Abstract
Obesity is a globally common metabolic condition that causes or exacerbates many diseases. High-intensity interval training (HIIT) and orlistat may affect cytokines and adipokines related to obesity. The purpose of this study was to investigate the independent and combined effects of 8 weeks of HIIT and orlistat on body weight, body mass index (BMI), neck circumference, aerobic power, interleukin‑6 (IL-6), tumor necrosis factor α (TNF-α), resistin, and adiponectin in young, obese women. 48 obese individuals were randomly divided into 4 groups: control-placebo (n = 12), HIIT-placebo (n = 12), control-orlistat (n = 12), and HIIT-orlistat (n = 12), and received group-specific interventions. Participant blood samples were taken 48 h before the intervention and 48 h after the last training session. Two-way multivariate analysis of covariance (MANCOVA) was used to investigate the effects of interventions, with significance set at P ≤ 0.05. The results showed that HIIT decreased body weight, BMI, neck circumference, TNF‑α, and resistin concentration, while increasing aerobic power, IL‑6, and adiponectin concentration. Orlistat decreased body weight, BMI, neck circumference, and resistin, and increased plasma IL‑6 levels. In conclusion, although the combined effects of HIIT and orlistat were significant in many factors, no synergistic effect was observed, and there appears to be a limit for changes in each factor that can be reached by either HIIT or medication interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Obesity is a globally common metabolic condition that causes or exacerbates many diseases (Kyrou, Randeva, Tsigos, Kaltsas, & Weickert, 2000). There are many physiological factors whose changes are associated with changes in fat accumulation and obesity (Saiga, Watanabe, & Yoshioka, 2013; Smith & Ravussin, 2005). Cytokines and adipokines are two of the most important physiological factors in obesity (Shi et al., 2016).
Interleukin‑6 (IL-6) is a multifunctional, pro-inflammatory cytokine produced by various cells such as immune cells, fibroblasts, endothelial cells, myocytes, and endocrine cells (Hou et al., 2008; Murakami, Kamimura, & Hirano, 2019). Tumor necrosis factor α (TNF-α) cytokine acts as a regulator of gene expression in adipocytes and is associated with obesity (Kern et al., 2018; Ruan, Hacohen, Golub, Van Parijs, & Lodish, 2002). Resistin is a pro-inflammatory factor secreted from adipose tissue (Zhao et al., 2019). Resistin is found in adipocytes and various cells, including peripheral blood mononuclear cells, macrophages, and bone marrow cells, and is involved in inflammatory conditions in humans (Jamaluddin, Weakley, Yao, & Chen, 2012). Although small amounts of resistin are secreted in adipose tissue in humans, obesity and visceral fat have been shown to express greater resistin levels in macrophage, liver, spleen, lung, and placenta cells (Makki, Froguel, & Wolowczuk, 2013). Adiponectin is a peptide hormone that is secreted from adipose tissue in humans and affects fat and glucose metabolism (Achari & Jain, 2017). Adiponectin reduces glucose output from the liver by increasing the liver’s sensitivity to insulin; it also increases glucose consumption in the muscles and prevents an increase in blood sugar and fat accumulation (Stern, Rutkowski, & Scherer, 2016). Overall, studies have shown that elevated levels of interleukin‑6, TNF‑α, and resistin are positively associated with obesity and body mass index (BMI; Azuma et al., 2003; Sindhu et al., 2015). There is also a negative relationship between obesity adiponectin levels and body mass index (Cohen et al., 2011).
Previous studies have shown a link between anthropometric indices and obesity-related diseases. For example, waist–hip ratio (WHR), BMI, waist circumference (WC), and hip circumference have been shown to be predictors of diabetes and hypertension (Wang et al., 2018; Y. Zhang et al., 2019), and WHR is a better predictor than BMI and WC (Y. Zhang et al., 2019). Measuring the circumference of the neck is one of the newer anthropometric indices that have been shown to be associated with obesity and cardiovascular disease (Alfadhli et al., 2017; Pei et al., 2018; J. Zhang et al., 2018).
Orlistat medication, which is has been approved by the U.S. Food and Drug Administration (FDA), is the subject of much medical attention at present. The drug was manufactured in 1998 and is widely available in pharmaceutical and medical centers. Orlistat is an enteric lipase enzyme inhibitor, marketed in the form of Xenical (Xenical, Aburaihan Pharmaceutical Co., Theran, Iran) 120 mg oral capsules, and is prescribed to people with a BMI above 28 (Krempf et al., 2003). The medication comprises a capsule that is administered at the same time or 1 h after each meal, with a fatty diet (Heck, Yanovski, & Calis, 2000; Sumithran & Proietto, 2014). Orlistat improves carbohydrate metabolism in healthy obese individuals or pre-diabetics (Mancini & Halpern, 2008; Oh, 2019). Orlistat also has beneficial regulatory effects on TNF‑α, adiponectin, resistin, lipid profiles, and insulin-resistance parameters (Derosa, Cicero, D’Angelo, Fogari, & Maffioli, 2012; Derosa et al., 2010). It has been shown that a hypocaloric diet + orlistat had more effect than diet alone on adipokines, CRP, TNF‑α, triglycerides, insulin-like growth factor (IGF)-1, and oxidative stress in obese women (Bougoulia, Triantos, & Koliakos, 2006).
In this study, high-intensity interval training (HIIT) and orlistat are considered as two potential contributors to changes in inflammation and obesity that may enhance or act independently of each other. The reason for selection of a HIIT program is its popularity, which is due to its usefulness and time-effectiveness (Nicolò & Girardi, 2016; Rahmati-Ahmadabad, Azarbayjani, Farzanegi, & Moradi, 2019; Ramírez-Vélez et al., 2019).
Rahmati-Ahmadabad et al., for example, showed that HIIT had a greater effect on the genes involved in reverse cholesterol transfer, along with better time-effectiveness than moderate-intensity continuous aerobic training (Rahmati-Ahmadabad et al., 2019). Some, but not all, studies have suggested a difference between HIIT and continuous training regarding cardiorespiratory fitness (Hannan et al., 2018).
The purpose of this study was to investigate the independent and interactive effects of 8 weeks of HIIT and orlistat on BMI, aerobic power, IL‑6, TNF‑α, resistin, and adiponectin in women with obesity.
Methods
Ethical considerations
The Research Ethics Committee of the Medical University, Alborz, Iran, approved the experimental protocol of the study (Ethical Code: 1390.40). This study was registered at Islamic Azad University, Central Tehran Branch, Iran (registration number: 10121423972005). This research was conducted in accordance with the principles stated in the Declaration of Helsinki. Before participating in the investigation, participants were informed about the study and each participant signed an institutionally approved informed consent document.
Research design
The method of this study was a double-blind randomized clinical trial with a pre-test/post-test design. The participants were identified using their codes instead of their actual names. A third party was asked to classify the participants randomly, using the (labelled) codes. Study groups also were given codes instead of names. The laboratory was blinded to the group names and only used the codes. Group codes were used in statistical analysis. Additionally, the supplement and placebo participants were unaware of their own group label. The participants did not know about the details of the exercise protocol. The control groups completed the warmup and cool down stages of the exercise protocol. Therefore, the participants of the control groups were blinded regarding exercise.
The statistical population of this study comprised volunteer obese women aged 18–23 in Tehran, with a BMI above 30 kg/m2.
Inclusion criteria included female students in the age range 18–23 years; regular menstruation; BMI above 30 kg/m2; non-participation in a specific exercise and/or diet program (6 months before the start of the study); no skeletal, thyroid, kidney, cardiovascular, and diabetic conditions; no anemia; no prescription medication; having a regular sleep cycle; and being a non-smoker. Any individuals who failed to meet the inclusion criteria based on the completed questionnaires were excluded from the study. It should be noted that the sample size in the present study was determined based on previous studies. The present study did not use a priori sample size estimation but used post-hoc power calculation. The post-hoc power calculation for each variable was > 0.85.
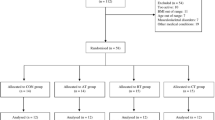
After initial evaluation, 48 eligible individuals were randomly divided into 4 groups: control-placebo (n = 12), HIIT-placebo (n = 12), control-orlistat (n = 12), and HIIT-orlistat (n = 12), each receiving a group-specific intervention. It should be noted that participants were requested to commence participation in the study 10 days after their most recent menstruation.
Exercise training protocol
A high-intensity interval training (HIIT) program was conducted for 8 weeks, with three sessions per week (exercise intensity was based on peak heart rate [HRpeak]). The remaining sections of the training program included brisk walking at an intensity of about 55% of HRpeak. In the present study, both the HIIT and HIIT + orlistat groups completed the training program for 8 weeks (Table 1). The exercise training was conducted on alternate days between 5:00 pm and 7:00 pm. Participants also performed 20 min of warmup and 20 min of cool-down, involving a variety of running, stretching, and elasticity exercises before and after each training session. Due to the fact that the participants exercised at high intensity, a doctor was constantly present during the procedure. The doctor remained near the participants at all times and monitored their heart rate and facial expressions. During the entire running exercise, a person stood behind the treadmill to prevent the participant from falling if she lost her balance.
Administration of orlistat
In the present study, the orlistat group and the HIIT + orlistat group received 3 capsules of 120 mg orlistat daily (Krempf et al., 2003) for 8 weeks. The capsules were manufactured by Aboureihan Company, Iran. Participants in the orlistat groups took one capsule after breakfast, lunch, and dinner, while the other groups received a placebo.
Blood sampling
Following 12 h of fasting, 10 cc of venous blood was obtained from the participants’ left arms using sterile venoject syringes containing an anticoagulant, both pre-test (48 h before the training program) and post-test (48 h after the training program). The mean blood sampling temperature was recorded at between 23 and 25 °C at both stages. The samples were taken in the same laboratory conditions in terms of temperature, light, humidity, and time of day (8:00–9:00am). The blood tubes were centrifuged at 4000 rpm for 5 min to separate the clot from the serum. Then the serum samples were frozen by liquid nitrogen and stored at −70 °C for subsequent analysis. It should be noted that in order to minimize the acute effects of training, participants did not exercise for 2 days prior to the measurements. Although orlistat has a lasting effect, the participants did not consume it 2 days prior to the measurements and were asked not to change their diet in the period before blood samples were taken.
Measuring research variables
To measure the participants’ weight, height, and neck circumference, the following tools were used, respectively: Chinese King Digital Scale (1-gram accuracy); Iran Kaveh Model 1124 height measuring scale; standard tape measure.
BMI was obtained by dividing the person’s weight in kilograms by the height in meters squared (x2).
Bruce protocol test was used to measure maximum oxygen consumption (Vo2max). Running on a treadmill, the intensity level gradually increased until the subjects withdrew due to excessive fatigue. The test was performed in six 3‑minute steps that varied in velocity and slope percentage in each step. The first step started at a speed of 2.7 km/h and a 10% slope, and then the speed and slope were added at a constant ratio at each stage. Specifically, 2% was added to the slope and the velocity increased from an initial 2.7 to 5.5 km/h by the fifth stage. The maximum oxygen consumption was determined based on the time taken in the test and the relevant tables.
All measurements (IL‑6, TNF‑α, resistin, and adiponectin) were taken using ELISA kits. IL-6: German ZellBio kit (ZellBio GmbH, Lonsee, Germany), sensitivity of 0.5 ng/ml and intra-assay coefficient of variation 1.1%; TNF-α: Swedish Mercodia Co (Mercodia, Uppsala, Sweden), sensitivity of 0.16 pg/ml and intra-assay coefficient of variation 2.1%; resistin: sensitivity of 0.5 ng/ml and intra-assay coefficient of variation 1.02%; adiponectin: sensitivity of 0.5 ng/ml and intra-assay coefficient of variation 0.085%.
Statistical analysis
Data were described in terms of mean and standard deviation. Assumptions about the use of multivariate analysis of covariance (MANCOVA) were tested, such as the normality of data distribution, variance homogeneity, absence of multi-collinearity, etc. The Shapiro–Wilks test was used to determine the normality of data distribution, and Levene’s test to determine variance homogeneity. The relationships were calculated using the Pearson product-moment correlation. In order to test the assumptions made between the independent and interaction groups, the two-way MANCOVA parametric test was used. In order to control for the effects of (albeit small) intergroup changes in the pre-test on the post-test, all pre-test values were covaried. The effect size of each variable was also reported. The post hoc power was then calculated for each variable. Statistical analysis was performed by SPSS software (version 22) and the significance level was set at P ≤ 0.05.
Results
The mean and standard deviation of the present study variables
The mean and standard deviation of the present study variables are shown in Table 2.
Effects of HIIT, orlistat, and their combination on body weight, BMI, and neck circumference
The body weight results showed that HIIT (F 1, 43 = 75.71, P = 0.001; partial η 2 = 0.63), orlistat (F 1, 43 = 18.87, P = 0.001; partial η2 = 0.30), and a combination of HIIT and orlistat (F 1, 43 = 8.75, P = 0.005; partial η2 = 0.16) all reduced the body weight of the participants (Fig. 1a). The BMI results showed that HIIT (F 1, 43 = 218.24, P = 0.001; partial η2 = 0.83), orlistat (F 1, 43 = 122.71, P = 0.001; partial η2 = 0.74), and a combination of HIIT and orlistat (F 1, 43 = 70.26, P = 0.001; partial η2 = 0.62) all reduced the BMI of the participants (Fig. 1b). The neck circumference results showed that HIIT (F 1, 43 = 65.92, P = 0.001; partial η2 = 0.60), orlistat (F 1, 43 = 13.10, P = 0.001; partial η2 = 0.24), and a combination of HIIT and orlistat (F 1, 43 = 40.28, P = 0.001; partial η2 = 0.48) all reduced the neck circumference of the participants (Fig. 1c).
Pre- and post-test body weight (kg; a), BMI (kg/m2; b), and neck circumference (cm; c) in the groups of the present study. Data are expressed as mean ± standard deviation. The participants were 12 in each group. HIIT high-intensity interval training. aHIIT versus control. bOrlistat versus placebo. cCombination of HIIT and orlistat. BMI body mass index, IL-6 Interleukin-6, TNF-α tumour necrosis factor alpha
Effects of HIIT, orlistat, and their combination on aerobic power
The aerobic power results showed that HIIT (F 1, 43 = 150.99, P = 0.001; partial η2 = 0.77) increased the aerobic power of participants. Orlistat (F 1, 43 = 0.27, P = 0.60; partial η2 = 0.006) and a combination of HIIT and orlistat (F 1, 43 = 0.17, P = 0.67; partial η2 = 0.004) showed no significant effect on the aerobic power of the participants (Fig. 2).
Effects of HIIT, orlistat, and their combination on serum IL-6, TNF-α, resistin, and adiponectin concentrations
The serum IL‑6 results showed that HIIT (F 1, 43 = 210.55, P = 0.001; partial η2 = 0.83), orlistat (F 1, 43 = 28.78, P = 0.001; partial η2 = 0.40), and a combination of HIIT and orlistat (F 1, 43 = 4.95, P = 0.03; partial η2 = 0.10) all increased serum IL‑6 levels in the participants (Fig. 3a). The serum TNF‑α results showed that HIIT (F 1, 43 = 433.10, P = 0.001; partial η2 = 0.91) decreased TNF‑α in participants. Orlistat (F 1, 43 = 1.22, P = 0.27; partial η2 = 0.02) and a combination of HIIT and orlistat (F 1, 43 = 1.43, P = 0.23; partial η2 = 0.03) showed no significant effect on serum TNF‑α levels in the participants (Fig. 3b). The serum resistin results showed that HIIT (F 1, 43 = 35.33, P = 0.001; partial η2 = 0.45), orlistat (F 1, 43 = 81.16, P = 0.001; partial η2 = 0.65), and a combination of HIIT and orlistat (F 1, 43 = 14.91, P = 0.001; partial η2 = 0.25) all decreased the serum resistin levels in the participants (Fig. 3c). The serum adiponectin results showed a significant increase in the HIIT group (F = 51.92, P = 0.001; partial η2 = 0.54). Orlistat (F 1, 43 = 1.51, P = 0.22; partial η2 = 0.03) did not cause a significant change in serum adiponectin. A combination of HIIT and orlistat (F 1, 43 = 23.25, P = 0.001; partial η2 = 0.35) showed an increase in serum adiponectin in the participants (Fig. 3d).
Pre- and post-test IL‑6 (ng/ml; a), TNF‑α (pg/ml; b), resistin (ng/ml; c), and adiponectin (ng/ml; d) in the groups of the present study. Data are expressed as mean ± standard deviation. The participants were 12 in each group. HIIT high-intensity interval training. aHIIT versus control. bOrlistat versus placebo. cCombination of HIIT and orlistat
Variable correlations and post hoc power calculation
The correlations between variables are reported in Table 3. The post hoc power calculation for each variable was > 0.85.
Discussion
The results of this study showed that HIIT decreased body weight, BMI, neck circumference, TNF‑α, and resistin concentration, while increasing aerobic power, IL‑6, and adiponectin concentration. Orlistat decreased BMI, neck circumference, and resistin, while increasing plasma IL‑6 levels. Although the interactive effect between HIIT and orlistat is significant in many factors, there seems to be no synergistic effect, and there is a limit to the improvements that each intervention factor can provide. Regarding the effects of HIIT and orlistat on the factors measured in the present study, certain mechanisms will be discussed below, based on data from previous studies.
It has been shown that there is a close relationship between IL‑6 level and BMI (Khaodhiar, Ling, Blackburn, & Bistrian, 2004). IL‑6 is affected by factors such as glucocorticoids, catecholamines, insulin, and certain cytokines, such as TNF‑α and IL‑1, androgens, and thyroid hormones (Straub, 2014; Vicennati, Vottero, Friedman, & Papanicolaou, 2002). Each of these factors plays an important role in influencing interleukin‑6 levels through exercise training and orlistat consumption. Exercise training causes metabolic changes and, by disrupting the cell’s energy charge, increases the cellular demand for the energy needed for survival (Radak, Zhao, Koltai, Ohno, & Atalay, 2013). In fact, high-intensity interval training and orlistat consumption may cause a negative energy balance and consequently a change in plasma levels of interleukin‑6. Previous studies have shown that weight loss due to exercise training (Freitas et al., 2015) and orlistat consumption (Yesilbursa et al., 2005), with a subsequent decrease in BMI, can alter plasma levels of interleukin‑6. IL‑6 is produced from both adipose and muscle tissue. Muscle tissue is believed to increase IL‑6 production in response to low glycogen content and may blunt the effects on TNF‑α. Based upon blood measurements as opposed to biopsies, it cannot be determined whether IL‑6 concentrations increase due to adipose or muscle changes. The increase in IL‑6 observed may not, in fact, have been detrimental.
Studies have shown that orlistat reduces body weight, BMI, and hip circumference (Davidson et al., 1999; Gokcel et al., 2002), similar to the results of the present study. TNF‑α is one of the pro-inflammatory cytokines, with increased levels associated with inflammatory states in obese individuals. Many studies have emphasized that regular exercise can modulate and modify these risk factors, with some research addressing physical inactivity—apart from being overweight/obese—associated with plasma lipid abnormalities and insulin resistance, and elevated levels of inflammatory markers. Changes in adiponectin concentrations associated with chronic exercise have also been observed in several studies, showing plasma adiponectin to be related to changes in body or fat mass (Bluher et al., 2006; Hsieh & Wang, 2005; Oberbach et al., 2006). It is worth noting that some studies have shown that adiponectin levels changed in the absence of clinically meaningful weight loss and may in fact be related to fitness.
Previous studies have shown that resistin increases inflammation and atherosclerosis (Reilly et al., 2005). Resistin also increases due to obesity and is reduced by exercise training. Kadoglou et al. (Kadoglou et al., 2007) observed that a HIIT program (16 weeks) reduced serum resistin in obese and diabetic participants. Balducci et al. (Balducci et al., 2010) observed that several months of HIIT reduced serum resistin in diabetic and obese participants. Shirvani et al. (Shirvani & Rahmati-Ahmadabad, 2019) suggested that a HIIT program can reduce plasma resistin concentration in rats. It is possible that the anti-inflammatory effect of exercise might be related to the suppression of nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, ERK1/2, and stress-activated protein kinases (SAPK)/JNK activities, as well as to increases in superoxide dismutase 1 (SOD-1) gene expression (Khadir et al., 2015; Shirvani & Rahmati-Ahmadabad, 2019). Studies have shown that orlistat administration decreases TNF‑α and increases adiponectin (Derosa et al., 2010). One year of orlistat treatment was observed to improve lipid profiles, and resistin and insulin-resistance parameters, compared to a control group (Derosa et al., 2012). It has also been suggested that orlistat should be used over a long period of time to have certain beneficial effects, perhaps not affecting certain factors in less than a year (Derosa et al., 2012). However, the present study showed that even a period of orlistat consumption of much less than 1 year had a beneficial effect on plasma resistin reduction.
Given that (despite a decreasing pattern of TNF‑α and increasing pattern of adiponectin) the present study did not show a significant effect in response to orlistat consumption but considering the aforementioned recommendation of usage for longer than 1 year (Derosa et al., 2012), it can be deduced that this drug may be applicable for longer interventions to influence adiponectin and TNF‑α levels. Finally, on the basis of the present study population, it must be re-stated that the findings of this study are applicable for non-exercising, young, obese women.
Conclusion
The present study showed that a HIIT program improved the inflammatory and adipokine markers, as well as body weight, BMI, neck circumference, and aerobic power measured in women with obesity. The use of orlistat medication over the course of 8 weeks had effects on certain markers (BMI, neck circumference, resistin, and IL-6), and had no effects on others (TNF‑α and aerobic power), which may suggest that longer periods of time are required to observe significant effects. The concurrent use of HIIT and orlistat demonstrated no synergistic effect, and there seem to be limits to the levels of change that can be achieved by exercise training or medication alone.
References
Achari, A. E., & Jain, S. K. (2017). Adiponectin, a therapeutic target for obesity, diabetes, and endothelial dysfunction. Int J Mol Sci. https://doi.org/10.3390/ijms18061321.
Alfadhli, E. M., Sandokji, A. A., Zahid, B. N., Makkawi, M. A., Alshenaifi, R. F., Thani, T. S., & Habeeb, H. A. (2017). Neck circumference as a marker of obesity and a predictor of cardiometabolic risk among Saudi subjects. Saudi Med J, 38(12), 1219–1223. https://doi.org/10.15537/smj.2017.12.20926.
Azuma, K., Katsukawa, F., Oguchi, S., Murata, M., Yamazaki, H., Shimada, A., & Saruta, T. (2003). Correlation between serum resistin level and adiposity in obese individuals. Obes Res, 11(8), 997–1001. https://doi.org/10.1038/oby.2003.137.
Balducci, S., Zanuso, S., Nicolucci, A., Fernando, F., Cavallo, S., Cardelli, P., Fallucca, S., Alessi, E., Letizia, C., Jimenez, A., Fallucca, F., & Pugliese, G. (2010). Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss. Nutr Metab Cardiovasc Dis, 20(8), 608–617. https://doi.org/10.1016/j.numecd.2009.04.015.
Bluher, M., Bullen Jr., J. W., Lee., J. H., Kralisch, S., Fasshauer, M., Kloting, N., Niebauer, J., Schon, M. R., Williams, C. J., & Mantzoros, C. S. (2006). Circulating adiponectin and expression of adiponectin receptors in human skeletal muscle: associations with metabolic parameters and insulin resistance and regulation by physical training. J Clin Endocrinol Metab, 91(6), 2310–2316. https://doi.org/10.1210/jc.2005-2556.
Bougoulia, M., Triantos, A., & Koliakos, G. (2006). Effect of weight loss with or without orlistat treatment on adipocytokines, inflammation, and oxidative markers in obese women. Hormones, 5(4), 259–269. https://doi.org/10.14310/horm.2002.11190.
Cohen, S. S., Gammon, M. D., Signorello, L. B., North, K. E., Lange, E. M., Fowke, J. H., Hargreaves, M. K., Cai, Q., Zheng, W., Blot, W. J., & Matthews, C. E. (2011). Serum adiponectin in relation to body mass index and other correlates in black and white women. Ann Epidemiol, 21(2), 86–94. https://doi.org/10.1016/j.annepidem.2010.10.011.
Davidson, M. H., Hauptman, J., DiGirolamo, M., Foreyt, J. P., Halsted, C. H., Heber, D., Heimburger, D. C., Lucas, C. P., Robbins, D. C., Chung, J., & Heymsfield, S. B. (1999). Weight control and risk factor reduction in obese subjects treated for 2 years with orlistat: a randomized controlled trial. JAMA, 281(3), 235–242. https://doi.org/10.1001/jama.281.3.235.
Derosa, G., Cicero, A. F., D’Angelo, A., Fogari, E., & Maffioli, P. (2012). Effects of 1‑year orlistat treatment compared to placebo on insulin resistance parameters in patients with type 2 diabetes. J Clin Pharm Ther, 37(2), 187–195. https://doi.org/10.1111/j.1365-2710.2011.01280.x.
Derosa, G., Maffioli, P., Salvadeo, S. A., Ferrari, I., Gravina, A., Mereu, R., D’Angelo, A., Fogari, E., Palumbo, I., Randazzo, S., & Cicero, A. F. (2010). Comparison of orlistat treatment and placebo in obese type 2 diabetic patients. Expert Opin Pharmacother, 11(12), 1971–1982. https://doi.org/10.1517/14656566.2010.493557.
Freitas, P. D., Ferreira, P. G., da Silva, A., Trecco, S., Stelmach, R., Cukier, A., Carvalho-Pinto, R., Salge, J. M., Fernandes, F. L. A., Mancini, M. C., Martins, M. A., & Carvalho, C. R. F. (2015). The effects of exercise training in a weight loss lifestyle intervention on asthma control, quality of life and psychosocial symptoms in adult obese asthmatics: protocol of a randomized controlled trial. BMC pulmonary medicine, 15, 124–124. https://doi.org/10.1186/s12890-015-0111-2.
Gokcel, A., Gumurdulu, Y., Karakose, H., Ertorer, M. E., Tanaci, N., BascilTutuncu, N., & Guvener, N. (2002). Evaluation of the safety and efficacy of sibutramine, orlistat and metformin in the treatment of obesity. Diabetes Obes Metab, 4(1), 49–55. https://doi.org/10.1046/j.1463-1326.2002.00181.x.
Hannan, A. L., Hing, W., Simas, V., Climstein, M., Coombes, J. S., Jayasinghe, R., Byrnes, J., & Furness, J. (2018). High-intensity interval training versus moderate-intensity continuous training within cardiac rehabilitation: a systematic review and meta-analysis. Open Access J Sports Med, 9, 1–17. https://doi.org/10.2147/oajsm.s150596.
Heck, A. M., Yanovski, J. A., & Calis, K. A. (2000). Orlistat, a new lipase inhibitor for the management of obesity. Pharmacotherapy, 20(3), 270–279. https://doi.org/10.1592/phco.20.4.270.34882.
Hou, T., Tieu, B. C., Ray, S., Recinos Iii, A., Cui, R., Tilton, R. G., & Brasier, A. R. (2008). Roles of IL-6-gp130 signaling in vascular inflammation. Curr Cardiol Rev, 4(3), 179–192. https://doi.org/10.2174/157340308785160570.
Hsieh, C. J., & Wang, P. W. (2005). Effectiveness of weight loss in the elderly with type 2 diabetes mellitus. J Endocrinol Invest, 28(11), 973–977. https://doi.org/10.1007/bf03345334.
Jamaluddin, M. S., Weakley, S. M., Yao, Q., & Chen, C. (2012). Resistin: functional roles and therapeutic considerations for cardiovascular disease. Br J Pharmacol, 165(3), 622–632. https://doi.org/10.1111/j.1476-5381.2011.01369.x.
Kadoglou, N. P., Perrea, D., Iliadis, F., Angelopoulou, N., Liapis, C., & Alevizos, M. (2007). Exercise reduces resistin and inflammatory cytokines in patients with type 2 diabetes. Diabetes Care, 30(3), 719–721. https://doi.org/10.2337/dc06-1149.
Kern, L., Mittenbuhler, M. J., Vesting, A. J., Ostermann, A. L., Wunderlich, C. M., & Wunderlich, F. T. (2018). Obesity-induced TNFalpha and IL‑6 signaling: the missing link between obesity and inflammation-driven liver and colorectal cancers. Cancers. https://doi.org/10.3390/cancers11010024.
Khadir, A., Tiss, A., Abubaker, J., Abu-Farha, M., Al-Khairi, I., Cherian, P., John, J., Kavalakatt, S., Warsame, S., Al-Madhoun, A., Al-Ghimlas, F., Elkum, N., Behbehani, K., Dermime, S., & Dehbi, M. (2015). MAP kinase phosphatase DUSP1 is overexpressed in obese humans and modulated by physical exercise. Am J Physiol Endocrinol Metab, 308(1), E71–83. https://doi.org/10.1152/ajpendo.00577.2013.
Khaodhiar, L., Ling, P. R., Blackburn, G. L., & Bistrian, B. R. (2004). Serum levels of interleukin‑6 and C‑reactive protein correlate with body mass index across the broad range of obesity. Journal of Parenteral and Enteral Nutrition, 28(6), 410–415. https://doi.org/10.1177/0148607104028006410.
Krempf, M., Louvet, J. P., Allanic, H., Miloradovich, T., Joubert, J. M., & Attali, J. R. (2003). Weight reduction and long-term maintenance after 18 months treatment with orlistat for obesity. Int J Obes Relat Metab Disord, 27(5), 591–597. https://doi.org/10.1038/sj.ijo.0802281.
Kyrou, I., Randeva, H. S., Tsigos, C., Kaltsas, G., & Weickert, M. O. (2000). Clinical problems caused by obesity. In K. R. Feingold, B. Anawalt, A. Boyce, G. Chrousos, K. Dungan, A. Grossman, J. M. Hershman, G. Kaltsas, C. Koch, P. Kopp, M. Korbonits, R. McLachlan, J. E. Morley, M. New, L. Perreault, J. Purnell, R. Rebar, F. Singer, D. L. Trence, A. Vinik & D. P. Wilson (Eds.), Endotext. South Dartmouth (MA).
Makki, K., Froguel, P., & Wolowczuk, I. (2013). Adipose tissue in obesity-related inflammation and insulin resistance: cells, cytokines, and chemokines. ISRN Inflamm. https://doi.org/10.1155/2013/139239.
Mancini, M. C., & Halpern, A. (2008). Orlistat in the prevention of diabetes in the obese patient. Vascular health and risk management, 4(2), 325–336. https://doi.org/10.2147/vhrm.s6808.
Murakami, M., Kamimura, D., & Hirano, T. (2019). Pleiotropy and specificity: insights from the Interleukin 6 family of cytokines. Immunity, 50(4), 812–831. https://doi.org/10.1016/j.immuni.2019.03.027.
Nicolò, A., & Girardi, M. (2016). The physiology of interval training: a new target to HIIT. J Physiol, 594(24), 7169–7170. https://doi.org/10.1113/JP273466.
Oberbach, A., Tonjes, A., Kloting, N., Fasshauer, M., Kratzsch, J., Busse, M. W., Paschke, R., Stumvoll, M., & Bluher, M. (2006). Effect of a 4 week physical training program on plasma concentrations of inflammatory markers in patients with abnormal glucose tolerance. Eur J Endocrinol, 154(4), 577–585. https://doi.org/10.1530/eje.1.02127.
Oh, T. J. (2019). The role of anti-obesity medication in prevention of diabetes and its complications. J Obes Metab Syndr, 28(3), 158–166. https://doi.org/10.7570/jomes.2019.28.3.158.
Pei, X., Liu, L., Imam, M. U., Lu, M., Chen, Y., Sun, P., Guo, Y., Xu, Y., Ping, Z., & Fu, X. (2018). Neck circumference may be a valuable tool for screening individuals with obesity: findings from a young Chinese population and a meta-analysis. BMC Public Health, 18(1), 529–529. https://doi.org/10.1186/s12889-018-5448-z.
Radak, Z., Zhao, Z., Koltai, E., Ohno, H., & Atalay, M. (2013). Oxygen consumption and usage during physical exercise: the balance between oxidative stress and ROS-dependent adaptive signaling. Antioxidants & redox signaling, 18(10), 1208–1246. https://doi.org/10.1089/ars.2011.4498.
Rahmati-Ahmadabad, S., Azarbayjani, M. A., Farzanegi, P., & Moradi, L. (2019). High-intensity interval training has a greater effect on reverse cholesterol transport elements compared with moderate-intensity continuous training in obese male rats. Eur J Prev Cardiol. https://doi.org/10.1177/2047487319887828.
Ramírez-Vélez, R., Hernández-Quiñones, P. A., Tordecilla-Sanders, A., Álvarez, C., Ramírez-Campillo, R., Izquierdo, M., Correa-Bautista, J. E., Garcia-Hermoso, A., & Garcia, R. G. (2019). Effectiveness of HIIT compared to moderate continuous training in improving vascular parameters in inactive adults. Lipids in Health and Disease, 18(1), 42–42. https://doi.org/10.1186/s12944-019-0981-z.
Reilly, M. P., Lehrke, M., Wolfe, M. L., Rohatgi, A., Lazar, M. A., & Rader, D. J. (2005). Resistin is an inflammatory marker of atherosclerosis in humans. Circulation, 111(7), 932–939. https://doi.org/10.1161/01.CIR.0000155620.10387.43.
Ruan, H., Hacohen, N., Golub, T. R., Van Parijs, L., & Lodish, H. F. (2002). Tumor necrosis factor-alpha suppresses adipocyte-specific genes and activates expression of preadipocyte genes in 3T3-L1 adipocytes: nuclear factor-kappaB activation by TNF-alpha is obligatory. Diabetes, 51(5), 1319–1336. https://doi.org/10.2337/diabetes.51.5.1319.
Saiga, M., Watanabe, T., & Yoshioka, S. (2013). Physical and mental factors associated with obesity in individuals with mental disorders attending psychiatric day-care facilities. Yonago Acta Med, 56(1), 1–6.
Shi, C., Pang, L., Ji, C., Wang, J., Lin, N., Chen, J., Chen, L., Yang, L., Huang, F., Zhou, Y., Guo, X., Liang, H., & Zhang, M. (2016). Obesityassociated miR148a is regulated by cytokines and adipokines via a transcriptional mechanism. Mol Med Rep, 14(6), 5707–5712. https://doi.org/10.3892/mmr.2016.5940.
Shirvani, H., & Rahmati-Ahmadabad, S. (2019). Irisin interaction with adipose tissue secretions by exercise training and flaxseed oil supplement. Lipids in Health and Disease, 18(1), 15. https://doi.org/10.1186/s12944-019-0960-4.
Sindhu, S., Thomas, R., Shihab, P., Sriraman, D., Behbehani, K., & Ahmad, R. (2015). Obesity is a positive modulator of IL-6R and IL‑6 expression in the subcutaneous adipose tissue: significance for metabolic inflammation. PLoS One, 10(7), e133494. https://doi.org/10.1371/journal.pone.0133494.
Smith, S. R., & Ravussin, E. (2005). Genetic and physiological factors in obesity. J La State Med Soc, 157(Spec No 1), S12–S18.
Stern, J. H., Rutkowski, J. M., & Scherer, P. E. (2016). Adiponectin, leptin, and fatty acids in the maintenance of metabolic homeostasis through adipose tissue crosstalk. Cell Metab, 23(5), 770–784. https://doi.org/10.1016/j.cmet.2016.04.011.
Straub, R. H. (2014). Interaction of the endocrine system with inflammation: a function of energy and volume regulation. Arthritis research & therapy, 16(1), 203–203. https://doi.org/10.1186/ar4484.
Sumithran, P., & Proietto, J. (2014). Benefit-risk assessment of orlistat in the treatment of obesity. Drug Saf, 37(8), 597–608. https://doi.org/10.1007/s40264-014-0210-7.
Vicennati, V., Vottero, A., Friedman, C., & Papanicolaou, D. A. (2002). Hormonal regulation of interleukin‑6 production in human adipocytes. Int J Obes Relat Metab Disord, 26(7), 905–911. https://doi.org/10.1038/sj.ijo.0802035.
Wang, Q., Xu, L., Li, J., Sun, L., Qin, W., Ding, G., Zhu, J., Zhang, J., Yu, Z., & Xie, S. (2018). Association of anthropometric indices of obesity with hypertension in Chinese elderly: an analysis of age and gender differences. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph15040801.
Yesilbursa, D., Serdar, A., Heper, Y., Sarac, M., Coskun, S., Kazazoglu, A. R., & Cordan, J. (2005). The effect of orlistat-induced weight loss on interleukin‑6 and C‑reactive protein levels in obese subjects. Acta Cardiol, 60(3), 265–269. https://doi.org/10.2143/ac.60.3.2005002.
Zhang, J., Guo, Q., Peng, L., Li, J., Gao, Y., Yan, B., Fang, B., & Wang, G. (2018). The association of neck circumference with incident congestive heart failure and coronary heart disease mortality in a community-based population with or without sleep-disordered breathing. BMC Cardiovasc Disord, 18(1), 108. https://doi.org/10.1186/s12872-018-0846-9.
Zhang, Y., Gu, Y. A., Wang, N., Zhao, Q., Ng, N., Wang, R., Zhou, X., Jiang, Y., Wang, W., & Zhao, G. (2019). Association between anthropometric indicators of obesity and cardiovascular risk factors among adults in Shanghai, China. BMC Public Health, 19(1), 1035. https://doi.org/10.1186/s12889-019-7366-0.
Zhao, C. W., Gao, Y. H., Song, W. X., Liu, B., Ding, L., Dong, N., & Qi, X. (2019). An update on the emerging role of resistin on the pathogenesis of osteoarthritis. Mediators Inflamm. https://doi.org/10.1155/2019/1532164.
Acknowledgements
The authors would like to thank all study participants.
Funding
Central Tehran Branch, Islamic Azad University.
Author information
Authors and Affiliations
Contributions
MAA designed the study. MA, MAA, FZ, and BGH participated in the acquisition of data. SRA analyzed the data. SRA wrote the first draft and revised the manuscript critically. All authors approved the final version of the manuscript to be published, and they are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
M. Aghajani, S. Rahmati-Ahmadabad, F. Zamani, B. Ghanbari, and M.-A. Azarbayjani declare that they have no competing interests.
The research ethics committee of the Medical University, Alborz, Iran, approved the experimental protocol of the study (ethical code: 1390.40). This study was registered at Islamic Azad University, Central Tehran Branch, Iran (registration number: 10121423972005). This research was conducted in accordance with the principles stated in the Declaration of Helsinki. The statistical population of this study comprised volunteer obese women in Tehran, who were aged 18–23 years and presented a BMI above 30 kg/m2. Before participating in the investigation, the participants were informed about the study and each participant signed an institutionally approved informed consent document.
Rights and permissions
About this article
Cite this article
Aghajani, M., Rahmati-Ahmadabad, S., Zamani, F. et al. The effects of high-intensity interval training and orlistat on selected adipokines and cytokines in obese women. Ger J Exerc Sport Res 52, 87–96 (2022). https://doi.org/10.1007/s12662-021-00749-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12662-021-00749-z