Abstract
Introduction
The incidence of recurrence of OKC varied from 2.5 to 62%. Studies have linked recurrence to treatment methods and also clinical and pathological features. The aim of this study was to evaluate the 5-year recurrence and the factors associated with recurrence in odontogenic keratocysts of the jaws.
Methods
A retrospective review of records was done from the Institute’s Medical Records Directory from 2010 to 2021. The following data were obtained of the lesion; age at presentation, gender, site, subsite, radiographic presentation (locularity), radiographic borders, presence or absence of satellite cysts, inflammatory infiltrate, and treatment rendered presence or absence of cortical perforation and soft-tissue extension and presence or absence of recurrence. Kaplan Meir estimator was used to evaluate recurrence rate and log rank test was used to compare the survival amongst groups. Cox regression analysis was used to evaluate the odds ratio to find out the possible factors influencing risk of recurrence. A p value of < 0.05 was considered statistically significant at 95% confidence interval.
Results
In our study cohort, 27.2% of patients had recurrence. Posterior maxillary lesions, multilocular lesions, lesions with scalloped borders, presence of soft-tissue extension and cortical perforation, presence of satellite cysts and inflammatory infiltrate and enucleation with peripheral ostectomy were significantly associated with recurrence. However, soft-tissue extension, cortical perforation, multilocular lesions and presence of satellite cysts were independent risk factors.
Conclusion
There is still debate on the best treatment modality for the management of OKCs. More studies are required to quantify the results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background: Odontogenic keratocyst (OKC) is reclassified as a cyst of developmental origin according to the updated 2017 WHO classification of Head and Neck Tumors [1]. The 2005 WHO classification of Head and Neck tumors classified OKC as a tumor and named it as keratocystic odontogenic tumor owing to it’s aggressive behavior, solid variance, gene mutation and higher degree of recurrence [2]. However, the 2017 WHO classification reclassified it as a cyst in view of its resolution following conservative treatments and presence of genetic mutations in other odontogenic/non neoplastic lesions like dentigerous cysts [3]. In the early 1970s the reported recurrence rates were in the order of 40–60% on account of unfamiliarity with the aggressiveness of the lesion. Enucleation and curettage was the mainstay of treatment [4].
The incidence of recurrence of OKC varied from 2.5 to 62% with great variation in reporting, treatment and followup. The reported recurrence rate with only enucleation varied from 17 to 56% and when adjunctive treatment modalities like decompression or Carnoy’s solution was used the recurrence rate varied from 1 to 8.7% [1, 5,6,7]. In 1976 Brannon proposed three mechanisms for OKC recurrence; incomplete removal of the lining, growth of new cysts from daughter cysts or rests left behind after surgery and development of new OKC in adjacent area [8]. The features that were considered to predict recurrence were higher level of cell proliferative activity in the epithelium, budding in the basal layer of the epithelium, parakeratinization of the surface layer, supraepithelial split of the epithelial lining, subepithelial split of the epithelial lining and presence of remnants/cell rests as well as daughter cysts [1]. Although these reasons have been cited there still remains debate on the exact cause for recurrence. Studies have linked recurrence to treatment methods and also clinical and pathological features (larger size, daughter cysts, cortical perforation, and association with dentition) [9,10,11,12,13]. The treatment modalities available include; enucleation (with primary closure, pack open, chemical fixation or cryosurgery), marsupialization (only or followed by enucleation) and resection [14, 15]. Owing to the variation in reporting, management, followup and lack of universal guidelines there still exists variation in reporting of outcome following management of OKCs. Hence we have undertaken a retrospective study to evaluate the recurrence free survival (RFS) and the factors associated with recurrence in non-syndromic odontogenic keratocysts of the jaws.
Methods
Study Design and Setting
A retrospective review was done from the Institute’s Medical Records Directory from 2010 to 2021. Ethical clearance was obtained from the ethical committee of the Institute. The following study was conducted in accordance with STROBE guidelines [16].
Participants
Records were reviewed from January 2010 to December 2021from the Medical Records Directory. Biopsy-proven patients of odontogenic keratocyst were taken into consideration. Patients with adequate preoperative data including imaging, morphological analysis and solitary lesions in the jaws were considered. Inadequate data, multiple jaw lesions, syndromic patients, inability to review pathological reports, or archive them were the exclusion criteria. We collected 5-year (60 months) followup data from the archives. Recurrence free survival was defined as the time frame from the final diagnosis with histological report till the occurrence of relapse or last visit to the department. Patients with less than 5-year followup or who could not be contacted for further review and recurrences after 5 years were excluded.
Evaluation and Outcome
From the medical records, the following data were obtained of the lesion; age at presentation, gender, site, subsite, radiographic presentation (locularity), radiographic borders, presence or absence of satellite cysts, inflammatory infiltrate, and treatment rendered, presence or absence of cortical perforation and soft-tissue extension and presence or absence of recurrence. Authors PT and MM were the principal investigators in the study. Data collection and assessment of data was done by authors RNB and ST.
Data Analysis
The statistical analysis was performed using IBM SPSS software, version 21.0 (IBM, Armonk, NY, USA). Kaplan Meir estimator was used to evaluate recurrence rate and log rank test was used to compare the survival amongst groups. Cox regression analysis (univariate and multivariate) was used to evaluate the odds ratio to find out the possible factors influencing risk of recurrence. A p value of < 0.05 was considered statistically significant at 95% confidence interval.
Results
Based on our selection criteria, a total of 180 patient records were accessed for final analysis. The mean age of presentation was 31.82 ± 0.27 years. The median age of presentation was 31 years (25–38). The male:female ratio in our study was 1:0.59. In our study cohort, a total of 49 patients (27.2%) had recurrence and 131 (72.7%) patients did not experience any recurrence at 5-year followup. Overall the power of the study was estimated to be 80%.
The most common site of involvement was posterior mandible (62.2%) followed by posterior maxilla (19.4%), anterior mandible (15.0%) and anterior maxilla (3.3%). Multilocularity was present in a total of 53.9% of patients. Most of the lesions had well-defined borders with scalloped margin being present in 38.9% of patients. Cortical perforation was present in 45% of patients and soft-tissue extension was present in 44.4% of patients. On histological analysis satellite cysts were present in a total of 44 patients and inflammatory infiltrate was present in 50.6% of patients (Table 1). Three treatment procedures were principally carried out in our patients; I(enucleation with peripheral ostectomy), II( marsupialization followed by enucleation and peripheral ostectomy) and resection. Unilocular lesions with no sinus communication, no cortical perforations were treated by enucleation followed by peripheral ostectomy. Larger lesions with multilocularity, sinus communication were initially decompressed followed by enucleation and peripheral ostectomy. Enucleation after marsupialization was done 6–15 months following the primary procedure. During this followup period after marsupialization regular iodoform dressing was done. Patients undergoing iodoform dressing were evaluated every 7–10 days for wound irrigation and pack change. In none of the maxillary lesions resection was done. Most of the posterior lesions had sinus involvement and marsupialization followed by enucleation was done. Resection was done in cases with multiple cortical perforations, extensive soft-tissue extension, pathological fracture or extensive involvement of ramus condyle area.
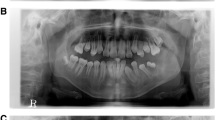
The overall 5-year recurrence free survival (RFS) in our cohort was 68.7%. A number of factors were evaluated which might affect recurrence (Figs. 1, 2, 3, 4, 5,6,7, 8, 9 and 10). The 5-year RFS was 72.7% for mandibular lesions and 55.5% for lesions in the maxilla. Multilocular lesions had a 5-year recurrence free survival of 55.9% compared to 87.6% of unilocular lesions. Lesions with scalloped margin had a 5-year recurrence free survival of 46.4% compared to 84.5% of lesions with well-defined borders. Soft-tissue extension was associated with RFS of 48.2% compared to 86.9% RFS of lesions without soft-tissue extension. Cortical perforation was associated with RFS of 49.2% and presence of inflammatory infiltrate had RFS of 53.3%. Lesions treated with resection had a RFS of 100% compared to 41% RFS of lesions treated with enucleation-peripheral ostectomy alone and 80% RFS of lesions treated in a staged manner. Presence of satellite cysts had a RFS of 42.6% (Table 1).
On univariate analysis lesions on the posterior maxilla, radiographic presentation, lesion border, soft-tissue extension, cortical perforation, treatment, satellite cysts and inflammatory infiltrate were significantly associated with recurrence. Recurrence was present in 41.2% of patients with multilocular lesions compared with 10.8% of patients with unilocular lesions (p < 0.001). With regard to lesions margins, recurrence was present in 50% of patients with scalloped margin compared to 12.7% of patients with well-defined margins (p < 0.001). Presence of soft-tissue extension was associated with 47.5% recurrence compared to 11% of patients without soft-tissue extension (p < 0.001). Presence of cortical perforation was associated with 45.7% recurrence compared to 12.1% recurrence in patients without cortical perforation (p < 0.001). Presence of satellite cysts and inflammatory infiltrate were significantly associated with recurrence (p < 0.001, p < 0.001). Enucleation with peripheral ostectomy was significantly associated with recurrence compared to staged procedure. No recurrence occurred in patients who were treated with resection (Table 2).
On multivariate analysis presence of soft-tissue extension, presence of cortical perforation, multilocular lesions and presence of satellite cysts were found as independent risk factors for recurrence. The OR (odds ratio) of having recurrence in the presence of soft-tissue extension was 8.203 compared to its absence (p 0.001). Cortical perforation was an independent risk factor for recurrence with OR 4.823 compared to its absence (p 0.018). The OR of having recurrence in the presence of satellite cysts was 8.004 compared to its’ absence (p 0.007). Presence of multilocular lesion was an independent risk for recurrence with OR 5.675 compared to its’ absence (p 0.023) (Table 3).
Discussion
Posterior maxillary lesions, multilocular lesions, scalloped margins on radiograph, soft-tissue extension, cortical perforation, presence of inflammatory infiltrate, presence of satellite cysts and enucleation with peripheral ostectomy were significantly associated with recurrence. However, presences of soft-tissue extension, cortical perforation, multilocular lesions and presence of satellite cysts were independent risk factors for recurrence.
Limitations
-
1.
Strict guidelines were not followed for treatment. Many times the treatment was decided based on patient’s expectations which might influence survival. Since it was a retrospective study based on medical records this factor could not be changed.
-
2.
No additional chemical fixation was carried out after enucleation. This might affect recurrence.
-
3.
Adequate data was not available on the nature of basal epithelium of the lining which was taken into consideration in some studies.
-
4.
We only considered 5-year recurrence rates. Long-term followups are needed to actually quantify the results.
-
5.
Our study only evaluated results of non-syndromic OKCs. The recurrence of OKC in syndromic cases was too few to be evaluated at our centre.
-
6.
Due to very few multiple lesions and inadequate data on followup, these lesions were not taken into consideration. Recurrence of multiple lesions and solitary lesions might be different.
Interpretation
Two recent studies focused on the recurrence and prognosticators of recurrence in OKC. The study by França et al. had a total of 18 (45%) recurrent cases over 5-year followup and the study by Fidele et al. had a recurrence rate of 15.09% over 2–12 years followup. Presence of satellite cysts, inflammatory infiltrate and previous decompression or marsupialization was significantly associated with recurrence in the study by França et al. In the study by Fidele et al. preservation of the involved teeth, multilocular lesions and presence of daughter cysts were independent factors for recurrence. Although size > 4 cm was significantly associated with recurrence it was not an independent risk factor. Similar findings were also found in the study by França et al. with regard to lesion size. Enucleation alone had the highest recurrence rate followed by marsupialization-enucleation and resection. Nineteen of their patients had involved teeth with cortical perforation and recurrence was 100% in these cases. Most of the recurrences occurred in first 5 years with decreasing incidence on subsequent years and the difference was statistically significant [17, 18].
A 2019 study by Kinard et al. [19] had an overall 19% recurrence with a median followup of 8 months. In their study maxillary lesions had more recurrence compared to mandible and multilocular lesions were significantly associated with recurrence. On multivariate analysis enucleation alone followed by enucleation with peripheral ostectomy had more recurrences compared to decompression followed by residual cystectomy. OKCs might present as both unilocular and multilocular lesions with unilocular being the predominant [19]. In our study a total of 83 patients had unilocular lesions and 97 had multilocular lesions. Recurrence was more in multilocular lesions and multilocularity was an independent risk factor.
In OKC satellite cysts takes three different forms; rounded keratin-filled cyst lined by flattened or cuboidal cells which can attain a very big size, squamoid structures with central degeneration occupied by epithelial debris and small irregular shaped cysts with lining indistinguishable from that of the main cyst. Postulation favors basal cell layer budding might be involved in formation of satellite cysts. However, evidence is more in support of satellite cysts being developed from cell rests of Serres [20]. Presence of satellite cysts significantly influenced recurrence in the study by França et al. In the study of Fidele et al. both in univariate and multivariate analysis daughter cysts were significantly associated with recurrence. In our study presence of daughter cysts was significantly associated with recurrence and also an independent risk factor for recurrence. Presence of inflammatory infiltrate has been shown to be associated with recurrence. Inflammation increases the epithelial thickness and signals the proliferation of epithelial lining cells.
Marsupialization followed by a delayed enucleation has been shown to reduce the recurrence as the residual defect reduces in size. The postulation is that the epithelial cyst lining will undergo metaplasia to become undistinguished from the oral mucosa. The idea behind this treatment is that remnants of the epithelial cyst lining might impact recurrence left over during enucleation [21, 22]. A 2019 meta-analysis [23] evaluated the effects of enucleation alone versus marsupialization followed by enucleation in the management of OKCs. Marsupialization followed by enucleation reduced recurrence compared to enucleation alone with an odds ratio of 0.57. However, there was no strong evidence to support the statement and concluded on further studies to evaluate the evidence. Marsupialization and delayed enucleation reduced recurrence in 52% of OKCs compared to enucleation alone (OR 0.39, p 0.10). With peripheral ostectomy, the recurrence rate was reduced in 26% (OR 0.67, p 0.65). Overall staged procedure reduced the recurrence rate in 34% over enucleation (OR 0.57, p 0.17). A 2017 meta-analysis of 6427 cases evaluated the recurrence probability in keratocystic odontogenic tumor [24]. Overall the recurrence was 21.1%; 15.3% in maxilla, 21.5% in mandible, unilocular 14.7%, multilocular 24.4%, marsupialization/decompression 28.7%, decompression + enucleation ± additional therapy 18.6%, enucleation/curettage 22.5%, enucleation + peripheral ostectomy 18.6%, enucleation + Carnoy's solution 5.3%, enucleation + cryotherapy 20.9%, marginal/segmental resection, 2.2%. The recurrence was not statistically significantly affected by lesion location (maxilla vs. mandible, risk ratio [RR] 0.92, P = 0.32) or patient's sex (male vs. female, RR 0.94, P = 0.44), but by locularity (unilocular vs. multilocular, RR 0.67, P = 0.007). Recurrence risk for surgical managements: marsupialization vs. enucleation (RR 1.65, P = 0.0006), marsupialization vs. resection (RR 3.17, P = 0.009), enucleation alone vs. enucleation + peripheral ostectomy (RR 1.66, P = 0.05), enucleation alone vs. enucleation + Carnoy's solution (RR 1.94, P = 0.03), enucleation alone vs. enucleation + cryotherapy (RR 0.88, P = 0.56). Another meta-analysis showed an overall recurrence rate of 19% with conservative treatment [25]. Decompression and marsupialization alone had a recurrence rate of 18.5 and 18.2% respectively. Decompression followed by enucleation and marsupialization followed by enucleation had a recurrence rate of 11.9 and 17.8% respectively. Enucleation alone had a recurrence of 20.8%. Decompression followed by enucleation had a recurrence of 15.8% compared to 27.2% with enucleation alone (OR 0.48, p 0.0163). Marsupialization followed by enucleation had fewer recurrence compared to enucleation alone; however, the results were not statistically significant. Comparing marsupialization alone versus enucleation also did not show statistical significant results. Similar insignificant difference was obtained for decompression alone compared to enucleation. However, enucleation was favored compared to either decompression or marsupialization alone in reducing recurrence and marsupialization followed by enucleation was also favored. Cutler and Zollinger’s modified Carnoy’s solution instillation into the cystic cavity fixes the lining and helps in more complete removal. Carnoy’s solution penetrates bone to a depth of 1.54 mm [26] and might cause irreversible neurotoxicity, adjacent soft-tissue toxicity, skin and dental follicles in children, irreversible damage to the devitalized osseous margin and no possibility of immediate bone grafting [25]. A recent clinical study has shown that the use of carnoy’s solution was not significantly related to the normalness of sensory function at the end of followup and there would be no damage to the nerves if the inferior alveolar nerve is not exposed to the solution more than 3 min [27].
Conclusion
Multilocular lesions, lesions with scalloped borders, presence of soft-tissue extension and cortical perforation, presence of satellite cysts and inflammatory infiltrate and enucleation with peripheral ostectomy were significantly associated with recurrence. However, soft-tissue extension, cortical perforation, enucleation with peripheral ostectomy and marsupialization followed by enucleation + peripheral ostectomy were independent risk factors for recurrence.
References
Wright JM, Vered M (2017) Update from the 4th Edition of the World Health Organization Classification of head and neck tumours: odontogenic and maxillofacial bone tumors. Head Neck Pathol 11:68–77
Wright JM, Odell EW, Speight PM, Takata T (2014) Odontogenic tumors, WHO 2005: where do we go from here? Head Neck Pathol 8(4):373–382
Soluk-Tekkeşin M, Wright JM (2018) The World Health Organization Classification of odontogenic lesions: a summary of the changes of the 2017 (4th) Edition. Turk Patoloji Derg, 34(1)
Stoelinga PJW (2022) The odontogenic keratocyst revisited. Int J Oral Maxillofac Surg 51(11):1420–1423
Blanas N, Freund B, Schwartz M, Furst IM (2000) Systematic review of the treatment and prognosis of the odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90(5):553–558
Li TJ (2011) The odontogenic keratocyst: a cyst, or a cystic neoplasm? J Dent Res 90:133–142
Kuroyanagi N, Sakuma H, Miyabe S et al (2009) Prognostic factors for keratocystic odontogenic tumor (odontogenic keratocyst): analysis of clinico-pathologic and immunohistochemical findings in cysts treated by enucleation. J Oral Pathol Med 38(4):386–392
Brannon RB (1976) The odontogenic keratocyst A clinicopathologic study of 312 cases. Part I. Clinical features. Oral Surg Oral Med Oral Pathol 42:54–72
Stoelinga PJ (2001) Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg 30(1):14–25
Kaczmarzyk T, Mojsa I, Stypulkowska J (2012) A systematic review of the recurrence rate for keratocystic odontogenic tumour in relation to treatment modalities. Int J Oral Maxillofac Surg 41(6):756–767
Kaczmarzyk T, Kisielowski K, Koszowski R et al (2018) Investigation of clinicopathological parameters and expression of COX-2, bcl-2, PCNA, and p53 in primary and recurrent sporadic odontogenic keratocysts. Clin Oral Investig 22(9):3097–3106
Naruse T, Yamashita K, Yanamoto S et al (2017) Histopathological and immunohistochemical study in keratocystic odontogenic tumors: predictive factors of recurrence. Oncol Lett 13(5):3487–3493
Chirapathomsakul D, Sastravaha P, Jansisyanont P (2006) A review of odontogenic keratocysts and the behavior of recurrences. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(1):5–9; discussion 10
Eyre J, Zakrezewska JM (1985) The conservative management of large odontogenic keratocysts. Br J Oral Maxillofac Surg 23:195–203
Morgan TA, Burton CC, Qian F (2005) A retrospective review of treatment of odontogenic keratocyst. J Oral Maxillofac Surg 63:635–639
Vandenbroucke JP, von Elm E, Altman DG et al (2007) STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 4(10):e297.
Fidele NB, Yueyu Z, Zhao Y, Tianfu W, Liu J, Sun Y, Liu B (2019) Recurrence of odontogenic keratocysts and possible prognostic factors: Review of 455 patients. Med Oral Patol Oral Cir Bucal 24(4):e491–e501
de França GM, da Silva LBA, Mafra RP, da Silva WR, de Lima KC, Galvão HC (2021) Recurrence-free survival and prognostic factors of odontogenic keratocyst: a single-center retrospective cohort. Eur Arch Otorhinolaryngol 278(4):1223–1231
Kinard B, Hansen G, Newman M, Dennis P, Haeffs T, Perez S, Hamao-Sakamoto A, Steed M, Hughes P, August M, Abramowicz S (2019) How well do we manage the odontogenic keratocyst? A multicenter study. Oral Surg Oral Med Oral Pathol Oral Radiol 127(4):282–288
Bello IO (2016) Keratocystic odontogenic tumor: a biopsy service’s experience with 104 solitary, multiple and recurrent lesions. Med Oral Patol Oral Cir Bucal 21(5):e538–e546
Pogrel MA (2005) Treatment of keratocysts: the case for decompression and marsupialization. J Oral Maxillofac Surg 63(11):1667–1673
Schlieve T, Miloro M, Kolokythas A (2014) Does decompression of odontogenic cysts and cystlike lesions change the histologic diagnosis? J Oral Maxillofac Surg 72(6):1094–1105
Slusarenko da Silva Y, Stoelinga PJW, Naclério-Homem MDG (2019) Recurrence of nonsyndromic odontogenic keratocyst after marsupialization and delayed enucleation vs. enucleation alone: a systematic review and meta-analysis. Oral Maxillofac Surg 23(1):1–11
Chrcanovic BR, Gomez RS (2017) Recurrence probability for keratocystic odontogenic tumors: an analysis of 6427 cases. J Craniomaxillofac Surg 45(2):244–251
de Castro MS, Caixeta CA, de Carli ML et al (2018) Conservative surgical treatments for nonsyndromic odontogenic keratocysts: a systematic review and meta-analysis. Clin Oral Investig 22(5):2089–2101
Rao K, Kumar S (2014) The Use of Enucleation and Chemical Cauterization (Carnoy’s) in the Management of Odontogenic Keratocyst of the Jaws. Indian J Otolaryngol Head Neck Surg 66(1):8–12
Jo HJ, Kim HY, Kang DC et al (2020) A clinical study of inferior alveolar nerve damage caused by Carnoy’s solution used as a complementary therapeutic agent in a cystic lesion. Maxillofac Plast Reconstr Surg 42(1):16
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
CPGIDSH/21/0185-A.
Consent for publication
Authors give full consent to publish.
Consent to participate
Not required. Retrospective study from medical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bera, R.N., Tandon, S., Tiwari, P. et al. Recurrence and Prognosticators of Recurrence in Odontogenic Keratocyst of the Jaws. J. Maxillofac. Oral Surg. (2023). https://doi.org/10.1007/s12663-022-01846-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-022-01846-8