Abstract
The purpose of this study was to evaluate the use of enucleation and chemical cauterization in the management of odontogenic keratocyst (OKC) of the jaw. This study involves the retrospective review of 32 patients (20 males and 12 females) with 34 biopsy proven odontogenic keratocysts. All patients received a combination of enucleation and chemical cauterization with every time freshly prepared Carnoy’s solution (absolute alcohol 6 mL, chloroform 3 mL, glacial acetic acid 1 mL, ferric chloride 0.1 gm/mL). None of these patients were diagnosed with basal cell nevus syndrome. Four of these patients did not give the follow up and were not included in the study. A total of 30 biopsy proven OKC were resolved with this treatment method. Post-operative follow up consists of clinical and radiographic examination. Follow up time ranged from a minimum of 2 years to a maximum of 5 years. Mean follow up was of 2.8 years. Recurrence rate of 5.8% was observed. Hence, concluded that the combination of enucleation and chemical cauterization may offer patients improved therapy in the management of odontogenic keratocysts of the jaws.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Odontogenic keratocyst (OKC) as a distinct entity was first described by Philipsen in 1956 [1], which used the term to describe jaw cysts exhibiting keratinization of their epithelial linings. OKC is now referred by WHO as a keratocystic odentogenic tumour tumour due to its aggressive and infiltrative behavior. WHO also defined it as unicystic or multicystic intraosseous tumour of odentogenic origin, with a characteristic lining of parakeratinized, squamous epithelium. (Barnes et al. 2005). The first reported series was of 30 cases followed by Pindborg and Hansen in 1963 [2]. Lesions present most frequently in the second, third, and fourth decades of life (54.2%). Some cases reported as early as the first decade and as late as the ninth decade of life. In addition, predilection for male gender and the posterior part of mandible has been reported, with a male to female ratio of 2:1 and 65–83% of the cases involving the posterior mandible [3]. Most of the lesions are found in molar, angle and ramus areas.
Odontogenic keratocysts (OKCs) are thought to be derived from the enamel organ or from the dental lamina and are probably not related to any kind of infection. Clinically they do not present with any characteristic features. There are some similarities however, with the ameloblastoma as to age of the patient, location of the lesion, the radiographic picture, and the tendency for recurrence. Although they grow to reach a larger size but may remain asymptomatic. When they do not, intraoral drainage and swelling are the most common findings. It is of the interest that these cysts more often penetrate bone rather than expanding it. They grow in an anterior to posterior direction rather than buccally to lingually [4].
Recommended treatments have included curettage with peripheral ostectomy [5], curettage plus liquid nitrogen cryotherapy [6], curettage plus application of Carnoy’s solution [7], localized en bloc resection [8, 9], and occasionally mandibular segmental resection [8]. Some authors have stated that they should be regarded as benign cystic neoplasms and treated accordingly [10–13].
OKCs are known for their propensity to recur. The rate of recurrence probably depends upon the modality of treatment used. Apart from this the high propensity for recurrence is almost certainly related to the tenuous and friable lining of keratocysts which results in incomplete surgical removal. To reduce the recurrence rate, tanning of the epithelial lining of the cyst with modified Carnoy’s solution (Cutler and Zollinger formula: absolute alcohol 6 mL, chloroform 3 mL, glacial acetic acid 1 mL, ferric chloride 0.1 gm/mL) has been advocated [14, 15]. The remarkably low recurrence rates achieved by Voorsmit are claimed to be an effect of instillation of Carnoy’s solution into the cystic lumen. The intra cystic use of the agent leads to intravital fixation of the lining and enables it to be more readily and completely removed. The proponents of Carnoy’s solution deny toxic effects on peripheral nerve tissue, bearing in mind that the inferior alveolar nerve (IAN) is often located in the bony cavity of large cysts of the mandibular angle or ascending ramus [16].
Materials and Methods
We collected and analyzed the available data on patients who presented with histologically verified OKCs in over a five years period starting on May 2006–July 2011.
Criteria used to establish a diagnosis were:
-
(1)
Radiographic findings.
-
(2)
Histological criteria as outlined by Pindborg and Hansen [2] and Browne [17].
Total 32 patients (21 males and 11 females) with 34 biopsy proven OKCs were included.
The data collected included age at diagnosis, gender, lesion location, clinical manifestations, radiographic features, any previous treatment modality and recurrence.
The location of the OKCs was classified as follows: maxillary incisor and canine, maxillary premolar, maxillary molar, mandibular incisor and canine, mandibular molar and mandibular angle and ramus. The clinical manifestation at diagnosis was recorded in 2 categories:
-
1)
OKC’s identified incidentally by other departments of dental college while doing dental check up and treatment for some other dental problems.
-
2)
OKCs identified in patients presenting with symptoms such as pain, swelling, inferior alveolar nerve paraesthesia, infection, or drainage. The lesions were also divided into unilocular and multilocular variants according to panoramic radiographs.
Results
This retrospective review evaluated 32 non-syndrome associated patients with 34 biopsy proven OKCs. The study included 20 men and 12 women. The age distribution is shown in Table 1.
All the patients range from 11 to 72 years age. Maximum patients were from fourth decade.
The duration of symptoms varied from one month to 23 months. Table 2 indicates the presenting symptoms recorded in 32 patients.
Out of 32 cases 20 patients were asymptomatic and they were diagnosed incidentally by other dental departments while doing dental checkup and treatment. They were referred to oral surgery department for further management.
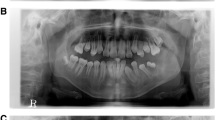
Out of the 34 OKCs found in 32 patients, 4 were in the maxilla and 30 were in the mandible. Mandibular lesions were more common than maxillary lesion in our study group. Most of the lesions were (32/34) parakeratnized type. All the cases were treated with enucleation followed by chemical cauterization with the Carnoy’s solution. All the lesions were biopsied and diagnosed as an OKC. 32 OKCs had no evidence of clinical or radiographic recurrence after treatment by enucleation and chemical cauterization. Recurrence was reported in 2 patients (5.8%). The treatment plan included extraction of the involved teeth, enucleation and chemical cauterization as shown in (Figs. 1, 2, 3).
The entire lesions were enucleated, and the cyst cavities were treated with carnoy’s solution technique i.e., applying it for 1 min. The region was watched closely with regular radiographs. Panoramic radiographs were used for follow up i.e. after 1 month, 3 months, 6 months and afterwards as long as patient came for follow-up.
Discussion
The approach to the treatment of OKCs is controversial. OKC requires special considerations because even if OKC cannot really be considered a malignancy, some of its characteristics make this pathology extremely serious. In fact, keratocyst tend to recur, can reach considerable dimensions, and can arise close to delicate and important anatomical structures like alveolar nerve. All these characteristics had suggested, in past that an aggressive surgical approach should be followed in order to eradicate these cysts completely. Such radical behavior might result in severe mutilation, so for this reason, it is not always advisable.
In the past decade, some conservative surgical approaches (lateral cystectomy, enucleation, cryosurgery, decompression, and marsupialization) have been proposed in order to reduce the negative effects of the aggressive surgery and thus, respecting the delicate anatomical structure of the jaws, giving the patient better quality of life.
Relative to historical controls listed in Table 3, the 2.94% recurrence rate obtained with enucleation and chemical cauterization with carnoy’s solution in this study is low. Branon’s [18] study is the largest series, with 312 keratocysts. With enucleation alone, the recurrence rate was 12%. However, the length of follow-up was not reported. The authors reporting significantly lower rates of recurrence are Voorsmit et al. [19] and Brondum and Jensen [20] with rate of 2.5 and 0% respectively. Voorsmit et al. compared 2 treatment methods: 52 keratocysts were treated conservatively with enucleation alone, and 40 keratocysts were removed along with excision of the over-lying mucosa and treatment of the cyst cavity with Carnoy’s solution. In the first group, 13.5% of the cysts recurred, whereas 2.5% of the cysts in the second group recurred. Given the 2 treatment variables in the second group, (i.e. excision of the overlying mucosa and application of Carnoy’s solution) the effective aspect of the therapy is difficult to determine. The rationale for using Carnoy’s solution is similar to that of cryosurgery. The goal of both techniques was to kill epithelial remnants and dental lamina in the osseous margin. Carnoy’s solution (absolute alcohol 6 mL, chloroform 3 mL, glacial acetic acid 1 mL, ferric chloride 1 gm) is a tissue fixative that penetrates bone to a depth of 1.54 mm [6, 21, 22]. The penetration and margin of cellular necrosis produced by liquid nitrogen cryosurgery in the mini pig model was shown to be average of 0.82 mm (0.51–1.52 mm) [23]. Brondum and Jensen [20] reported low recurrence rate was obtained by using a polyethylene drainage tube implanted at the time of cystotomy and biopsy to decompress the keratocyst months before primary cystectomy. At the second stage, the author found that the cystic epithelium did not adhere to surrounding structures. No recurrences were observed with in an observation period of 7–17 years. The limitation of this study is that only 12 keratocysts were followed.
The results obtained in the present study with enucleation with chemical cauterization with Carnoy’s solution are encouraging. An evaluation of the recurrences observed in the 2 cases may have been due the location of the cyst with intimate association with the dentate area. From this study one can conclude that Enucleation with chemical cauterization is well tolerated and has few complications associated with it. The most common complication is wound dehiscence, and this can be typically managed conservatively.
Conclusion
It is clear that OKCs can recur years and even decades after treatment. The mean follow-up of 2.8 years in this study is short given the natural history of these lesions. However, a recurrence rate of 5.8% is clearly lower than that in many previous studies evaluating enucleation alone. The recurrence rate could even be significantly lower with strict attention to the basic principles of surgical and chemical cauterization technique. Based on these results, the combination of enucleation and chemical cauterization offer patients improved therapy in the management of OKCs.
References
Philipsen HP (1956) On keratocysts in the jaw. Tandlaegebladet 60:963
Pindborg JJ, Hansen J (1963) Studies on odontogenic cyst epithelium, II: Clinical and roentgenologic aspects of odontogenic keratocysts. Acta Pathol Microbiol Scand 58:283
Thawley SE, Panje WR, Batsakis JG et al (1999) Comprehensive management of head and neck tumors, vol 2, 2nd edn. WB Saunders, Philadelphia, p 1556
Zachariades N, Papanicolaou S, Triantafyllou D (1985) Odontogenic keratocyst: review of the literature and report of sixteen cases. J Oral Maxillofac Surg 43:177–182
Irvine GH, Bowerman JE (1985) Mandibular keratocysts: surgical management. Br J Oral Maxillofac Surg 23:204
Schmidt BL, Pogrel MA (2001) The use of enucleation and liquid nitrogen cryotherapy in the management of odontogenic keratocysts. J Oral Maxillofac Surg 59:720
Stoelinga PJ (2001) Long-term follow-up on keratocysts treated according to a defined protocol. Int J Oral Maxillofac Surg 30:14
Bramley P (1974) The odontogenic keratocyst—an approach to treatment. Int J Oral Surg 3:337
Bataineh AB, al Qudah M (1998) Treatment of mandibular odontogenic keratocysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 86:42
Ahlfors E, Larsson A, Sjogren S (1984) The odontogenic keratocyst: a benign cystic tumor? J Oral Maxillofac Surg 42:10
Shear M (2002) The aggressive nature of the odontogenic keratocyst: Is it a benign cystic neoplasm? Part 1. Clinical and early experimental evidence of aggressive behavior. Oral Oncol 38:219
Shear M (2002) The aggressive nature of the odontogenic keratocyst: is it a benign cystic neoplasm? Part 2 Proliferation and genetic studies. Oral Oncol 38:323
Shear M (2002) The aggressive nature of the odontogenic keratocyst: Is it a benign cystic neoplasm? Part 3. Immunocytochemistry of cytokeratin and other epithelial cell markers. Oral Oncol 38:07
Voorsmit RACA (1985) The incredible keratocyst: a new approach to treatment. Dtsch Zahnlrztl Z 40:641
Stoelinga PJW, Bronkhorst FB (1988) The incidence, multiple presentation and recurrence of aggressive cysts of the jaws. J Craniomaxillofac Surg 16:184
Frerich B, Cornelius CP, Wlethijlter H (1994) Critical time of exposure of the rabbit inferior aiveoiar nerve to Carnoy’s solution. J Oral Maxillofac Surg 52:599–606
Browne RM (1971) The odontogenic keratocyst: histological features and their correlation with clinical behavior. Br Dent J 131:249
Brannon RB (1976) The odontogenic keratocyst—a clinicopathologic study of 312 cases. Part I. Clinical features. Oral Surg 42:54
Voorsmit RA, Stoelinga PJ, van Haelst VJ (1981) The management of keratocysts. J Maxillofac Surg 9:228
Brondum N, Jensen VJ (1991) Recurrence and decompression treatment: a long-term follow-up of forty-four cases. Oral Surg Oral Med Oral Pathol 72:265
Williams TP, Connor FA (1994) Surgical management of the odontogenic keratocyst: aggressive approach. J Oral Maxillofac Surg 52:964
Voorsmit RACA (1984) The incredible keratocyst (thesis). University of Nijmegen, The Netherlands
Pogrel MA, Regezi J, Fong B et al (1998) Liquid nitrogen cryotherapy and immediate bone grafting: an animal model. J Oral Maxillofac Surg 56(suppl):53
Vedtofte P, Praetorius F (1979) Recurrence of the odontogenic keratocyst in relation to clinical and histologic features. Int J Oral Surg 8:412
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rao, K., Kumar, S. The Use of Enucleation and Chemical Cauterization (Carnoy’s) in the Management of Odontogenic Keratocyst of the Jaws. Indian J Otolaryngol Head Neck Surg 66, 8–12 (2014). https://doi.org/10.1007/s12070-012-0523-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-012-0523-8