Abstract
In this era of microvascular expertise, free flaps are the preferred option by reconstructive surgeons but has technical limitation in rural set up. Nasolabial flaps has been widely mentioned in literature for smaller defect reconstruction with minimal morbidity. It is a robust flap for soft tissue reconstruction in early stage lesion of oral cavity. We present a series of single stage oral cavity reconstruction using inferiorly based islanded nasolabial flaps in small to moderate soft tissue defects. This is a retrospective study which included biopsy proven 10 patients diagnosed with early stage oral cavity malignancy. All the patients underwent single stage islanded nasolabial flap for small to moderate oral defects. Follow up of all patients were recorded with respect to clinical photographs, mouth opening, tongue mobility, deglutition, speech and patient satisfaction. All operated patients had good functional outcome in terms of swallowing, speech and tongue mobility. All patients were satisfactory with the postoperative results. In early stage oral malignancy patients, this option justifies a reliable and cost effective approach. Inferiorly based islanded nasolabial flaps provides a single stage, safer, faster and reliable option for small to moderate oral cavity defects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Out of all the reported oral malignancy cases, major burden belongs to rural population of central India. This can be attributed to lack of awareness and chronic tobacco chewing habits [1]. Early detection and diagnosis in oral malignancy patients is an important step to be followed in our health care system with special focus on disease burden areas. At present, up to 50% patients are detected at later stages, which increases their morbidity and mortality [2]. In this era of microvascular expertise, free flaps are the preferred option by reconstructive surgeons but has technical limitation in rural set up [3]. Although, complex defects need microvascular reconstruction or regional pedicled flaps yet early stage lesions can be dealt with local tissue reconstruction as per the reconstruction ladder [4]. Oral cavity defects require a functional and aesthetic reconstruction. The type of reconstruction determines the quality of life in operated patients. Other options for early lesions like primary closure, secondary intention healing with mucosalisation and coverage with split thickness skin grafts are prone for complications like trismus, wound dehiscence and infection [5].
One of the local flaps like “Nasolabial flaps” has been widely mentioned in literature for smaller defect reconstruction in oral cavity [6]. This flap was first described in Sushruta Samhita text in 600BC, for coverage of facial defects. It is a robust flap for soft tissue reconstruction in early stage lesion of oral cavity. This flap incorporates the redundant skin of the nasolabial and nasofacial groove responsible for minimal donor site morbidity especially in elderly patients. Based on angiogram study, this is a random pattern flap nourished by rich sub-dermal plexus. Perforators from facial, lateral nasal, transverse facial, infraorbital and angular vessels anastomose to form an extensive sub dermal plexus which are oriented along angular artery axis. Hence, it can be harvested like true axial pattern flaps. These perforators are specially concentrated in inferior two-third of nasolabial groove, which forms the basis of inferiorly based flaps for intraoral soft tissue reconstruction [7]. This flap survives even after facial artery ligation though its preservation increases flap reliability [8]. In small to moderate oral cavity defects after wide local excision, inferiorly based islanded nasolabial flaps provide a safer, faster and reliable option in alternative to sophisticated microvascular free tissue transfer. It can be used for reconstruction of various oral cavity defects like buccal mucosa, palate, floor of mouth, vestibule, tongue and maxillary /mandibular alveolar defects. It is preferable in edentulous patients with oral malignancy [5]. It provides a safer option for elderly patients with medical comorbidities, where long duration anaesthesia as in microvascular reconstruction is avoided.
In this article, we present a series of single stage oral cavity reconstruction using inferiorly based islanded nasolabial flaps in small to moderate soft tissue defects.
Patients and Methods
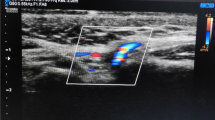
This study included biopsy proven 10 patients diagnosed with early stage oral cavity malignancy. These patients are retrieved from rural camps regularly conducted by JNMC Sawangi, Wardha in adjacent remote areas to facilitate early detection of oral malignancy. Data analysed retrospectively from operated patient records. All patients got operated in Department of ENT from July to December 2019. All these patients underwent single stage islanded nasolabial flap for small to moderate sized defect with neck dissection. All the intraoral defects were partial thickness, less than 4 cm in width and less than 6 cm in length. Information regarding patient registration, preoperative clinical photos, clinical examination findings, necessary investigation, treatment details and associated complications were collected from patient records (Tables 1 and 2). Patients were referred for post-operative adjuvant radiotherapy, if indicated. Follow up of all patients were recorded with respect to clinical photographs, mouth opening, tongue mobility, deglutition, speech and patient satisfaction. We tried to follow up these patients up to 6 months after discharge.
Surgical Technique
After neck node dissection and primary tumour excision, specimen sent for frozen section for negative margins. Depending on the defect size, ipsilateral islanded nasolabial flaps planned. Flap dimensions can be extended maximum up to 15 mm from medial canthus (superior limit) and 1 cm from mandibular border (inferior limit) depending on defect. Facial artery is preserved meticulously in all cases during neck dissection. After infiltration of 1:2 lac normal saline-adrenaline infiltration, incision deepened till subcutaneous layer. Thereafter, flap is harvested above superficial musculo-aponeurotic layer (SMAS) using needle tip monopolar cautery. Flap is islanded around subcutaneous pedicle near modiolus with approx. diameter of 1 cm. Flap is transferred gently through adequate buccal tunnel into oral cavity defects of buccal mucosa, palate, floor of mouth, alveolar defects and defects of lower gingivo-labial and gingivo-buccal sulcus defects [9]. Palatal defects can be addressed only in edentulous patients. For defects of tongue and floor of mouth in dentulous patients, we have used a newer technique by skeletonizing the facial vascular pedicle inferiorly and tunnelling the flap with pedicle behind the mandible. This technical modification improves distal reach of the flap [10]. After flap tunnelisation, check for any venous congestion for few minutes. Slight mobilisation of subcutaneous tissue inferiorly and widening of tunnel is required if flap is found congested. Flap is insetted onto intraoral defect with vicryl 2–0 suture. Closure of the donor defect is done in two layers aesthetically with vicryl 3–0 and prolene 4–0. Closure of neck wound after drain placement.Post operatively nasogastric tube feeding is started from next day. Flap is monitored up to 24 h for any congestion. Distal most sutures of flap are opened if there is any evidence of venous congestion. Frequent gargles and good oral cleaning is advised in the postoperative period. Patients are discharged once intraoral and neck sutures are healed usually up to 7–10 days.
Results
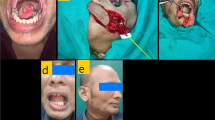
Out of 10 operated patients, 9 patients underwent ipsilateral flap reconstruction and one patient underwent bilateral flap reconstruction. This patient had severe oral sub-mucous fibrosis (OSMF) with left side buccal malignancy. The patient was managed with bilateral islanded nasolabial flap for left side buccal mucosal defect reconstruction and right side for OSMF release and adequate mouth opening was achieved. We had operated seven male and three female patients with early stage oral malignancy. Their age ranges between 35 and 65 years. Out of them, 7 patients had medical comorbidities like hypertension, diabetes, cardiovascular disease and Australian antigen positivity. All the operated patients were dentulous. We had used this flap for coverage of three buccal defects, three lateral tongue defects, two lower gingivo-buccal sulcus with marginal mandibulectomy defects and 2 gingivo-labial sulcus defect. We have reconstructed partial thickness defects with maximum dimensions up to 6 cm in length, 4 cm in width. Ipsilateral facial artery was preserved in every patient. Out of 10, 3 of them had verrucous carcinoma on biopsy. Rest of them had squamous cell carcinoma (4 well-differentiated and 3 moderately differentiated) and underwent neck dissection respectively. All the operated patients had T2/T3 disease with N0/N1 nodal status on histopathology. Maximum duration of surgery including wide local excision, neck dissection and flap reconstruction was 4 h. Maximum duration of hospital stay postoperatively was 10 days. One patient with lower vestibule reconstruction had venous congestion after 6 h which was managed by opening the distal most sutures hitched to the anterior alveolus and residual defect was left for mucosalization. None of the patients had flap failure. All operated male patients had complaints of hair growth over flap which became sparse after postoperative radiotherapy. All operated patients had satisfactory results (Figs. 1, 2 and 3). Patients with buccal mucosal reconstruction had adequate mouth opening more than two finger. Patients with lateral tongue defect reconstruction had adequate tongue mobility, comprehensive speech and able to swallow solids and liquids.
Discussion
Vascular basis of nasolabial flap has been documented by many authors in literature. This flap can be harvested with little technical expertise, less duration of surgery and minimal risk of complications. It can be used as a good alternative to free flap in small to moderate defects in patients with medical comorbidities especially in centres with limited technical expertise [4]. The flap survives even if ipsilateral facial artery has been ligated during neck dissection [3, 8]. Hence it has been used as a backup option in failed free flaps for small to moderate defect. Utility of nasolabial flaps in buccal mucosa reconstruction has been shown in various studies [11]. Partial Defects of buccal mucosa and vestibule needs to be replaced by a thin, pliable flap. Bulky flaps in moderate defects hamper potential space of oral cavity. Attempts of primary closure or skin grafting in such cases leads to tissue contracture and restricts mouth opening. Most preferred option in such cases is free radial artery forearm flap with microvascular anastomosis [12]. Islanded nasolabial flaps can be used for such partial defects in a single stage reconstruction with minimal morbidity. By islanding the flap around subcutaneous (1.5–2 cm) pedicle over modiolus, we can perform oral cavity defect reconstruction in single stage [9]. Flap has to be monitored only for 12–24 h for early venous congestion which occurs due to stretch over the pedicle or tight tunnel. This can be managed by release of distal most sutures of flap inset.
Immediate risk of iatrogenic dermoid (inclusion) cysts is also avoided which is associated with flap de-epithelisation technique in conventional methods [13]. Islanded nasolabial flaps has a good arc of rotation and can be transposed to various oral cavity defects. This flap was previously used for single stage reconstruction of tongue and floor of mouth in edentulous patients. Even in dentulous patients with small to moderate defects of tongue and floor of mouth, 2 stage reconstruction with nasolabial flap has been described using through transbuccal tunnel. We have used a modification of conventional technique as described earlier in this article by islanding nasolabial flap on facial vascular pedicle and tunnelled behind mandible through mylohyoid tunnel. This technique can be used in single stage and gives comparable results to free radial artery forearm flap [10]. The limitation of flap biting has been avoided and can be performed irrespective of patient dentition. This flap is associated with few limitations such as the width of the flap is limited, appearance of hair in males in intraoral reconstruction. Although, facial scar along the nasolabial crease line is minimal yet it may bother younger patients. Most of the operated patients belong to poor socioeconomic status and work on daily wages. Hence, they are less compliant to follow up in any future recurrence.
Conclusions
Nasolabial flap proves to be a versatile flap for oral cavity defects. Despite its few limitations, this option justifies a reliable and cost effective approach in early stage malignancy especially in economically constraints patients.
References
Sharma S, Satyanarayana L, Asthana S, Shivalingesh KK, Goutham BS, Ramachandra S (2018) Oral cancer statistics in India on the basis of first report of 29 population-based cancer registries. J Oral Maxillofac Pathol 22:18–26
Coelho KR (2012) Challenges of the oral cancer burden in India. J Cancer Epidemiol 2012:1–17
Bhambar R, Baliga M, Kumar A, Jagannathan S, Kumar H, Kumar R et al (2016) Revisit of Nasolabial flap in the reconstruction of defects involving the oral floor. Niger J Surg 22:21
Eckardt AM, Kokemüller H, Tavassol F, Gellrich NC (2011) Reconstruction of oral mucosal defects using the nasolabial flap: clinical experience with 22 patients. Head Neck Oncol 3:28
Chitlangia P, Kumuran E, Sabitha KS (2012) Use of nasolabial flap in intra and extraoral reconstruction: our experience with 40 cases. J Maxillofac Oral Surg 11:451–454
Alonso-Rodríguez E, Cebrián-Carretero JL, Morán-Soto MJ, Burgueño-García M (2014) Versatility of nasolabial flaps in oral cavity reconstructions. Med Oral Patol Oral Cir Bucal 19:e525-530
Hynes B, Boyd JB (1988) The nasolabial flap: axial or random? Arch Otolaryngol Head Neck Surg 114:1389–1391
Singh S, Singh RK, Pandey M (2012) Nasolabial flap reconstruction in oral cancer. World J Surg Oncol 10:1
Mitra GV, Bajaj SS, Rajmohan S, Motiwale T (2017) Versatility of modified nasolabial flap in oral and maxillofacial surgery. Arch Craniofac Surg 18:243–248
Riju DJ, Thomas DS, Mathew DE, George DNA (2018) Nasolabial flap tunneled under mandible (NLFTUM): an alternative to free flap in T3 tongue reconstruction. Int J Innov Res Med Sci 3:2324–2328
Lazaridis N, Tilaveridis I, Karakasis D (2008) Superiorly or inferiorly based “Islanded” nasolabial flap for buccal mucosa defects reconstruction. J Oral Maxillofac Surg 66:7–15
Fang QG, Li ZN, Zhang X, Liu FY, Xu ZF, Sun CF (2013) Clinical reliability of radial forearm free flap in repair of buccal defects. World J Surg Oncol 11:1
Mann R, Srinivasan B, Webb R, Webb A (2017) An unusual complication of nasolabial flap reconstruction. Ann R Coll Surg Engl 99:e60-61
Funding
None.
Author information
Authors and Affiliations
Contributions
RG: Study conception and design; Writing original draft; reviewing and editing. CVS: Study conception and design; Data collection and analysis. SJ: Study conception and design; reviewing and editing. SP: Data collection and analysis. PG: Writing original draft; reviewing and editing. DG: Data collection and analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
Ethical approval was waived by the local Ethics Committee of DMIMS in view of the retrospective nature of the study and all the procedures being performed were part of the routine care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goyal, R., Singh, C.V., Jain, S. et al. Our Experience with Nasolabial Flaps in Soft Tissue Reconstruction of Oral Malignancy; Feasible Option in Rural Set Up. Indian J Otolaryngol Head Neck Surg 74 (Suppl 2), 2533–2538 (2022). https://doi.org/10.1007/s12070-020-02257-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-020-02257-2