61.
Sharma S, Kumar SI, Poddar U, Yachha SK, Aggarwal R, Factor V. Leiden and prothrombin gene G20210 A mutations are uncommon in portal vein thrombosis in India. Indian J Gastroenterol. 2006;25:236–9.
Seixas CA, Hessel G, Ribeiro CC, Arruda VR, Annichino-Bizzacchi JM, Factor V. Leiden is not common in children with portal vein thrombosis. Thromb Haemost. 1997;77:258–61.
Seixas CA, Hessel G, Siqueira LH, Machado TF, Gallizoni AM, Annichino-Bizzacchi JM. Study of hemostasis in pediatric patients with portal vein thrombosis. Haematologica. 1998;83:955–6.
Acknowledgments
The study was supported by an intramural research grant from the Sanjay Gandhi Postgraduate Institute of Medical Sciences for a research grant (to PR). The DNA sequencing facility in the authors’ department is supported by the Department of Science and Technology, Government of India under its FIST program. SM was supported by a research fellowship from the Indian Council of Medical Research, New Delhi. The authors also thank Dr. Renu Saxena, All India Institute of Medical Sciences, New Delhi, India, for providing a positive control specimen (the other positive control was generated in-house).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PR, PK, SM, and RA confirm that they have no conflict of interest to declare.
Ethics statement
The authors affirm that the study was performed in a manner confirming with the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning Human and Animal Rights, and that the authors followed the policy concerning informed consent as shown in Springer.com.
Rights and permissions
About this article
Cite this article
Rai, P., Kumar, P., Mishra, S. et al. Low frequency of V617F mutation in JAK2 gene in Indian patients with hepatic venous outflow obstruction and extrahepatic portal venous obstruction. Indian J Gastroenterol 35, 366–371 (2016). https://doi.org/10.1007/s12664-016-0691-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-016-0691-7