Abstract
Background
The incidence of common bile duct (CBD) calculi has been reported to be 8 % to 20 % among the patients with cholelithiasis. Failure to detect CBD stones on the part of the surgeon not only fails to relieve symptoms but also subjects them to potentially life-threatening complications such as cholangitis, pancreatitis or obstructive jaundice. Modalities for detection of CBD stones have evolved over time from CBD exploration based on clinical and operative findings to intraoperative cholangiography (IOC), to endoscopic retrograde cholangiopancreaticography (ERCP) and, recently, to magnetic resonance cholangiopancreaticography (MRCP) and endoscopic ultrasonography (EUS). We felt a need for a scoring system to predict a patient population having a higher risk of choledocholithiasis so that these modern interventions can be selectively utilized.
Setting
This study was performed in a tertiary care medical college hospital in a metropolitan city.
Design
This is a prospective observational study.
Methods
All patients with symptomatic cholelithiasis admitted to the hospital were included. Patients were diagnosed as having choledocholithiasis either by ultrasonography (USG), computed tomography scan, MRCP, EUS or ERCP and were followed up for at least 6 weeks.
Results
The prevalence of choledocholithiasis among the 275 patients with symptomatic biliary colic in our study was 18.9 % (n = 77). On bivariate analysis, dilated bile duct on USG (>6 mm), raised total bilirubin, raised alkaline phosphatase (ALP), raised amylase, raised SGPT and SGOT were significantly associated with choledocholithiasis (p < 0.05). On multivariate analysis also, all these factors except amylase and SGPT showed a significant correlation with choledocholithiasis (p < 0.05). These observations were used to build a scoring system consisting of four factors: dilated bile duct on USG (>6 mm), total bilirubin >2 mg/dL, ALP >190 IU/L and SGOT >40 IU/L.
Conclusion
A positive predictive value of 3 or more factors was over 95 %, necessitating an endoscopic intervention. A negative predictive value of the absence of any factor was 100 %, which ruled out CBD calculi. If only one or two factors are positive, then further evaluation is recommended preferably using non-minimal or minimal invasive investigations like EUS or MRCP.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Common bile duct (CBD) stones constitute the main etiology of non-malignant biliary obstructions. The quoted prevalence of CBD stones in patients with symptomatic gallstones varies but probably lies between 8 % and 20 % [1]. The manifestation of choledocholithiasis is variable. Patients may be asymptomatic or may present with severe abdominal pain with or without fever or jaundice and, at times, potentially life-threatening complications. More commonly, stones obstruct the lumen of the CBD, causing potentially life-threatening complications that may include obstructive jaundice, gallstone pancreatitis or ascending cholangitis. Fortunately, some patients with choledocholithiasis are spared by this degree of illness.
With the advent of ultrasound, an early diagnosis of cholelithiasis has been possible. Today, laparoscopic cholecystectomy (LC) is considered as the gold standard for treatment of cholelithiasis. However, a surgeon needs to rule out the presence of choledocholithiasis and treat the same if present. Historically, exploration of the CBD was recommended in patients with a history of jaundice or pancreatitis, operative findings of multiple gallbladder stones, single-faceted stone, dilated CBD and palpable stone in the bile duct. Observance of these criteria for CBD exploration led to a significant proportion of unnecessary CBD explorations, and a patient suffered complications like prolong T-tube drainage and biliary stricture [2].
To avoid these complications, intraoperative cholangiography (IOC) was introduced which meant the availability of a portable X-ray machine and increased operative time of 30 ± 10 min [3]. With the development of fibreoptic technology, endoscopic retrograde cholangiopancreaticography (ERCP) gradually replaced IOC as a preferred investigation for detection of choledocholithiasis [4]. The major advantage was its therapeutic role in clearing the CBD off stone and achieving drainage by stent insertion. However, when used as a diagnostic investigation alone, the risks of complications like pancreatitis, cholangitis and iatrogenic injuries were unacceptable. The development of magnetic resonance cholangiopancreaticography (MRCP) and endoscopic ultrasonography (EUS) has provided a safe alternative for detecting CBD stones. However, owing to the cost and the limited availability of these investigations, we felt a need for a scoring system to predict a patient population having a high risk of choledocholithiasis so that these modern interventions can be selectively utilized.
This study was designed to assess if common clinical, biochemical and imaging parameters predict the presence of CBD calculi in patients with gallstones.
Methods
The prospective observational study was conducted in a tertiary care medical college hospital in Mumbai from February 2014 to November 2015 after the approval by the institutional ethics committee. All patients admitted with a symptomatic gallstone disease, who were willing to participate, were screened for choledocholithiasis. Patients with incomplete data set were excluded.
All patients were initially evaluated with a detailed history of presenting symptoms like pain and vomiting and history of jaundice and pancreatitis, followed by detailed clinical examination. A blood work up of all these patients included complete hemogram, total and direct bilirubin, alkaline phosphatase (ALP), SGOT and SGPT, serum amylase and lipase, prothrombin time/international normalized ratio and blood urea nitrogen and creatinine. All the patients underwent chest X-ray–PA view and abdomen erect–AP view, transabdominal ultrasonography (USG) and contrast-enhanced computed tomography (CECT) to rule out other causes of abdominal pain. Patients with USG or CECT with oral contrast and blood investigations suspicious of choledocholithiasis underwent MRCP or EUS.
Choledocholithiasis was diagnosed by confirming the presence of stone in the bile duct in any of the imaging investigations (i.e. ultrasonography, CT scan, EUS or MRCP) or in ERCP. The first-line management of choledocholithiasis was endoscopic clearance (with or without stenting). Whenever an endoscopic clearance was not successful, open CBD exploration with T-tube drainage or biliary-enteric bypass was carried out. Cholecystectomy was performed by an open technique whenever a laparoscopic approach was not possible or whenever open bile duct exploration was conducted. All the blood investigations done on admission were repeated 6 weeks post intervention and compared. Six weeks post intervention, follow up USG was done to evaluate the gallbladder fossa/bile duct status/liver parenchyma and to assess for residual stones or bile duct calculi in patients previously operated for cholelithiasis.
Patients were grouped according to an age range of 20–40, 41–60 and >60 years, and its association with choledocholithiasis was analyzed. Gender of the patients as well as history of pancreatitis and cholangitis were documented. Blood investigations like ALP, total bilirubin and amylase were dichotomised at 180 IU, 2 mg/dL and 90 IU, respectively, based on the institutional cut-off values. SGOT and SGPT were also dichotomised and associated at 40 IU each, and its association with choledocholithiasis was analyzed. Patients having a CBD size of >6 mm on USG were considered to have a dilated CBD, and its association with the diagnosis of choledocholithiasis was also studied. The cohort of patients with choledocholithiasis was compared to the cohort of patients having gallbladder stones alone. The parameters/variables compared were age, gender, history of jaundice or pancreatitis or cholangitis, liver function tests, serum amylase and CBD size on ultrasonography.
Categorical and nominal variables were compared using chi-square and Fisher’s exact tests. Variables that were found in the bivariate analyses to have a statistically significant (p < 0.05) prediction of choledocholithiasis were included in the multiple predictors logistic regression to identify the independent effect of these variables on the diagnosis of choledocholithiasis.
ERCP was considered as the gold standard for diagnosing choledocholithiasis, and all the patients of biliary colic were followed up at 6 weeks to further undergo blood investigations and USG to diagnose any missed CBD stones.
Results
Of the 407 patients of symptomatic gallstone disease satisfying the inclusion criteria, 77 patients were diagnosed of choledocholithiasis from a period of February 2014 to November 2015. Thus, the prevalence of choledocholithiasis was 18.9 %. The age range was from 22 to 79 years [mean age of 40.1 years, standard deviation (SD) of 1.934, median of 39 years, interquartile range (IQR) of 32–47 years]. There were 98 men (24 %) and 309 women (76 %).
The results of comparison of patients of gallstone disease with and without CBD calculi are shown in Table 1.
On bivariate analysis, dilated bile duct on USG (>6 mm), total bilirubin >2 mg/dL, amylase >90, ALP >190 IU/L and SGPT and SGOT >40 IU/L were significantly associated with choledocholithiasis (p < 0.05) (Table 1). A multivariable logistic regression analysis was done to negate the influence of the above-mentioned predictors on each other, the result of which is presented in Table 2. The accuracy of prediction for this model was 98.3 %. The relationships between these factors with the diagnosis of choledocholithiasis were expected as per bivariate analysis in Table 1, except amylase and SGPT which did not show a significant correlation with choledocholithiasis (p < 0.05). The positive predictive value (PPV) and negative predictive value (NPV) of each of these predictors found to be positive on logistic regression are documented in Table 3.
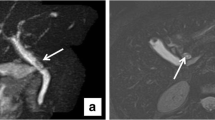
When considered individually, these factors had variable positive and negative predictive values in diagnosing choledocholithiasis and, hence, these observations were used to build a scoring system consisting of four factors: dilated bile duct on USG (>6 mm), total bilirubin >2 mg/dL, ALP >190 IU/L and SGOT >40 IU/L. Each of these predictors was given a score of 1. The scoring system was applied to all patients with acute biliary pain. Based on the number of factors found positive, each patient was assigned a score. The utility of this scoring was studied by assessing the positive and negative predictive values of diagnosing choledocholithiasis of each set of scores as shown in Table 4. Our observations suggest that the scoring system is useful in predicting the presence of bile duct stones: a score of 0 practically rules out the presence of choledocholithiasis (NPV = 100 %) whereas a score of 3 and 4 has a predictive value nearing 100 % in diagnosing choledocholithiasis. Figure 1 shows the distribution of patients with choledocholithiasis with respect to the scoring system.
Discussion
The prevalence of choledocholithiasis among the patients with symptomatic biliary colic in our study was 18.9 %. The median age was 39 years with 76 % of choledocholithiasis patients being females. On bivariate analysis, dilated bile duct on USG (>6 mm), total bilirubin >2 mg/dL, amylase >90, ALP >190 IU/L and SGPT and SGOT >40 IU/L were significantly associated with choledocholithiasis (p < 0.05), whereas on multivariable logistic regression analysis, the predictors of choledocholithiasis include dilated bile duct on USG, total bilirubin, ALP and SGOT.
The review of literature reveals that ALP, total bilirubin (T Bil), SGOT, SGPT and gamma-glutamyl transpeptidase (GGT) and dilated CBD on USG have been considered as predictors of choledocholithiasis [1, 5–11]. However, most of these studies were retrospectively analyzed and were criticised to include only a subset of patients having a high risk of choledocholithiasis. A large prospective study by Videhult et al. analyzed these biochemical parameters in a cohort of patients with symptomatic cholelithiasis which found ALP and total bilirubin to predict choledocholithiasis [7]. Our results were similar to the study conducted by Sgourakis et al. in 2004 to evaluate predictors of choledocholithiasis [11].
The positive and negative predictive values of the variables found to be significantly associated with the diagnosis of choledocholithiasis were analyzed (Table 3). Although the negative predictive value of these variables was high, the positive predictive values of SGOT (56 %), ALP (82 %) and dilated CBD on USG (78 %) were low. This meant that a significant number of patients having choledocholithiasis would be missed if these predictors were considered independently. This would thereby subject patients to potentially life-threatening complications that may include obstructive jaundice, gallstone pancreatitis or ascending cholangitis, owing to the delayed diagnosis of choledocholithiasis. Thus, a need of an accurate scoring system combining these variables arose.
Previously, Menezes et al. attempted to predict choledocholithiasis preoperatively using a scoring system; however, owing to its complexity, it was rarely used clinically [12]. Barkun et al., while predicting patients needing preoperative ERCP, found age >55, raised total bilirubin and CBD stone and/or CBD dilatation on USG. The predictive value ranged from 8 % when none of these factors were present to 94 % when all these factors were present [5].
While in the process of analysing our data on a symptomatic gallstone disease, we came across a scoring system to predict bile duct calculi by Sherman et al. [13]. Our scoring system was designed on similar grounds.
Our observations suggest that the scoring system is useful in predicting the presence of bile duct stones: a score of 0 practically rules out the presence of choledocholithiasis, and thus, a patient can go ahead with cholecystectomy. A score of 1 and 2 with low predictive values indicates the need for further imaging like MRCP or EUS in patients with acute biliary pain, while patients with a score of 3 and 4 with a predictive value of nearly 100 % confirm the diagnosis of choledocholithiasis, thus needing endoscopic, laparoscopic or open surgical exploration to deal with the presence of bile duct calculi (Fig. 1).
This scoring system would avoid the unnecessary ERCP and thereby its complications as also expensive and time-consuming investigations like EUS and MRCP could be used selectively. Along with the advantage of diagnosing choledocholithiasis with basic biochemical and radiologic parameters in most of the cases, this study also intends to evade the need of time-consuming intraoperative cholangiography.
In order to increase the frequency of detection of CBD stone intraoperatively, few surgeons started to use intraoperative cholangiography and laparoscopic USG. However, because it adds to the operative time and to the risk of radiation exposure, many surgeons use intraoperative cholangiography selectively during the performance of a cholecystectomy. Relying only on intraoperative cholangiography can be disappointing, with 2 % to 3 % false-negative and about 2 % false-positive results [9]. In one of the more notable recent experiences, Collins et al. in 2004 identified filling defects consistent with stones in 4.6 % of patients [14]. In these patients, access was maintained for the performance of postoperative cholangiograms. At 48 h, 26 % of patients had a normal cholangiogram, and an additional 26 % had evidence for passage of the stones by 6 weeks, thus highlighting its limited role in symptomatic choledocholithiasis [14]. Noting this, none of the patients from among the cohort of symptomatic cholelithiasis in our study underwent cholangiography. However, all the patients were followed up with blood investigations and liver function tests at 6 weeks to check for residual or recurrent stones in the CBD.
Also, it is now recognized that postoperative ERCP is usually successful, and as the National Institutes of Health consensus noted, the overall rate of morbidity is the same as when ERCP precedes surgery [15]. Thus, even if the scoring system failed to detect CBD stones, post-cholecystectomy ERCP does remain an option.
GGT which has been considered by previous studies as an important predictor of choledocholithiasis was not assessed which may be a limitation of this study. Also, although all patients with symptomatic cholelithiasis were followed up with blood work up and USG at 6 weeks, no confirmatory tests like MRCP or EUS were done in these patients to definitely conclude that these patients did not have choledocholithiasis which may be a weakness of this study. This study needs to be followed up by a prospective study to validate this scoring system before this system can be accepted in clinical practice.
Surgeons have been familiar with biochemical and USG criteria to predict the presence of CBD stones. Rapidly developing medical technologies that prompt new and costly diagnostic options coexist with scarce financial resources in a developing nation. The optimal allocation of these scarce resources means that these technologies should be used rationally, only when they are likely to improve patient care. This scoring system strengthens interest in low-cost non-invasive diagnostic test for choledocholithiasis. Surgeons have long been familiar with clinical and biochemical criteria to predict the presence of common bile duct stones.
References
Tozatti J, Mello AL, Frazon O. Predictor factors for choledocholithiasis. Arq Bras Cir Dig. 2015;28:109–12.
Ahmed R, Duncan MD. The Management of common bile duct stones. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. Elsevier Inc. Philadelphia. PA; 2014. pp. 391-5.
Shojaiefard A, Esmaeilzadeh M, Ghafouri A, Mehrabi A. Various techniques for the surgical treatment of common bile duct stones: a meta review. Gastroenterol Res Pract. 2009;2009:840208.
Kessler RE, Falkenstein DB, Clemett AR, Zimmon DS. Indications, clinical value and complications of endoscopic retrograde cholangiopancreatography. Surg Gynecol Obstet. 1976;142:865–70.
Barkun AN, Barkun JS, Fried GM, et al. Useful predictors of bile duct stones in patients undergoing laparoscopic cholecystectomy. McGill Gallstone Treatment Group. Ann Surg. 1994;220:32–9.
Notash AY, Salimi J, Golfam F, Habibi G, Alizadeh K. Preoperative clinical and paraclinical predictors of choledocholithiasis. Hepatobiliary Pancreat Dis Int. 2008;7:304–7.
Videhult P, Sandblom G, Rudberg C, Rasmussen IC. Are liver function tests, pancreatitis and cholecystitis predictors of common bile duct stones? Results of a prospective, population-based, cohort study of 1171 patients undergoing cholecystectomy. HPB (Oxford). 2011;13:519–27.
Yang MH, Chen TH, Wang SE, et al. Biochemical predictors for absence of common bile duct stones in patients undergoing laparoscopic cholecystectomy. Surg Endosc. 2008;22:1620–4.
Prat F, Meduri B, Ducot B, Chiche R, Salimbeni-Bartolini R, Pelletier G. Prediction of common bile duct stones by noninvasive tests. Ann Surg. 1999;229:362–8.
Byrne MF, McLoughlin MT, Mitchell RM, et al. For patients with predicted low risk for choledocholithiasis undergoing laparoscopic cholecystectomy, selective intraoperative cholangiography and postoperative endoscopic retrograde cholangiopancreatography is an effective strategy to limit unnecessary procedures. Surg Endosc. 2009;23:1933–7.
Sgourakis G, Dedemadi G, Stamatelopoulos A, Leandros E, Voros D, Karaliotas K. Predictors of common bile duct lithiasis in laparoscopic era. World J Gastroenterol. 2005;11:3267–72.
Menezes N, Marson LP, Debeaux AC, Muir IM, Auld CD. Prospective analysis of a scoring system to predict choledocholithiasis. Br J Surg. 2000;87:1176–81.
Sherman JL, Shi EW, Ranasinghe NE, Sivasankaran MT, Prigoff JG, Divino CM. Validation and improvement of a proposed scoring system to detect retained common bile duct stones in gallstone pancreatitis. Surgery. 2015;157:1073–9.
Collins C, Maguire D, Ireland A, Fitzgerald E, O’Sullivan GC. A prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisited. Ann Surg. 2004;239:28–33.
Rhodes M, Sussman L, Cohen L, Lewis MP. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351:159–61.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SUK, SBD, and VK declare that they have no conflict of interest.
Ethics statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kamath, S.U., Dharap, S.B. & Kumar, V. Scoring system to preoperatively predict choledocholithiasis. Indian J Gastroenterol 35, 173–178 (2016). https://doi.org/10.1007/s12664-016-0655-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-016-0655-y