Abstract
Aim
To evaluate the effectiveness of a modified maxillo-mandibular nerve block technique that includes anesthetizing the maxillary and mandibular nerve with single injection.
Materials and Methods
A prospective, clinical cohort study was carried out including patients who presented for surgical removal of maxillary and mandibular third molars. All patients were administered maxilla-mandibular nerve block through a single injection on one side. Three clinical neurosensory tests were used for mapping the area of anesthesia and to assess and grade objectively the effect of the block. Light touch (LT), two-point discrimination (TPD), pin prick (PP) and Electric pulp testing (EPT) were used for all branches of maxillary and mandibular nerve. An extra oral mapping chart for depth of anesthesia was maintained for each patient to categorize the grades as nil, intermediate and highly anesthetized areas.
Results
62 patients were assessed in the study. EPT showed greater depth of pulpal anesthesia in posterior teeth than the anterior in both maxilla and mandible. PP and TPD tests also showed that the anesthetic effect varied between posterior divisions demonstrating extreme anesthesia compared to the anterior divisions.
Conclusion
This technique was found to be successful for surgical extractions involving the maxillary and mandibular regions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Local anesthesia is a prerequisite for painless dental extractions. However, the fear of local anesthetic injections can itself be a cause of concern in anxious patients sometimes leading to avoidance of dental care [1]. The most common method for achieving local anesthesia for dental procedures is by intra oral injections.
Multiple intraoral blocks are often required for procedures like third molar removal, intermaxillary fixation and full mouth rehabilitation. For the removal of ipsilateral bimaxillary third molars, a minimum of four injections at four different locations need to be given. This requires patient compliance and expertise of the operator to make sure the injection itself is minimally painful. This occasionally leads to increase in the dose of the anesthetic solution administered and heightens patient anxiety over repeated needle penetrations. The extra-oral maxillo-mandibular never blocks can be of great value when multiple nerves needed to be anesthetized in regard to the extent of the surgical procedures planned. They were first described in the literature at the beginning of the twentieth century chiefly for diagnostic purposes [2].
In the present study, we evaluated the efficacy of one such modified method of maxillo-mandibular nerve block technique that includes anesthetizing the entire distribution of the maxillary and mandibular nerves with single injection. Extra oral nerve block for maxillary and mandibular divisions was originally introduced by Adriani in the year 1956 [11]. He described the extra-oral technique via prearticular fossa to target maxillary and mandibular nerve branches in close approximation with pterygomaxillary fissure and Foraman Ovale, respectively. In our study we adapted the same technique landmarks with modification in specific angulation of 15 degree in both anterior and posterior direction with single injection site. The specific objectives of this study were to evaluate and define the area of distribution of anesthesia, to assess the depth of anesthesia through subjective and objective parameters, and to determine the relative effectiveness of the maxillo-mandibular nerve block for dentoalveolar procedures in both arches.
Patients and Methods
The study was designed as a prospective clinical cohort study. The Study protocol was approved by Institutional Review Board. Informed consent was obtained from the patients for participation in the study. Patients were included based on the following inclusion criteria: (1) Patient requiring surgical extraction of maxillary and mandibular third molars, (2) Physical status of ASA I or II, (3) Presence of a full complement of teeth on the same side as the extraction, (4) Patients with healthy pulp of the second molar, second premolar, upper and lower central incisors on the side of injection for the purpose of uniformity in pulpal response testing. The exclusion criteria were as follows: (1) inflammatory conditions of the head and neck region like parotitis, zygomatic arch and mid-face fractures (2) known allergies to local anesthetic solution, (3) Patients with dentofacial deformities like Hemifacial microsomia and Treacher-Collins syndrome, (4) Space infections like buccal and massetric space infection.
Anesthesia Technique (Video 1)
Modified extra-oral sub-zygomatic maxillo-mandibular nerve block as a single injection technique:
After aseptic preparation of the area around the zygomatic arch region, the pre-eminence region of the zygomatic arch corresponding to the anterior one third of the supra sigmoid notch area of the mandible, was marked. The thumb was pressed on the pre-eminence region as the surface marking for the insertion. A spinal needle with a stopper at 45 mm was inserted after raising a small subcutaneous wheal for anesthesia. The needle was inserted to the stopper, and at about 45 mm it was expected to hit the lateral aspect of the lateral pterygoid plate (Fig. 1). On hitting the bone, the needle was withdrawn one third of its length and inserted anteriorly and upward with a 15-degree angulation to the same depth of 45 mm and after negative aspiration of the cartridge a volume of 2.5 ml of local anesthetic (Lignocaine with 1:80,000 dilution. Adrenaline) was injected in the space. This corresponded to the region immediately lateral to the pterygomaxillary fissure through which the maxillary nerve trunk passes (Fig. 2). Diffusion of the anesthetic solution through the fissure ensured anesthesia of the maxillary nerve trunk. The needle was then withdrawn to one third of its length, angulated 15 degrees posterior and upward in the coronal plane, aspirated and the remaining 2.5 ml of solution was injected slowly. The position of the needle now corresponded to the area below the Foramen Ovale where the main trunk of the mandibular branch descends from its intra cranial course (Fig. 3). All the injections were administered by a single operator.
Clinical photograph demonstrating the area of insertion of needle for administering the Maxillo-mandibular nerve block. Graphic representations of the surface markings, a Mandibular outline with the posterior border, sigmoid notch and the coronoid process, b Zygomatic arch with the eminence and the pre-eminence region and c Point of insertion of the needle
Clinical Parameters
Four clinical neurosensory tests were used for mapping the area of anesthesia. Mechanoceptive tests were done using Light touch (LT) and two point discrimination (TPD) and nociceptive tests were done by pin prick (PP) and Electric pulp testing (EPT). The tests were used to assess objectively the effect of the block by performing each test three times. The depth of the nerve block for each patient were categorized as (1) Nil—Deduction of a response two out of three times was considered un-anesthetized or lack of anesthetic effect. (2) Intermediate—Failure to respond two out of three times was considered to be intermediately anesthetized. (3) High—When the patient did not respond all three times, the zone was considered effectively anesthetized. An extra oral skin mapping chart for depth of anesthesia was maintained (Fig. 4) and documented.
Assessment parameters for anesthetic effect were evaluated by a single investigator. All extractions were performed by a single operator. Any need for supplemental injections used and complications during procedures were documented. Descriptive statistics were presented as numbers and percentages.
Results
62 patients were assessed, of which 30 were male and 32 were female. The mean age was 28.36 years. The age range was 19–52 years.
Infraorbital (IO), auriculotemporal (ATN), mylohyoid (MHN) and mental nerve (MN) areas were tested for two-point discrimination and light touch tests. MN showed maximum response to these tests, 49 (79%) of the 62 patients were highly anesthetized whereas ATN showed the least 2(3.2%) patients (Fig. 5).
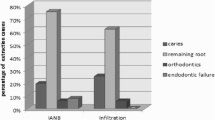
Anterior superior alveolar nerve (ASA), Middle superior alveolar (MSA), Posterior superior alveolar (PSA), Greater Palatine (GP), and Nasopalatine (NP), branches of maxillary nerve were studied for pin prick test over a defined area. PSA showed maximum response with 59 (96.8%) of patients, whereas ASA showed the least with only 35 (56.5%) of patients (Fig. 6). Among the mandibular branches, Inferior alveolar nerve showed high frequency of extremely anesthetized area in 53 (85.5%) patients whereas incisive nerve showed the least in 37 (59.7%) patients.
ASA, MSA, PSA, IAN, and IN, PSA were tested with electric pulp testing (EPT). PSA showed maximum response whereas ASA showed the least. IAN showed 53(85.5%) patients of extremely anesthetized response (Fig. 7).
Discussion
Local anesthetic technique is pivotal in making dental treatment painless and secure. Ironically, the anxiety associated with receiving dental injections can avert the patients from seeking dental care. This fear is often related to the feeling of needle penetration and pain during the injection. This is further complicated in situations requiring multiple injections to anesthetize a particular area [3].
In order to overcome these drawbacks, the extra oral nerve block can be adopted over conventional intraoral techniques. These nerve blocks are helpful in anesthetizing the entire distribution of both nerves. It involves injecting the local anesthetic solution in the vicinity of the Foramen Rotundum and Foramen Ovale, via the infratemporal fossa. Adequate knowledge of infratemporal fossa anatomy is a prerequisite for successful outcomes.
It is often stated that the deep location of the maxillary nerve trunk at the Foramen Rotundum, as well as of the mandibular nerve at the Foramen Ovale makes regional blocks of these nerves difficult and complicated [4]. The depth of penetration in the extra oral technique is considered controversial as the anatomical landmarks are not consistent and change between patients [8]. In 2002, Radder et al. improved the extra oral injection technique by using the lower lateral orbital angle and the junction of the external acoustic canal and mastoid process as consistent landmarks [4]. Stajcic Z et al. in 1997 showed that blocks at the level of Foramen Rotundum and the Foramen Ovale, reported an overall success rate of 88% [5]. Later in 2010 Okuda et al. studied the anatomy of the Pterygopalatine fossa for the technique of maxillary nerve block at the Foramen Rotundum [6]. Their technique for the maxillary nerve block using the suprazygomatic route was guided by computed tomography.
In our technique, the pre-eminence region of the zygomatic arch (sub zygomatic region) is taken as the landmark and on contacting the lateral pterygoid plate (depth of 45 mm) the needle is withdrawn one third of its length and inserted anteriorly and upward with a 15° angulation to the same depth of 45 mm that corresponds to the pterygomaxillary fissure through which the maxillary trunk passes. Then the needle is angulated 15° posterior and upward to the coronal plane. This position corresponds to the area below the foramen Ovale where the main trunk of the mandibular branch descends from its intra cranial course. Diffusion of the anesthetic solution in that region ensures adequate anesthesia of the maxillary and mandibular nerve. Thus, with a single needle insertion, by changing the angulation and direction of the needle, both nerves are blocked.
While many of these studies succeeded in shedding light on the extra oral injection technique, an objective assessment of clinical effectiveness and diffusion of anesthesia was not made. Through this study, we have attempted to define the areas of anesthesia of individual branches and their frequency of getting anesthetized.
In the present study, the EPT showed greater depth of pulpal anesthesia in posterior teeth than the anteriors in both, the maxilla and mandible. PP and TPD tests also showed that the anesthetic effect varied from posterior divisions, which showed extreme anesthesia compared to the anterior divisions. This may be due to the incisive nerve that extensively branches and offers anastomoses over the midline to the contralateral side, thus creating a crossover effect in the innervation of the anterior teeth [7].
The ATN showed least anesthetic effect, this might be because of its anatomical variation in the courses. Gulekon et al. in 2005 studied complex variations in the anatomy of ATN in cadaveric skull [8]. These variations hinder the diffusion of anesthetic solution and results in the failures of surgical interventions and anesthesia. Similarly, the posterior branches of maxillary nerve were found to be more anesthetized than the anterior branches. The ASA for example, due to its most distal location from the injection site showed least anesthesia [9]. The MSA also showed less response, due to its incidence in the range of 30–72%.
For this particular trial, our aim was to map the distribution of anesthesia where every patient was objectively assessed for the effectiveness of the block. Patients who had failure of anesthesia were planned for supplemental injections to aid their procedure for third molar extractions; intra oral IAN blocks for the mandible and buccal infiltration for the maxillary molars. But in our cohort of patients who needed third molar removals, no one complained of pain during the procedure and hence no supplemental injections were given. This suggests that though the clinical testing reveals that not every patient reported anesthesia, it was sufficient enough to perform the procedure without any clinical difficulty.
The complex regional anatomy associated with the technique, necessitate the administering clinician to be proficient in the loco-regional surgical anatomy. This would ensure minimal adverse outcomes such as hematomas, intra-vascular injections and ophthalmic complications. Out of the total 62 patients, only one patient experienced positive aspiration because of the proximity of the maxillary artery. In such case, the injection needle was completely withdrawn and reinserted with a slight anterior angulation of 16 degrees. One patient experienced transient diplopia that subsided as the anesthetic effect reduced. This can be due to the anesthetic solution permeating into the orbit by local diffusion, along tissue planes, between the pterygomaxillary fossa and the orbit [10].
The main limitation of this extra-oral technique is the inability to perform this block in conditions like space infections (buccal space infection), local infections at the site of injection (sebaceous cyst, parotitis) and midface and zygomatic arch fractures. These factors may complicate the assessment of landmarks for needle insertion. A further limitation may be the fact that a facial injection for intra-oral procedures, may be a deterrent in few patients. However, this was not seen frequently in our experience. The value of the technique may further be documented in future studies as a controlled trial between conventionally practiced block techniques and the maxilla-mandibular nerve block which will authenticate the superiority of one over the other. An additional parameter of patient anxiety score may also add value in the compliance of patients to accept this technique.
In future, the application of this technique can be used for bimaxillary multiple dental extractions, placement of intermaxillary fixation and obturators, removal of suspension wiring and extensive wound closure on the face. The indications may also be expanded to encompass pain management in major surgeries such as facial trauma, orthognathic surgery, tumor resections and, cleft lip and palate surgeries.
Conclusion
With the sparse literature available for the various techniques of the extra oral nerve blocks, we have attempted to evaluate the effectiveness and indications of this nerve block technique on 62 patients. This technique was found to be successful for surgical extractions involving the posterior maxillary and mandibular regions.
References
Crean SJ, Powis A (1999) Neurological complications of local anaesthetics in dentistry. Dent Update 26(8):344–349
de Villa GH, Nicholoff TJ Jr (1998) Extraoral maxillary and mandibular nerve blocks for a patient with Sutton’s disease. J Philipp Dent Assoc 50(1):24–27
McCartney M, Beck M (2007) Injection pain of the inferior alveolar nerve block in patients with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104:571
Radder K, Shah A, Fatima S, Kothari C, Zakaullah S, Siddiqua A (2013) Efficacy and feasibility of frontozygomatic angle approach for extra oral maxillary nerve block in oral surgery: a descriptive clinical trial. J Maxillofac Oral Surg 13(3):231–237
Stajcić Z, Todorović L (1997) Blocks of the foramen rotundum and the oval foramen: a reappraisal of extraoral maxillary and mandibular nerve injections. Br J Oral Maxillofac Surg 35(5):328–333
Okuda Y, Okuda K, Shinohara M, Kitajima T (2000) Use of computed tomography for maxillary nerve block in the treatment of trigeminal neuralgia. Reg Anesth Pain Med 25(4):417–419
Dreven LJ, Reader A, Beck M, Meyers WJ, Weaver J (1987) An evaluation of an electric pulp tester as a measure of analgesia in human vital teeth. J Endod 13(5):233–238
Gülekon N, Anil A, Poyraz A, Peker T, Turgut HB, Karaköse M (2005) Variations in the anatomy of the auriculotemporal nerve. Clin Anat 18(1):15–22
Velasco I, Soto R (2012) Anterior and middle superior alveolar nerve block for anesthesia of maxillary teeth using conventional syringe. Dent Res J (Isfahan) 9(5):535–540
Moiseiwitsch J, Irvine T (2001) Clinical significance of the length of the pterygopalatine fissure in dental anesthesia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92(3):325–328
Topazian RG, Simon GT (1962) Extraoral mandibular and maxillary block techniques. Oral Surg Oral Med Oral Pathol 15:296–300. https://doi.org/10.1016/0030-4220(62)90108-1
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Technique of extra oral nerve block administered to a patient on a dental chair (MP4 16757 kb)
Rights and permissions
About this article
Cite this article
Fauziya, D., Anantanarayanan, P. & Shankar, D.P. Effectiveness and Distribution of Anesthesia for a Modified Extra Oral Maxillo-Mandibular Nerve Block for Dento-Alveolar Procedures: A Prospective Cohort Study. J. Maxillofac. Oral Surg. 23, 561–567 (2024). https://doi.org/10.1007/s12663-022-01755-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-022-01755-w