Abstract
Objectives
The aim of this study was to investigate the effectiveness of a local anesthetic agent comprising of 4 % articaine with 1:100,000 adrenaline, administered through an infiltration technique prior to the extraction of mandibular permanent first molar teeth.
Materials and methods
The study adopted a split mouth approach and involved patients who needed simple extractions of permanent mandibular first molar teeth on both sides. A combination of buccal and lingual infiltrations was used on one side, while the conventional inferior alveolar nerve block (IANB) technique, with a 1.8-ml cartridge of 4 % articaine with 1:100,000 epinephrine, was administered to the other. The patients’ pain perception was assessed using visual analogue scale (VAS) and verbal rating scale (VRS) after the injection, followed by extraction.
Results
As a part of the study, 104 teeth were extracted from mouths of 52 patients. The difference in pain perception was statistically insignificant (p > .05) regarding the local anesthetic injection between the two techniques. The difference in pain perception regarding the extraction between the two techniques was also statistically insignificant (p < .05).
Conclusion
No difference in pain perception between the two techniques among the study population was noted. This indicates that the extraction of permanent mandibular first molar teeth is possible without the administration of an IANB with the use of 4 % articaine with 1:100,000 epinephrine.
Clinical relevance
The buccal and lingual infiltrations are slightly less painful than the conventional IANB technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Local anesthesia refers to a temporary loss of sensation in a circumscribed area of the body. It is produced by an inhibition of the conduction process of the action potential in peripheral nerves without depressing the level of consciousness [1]. Profound local anesthesia results in complete absence of pain, temperature, and touch sensations, although it does not anesthetize the proprioceptive fibers of the involved nerves [2].
Articaine, which was previously known as “Carticaine,” was originally synthesized in 1969 by H. Rushing and his colleagues and entered clinical practice in 1976. Articaine is a unique hybrid of an amide- and ester-class local anesthetic due to the presence of both an amide and an ester intermediate chain in its chemical structure that contributes to rapid drug metabolism [3]. It is also unique in that it consists of a thiophene ring instead of a benzene ring, which significantly increases the lipid solubility of articaine [4–6].
The thiophene ring consists of a sulfur molecule, which has led some practitioners to avoid the use of articaine in patients with sulfur- and sulfa-based drug allergies [5, 6]. Nonetheless, articaine remains a very popular local anesthetic worldwide, especially in Europe. Articaine appears to be a safe and effective drug for use with routine clinical dental procedures, and its adverse effects are very rare [7].
The infiltration and inferior alveolar nerve block (IANB) techniques are the most frequently utilized injection techniques for achieving local anesthesia in a variety of oral surgeries [3]. Mandibular infiltration has been routinely avoided in treating mandibular molars due to its questionable effectiveness, likely arising due to a thickness of a buccal cortical plate, which precludes dissemination of the local anesthetic solution [8]. Infiltration anesthesia is a common method used to anesthetize maxillary teeth [3].
The IANB injection is the anesthetic technique of choice when extracting lower mandibular posterior teeth. However, this technique does not always result in successful pulpal anesthesia, as highlighted by failure rates that are reported to range from 20 to 25 %. Some authors attribute this failure rate to the limited accessibility to the inferior alveolar nerve and a wide anatomical variation among patients [9]. The IANB technique involves insertion of a needle near the mandibular foramen in order to deposit a local anesthetic solution in close proximity to the nerve before it enters the foramen. The use of IANB is associated with several complications, which include pain, trismus, needle breakage at the point of injection, facial paralysis, and hematoma [10, 11]. Other, less frequent, complications include extraocular muscle paralysis and necrosis of the skin of the chin [12]. Recently, practicing clinicians started investigating the possibility of making the infiltration anesthesia an effective alternative to the IANB approach [13–17]. The duration of IANB and its associated discomfort due to lip and tongue numbness usually exceeds the length of the dental treatment, especially extraction.
The aim of this study was to investigate the effectiveness of a local anesthetic agent comprising of 4 % articaine with 1:100,000 adrenaline, administered through the infiltration technique prior to the extraction of mandibular permanent first molar teeth.
Materials and methods
This prospective controlled study followed a split mouth protocol and involved 56 patients, who were referred from the Initial Treatment Unit of the Dental Teaching Center to Oral and Maxillofacial Surgery Clinics at Faculty of Dentistry at Jordan, University of Science and Technology, for the extraction of bilateral mandibular permanent first molar teeth.
In order to participate in the study, patients had to be above the age of 18, have no relevant medical history, and not be taking any medication that would alter pain perception, such as opioids. These inclusion criteria were applied by viewing participants’ written health histories and asking patients to provide pertinent information.
Patients were excluded from the study if they met any of the following criteria: familiarity with the researcher, known or suspected allergies to local anesthetics or sulfites, pregnancy, history of significant medical conditions (American Society of Anesthesiology Class II or higher), an active infection or presence of pus at the site of injection, need for an emergency extraction because of intense pain, inability to provide informed consent, and failure of local anesthesia after more than half an hour.
The lower first molars of patients that were recruited for the study were examined clinically and radiographically for the presence of any signs of periodontal disease, including, tooth mobility, bone resorption, and periapical pathosis.
After the treatment was explained to the patient, he/she was encouraged to ask questions to alleviate any worries or doubts before signing the consent form. Approval was obtained from the Institutional Review Board (IRB), at Jordan University of Science and Technology. All recruited patients provided informed written consent. Prior to commencing the treatment, all participants were interviewed by the researcher in the Oral and Maxillofacial Surgery Clinic using a health history form for recording the following data: name, gender, age, job, marital status, address phone number, medical history, medications, oral hygiene measures, past dental history, and social history (including cigarette smoking frequency and the number of cigarettes smoked per day, whereby those that reported ≥5 were considered smokers).
Of the original 56 patients, 52 met the inclusion criteria and reported none of the exclusion criteria. These patients received two separate injections, whereby a combination of Buccal and lingual infiltration injections was administered on one side of the mouth, whereas a standard IANB was employed on the other, via a 1.8-ml cartridge of 4 % articaine with 1:100,000 epinephrine (Septanest, Septodont, Saint Maur des Fossés, Cedex, France). Each patient received each treatment over two visits, separated by at least 1 week. All anesthetic injections were administered by the same surgeon and no topical anesthetic was used before injection.
The infiltration injections were administered using standard cartridges of 1.8 ml 4 % articaine. For the buccal infiltration, the needle was positioned toward the mandibular first molar at the location of the apex bisecting the approximate location of the mesial and distal roots. After aspiration, the full cartridge was deposited over a period of 60 s. The lingual infiltration was administered to the lower first molar, at an approximate location at the root apices at the lingual site of the lower first molar. A 0.9 ml cartridge of articaine was deposited slowly over 30 s.
The IANB LINDSAY technique was also administered using one cartridge of 1.8 ml for the inferior alveolar and lingual nerve block and a cartridge of 0.9 ml for the long buccal nerve block. Subjective symptoms included tingling and numbness of the lower lip and tip of the tongue. Objective symptoms comprised of the absence of pain sensation during mucosal puncturing with a probe around the tooth, as well as the absence of pain at the start of extraction. Each patient was frequently asked for the incidence of lip numbness. If profound lip numbness was not achieved, the block injection was repeated by applying an additional amount of local anesthetic solution. If the waiting time to commence the surgical procedure exceeded 30 min, the patient was excluded from the study. The amount of local anesthetic solution needed to complete the extraction was recorded (expressed in ml) for both techniques.
A visual analogue scale (VAS) provides easy, sensitive, valid, and reliable means to measure a variety of subjective parameters in both clinical and research settings [18]. The most common VAS consists of a 10-cm horizontal line with one end defined as complete absence of pain and the other as the worst pain imaginable. Verbal rating scale (VRS) contains series of verbal pain descriptors pertaining to different levels of pain intensity, ranging from the least to most intense. When administering this scale, the patient is asked to choose the word that best matches the level of perceived pain. The main advantages of these scales include that they are easy and simple to score, provide validity and reliability, and can be read to the patient by the interviewer, making them particularly suitable for older individuals [19].
For the evaluation of the pain induced by the injection, three scales were employed, comprising of 100-mm VAS and two VRS (VRS1 and VRS2).
Following local anesthetic injection, each patient was asked to make a vertical mark in the line corresponding to the pain that was experienced during the injection, and the distance from the left end of the scale to the patient’s mark was used as a numerical index of the severity of pain experienced. The VRS1 allowed the patient to choose among “mild,” “moderate,” and “severe” pain. The VRS2 also offered only three categories describing the intensity of “painless than expected,” “as expected,” and “greater than expected.” All participants were first asked to complete the VAS, whereby the effectiveness of each anesthesia technique was assessed by evaluating the presence or absence of pain. The reason for extraction was also recorded.
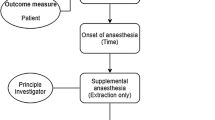
For the side of patient’s mouth on which the infiltration technique was used, after the sequence of the anesthetic administration, a 5-min waiting period was allowed to elapse before the tooth was extracted, while surreptitiously checking for lip numbness. The extraction was performed by forceps or elevator after examining local anesthetic success by puncturing the surrounding mucosa. If the patient expressed any signs of pain, waiting time was prolonged by 5-min increments, up a maximum of 30 min. If pain was still present after 30 min have elapsed, change to standard IANB was necessary and the patient was excluded from the subsequent analyses. Following tooth removal, each patient was asked to rate the pain induced by extraction using the VAS and VRS scales. The time of extraction in minutes from the first relatively painless application of forceps and elevator until complete tooth removal was also recorded. Any intraoperative complications that occurred during the extraction were recorded as well. The extraction procedure was performed by the same surgeon.
The data yielded by administering the above scales and questionnaires were numerically coded, before being analyzed using Statistical Package for Social Sciences (SPSS) software (version 15.0 SPSS® Inc., Chicago, IL, USA), descriptive statistics, paired sample t test, and independent samples t test, to determine if the differences were statistically significant (at p < .05).
Results
From the 56 patients seen at the clinic, 52 remained in the study, as four were excluded. Of those, one patient required surgical extraction with mucoperiosteal flap reflection, two patients failed to attend the next appointment scheduled for extraction of the tooth on the other side, and one individual did not respond to anesthesia within the prescribed 30 min. Thus, the study sample comprised of the remaining 52 patients, from whom 104 permanent mandibular first molar teeth were extracted. As previously noted, the split mouth study protocol was adopted, whereby 52 permanent mandibular first molar teeth of one side were extracted using the infiltration technique, whereas the other 52 teeth were extracted under the conventional inferior alveolar nerve block technique. The study sample comprised of 19 male and 33 female patients, aged from 18 to 60 years, with the mean age of 33 ± 11.26 years, as shown in Table 1.
When patients’ medical histories were analyzed, the findings revealed that 39 (75 %) participants had previous extractions in the mandible, whereas the remaining 13 (25 %) did not. In addition, 28 patients (53.8 % of the sample) reported being smokers; however, no statistically significant differences were found between smokers and nonsmokers (p = .12).
The reasons for requiring extraction included caries, retained roots, orthodontics, and endodontic failure. The extractions performed following the application of the infiltration technique included 13 (25 %) due to caries, 32 (61.5 %) due to root retention, 3 (5.8 %) due to orthodontic reasons, and 4 (7.7 %) due to endodontic failure. The extractions performed following the application of the IANB technique comprised of 10 (19.2 %) due to caries, 39 (75 %) due to root retention, and 3 (5.8 %) due to orthodontic reasons, with no teeth extracted due to endodontic failure. There were no statistically significant differences between causes of extraction between the two techniques (p = .052), as shown in Fig. 1.
Intraoperative complications that were encountered during the extraction procedure included fracture of the tooth crown or the root, trauma to the soft tissues, and pain. On the inferior alveolar nerve block side, fracture of tooth was encountered in six extractions, soft tissue trauma was recorded in one extraction, and patients reported pain in three cases, with no complications encountered in 42 extractions, which corresponds to 11.5, 1.9, 5.8, and 80.8 % of the sample, respectively. On the infiltration side, tooth fracture was encountered in seven extractions (13.5 %), with no complications in the remaining 45 extractions (86.5 %). No significant differences were noted between the two techniques (p = .10).
The amount of local anesthesia injected was recorded for both techniques (expressed in ml) and ranged from 2.7 to 5.4 ml with a mean of 3.6 ± 0.9 for IANB technique and 2.7 to 3.6 ml with a mean of 2.7 ± 0.02 for the infiltration technique. The difference between the two techniques regarding the amount of local anesthesia was statistically significant (p = .04), as shown in Fig. 2.
The waiting time between administering the IANB technique and commencing extraction ranged from 4 to 23 min with a mean of 13.13 ± 4.25, while for the infiltration technique, it ranged from 5 to 30 min with a mean of 18.55 ± 7.6. The difference in the mean waiting time between two techniques was statistically significant (p = .02), as shown in Fig. 3.
The extraction time following the application of IANB and was anesthesia ranged from 8 to 34 min with a mean of 13.42 ± 5.31 and for the infiltration technique it ranged from 7 to 27 with a mean of 16.92 ± 14.58. The difference in the extraction time between the two techniques was not statistically significant (p = .12).
The VAS scores for the pain experienced due to the IANB injection ranged from 14 to 75 mm with a mean of 41.37 ± 15.16 mm, while for the infiltration technique, the patients reported 15 to 71 mm with a mean of 38.58 ± 15.18 mm. The difference between the two techniques was not statistically significant (p = .28).
Following the application of the IANB technique, 37 (71.2 %) patients reported experiencing mild pain, and the remaining 15 (28.8 %) reported no pain, whereas severe pain was not reported by any of the patients. For the infiltration technique, 24 (65.4 %) patients reported mild pain and two (3.8 %) reported severe pain, with the remaining 26 patients reporting no pain. The difference between the two techniques was not statistically significant (p = .82).
For the IANB technique, 36 (69.2 %) patients stated that the pain experienced was less severe than they expected and none described it as greater than they expected. For the infiltration technique, 35 (67.3 %) patients noted that the pain experienced was less severe than they expected and 17 (32.7 %) rated it “as expected.” There were no statistically significant differences between the two techniques (p = .76).
The VAS scores pertaining to the extraction procedure performed following the administration of the IANB technique ranged from 0 to 70 with a mean of 16.78 ± 15.18, and for the infiltration technique, it ranged from 0 to 35 with a mean of 12.78 ± 11.73. The difference between the two techniques was statistically insignificant (p = .11).
Following the application of the IANB technique, mild pain during extraction was reported by 42 (80.8 %) patients, and only one individual (1.9 %) reported severe pain. In the infiltration technique, 37(68 %) patients reported mild pain and 15 (32 %) reported moderate pain. The difference between the two techniques was statistically significant (p = .006), as shown in Fig. 4.
Following the administration of the IANB technique, 46 (88.5 %) patients indicated that the pain they experienced was less severe than expected, while this rating was noted by 51 (98.1 %) patients in the infiltration technique. No one stated that the pain was greater than they expected in either technique. The difference between the two techniques was statistically significant (p = .02), as shown in Fig. 5.
Finally, while female patients reported overall higher mean pain ratings for injection, the gender differences were not statistically significant (p = .05).
Discussion
The long-held view that an IANB with subsequent lingual nerve block and long buccal nerve block injection is necessary to attain adequate anesthesia for the extraction of permanent mandibular teeth is now being challenged by both researchers and practitioners. The administration of a local anesthetic is the most common procedure in dentistry. While IANB is the most widely used mandibular injection technique for achieving local anesthesia for restorative and surgical procedures, it has a significant failure rate. This adverse outcome is typically attributed to its susceptibility to anatomical variations in the mandibular foramen and difficulty of anesthetizing a number of accessory innervations pathways [20]. Infiltration anesthesia is the most frequently employed technique in the upper jaw through which pulpal anesthesia is gained by diffusion of local anesthetic solution into the cancellous bone via the thin cortical plate of the maxillary alveolus [13]. Several authors have conducted studies comparing pain from various forms of anesthetic [14–16]. However, to our knowledge, no controlled trials comparing pain experienced with these two approaches to anesthetic injection have been conducted to date. The use of primary infiltration anesthetic technique when treating or extracting the mandibular teeth has been investigated in the past, with some studies reporting that infiltration is effective for many treatments in the mandibular deciduous dentition [21, 22]. Corbett et al. [16] compared the efficacy of buccal infiltration with Articaine to buccal plus lingual infiltration with articaine, whereby the mean pain score for the of overall injection was 20.9 mm on a 100-mm VAS without topical anesthesia. Buccal alone and buccal plus lingual infiltration injections were also compared for efficacy of pulpal anesthesia of the mandibular first molar using lidocaine in a study by Meechan and Kanaa [23]. In addition, 95 % success was shown for mandibular premolar forceps extraction with buccal infiltration with articaine only [24, 25]. Infiltration in the buccal vestibule opposite the mandibular first molar by A100 3.6 mL may be a good option for extraction of mandibular third molars, with supplemental lingual anesthesia [26]. Buccal infiltration at the first mandibular molar is more effective than lingual infiltration in the same region in obtaining anesthesia of the mandibular first molar and premolar teeth [27].The pain of the local anesthetic injection is known to be poorly tolerated by patients. It provides many advantages over block technique, because it is simple to use, more comfortable to patients, provides hemostasis, counters collateral supply, avoids nerve trunk damage (particularly inferior alveolar nerve block which is frequently used), minimizes the risk of intravascular injection, is safer in bleeding diatheses such as hemophilia, and minimizes needle stick injury [13]. Authors of two recent investigations reported that articaine was superior to lidocaine in producing pulpal anesthesia in the mandibular first molars after buccal infiltration [14, 15]. Therefore, this study evaluated pulpal anesthesia using articaine for extraction of mandibular permanent first molar teeth. Articaine has the clinical reputation for successfully penetrating bone, allowing successful pulpal anesthesia of mandibular teeth with buccal injection. Thus, practitioners could use this technique routinely to anesthetize the mandibular posterior teeth and avoid the lip numbness typically associated an inferior alveolar nerve block. Some authors have shown that only buccal or buccal plus lingual infiltrations could provide successful anesthesia, in 32 % to 67 % of patients with lidocaine and 57 % to 92 % with articaine, even without giving standard IANB [14–16, 23]. Corbett et al. [16] found that efficacy of buccal or buccal plus lingual infiltrations of 4 % articaine with epinephrine for first molar pulp anesthesia was similar to that of an IANB using lidocaine with epinephrine. Some studies also indicate that articaine is able to diffuse through soft and hard tissues more reliably than other local anesthetics. Moreover, pertinent literature suggests that mandibular buccal infiltration of articaine provides pulpal anesthesia of the lower first molar, obviating the need for an IANB [16]. The purpose of the current study was to evaluate the possibility of extracting the mandibular molar teeth by infiltration technique, as well as compare the patients’ perceived level of pain associated with both injection and extraction. In this investigation, no study power or sample size calculations were performed. The research protocol chosen was split mouth, whereby the extraction of permanent lower first molars in both sides was performed in each study participant.
The study population comprised of 52 patients, of whom 19 were males and 33 females. The participants were aged 18 to 60 years, with an average of 33 years. The age range in this study was similar to that in the sample of another study [15]; however, the mean age in this study is higher. Subjects younger than 18 years were not included in this study, since evidence suggests that young patients may find the process challenging due to psychological aspects, such as strong anxiety, possibly leading to panic, in addition to the potential difficulty of evaluating pain [25]. Regarding previous extractions in the mandible, only Uckan et al. [28] considered this variable in the recruitment of their sample, with the experience of previous extraction in the maxilla being a condition of inclusion in their study. In the present study, such experience was not required for inclusion. However, previous extraction experience yielded statistically significant differences in pain perception among the participants (p = .03). Therefore, we posit that some of the patients that required extraction in the past may have had negative experience, which would likely affect their pain rating. In addition, patients’ smoking status was based on their self-reports rather than measurement of nicotine level, even though relying on patients to provide this data has been found to lead to underestimates of up to 4 % [29]. In this study, all individuals that noted smoking ≥5 cigarettes per day were classified as smokers, whereas all others were classified as nonsmokers. Still, the pain perceptions were unaffected by this variable, as no statistically significant differences between smokers and nonsmokers were noted (p = .12).
The bilateral permanent mandibular first molars were extracted to conduct this study that adopted split mouth design, in line with the work of Padhye et al. [30] The lower permanent first molar was chosen due to many clinical trials conducted in endodontic field, focusing on this tooth. Some studies also assessed it for possibility of pulpal anesthesia using an infiltration technique only, owing to the slightly thinner buccal plate compared to the most posterior teeth [3].
In the present study, the reasons for tooth extraction included caries, orthodontics, remaining roots, and endodontic failures and had no effect on the study results (p = .052). Patients that presented with any signs of periodontal disease were excluded from the study because a decrease in the bony support around these teeth may facilitate the escapement of buccally or lingually administered local anesthesia to periodontal ligament. As a result, this becomes intraligamentary anesthesia administration, rather than infiltration, which would adversely affect the accuracy of results of the study that investigates the ability of local anesthetic agent to pass through a bony barrier buccally and lingually. Similarly, because the effect of local anesthetic decreases, patients with symptomatic teeth that required an emergency extraction due to irreversible pulpitis were excluded from the study. In fact, available evidence suggests that local anesthetic failure is eight times higher in symptomatic teeth, due to irreversible pulpitis, compared to normal vital teeth [15], and thus may need repeated block to be anesthetized due to hyperalgesia [31]. Furthermore, patients presenting with teeth showing any signs of symptomatic periapical infection or surrounding inflammation were also excluded because, during inflammation, polymodal nociceptors are sensitized and their excitation threshold declines, whereby even light normally innocuous stimuli would activate them and cause pain. Because all injections were given by the same practitioner, operator difference was not a factor in the findings of this study.
Intraoperative complications that were encountered during the extraction procedure included fracture of the tooth, whether fracture of the crown or the root, soft tissue trauma, and intolerable pain. Supplemental anesthesia according to the study protocol was administered to patients that reported intolerable pain. The difference in the occurrence of intraoperative complications between the two techniques was not statistically significant (p = .10). In addition, the amounts of buccally and lingually administered local anesthesia were recorded for each patient (in ml) until complete tooth removal. As the researcher performed all procedures and measurements, any errors introduced could be ignored, since they would apply equally to both techniques. The mean amount of buccally and lingually administered local anesthesia was significantly different between the two treatments (p = .04). This clearly demonstrates that, if the IANB is to be avoided, less local anesthetic could be used. This is most likely because three sites would be anesthetized (inferior alveolar, lingual, and long buccal), which require a proper technique with an adequate amount of solution. In the infiltration technique, a larger volume with higher concentration of anesthetic agent is deposited closely to the tooth, assuming that articaine is capable to penetrate and diffuse through dense compact bone to reach the sensory supply of the tooth [3]. In fact, in the case of 2 % lidocaine with epinephrine, 2 ml of anesthetic solution was reported effective [32]. Therefore, in the present study, all patients were given only 1.5 cartridge for the infiltration technique, with a similar amount used for IANB, lingual, and long buccal nerve blocks before beginning the extraction procedure. Moreover, additional anesthesia was delivered only when it was judged that it was needed to complete the procedure. In the current study, the volume of anesthetic agent was similar for both techniques. The protocol of local anesthetic administration adopted in this work allowed adequate waiting time and amount of local anesthesia in both techniques to diffuse and provide adequate anesthesia for both hard and soft tissues. Thus, if the desired effect was not achieved at the end of the procedure, it would be the result of inability of the anesthetic solution to diffuse through thick bony barriers. As previously noted, waiting time was measured from the time of the needle insertion until the appropriate manifestation of anesthesia suitable for whatever work is to be carried out painlessly and was recorded for both techniques. The mean waiting time in the infiltration technique was longer than for the IANB technique and this difference was statistically significant (p = .02). This finding suggests that, in the infiltration technique, longer time was needed to allow the anesthetic agent to pass through thick bony tissue to reach and anesthetize the pulp of the molar teeth, compared with the IANB, which deposited the anesthetic agent near the mandibular foramen, where the main inferior alveolar nerve trunk enters the mandible. The waiting times for the IANB ranged from 5 to 20 min with a mean of 10.13 ± 4.25, whereas for the infiltration technique, it ranged from 5 to 30 min with a mean of 20.55 ± 7.6. These values are similar to the findings reported elsewhere, as the authors reported that higher diffusion of articaine was obtained after a waiting period of 15 min [33]. Extraction time was recorded for each patient, measured in minutes from the relatively pain-free application of an elevator or forceps until total removal of the tooth from its socket. The difference in the mean of extraction time between the two techniques was statistically insignificant (p = .12). This suggests that extraction difficulty was comparable between the two techniques, strengthening the study results. The IANB was administered first, in order to lessen the stress for the patient due to waiting for a long period and the patient was encouraged to come to the next visit for the infiltration technique. Topical anesthesia was not applied prior to needle insertion in this study because the efficacy of topical anesthesia in posterior mandible is questionable and it may be considered as a confounding variable that can mask the subject’s pain perception [34]. A 25-gauge needle was used, as it has been shown to minimize needle deflection because of its larger diameter and heavier construction [35]. In addition, local anesthetic solution was deposited over a period of 1 min. The adequacy of anesthesia was determined by the presence or absence of pain, as indicated by the patient. The perception of pain induced by the injection and the pain perception during extraction were assessed using one visual analogue scale and two verbal rating scales in all subjects. As suggested by Brigg and Closs [20], the VAS scores were obtained before administering the VRS, to minimize bias caused by patient trying to match the word chosen with a mark on the VAS. The main advantage of these scales is that they directly measure the level of discomfort perceived by the patient and are considered to have a good reliability and validity when participants self-report the pertinent information [20]. While the VAS is more sensitive and allows the use of parametric statistical methods, the VRS is easier to administer, especially for elderly patients, as well as allows for nonparametric statistical methods. [36] Therefore, in order to increase the reliability of the study results, three different scales were used. Many authors used a combination of VAS and VRS to assess patients’ perceptions of pain during the anesthetic injections and extractions [28, 37, 38]. Subjects were instructed to score the VAS based on the overall level of discomfort experienced during the injection. In this study, the experienced injection pain and discomfort is possibly due to the needle piercing through the mucosa, the needle tip hitting periosteum, the rate of local anesthetic deposition, and the expansion of the tissue in the pterygomandibular space on one side and buccal with lingual tissues on the other side [39]. The mean VAS score associated with the two techniques was comparable (p = .28), which is in contrast with the findings reported by Sharaf [20]. The difference in pain perception between the infiltration and IANB is, on the other hand, similar to that reported by Jung et al. [16] The results of VAS regarding the injection pain were mirrored by the result of VRS1, where the vast majority of patients rated the injection pain associated with both techniques as mild, with a few individuals rating it as moderate and none as severe. The difference between the two techniques was not statistically significant (p = .82). On the other hand, when rating the injection pain associated with IANB, only half of the patients noted it as mild, with a similar number experiencing moderate pain and some reporting severe pain. The VRS2 results revealed that the vast majority of patients expected the injections to be more painful than they actually are. Moreover, it seems that patients in general expect the infiltration injection to be more painful than the IANB one. This is probably the reason behind lack of significant differences between the two techniques with respect to the expected injection-related pain (p = 0.76). It is likely that previous extraction experience prepares patients for pain associated with injections. The majority of patients in this study had previous extractions and hence injections in the mandible. When the VAS scores for the extraction itself are considered, no significant differences between the two techniques were noted (p = 0.11). On the other hand, the VRS1 scores for pain induced by extraction revealed statistically significant differences between the two techniques. The vast majority of participants rated pain of extraction as either mild or moderate, with only a few rating it as severe. These differences can be explained by varying pain thresholds among patients and the intense pressure felt by some patients during the extraction, which may be difficult to differentiate from pain. Regarding patient’s expectation of extraction pain, the VRS2 scores pertaining to the two techniques indicate that the difference in the extraction pain perception was not due to the anesthetic injection. In addition, the fact that the majority of patients, regardless of the technique, noted that the pain was less severe than they expected is difficult to explain, given that the majority had mandibular extraction in the past. It is possible that the fear of tooth extraction exaggerated patient’s expectation before the actual extraction. The VAS and VRS results for the extractions suggest that the extraction of mandibular molar teeth without the administration of IANB injection is possible, whereby the buccal and lingual administration of articaine is used instead. This study was designed so that IANB injections would be given to any patient for whom the infiltration approach was insufficient. However, none of the participants required additional IANB injection. This makes the success rate of infiltration technique for mandibular first molar extraction without IANB 100 %. When extraction reasons were ranked according to their respective success rates, the order was remaining roots > orthodontic treatment > profound caries > endodontic failure. This finding can be explained by the fact that most of the extractions were performed on root remnants, with only a small percentage of vital pulp teeth. The pain that occurred due to the IANB failure can probably be ascribed to the presence of accessory innervations, anatomical variations, or faulty technique.
While female patients reported overall higher mean pain ratings for injection, the gender differences were not statistically significantly different (p = .05). When the type of injection was ignored in the analyses and the pain perceptions of male and female patients were compared, the extraction-related pain was significantly higher in female than in male group (p = .01), which can be explained by the posited lower pain threshold in females [39]. On the other hand, Unruh [40] reported that females have higher pain tolerance, experience pain more frequently, and can endure pain for longer periods compared to males. In addition, the perception of extraction pain was found to increase with extraction duration, which is consistent with the findings reported by Badcock et al. [39] However, when the type of injection was ignored in the analyses, the reason for the tooth extraction did not affect the perception of extraction pain, which contradicts the findings reported by Fan et al. [38] Although these authors stated that articaine is associated with nerve sensation alteration more highly than other local anesthetic agents, none of the participants in the present study experienced this complication. However, a comparison of the two injection techniques for extraction of lower molar teeth has never been conducted in the past. In this study, lip numbness that occurred in five patients following the infiltration technique may be due to wide diffusion of the local anesthetic agent Articaine to the mental foramen due to the close proximity of injection site to the mental foramen. Phillips et al [41] noted that the foramen is aligned with the long axis of the second premolar in 63 % cases. In addition, when the foramen was mesial or distal to the long axis of the second premolar, it was within 2 mm of the long axis.
References
Haas DA (2002) An update on local anesthetics in dentistry. J Can Dent Assoc 68:546–551
Peterson LJ (2003) Contemporary oral and maxillofacial surgery, 4th edn. Mosby, St Louis
Malamed SF, Gagnon S, Leblanc D (2000) Efficacy of articaine: a new amide local anesthetic. J Am Dent Assoc 131:635–642
Van Oss GE, Vree TB, Baars AM, Termond EF, Booij LH (1989) Pharmacokinetics, metabolism, and renal excretion of articaine and its metabolite articainic acid in patients after epidural administration. Eur J Anaesthesiol 6:49–56
Lima JLJ, Dias-Ribeiro E, Ferreira-Rocha J, Soares R, FW C, Fan S, Sant’ana E (2013) Comparison of buccal infiltration of 4 % articaine with 1: 100,000 and 1: 200,000 epinephrine for extraction of maxillary third molars with pericoronitis: a pilot study. Anesth Prog 60:42–45 6
Oertel R, Rahn R, Kirch W (1997) Clinical pharmacokinetics of articaine. Clin Pharmacokinet 33:417–425
Kakroudi SH, Mehta S, Millar BJ (2015) Articaine hydrochloride: is it the solution? Dent Update 42:88–90 92-93
Wong MK, Jacobsen PL (1992) Reasons for local anesthesia failures. J Am Dent Assoc 123:69–73
Smyth J, Marley J (2010) An unusual delayed complication of inferior alveolar nerve block. Br J Oral Maxillofac Surg 48:51–52
Chevalier V, Arbab-Chirani R, Tea SH, Roux M (2010) Facial palsy after inferior alveolar nerve block: case report and review of literature. Int J Oral Maxillofac Surg 39:1139–1142
Torrnte-Castells E, Gargallo-Albiol J, Rodriguez-Baeza A, Berini-Aytes L, Gay-Escoda C (2008) Necrosis of the skin of the chin: a possible complication of inferior alveolar nerve block injection. J Am Dent Assoc 139:1625–1630
Meechan JG (2010) Infiltration for the mandible. Int Endod J 10:221–229
Kanaa MD, Whitworth JM, Corbett IP, Meechan JG (2006) Articaine and lidocaine mandibular buccal infiltration anesthesia: a prospective randomized double-blind cross-over study. J Endod 32:296–298
Robertson D, Nusstein J, Reader A, Beck M, McCartney M (2007) The anesthetic efficacy of articaine in buccal infiltration of mandibular posterior teeth. J Am Dent Assoc 138:1104–1112
Jung IY, Kim JH, Kim ES, Lee CY, Lee SJ (2008) An evaluation of buccal infiltrations and inferior alveolar nerve blocks in pulpal anesthesia for mandibular first molars. J Endod 34:11–13
Corbett IP, Kanaa MD, Whitworth JM, Meechan JG (2008a) Articaine infiltration for anesthesia of mandibular first molars. J Endod 34:514–518
Huskisson EC (1983) Pain measurement and assessment, Raven Press. New York, NY. IASP, Sub-committee on Taxonomy (1980). Pain terms: a list with definitions and notes on usage. Pain 8:249–452
Kaltz J, Melzack R (1999) Measurement of pain. Surg Clin North Am 79:231–252
Hannan L, Reader A, Nist R (1999) The use of ultrasound for guiding needle placement for inferior alveolar nerve blocks. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87:658–665
Briggs M, Closs JS (1999) A description study of the use of visual analogue scales and verbal rating scales for the assessment of post-operative pain in orthopedic patients. J Pain Symptom Manag 18:438–446
Oulis CJ, Vadiakas GP, Vasilopoulou A (1996) The effectiveness of mandibular infiltration compared to mandibular block anesthesia in treating primary molars in children. Pediatr Dent 18:301–305
Sharaf AA (1997) Evaluation of mandibular infiltration versus block anesthesia in pediatric dentistry. J Dent Child 64:276–281
Meechan JG, Kanaa MD, Corbett IP (2006) Pulpal anaesthesia for mandibular permanent first molar teeth: a comparison of buccal and buccal plus lingual infiltration injections. Int Endod J 39:764–769
Kirsch A (1985) Ultracaine product monograph. Hoechst Canada Inc, Montreal
Schulze-Husman M. 1974 Experimental evaluation of the new local anesthetic ultracaine in dental practice. Dissertation, Bonn, West Germany;
El-Kholey KE (2013) Infiltration anesthesia for extraction of the mandibular molars. J Oral Maxillofac Surg 71:1658.e1–1658.e5
Meechan JG, Jaber AA, Corbett IP, Whitworth JM (2011) Buccal versus lingual articaine infiltration for mandibular tooth anaesthesia: a randomized controlled trial. Int Endod J 44:676–681
Uckan S, Dayangac E, Araz K (2006) Is permanent maxillary tooth removal without palatal injection possible? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102:733–735
Wagenknech LE, Burke GL, Perkins LL, Haley NJ, Friedman GD (1992) Misclassification of smoking status in the cardiac study: a comparison of self-report with serum cotinine levels (abstract). Am J Pub Heal 82:33–36
Padhye M, Girotra C, Shah P (2009) Comparison of Efficacy of 4 % articaine with 1:100,000 adrenaline to that of 2 % lignocaine with 1:80,000 adrenaline in exodontia cases. Scientific J l3:1–5
Budenz AW (2003) Local anesthetics in dentistry: then and now. J Calif Dent Assoc 31:388–396
Tortamano IP, Siviero M, Costa CG, Buscariolo IA, Armonia PL (2009) A comparison of the anesthetic efficacy of articaine and lidocaine in patients with irreversible pulpitis. J Endod 35:165–168
Lima-Júnior JL, Dias-Ribeiro E, de Araújo TN (2009) Evaluation of the buccal vestibule-palatal diffusion of 4 % articaine hydrochloride in impacted maxillary third molar extractions. Med Oral Patol Oral Cir Bucal 14:e129–e132
Nakanishi O, Haas DA, Ishikawa T, Kameyama S, Nishi M (1996) Efficacy of mandibular topical anesthesia varies with the site of administration. Anesth Prog 43:14–19
Robison SF, Mayhew RB, Cowan RD, Hawley RJ (1984) Comparative study of deflection characteristics and fragility of 25, 27, and 30 gauge short dental needles. Journal of the Am Dent Assoc 109:920–924
Oliveira PC, Volpato MC, Ramacciato JC, Ranali J (2004) Articaine and lignocaine efficiency in infiltration anaesthesia: a pilot study. Br Dent J 197:45–46
Jakobs W, Ladwig B, Cichon P, Ortel R, Kirch W (1995) Serum levels of articaine 2 % and 4 % in children. Anesth Prog 42:113–115
Fan S, Chen WL, Pan CB (2009) Anesthetic efficacy of inferior alveolar nerve block plus buccal infiltration or periodontal ligament injections with articaine in patients with irreversible pulpitis in the mandibular first molar. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:89–93
Badcock ME, Gordon I, McCullough MJ (2007) A blinded randomized controlled trial comparing lignocaine and placebo administration to the palate for removal of maxillary third molars. Int J Oral Maxillofac Surg 36:1177–1182
Unruh AM 1996 Gender variations in clinical pain experience. 65:123–167
Phillips JL, Weller RN, Kulild JC (1990) The mental foramen: size, orientation, and positional relationship to the mandibular second premolar. J Endod 16:221–223
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
This study received no funding.
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bataineh, A.B., Alwarafi, M.A. Patient’s pain perception during mandibular molar extraction with articaine: a comparison study between infiltration and inferior alveolar nerve block. Clin Oral Invest 20, 2241–2250 (2016). https://doi.org/10.1007/s00784-016-1712-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-016-1712-8