Abstract
Background
One of the main objectives of the reconstruction of oral deformities is the return of form and function. There are many alternatives, including, forehead, pectoralis major myocutaneous, submental, and various free flaps depending on the need. Local flaps are technically easy and less time consuming. Because the facial artery is ligated in the cases of oral cancer surgery, the nasolabial flap (NLF) is not commonly considered. Therefore, our research question was to evaluate the survival of randomly patterned inferior-based nasolabial flaps.
Materials and Method
Nineteen patients were included in this retrospective study. All the cases were of early stage (T1, T2) involving alveolar, buccal mucosa, and tongue. The transverse facial, superior, and inferior labial arteries of both sides including perforators were evaluated using colour Doppler ultrasonography. In every instance, ipsilateral facial artery ligation was performed. A double-staged, inferiorly based NLF was used for reconstruction. Patients were followed up to 6–12 months for the reconstructed part.
Results
Out of 19 patients, Doppler study revealed rich vascular supply in 14 patients. Out of 19 surgeries, 9 flaps survived well with intact skin pedicle, 7 patients had partial necrosis at the tip of flap, and 3 flaps were totally necrosed.
Conclusion
Modiolus (corner of mouth) which is a chiasma of 9 facial expression muscles, is supplied by muscular branches of facial artery and anastomosed by transverse facial artery and ipsilateral and contralateral superior labial artery. After facial artery ligation, these muscular branches of the chiasma of muscles are responsible for the survival of inferiorly oriented random-patterned NLF after MRND. This is because the muscular branches of the facial artery provide an alternate blood supply to the modiolus and its associated muscles. This helps to prevent necrosis or tissue death in the area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the head and neck region, squamous cell carcinoma (SCC) is the most prevalent malignancy (90%) [1]. The most prevalent primary sites for SCC in the oral cavity are the buccal mucosa, mandibular alveolus, and tongue, while the peritonsillar area is the least frequent site [2]. Since the dawn of time, oncologists have puzzled over how to restore the damage caused by excision in cases of oral cancer. The secondary prevention of oral cancer and quality of life (QOL) are significantly impacted by surgical defect reconstruction. There are numerous treatment options, including pectoralis major myocutaneous (PMMC), forehead flaps, and vascularized free flaps. A few authors have also mentioned the usage of buccal fat pads in addition to these. NLF is less common among surgeons while treating OSCC patients due to the ligation of the facial artery. The most popular form of local flap, the inferiorly based nasolabial flap, was successfully used in the current study to reconstruct the buccal mucosa (BM), the alveolo-buccal complex (ABC), and other areas of the oral cavity in OSCC patients who underwent surgery. This retrospective investigation allowed us to demonstrate the results of NLF following facial artery ligation.
Material and Methods
This retrospective study included 19 OSCC patients who had undergone surgery between July 2021 and July 2022. Through case sheets and the operation register, histopathological information including surgical margin, depth of invasion, neural involvement, nodal metastasis, systemic metastasis, age, sex, tobacco chewing history, site, size of lesion, records related to preoperative investigation like colour Doppler of area near angle of mouth, and records of flap success were documented.
Inclusion criteria
-
1.
SCC of buccal mucosa (BM), alveolo-buccal complex (ABC), and other sites of oral cavity.
-
2.
Clinically stage T1, T2, and N0 disease reconstructed with nasolabial flap.
-
3.
Age in between 30 and 60 years.
Exclusion criteria
-
1.
Flap other than nasolabial flap.
-
2.
Follow-up time not recorded in case sheet
Flap Design
The dimensions of the flap were determined by the extent of the defect and were marked superiorly from 5 mm lateral to the medial canthus up to 1 cm below the oral commissure. The medial edge of the flap was in the nasolabial groove. To ensure the flap had a rich vascular supply, the base of the flap was identified before surgery using colour Doppler (Fig. 1).
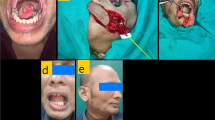
Surgical Technique
After MRND and wide local excision, incision was made in a downward motion, moving from superior to inferior. Dissection was performed from 5 mm lateral to the medial canthus before the flap was elevated to protect the angular artery (Figs. 2, 3).
When elevating the flap, the infraorbital nerve that extends 8 to 10 mm inferior to the infraorbital margin should be retained. After a thorough dissection, the flap was raised superficially to the mimicking muscles, such as the levator superioris and zygomaticus, leaving the nasal periosteum behind. The superior and inferior labial arteries were protected as they descend. Elevation of flap was performed in such a way that perforators arising from modiolus, and superior labial artery should be preserved. A transbuccal tunnel flap was positioned over the defect and sutured. Donor site was mostly closed off without any obvious deformities. The needle prick test was used appropriately for flap monitoring. The flap was parted, and the tunnel was sealed after 3 weeks.
Results
Clinically, each patient was at a T1 or T2 N0 M0 stage. Age- and sex-related demographic data, relationships with nearby arteries, pathological staging, flap outcome, and post-operative radiation effects were all compared.
Demographic Data, Location of the Lesion, and TNM staging
Twelve (63.2%) of the 19 cases were males, while 7 (36.8%) were females. 68.4% of cases were older than 40 years, whereas 31.6% were younger than 40 years. In 42.1% of cases, the defect location was ABC, while in 36.8% of cases, it was BM. Other locations were discovered in 21.1% of instances. The proportions of T1, T2, and T3 histopathological staging were 31.6%, 47.4%, and 21.1%, respectively.
Relation with Adjacent Arteries
Conjunction with adjacent arteries was found in 73.7% cases and absent in 26.3% of cases.
Adjuvant Radiotherapy
Adjuvant radiotherapy was done in 68.4% cases out of 19 cases.
Flap Morbidity
Out of 19 cases, 9 (47.4%) flaps survived, 36.8% cases partial necrosis was observed in flaps, while in 15.8% cases, complete necrosis was found (Fig. 4).
Post-operative Results
Ectropion was found in 4 (21.1%) cases, while Fistula in 15.8% cases. There was no recurrence in any of the cases.
Flap Morbidity with Influencing Factors
Flap morbidity was not significantly associated with gender (p = 0.325), age (p = 1.000), defect site (p = 0.073), histopathological stage (p = 0.421), or adjuvant radiotherapy (p = 1.000). A strong correlation was found in conjunction with adjacent arteries at modiolus area and flap mortality (p = 0.030). All flap survival was seen in the presence of neighbouring arteries (Table 1).
Discussion
The inferiorly based nasolabial flap is an axial patterned flap supplied by the subdermal plexus of the facial artery, some maxillary artery branches, and the transverse facial artery. Facial artery conservation is not in routine practice in oral squamous cell carcinoma, during neck dissection. All 19 operated cases of OSCC were treated with NLF in this retrospective study. Patients were included in the study after being evaluated on the basis of inclusion criteria. Since most OSCC cases were diagnosed and treated at an advanced stage, only 19 patients met the inclusion criteria [3]. Observations have been made in terms of gender, age, defect site, pathological size (T stage), and conjunction with adjacent and contralateral arteries. After analysing all the data, we found that males were involved in a higher percentage (63.2%) than females (36.8%), involving buccal mucosa (36.8%) and ABC (42.1%). Most of the patients (68.4%) were in their fifth or sixth decade of life. Tobacco chewing and placing it in the buccal vestibule is the primary cause of oral cancer in India. Furthermore, males are more prone to oral cancer, and the incidence rises with age [2, 4]. Our data are suggestive of a similar outcome as available in literature regarding the demographics of OSCC. T2 histopathological size (47.4%) was dominated by small- or intermediate-sized defects.
For ideal reconstruction, flap dimensions should be good enough for the defect size, depth, location, and type of tissue needed, so inferiorly based NLF is most suitable for clinically T1 and T2 and intermediate-sized defects in OSCC patients. Lazaridis et al. have reported a 100% survival rate of nasolabial flap in OSCC of buccal mucosa [5]. This study concluded that patient-specific anatomic factors play a crucial role in the positive outcome of inferiorly based NLF in OSCC patients. The relationship with adjacent vascular channels such as the transverse facial artery, inferior labial artery, and ipsilateral and contralateral superior labial artery played a significant role in the survival of random patterned NLF (p = 0.030) (Table 1). This relationship of arteries makes a well-vascularized area at the corner of the mouth, supplying the chiasma of nine facial muscles, making the pedicle of a flap that doesn’t depend totally on the facial artery for its vascular supply. Herbert and Harrison discussed the rich collateral blood supply of the cheek. He also said that tying off the facial artery on the same side is not a reason to not do inferiorly based NLF [6].
Before planning for random patterned NLF, colour Doppler of an area of 2 × 3 cm near the angle of the mouth is an important pre-operative investigation. All the patients in this retrospective study underwent colour Doppler and 14 patients reported rich vascular supply by the conjunction of adjacent and contralateral arteries. In the remaining 5 patients, USG failed to locate adequate perforators and anastomoses of vascular channels. Out of 19 patients, 9 flaps survived totally, 7 had partial necrosis at the tip of the flap without any loss of pedicle, and 3 flaps were lost within 3 weeks of surgery. Totally necrosed flaps (15.8%) showed poor correlation with arteries in the pre-operative colour Doppler test in comparison with those flaps that survived or partially necrosed. The above data is more convincing, stating that in facial artery ligation, inferiorly based NLF will give a positive outcome only if there is rich vascularity adjacent to corner of mouth. Gunnarsson et al. also used a modiolus perforator-based flap, but facial artery ligation was not performed in any of his cases.[7]. Hamdy H. El-Marakby et al. performed facial artery ligation in only 10% of cases and stated that the reason for flap survival was the high vascularity of the face [8]. Similarly. according to Chitlangia P et al. and Estefania Alonso-Rodriguez et al., there is a strong vascular anastomosis on the face that has accounted for the survival of random patterned NLF. However, in the present study, 10 flaps showed signs of necrosis where colour Doppler failed to locate adequate perforators at the modiolus.
Thirteen patients underwent adjuvant radiotherapy according to the NCCN guidelines. Though there was no significant association between post-operative radiotherapy and survival of the flap (p = 1.000). Literature strongly suggests that NLF is a good choice for reconstruction in oral carcinoma patients, and its blood supply is not affected by post-operative radiotherapy (Fig. 5). [11, 13]
Varghese et al. [12] mentioned that there is a detrimental effect of radiation on endothelial cells of the subdermal plexus of the flap and surrounding tissues, causing post-radiotherapy complications of the flap-like fistula formation over the donor site. In the present study, two flaps were necrosed completely and five flaps were partially necrosed. Necrosed flaps had less perforators at the modiolus in USG. This suggests that the presence of adequate perforators at the modiolus can help prevent complete necrosis of the flaps, after radiotherapy, thus increasing the success rate of the surgery.
Ectropion was reported in 4 cases that was possibly due to extension of the flap design superiorly, closer to the medial canthus because of the greater requirement of donor tissue to fill the defect. There were no reported cases of recurrence. As in cases of SCC of the buccal mucosa, a pre-operative CT is required to rule out the proximity of the skin of the cheek and depth of the lesion. [13] Furthermore, as T size increases, so does the requirement for flap size, resulting in closer proximity of the flap design to the medial canthus as well as more tension in the closing donor site, resulting in post-operative secondary deformity.
Conclusion
In conclusion we cannot rely upon rich vascular anastomosis of face to harvest random-patterned NLF. Additionally, an ultrasound scan before surgery helps to identify the appropriate perforators (perforators may be lacking also) to ensure a successful flap outcome. This retrospective study showed that if the chiasma of muscles at the modiolus and branches of the superior labial artery were kept intact during surgery, the flap had a better chance of surviving. Base of the pedicle should be positioned at the modiolus to ensure optimal blood flow to the flap. There are some limitations of NLF in onco-surgery, such as the absence of bulk and poor function, especially in cases of posterior mandibles where the mandible deviates towards the side that was resected.
References
Vigneswaran N, Williams MD (2014) Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral Maxillofac Surg Clin 26(2):123–141. https://doi.org/10.1016/j.coms.2014.01.001
Tandon P, Dadhich A, Saluja H, Bawane S, Sachdeva S (2017) The prevalence of squamous cell carcinoma in different sites of oral cavity at our Rural Health Care Centre in Loni, Maharashtra—a retrospective 10-year study. Contemp Oncol 21(2):178–183
Jeihooni AK, Jafari F (2021) Oral cancer: epidemiology, prevention, early detection, and treatment. In: Sridharan G (ed) Oral cancer—current concepts and future perspectives. IntechOpen, London. https://doi.org/10.5772/intechopen.99236
Sharma S, Satyanarayana L, Asthana S, Shivalingesh KK, Goutham BS, Ramachandra S (2018) Oral cancer statistics in India on the basis of first report of 29 population-based cancer registries. J Oral Maxillofac Pathol 22(1):18–26. https://doi.org/10.4103/jomfp.JOMFP_113_17
Lazardis N, Tilaveridis I, Karakasis D (2008) Superiorly or inferiorly based islanded nasolabial flap for buccal mucosa defects reconstruction. J Oral Maxillofac Surg 66:7–15
Herbert DC, Harrison RG (1975) Nasolabial subcutaneous pedicle flaps. Br J Plast Surg 28:85
Gunnarsson GL, Thomsen JB (2016) The versatile modiolus perforator flap. Plast Reconstr Surg Global Open 4(3):661
El-Marakby HH, Fouad FA, Ali AH (2012) One stage reconstruction of the floor of the mouth with a subcutaneous pedicled nasolabial flap. J Egypt Natl Canc Inst 24:71–76. https://doi.org/10.1016/j.jnci.2012.02.002
Chitlangia P, Kumuran E, Sabitha KS (2012) Use of nasolabial flap in intra and extraoral reconstruction: our experience with 40 cases. J Maxillofac Oral Surg 11(4):451–454. https://doi.org/10.1007/s12663-012-0336-z
Alonso-Rodríguez E, Cebrián-Carretero J-L, Morán-Soto M-J, Burgueño García M (2014) Versatility of nasolabial flaps in oral cavity reconstructions. Med Oral Patol Oral Cir Bucal. 19(5):e525–e530. https://doi.org/10.4317/medoral.19376
Singh S, Singh RK, Pandey M (2012) Nasolabial flap reconstruction in oral cancer. World J Surg Oncol 10:227
Varghese BT, Sebastian R, Cherian T, Mohan RM, Ahmed I, Koshy CM, Thomas S (2001) Nasolabial flaps in oral reconstruction: an analysis of 224 cases. Br J Plast Surg 54:499–503
Chandraiah RB, Hoda N, Ghosh S, Sabitha KS, Nathani J, Bhattiprolu VD (2020) Versatility of the inferiorly based nasolabial flap for reconstruction in early oral cancer patients: our experience in a tertiary cancer centre. Int J Otorhinolaryngol Head Neck Surg 6(12):2207. https://doi.org/10.18203/issn.2454-5929.ijohns20205060
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
USP helped in conceptualization; SKY helped in methodology; HM done formal analysis, investigation, and writing—original draft preparation; VK done writing—review and editing; Funding acquisition was done by none; MVS helped for resources; SK contributed to supervision.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The institutional ethics committee approved the study, which was conducted in conformity with the ethical guidelines specified in the 1964 Declaration of Helsinki. The reference code for the study is 115 ECM IIA/P 31.
Consent to Publish
I declare that I have read all your terms and conditions and I provide my consent to publish this article in your journal.
Consent to Participate
This study was conducted after getting institutional ethical approval and informed consent from the participant.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pal, U.S., Maurya, H., Yadav, S.K. et al. Nasolabial flap: Reconstruction in Oral Cancer—An Unfolding Fact of Survival. J. Maxillofac. Oral Surg. (2023). https://doi.org/10.1007/s12663-023-01961-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-023-01961-0