Abstract
Purpose
This narrative review examines the current evidence on whether obstructive sleep apnea (OSA) is associated with postoperative delirium (POD) and postoperative cognitive dysfunction (POCD). The mechanisms that could predispose OSA patients to these disorders are also explored.
Source
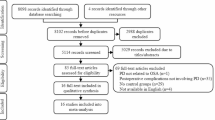
Relevant literature was identified by searching for pertinent terms in Medline®, Pubmed, ScopusTM, and Google scholar databases. Case reports, abstracts, review articles, original research articles, and meta-analyses were reviewed. The bibliographies of retrieved sources were also searched to identify relevant papers.
Principal findings
Seven studies have investigated the association between OSA and POD, with mixed results. No studies have examined the potential link between OSA and POCD. If these relationships exist, they could be mediated by several mechanisms, including increased neuroinflammation, blood–brain barrier breakdown, cerebrovascular disease, Alzheimer’s disease neuropathology, disrupted cerebral autoregulation, sleep disruption, sympathovagal imbalance, and/or disrupted brain bioenergetics.
Conclusion
There is very limited evidence that OSA plays a role in postoperative neurocognitive disorders because few studies have been conducted in the perioperative setting. Additional perioperative prospective observational cohort studies and randomized controlled trials of sleep apnea treatment are needed. These investigations should also assess potential underlying mechanisms that could predispose patients with OSA to postoperative neurocognitive disorders. This review highlights the need for more research to improve postoperative neurocognitive outcomes for patients with OSA.
Résumé
Objectif
Ce compte rendu narratif examine les données probantes actuelles quant à l’association entre l’apnée obstructive du sommeil (AOS) et le syndrome confusionnel postopératoire (SCPO) ainsi que le dysfonctionnement cognitif postopératoire (DCPO). Les mécanismes qui pourraient prédisposer les patients atteints d’AOS à ces troubles sont également explorés.
Sources
La littérature concordante a été identifiée en recherchant des termes pertinents dans les bases de données Medline®, Pubmed, ScopusTM et Google Scholar. Les présentations de cas, résumés, articles de synthèse, articles de recherche originaux et méta-analyses ont été examinés. Les bibliographies des sources récupérées ont également été recherchées pour identifier les articles pertinents.
Constatations principales
Sept études ont examiné l’association entre l’AOS et le SCPO, avec des résultats mitigés. Aucune étude n’a exploré le lien potentiel entre l’AOS et le DCPO. Si ces relations existent, elles pourraient être médiées par plusieurs mécanismes, notamment une neuroinflammation accrue, une dégradation de la barrière hémato-encéphalique, une maladie cérébrovasculaire, une neuropathologie de la maladie d’Alzheimer, une autorégulation cérébrale perturbée, une perturbation du sommeil, un déséquilibre sympathovagal et / ou une bioénergétique cérébrale perturbée.
Conclusion
Il existe très peu de données probantes soutenant que l’AOS joue un rôle dans les troubles neurocognitifs postopératoires parce que peu d’études ont été menées dans le contexte périopératoire. D’autres études de cohorte observationnelles prospectives périopératoires et des études randomisées contrôlées sur le traitement de l’apnée du sommeil sont nécessaires. Ces études devraient également évaluer les mécanismes sous-jacents potentiels qui pourraient prédisposer les patients atteints d’AOS à des troubles neurocognitifs postopératoires. Ce compte rendu souligne la nécessité de recherches supplémentaires pour améliorer les devenirs neurocognitifs postopératoires des patients atteints d’AOS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Worldwide, up to 40% of older adults who undergo surgery every year will experience perioperative neurocognitive disorders such as delirium and postoperative cognitive dysfunction (POCD). Postoperative delirium (POD) is characterized by acute deficits in attention, altered level of consciousness, and disorganized thinking, which typically occur within the first few days after surgery.1 Postoperative cognitive dysfunction is a syndrome of objectively measurable cognitive deficits that occur 1–12 months after anesthesia and surgery.2 The timing of cognitive testing and the magnitude of cognitive deficits that define POCD are heterogeneous; therefore, a new standardized nomenclature for perioperative neurocognitive disorders has recently been created.3 Postoperative neurocognitive disorders (NCD) refers to objectively measured cognitive decline from before surgery to 1–12 months after surgery accompanied by subjective complaints of cognitive deficits that disrupt instrumental activities of daily living. In this review, we will use the term POCD when referring to individual studies that measured only objective cognitive deficits, many of which were conducted before this new nomenclature was published.
Some studies suggest that POD and POCD have a similar pathogenesis,4 despite differences in their presentation. Indeed, POD and POCD share many known risk factors such as increased age, pre-existing dementia or cognitive impairment, multiple comorbidities, and longer surgery. Nevertheless, much remains unknown about specific comorbidities and/or mechanisms that underpin POD and POCD. Further research is needed to identify specific disorders that increase the risk for cognitive impairment after anesthesia and surgery, particularly because some comorbidities could be optimized before surgery. One comorbidity that could increase the risk for POD and POCD is obstructive sleep apnea (OSA), a disorder that is highly prevalent in older surgical patients and often is undiagnosed and untreated. Here, we summarize studies evaluating the relationship between OSA and increased risk for POD and POCD. We also discuss potential mechanisms that could mediate an increased risk for POD and POCD in patients with OSA.
Search strategy
To conduct this narrative review, we searched for relevant terms in Medline®, Pubmed, Scopus™, and Google scholar databases between 14 December 2018 and 28 January 2022. Case reports, abstracts, review articles, original research articles, and meta-analyses were reviewed. The bibliographies of retrieved sources were also searched to identify relevant papers. We also included relevant articles found during manuscript writing after the search. In particular, our search focused on identifying studies assessing the link between sleep apnea and POD and cognitive dysfunction. Further attention was given to the pathophysiology of cognitive impairment in OSA patients. The scale for the quality assessment of narrative review articles was followed when preparing this manuscript.5
Obstructive sleep apnea: definition, treatment, and relevance in the perioperative period
Obstructive sleep apnea is a syndrome of repetitive breathing cessations during sleep that are caused by airway obstruction. Obstructive sleep apnea is diagnosed by measuring these breathing interruptions, which are classified as apneas (a complete cessation of breathing associated with oxygen desaturation) or hypopneas (inadequate breathing associated with oxygen desaturation). Obstructive sleep apnea is the most common form of sleep-disordered breathing (SDB) and is a highly prevalent disorder with substantial public health impact. It is estimated that nearly 20% of the adult North American population have OSA, and at least 70% of adults with OSA remain undiagnosed.6 The prevalence of OSA is even higher in older adults, with estimates of about 50% in those over 60 years of age.6
Treatment of OSA typically involves a continuous positive airway pressure (CPAP) device, which delivers titrated positive airway pressure to keep the upper airway patent during inspiratory efforts.7 Although CPAP treatment is effective, results as to whether it decreases OSA complications such as hypertension, cardiovascular disease, and dementia are conflicting. This is because it is challenging to adhere to CPAP because of patient discomfort and cultural and socioeconomic barriers.8 Thus, research has focused on new therapies for OSA, including oral appliances, palatopharyngeal surgery, and hypoglossal nerve stimulation.9
Patients with OSA have an increased risk of intraoperative and postoperative complications, including a 3–4-fold increased risk of difficult intubation and mask ventilation, and an increased incidence of postoperative respiratory failure, adult respiratory distress syndrome, cardiac arrest, atrial fibrillation, and delirium.10 Because OSA has been associated with increased perioperative complications, OSA risk assessment tools such STOP-BANG have been used to identify patients at risk for undiagnosed OSA. STOP-BANG is a validated 8-point screening questionnaire that assesses snoring, tiredness, observed apneas, high blood pressure, body mass index (BMI), age, increased neck circumference, and male gender, and indicates patients with a higher risk for OSA and increased postoperative complications.11 Once identified, these patients should be managed perioperatively with careful airway management, optimization of comorbid conditions, and increased postoperative respiratory monitoring.12
Obstructive sleep apnea and cognitive sequelae
Growing evidence suggests that OSA is associated with neurocognitive sequelae outside of surgery in older adults, including depression,13 Alzheimer’s disease (AD), and dementia.14 Indeed, older adults with OSA have increased AD neuropathology, as measured by decreased amyloid beta in the cerebrospinal fluid (CSF)15 and increased amyloid deposition on positron emission tomography (PET) images of the brain.16 Since disrupted sleep disturbs the balance of amyloid beta production and clearance,17 these data raise the possibility that OSA-related sleep disruptions drive increased AD neuropathology in OSA patients. Further, these patients might also have a higher likelihood of developing vascular dementia.18 Indeed, magnetic resonance imaging has identified neurologic damage in both white and gray matter in OSA patients.19 Further study is needed to determine the extent to which OSA comorbidities, such as obesity, diabetes, and hypertension, contribute to the link between OSA and depression, dementia, and AD. Animal models of OSA also exhibit neurodegeneration mediated by inflammation, hypoxia, sleep fragmentation, metabolic disruption, and decreased amyloid beta clearance, which suggests that OSA plays a causal role in neurocognitive decline.20 Indeed, randomized controlled trials of CPAP in OSA patients have shown improvement in attention, working memory, and executive function, particularly in patients with severe OSA who also suffer from severe excessive daytime somnolence.21
Although these recent studies suggest that OSA is independently associated with cognitive disorders outside of surgery, it remains an open question to what extent OSA is associated with postoperative neurocognitive disorders such as POD and POCD. By increasing brain vulnerability through various mechanisms, OSA could impact cognitive recovery following insults. For example, stroke patients with OSA have poorer recovery of neurologic function than stroke patients without OSA.22
Obstructive sleep apnea and postoperative delirium
Although POD and POCD are both common postoperative neurocognitive disorders, they differ in key ways. First, POD is typically diagnosed in the initial postoperative period (24–72 hours after surgery) with delirium assessment tools that operationalize the criteria for delirium in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). In contrast, POCD is not defined in the DSM-5, so patients must undergo in-depth neuropsychological testing of memory, attention, and executive and visuospatial function before and 1–12 months after surgery.2 The incidence of POCD varies depending on the time of postoperative assessment, and decreases from 65% at hospital discharge to 40% a few months later in cardiac surgery patients.23 Similar to POD, POCD is associated with decreased quality of life,24 increased mortality,25 and, potentially, increased risk for dementia.26
Although POD and POCD are measured using different tools and are defined in different time frames during the postoperative period, they share some of the same risk factors, and may in fact represent a spectrum of postoperative brain dysfunction. Among these shared risk factors are older age, depression, and baseline cognitive impairment.27 The pathogenesis of POD and POCD is not fully understood, and is likely multifactorial. Studying the medical disorders that make certain patients susceptible to postoperative cognitive changes provides an opportunity to understand the pathogenesis of POD and POCD. One possible risk factor for POCD is OSA, which is associated with earlier onset of dementia and cognitive decline outside of surgery.
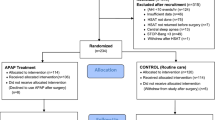
In OSA patients, anesthesia and surgery may constitute a “second hit” that leads to POD and POCD. Our search yielded seven studies that have attempted to determine whether SDB is a risk factor for POD (Table 1). Gupta et al. conducted a retrospective case–control study that considered a range of postoperative complications, including POD, in OSA patients undergoing elective hip or knee replacement.28 The authors reported an insignificant trend toward higher POD incidence, as noted by caregivers, in patients with confirmed OSA (P = 0.07). Nevertheless, given the lack of systematic delirium screening of the study participants and the retrospective nature of the study design, the incidence of delirium in both the OSA group and the control group was likely significantly underestimated.
In a prospective cohort study, the incidence of POD in OSA patients undergoing elective knee replacement was 53% (compared with 21% in patients without OSA).29 Participants without pre-existing dementia or baseline delirium were assessed for POD on postoperative days 2 and 3, according to DSM-IV criteria. Their data showed that OSA is a statistically significant independent predictor of POD after controlling for covariates that included comorbidities and BMI. In another prospective study, Roggenbach et al. measured delirium incidence using the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) screening tool in patients undergoing cardiac surgery.30 They found that a preoperative apnea-hypopnea index (AHI) value ≥ 19 is associated with POD (odds ratio [OR], 6.4; P ≤ 0.001).
More recently, Chan et al. examined the association between OSA and postoperative cardiovascular events in patients undergoing non-cardiac surgery, and also assessed POD as a secondary outcome.31 Patients underwent home sleep apnea testing up to one month before surgery, and POD was assessed the morning after surgery using the confusion assessment method. Only 4.5% of patients met those criteria for delirium, likely due to under-detection because of the low frequency of delirium assessments, which are typically administered twice daily for several days postoperatively. Another contributor to the low incidence of POD in this study is that nearly 40% of the patient cohort were younger than 65 and thus, at lower risk for POD. The authors found that patients who tested positive for OSA did not have significantly higher delirium rates in either adjusted or unadjusted analyses. Given this low rate of delirium, infrequent delirium assessments, and lack of power analysis for the secondary outcome, it is likely that this study lacked sufficient power to assess the relationship between OSA and POD.
Although STOP-BANG is limited by poor specificity for sleep apnea, two studies have investigated the relationship between STOP-BANG scores and POD. In a secondary analysis of a prospective trial, Wang et al. showed that thoracic patients with a STOP-BANG score ≥ 3 had higher incidence and duration of delirium and/or coma.32 In another study, Strutz et al. used STOP-BANG to stratify 1,441 older surgery patients into groups of low (score 0–2), intermediate (score 3–4) and high (score 5–8) risk for OSA. In unadjusted analyses, patients at high risk for OSA had a significantly higher incidence of POD than patients at low risk did (OR, 1.77; 95% confidence interval, 1.22 to 2.57; P = 0.003). After adjusting for age, sex, BMI, surgery type, alcohol use, comorbidities (i.e., hypertension, chronic obstructive pulmonary disease, asthma, stroke, dementia, depression, sensory impairment, and diabetes), and self-reported sleepiness, they found no independent association between OSA and POD.33 It must be considered that this analysis could have adjusted out potential mediators of delirium in OSA, especially considering that BMI, sleepiness, hypertension, and depression are tightly associated with OSA. In other words, the statistical adjustment for the STOP-BANG factors sleepiness, hypertension, and elevated BMI might have resulted in selecting patients resistant to the downstream effects of OSA. Thus, additional POD studies employing rigorous sleep apnea testing and measurement of covariates are needed to disentangle the complex inter-relationships between OSA, OSA risk factors, OSA downstream effects, and POD.
Obstructive sleep apnea and postoperative cognitive dysfunction
There is a paucity of data on the relationship between OSA and POCD. In fact, we only found one study that examined this link.34 Surprisingly, this study by Wagner et al. found that those at high risk for OSA, based on their STOP-BANG score, had a statistically significant improvement in memory postoperatively. Nevertheless, the neuropsychological test battery used to detect POCD was administered within the first two postoperative days in the acute postoperative period, during which several factors confound assessment of postoperative cognitive function. These factors include postoperative pain, opioid use, sleep disturbances, and nutritional deficiencies, in addition to the emotional stress of surgery and hospitalization. For this reason, there is general consensus that POCD cannot ideally be detected up to 30 days postoperatively or until discharge (if < 30 days).2 Thus, we cannot conclude that patients at high risk for OSA have postoperative cognitive improvement based on the study by Wagner et al.
Role of perioperative obstructive sleep apnea treatment in preventing postoperative delirium and postoperative cognitive dysfunction
Evidence that CPAP treatment for OSA improves gray matter volume in the hippocampus and frontal lobe, as well as cognition, raises the question of whether POD and POCD could be prevented by initiating CPAP preoperatively.35 A secondary aim of the abovementioned study by Strutz et al., was to compare the POD incidence in patients with a previous diagnosis of OSA who were compliant with treatment with the POD incidence in those who were not compliant.33 They found that OSA treatment did not protect against POD; however, CPAP was self-reported, and likely overestimated the actual compliance rate. In a small randomized trial, patients at high risk for OSA (STOP-BANG ≥ 3) were randomly assigned to an auto-titrating CPAP or routine care at the preoperative clinic.36 Although CPAP therapy was not associated with reduced POD incidence or severity, the authors reported poor use of the auto-titrating CPAP. Another problem is that several months of CPAP is typically required before beneficial cognitive effects in non-surgical patients are appreciated.35 In the abovementioned randomized trial, patients were initiated on CPAP only days to weeks before surgery. Of note, perioperative CPAP treatment has not been shown to alleviate many other postoperative complications with established links to OSA, potentially because of issues with CPAP adherence and a short duration of implementation before surgery.37 Thus, future studies are needed to determine whether weeks to months of adherent CPAP treatment reduces POD and/or POCD incidence and severity.
Obstructive sleep apnea, postoperative delirium, and postoperative cognitive dysfunction: important future research
More prospective studies are needed to study the extent to which OSA is associated with POD and/or POCD and whether perioperative treatment of OSA prevents these disorders. We have detailed these important future research questions in Table 2. Studies addressing these questions should employ sleep apnea testing to rigorously diagnose sleep apnea and quantify its severity as well as measures of oxygenation. Delirium should be assessed at least twice daily using a tool suitable for the study population (ward vs ICU) that also measures delirium severity. For POCD assessment, cognitive testing should be performed preoperatively and at least 30 days after surgery. To help identify patients most likely to benefit from preoperative urgent evaluation and treatment of OSA, patient factors such as comorbidities (i.e., hypertension, diabetes, etc.), excessive daytime somnolence, and frailty should be carefully assessed preoperatively. In addition to improving our understanding of the relationship between OSA and POD and/or POCD, these studies could also shed insight into mechanisms underlying cognitive dysfunction in OSA patients outside of surgery (Figure 1).
Potential mechanisms underlying perioperative neurocognitive disorders in patients with obstructive sleep apnea. Summary of potential mechanisms that could increase susceptibility to postoperative delirium and cognitive dysfunction in obstructive sleep apnea patients. Intermittent upper airway obstruction and resulting apneas cause intermittent hypoxia that evokes potential downstream mechanisms. These mechanisms include A) Blood-brain barrier (BBB) breakdown and Neuroinflammation, including increased brain inflammatory mediators such as tumor necrosis factor (TNF), interleukin- (IL-1), interleukin-8 (IL-8), and monocyte chemoattractant protein-1 (MCP-1); B) Cerebrovascular Disease, which includes increased cerebral small vessel disease and postoperative covert stroke risk; C) Alzheimer’s disease neuropathology, which includes increased brain deposition of amyloid beta (Aβ) and formation of neurofibrillary tau tangles; D) Altered Cerebral Autoregulation, comprising a right shift in the autoregulation curve that increases risk for cerebral hypoperfusion during periods of hypotension; E) Sleep Disruption, characterized by decreased deeper stages (stages 3 and 4) of non-rapid eye movement (NREM) and decreased rapid eye movement (REM) sleep; F) Sympathovagal Imbalance characterized by predominance of the sympathetic nervous system activity shown here; G) Disrupted Brain Bioenergetics, including decreased adenosine triphosphate (ATP) production due to mitochondrial damage from intermittent hypoxia.
Potential mechanisms linking obstructive sleep apnea to cognitive impairment, postoperative delirium, and postoperative cognitive dysfunction
Because OSA is characterized by periods of intermittent hypoxia that disrupt normal sleep, many downstream sequelae due to chronic intermittent hypoxia occur.38 These downstream mechanisms are discussed below and include increased neuroinflammation, blood–brain barrier (BBB) breakdown, cerebrovascular disease, increased AD neuropathology, altered cerebral autoregulation, sleep disruptions, disrupted brain bioenergetics, and sympathovagal imbalance. While these consequences of hypoxia and sleep disruptions from OSA may be subclinical preoperatively, they could become unmasked following a “second-hit” insult from surgery, anesthesia, and postoperative complications. We review evidence of these mechanisms in sleep apnea animal models and human studies, and discuss evidence that these mechanisms contribute to POD and/or POCD.
Neuroinflammation (Figure panel A)
Several lines of evidence suggest that OSA patients experience neuroinflammation. First, neuroinflammation is prominently found in animal models of OSA. These models involve exposing animals to chronic intermittent hypoxia, since most non-human mammals do not exhibit obstructive apneas.39 Exposure to chronic intermittent hypoxia evokes neuroinflammation,40 hippocampal and frontoparietal cortical apoptosis,41 and decreased neuroplasticity.42 Despite these findings in animal models, few studies have been able to assess neuroinflammation in patients with OSA. Nevertheless, many studies have shown that OSA patients exhibit increased peripheral markers of inflammation, including c-reactive protein, interleukin (IL)-6, IL-8, and vascular cell adhesion molecule (VCAM)-1, which are reduced with CPAP therapy.43 Although no human studies have determined whether these peripheral inflammatory mediators cross the BBB to cause neuroinflammation, neuroimaging studies have shown that OSA patients have increased white matter hyperintensities and gray matter losses.44 Particular regions affected include hippocampal, parahippocampal, and other temporal and cerebellar regions, which are particularly sensitive to injury from hypoxia.45 Similarly, chronic intermittent hypoxia in animal models evokes neurodegeneration in the cortex, hippocampus, and motor nuclei, and has detrimental effects on cognitive function, memory, and motor ability.46
Recently, the role of microglial activation in response to chronic intermittent hypoxia has become an area of particular interest. Microglia are resident phagocytes within the brain, and are the primary innate immune response mediators in the central nervous system (CNS).47 Microglial functions include cytotoxic and inflammatory responses to infection, removal of neural plaques and damaged synapses,48 recruitment of neural and glial cells for CNS growth and repair,49 and extracellular signaling via cytokine release.50 Recently, rodent model studies have shown a variety of mechanisms by which hypoxia activates CNS microglia, including toll-like receptor activation, reactive oxygen species generation, peripheral cytokine release, and epigenetic modifications.51 The effects and duration of microglial activation appear to differ by CNS region because of the heterogeneity of microglial populations, although in general, hypoxia shifts the microglial balance toward the M1 proinflammatory phenotype, with increased expression of inflammatory cyclooxygenase-2-derived products, tumor necrosis factor alpha (TNFα), IL-1β, and IL-6.40,51 Together, these studies suggest that microglia are key cellular mediators of chronic intermittent hypoxia-driven neuroinflammation.
Although most studies that measure the effects of OSA and intermittent hypoxia on the brain focus on cognitive performance and markers of CNS inflammation, changes in brain architecture have also been visualized by magnetic resonance imaging (MRI). While cerebral damage secondary to OSA is not obvious from routine MRI, comparison studies between OSA patients and matched controls have revealed patterns of anatomic change associated with OSA. The hallmark structural abnormality in patients with OSA appears to be decreased hippocampal volume. Similar hippocampal atrophy occurs in patients without OSA who have suffered carbon monoxide poisoning or who have been exposed to prolonged periods at high altitude, further supporting the hypothesis that hippocampal injury is a result of hypoxia.52 These losses in hippocampal volume have been associated with impaired learning and memory in OSA patients, suggesting that chronic intermittent hypoxia may be a primary mediator of OSA-associated cognitive dysfunction. Further, at least one study has shown that CPAP reverses hippocampal atrophy, verifying its consequential relationship to sleep apnea.53 Other anatomic changes due to sleep apnea have not been as clearly defined. Some studies have found diffuse decreases in gray matter volume in other cortical regions,54 while others have reported no other anatomic differences. Such discrepancies are likely due to a combination of different analysis methods and aging-related patient variability.55
In addition to hippocampal and cortical degeneration, several studies have found evidence of white matter changes in patients with OSA. Macey et al. reported extensive axonal injury in a variety of white matter tracts, including those associated with the limbic system, which they hypothesize may contribute to the increased rates of depression and mood disorders in patients with OSA.56 Given the tight correlation between depressive symptoms and cognitive impairment, these limbic system abnormalities could contribute to cognitive impairment as well as depression. Other groups have found evidence of increased white matter hyperintensities on MRI scans in patients with OSA, suggesting subcortical axonal or glial injury.57 Correlating the effects of these lesions with clinical findings is an emerging area of research, and the role of these lesions in predisposition to POCD and POD is unclear. Further studies are needed to determine whether neuroinflammation and white and gray matter damage are associated with POCD and/or POD in OSA patients.
Blood–brain barrier breakdown (Figure, panel A)
The vascular BBB consists of tight junctions between brain endothelial cells, which prevent plasma components, blood cells, and pathogens from entering the brain. Thus, the brain milieu is tightly controlled via regulated transport of large molecules and cells through the BBB. Disrupted BBB function can result in leakage of plasma molecules and blood cells into the brain, as well as altered transport and clearance of molecules, resulting in neurotoxicity. In OSA patients, the BBB could be compromised for several reasons. First, peripheral inflammatory cytokines, such as TNFα and IL-1β, can actually weaken the integrity of brain endothelial tight junctions, thereby compromising the BBB.58 Second, hypoxia-triggered neuroinflammation may also result in free radical-mediated damage to the BBB endothelium.59 Third, hypoxia upregulates vascular endothelial growth factor,60 which alters the expression of tight junction proteins.59 Even without hypoxia, interrupted sleep in mice increases extravasation of Evans Blue dye into the brain, which is reversed after allowing for uninterrupted sleep.61 These findings from OSA animal models suggest that BBB breakdown is one feature of OSA that could contribute to POCD and/or POD.
Despite evidence from animal models that OSA could cause BBB breakdown, whether OSA patients experience BBB breakdown is not conclusive. Several studies, however, have suggested that BBB breakdown does occur in patients with OSA. First, isolated plasma exomes from pediatric OSA patients evoked BBB breakdown in an in vitro model of brain endothelium.62 Second, older OSA patients had increased brain parenchymal water,63 indicating increased unregulated BBB leakage. This evidence, along with findings that OSA patients have increased white matter hyperintensities (discussed above), suggest that BBB breakdown plays a role in increased incidence of mild cognitive impairment, dementia, and AD in OSA patients.64
Indeed, BBB breakdown in OSA patients could increase the predisposition to POD and POCD, especially considering that BBB breakdown has been associated with postoperative cognitive deficits in human and animal studies. For example, in rodent POCD models, surgery and anesthesia disrupt the BBB,65 and this BBB breakdown is necessary for the development of postoperative cognitive deficits.66 In humans, BBB breakdown occurs after cardiac surgery, as shown by an elevated CSF-to-plasma ratio of albumin and brain MRI contrast enhancement, and the extent of this BBB breakdown is associated with the degree of POCD.67 Further studies are needed to determine whether BBB breakdown occurs after other types of surgery and to determine whether BBB breakdown is associated with POD and POCD in these surgical populations. Finally, we do not yet know whether specific comorbidities such as OSA or perioperative sleep deprivation increase BBB breakdown and risk for POCD and POD, or whether specific perioperative interventions or anesthetic techniques could decrease postoperative BBB breakdown.
Cerebrovascular disease (Figure, panel B)
Older OSA patients have an increased risk of stroke, even after adjusting for the comorbid stroke risk factors hypertension, atrial fibrillation, and heart failure.68 Several mechanisms are thought to underlie this increased risk.69 First, intermittent hypoxemia causes endothelial damage through increased oxidative stress, which activates platelet aggregation and promotes atherosclerosis to increase the risk of ischemic stroke. Second, OSA exacerbates cardiac arrhythmias, most commonly atrial fibrillation, which increases risk of cardioembolic stroke. Third, altered cerebral autoregulation (covered below) increases the risk for watershed stroke during periods of hypotension. These mechanisms also likely contribute to greater cerebral small vessel disease burden in OSA patients,70 which has been theorized to increase cognitive dysfunction and vascular dementia in OSA patients.71 Taken together, these findings suggest that OSA patients have significant cerebrovascular disease that increases their risk of stroke and cerebral small vessel disease outside of surgery.
Because perioperative stroke is a rare event occurring in less than 1% of older non-cardiac surgery patients,72 no studies have thoroughly investigated whether OSA is associated with perioperative stroke. Nevertheless, one recent study found that severe OSA in non-cardiac surgery patients is associated with increased cardiovascular events, defined as a composite outcome that included stroke.31 In another study, acute cerebral ischemic events that are not clinically apparent and termed “covert strokes” were found in 10% of older non-cardiac surgical patients.73 Because patients in this study were not tested for OSA, it is unknown whether covert strokes occurred more frequently in OSA patients. Nevertheless, covert strokes were associated with a two-fold increased risk of POD and as well as an increased risk for decreased global cognition one year after surgery.74 Altogether, these findings raise the question of whether OSA patients have a greater risk of perioperative covert strokes and whether this increased cerebrovascular disease underlies POD and/or POCD in OSA patients. Additional studies are needed to determine whether cerebrovascular dysfunction increases risk for POD and POCD in OSA patients.
Alzheimer’s disease neuropathology (Figure, panel C)
Obstructive sleep apnea is associated with an increased risk for developing mild cognitive impairment and dementia, including AD dementia. A recent meta-analysis that included 18 longitudinal studies found that patients who reported sleep disturbances had a higher risk for incident all-cause dementia, and in subgroup analyses, OSA was associated with all-cause dementia and AD dementia.75 Further, patients with moderate to severe OSA have increased AD neuropathology, including elevated CSF tau, decreased CSF amyloid beta,15 and increased deposition of amyloid beta in the brain as measured by Pittsburgh Compound B PET imaging.16 In addition, AD patients with untreated OSA exhibited faster progression of AD dementia and worse cognitive function. This accelerated AD neuropathology and cognitive decline might primarily be due to sleep disruptions in OSA patients because disruptions in non-rapid eye movement (NREM) and slow-wave sleep increase amyloid-β aggregation.76 Additionally, CSF amyloid-β and tau levels in AD patients correlate with decreased slow-wave sleep time, rapid eye movement (REM) sleep, and sleep efficiency.76 Together, these studies suggest that OSA is a risk factor for developing AD and raise the question whether increased perioperative AD neuropathology could increase the degree of POD and POCD in OSA patients.
To better understand the potential role of increased AD neuropathology in POD and POCD in OSA patients, we need to consider what is known about the relationship between AD neuropathology and POD and POCD. Animal studies have shown that increased amyloid deposition occurs following anesthesia and surgery,77 and retrospective studies have found increased postoperative AD neuropathology in patients with POCD. Nevertheless, our recent prospective study of 140 non-cardiac surgery patients showed that postoperative changes in CSF amyloid, tau, or phosphorylated tau are not associated with POCD or POD.78 Thus, while pre-existing AD dementia is a clear risk factor for POD and POCD, postoperative increases in AD neuropathology are not associated with POD or POCD. Additionally, the extent to which preoperative AD neuropathology without dementia increases the risk for POD and POCD is not fully understood. While older hip arthroplasty patients with a lower CSF amyloid beta/tau ratio79 and lower CSF amyloid beta80 are more likely to develop POD, CSF amyloid beta and tau could not predict POD risk in hip fracture patients.81 One possible explanation here is that POD and POCD risk depends on the interaction between precipitating factors and susceptibility factors. Indeed, AD neuropathology increases susceptibility to insults like neuroinflammation.82 These results, taken in context, suggest that pre-existing AD neuropathology could increase the risk for POD and POCD depending on the operative insult. Further studies are needed to confirm this and to determine whether AD neuropathology alone increases risk for these disorders in OSA patients.
Altered cerebral autoregulation (Figure, panel D)
Another possible contributor to the elevated risk for POCD and POD in OSA patients is changes in cerebral blood flow secondary to altered cerebral autoregulation. Cerebral autoregulation maintains normal cerebral blood flow during periods of hypotension and hypertension via regional cerebral arteriolar vasodilation or vasoconstriction, respectively (Figure 1). Below the lower limit of cerebral autoregulation, cerebral blood flow decreases with further reductions in cerebral perfusion pressure. Similarly, hypertension can overwhelm autoregulatory vasoconstriction and can increase cerebral blood flow. Obstructive sleep apnea patients display severely attenuated vasodilatory responses, resulting in decreased cerebral blood flow at lower blood pressure thresholds. The end result is that OSA patients are at risk for decreased cerebral perfusion during hypotension, which can impair tissue oxygenation and worsen metabolic dysfunction. Disrupted cerebral autoregulation in OSA patients can be reversed with CPAP treatment, suggesting it develops independent of comorbid chronic vascular disease in OSA patients.83
Since brief periods of hypotension frequently occur during surgery,84 impaired cerebral autoregulation could place OSA patients at risk for decreased intraoperative cerebral perfusion and subsequent POCD and POD. Indeed, maintaining mean arterial pressure above the lower limit of cerebral autoregulation decreases the odds for delirium after cardiac surgery.85 These results suggest that disrupted cerebral perfusion due to altered cerebral autoregulation and hypotension contributes to POD and perhaps even POCD. Nevertheless, no studies have shown that altered cerebral autoregulation specific to OSA patients results in impaired cerebral perfusion perioperatively or is associated with POD or POCD. Further studies are needed to clarify the role of altered cerebral autoregulation in perioperative neurocognitive disorders in OSA patients. If altered cerebral autoregulation is found to put OSA patients at risk for impaired cerebral perfusion, future studies could inform guidelines for maintaining cerebral perfusion in OSA patients to prevent the development of POD and/or POCD.
Perioperative sleep disruption (Figure, panel E)
Although the physiologic function of sleep remains an active area of investigation, it is widely appreciated that adequate sleep is essential for maintaining normal endocrine, immune, and neurologic function. Additionally, disrupted sleep in animal models increases BBB permeability, inflammation, and AD neuropathology (each addressed in detail above). Moreover, sleep deprivation negatively affects memory consolidation and synaptic homeostasis.86 Because of these widespread implications of sleep disruption, OSA-induced sleep disruptions may impact susceptibility to delirium and cognitive dysfunction.
Indeed, many OSA patients exhibit chronic sleep disruptions, resulting in chronic sleep deficits, which are likely exacerbated following anesthesia and surgery. In the postoperative period, sleep disruption is characterized by a pattern of decreased REM sleep on the first night after surgery, followed by a rebound increase in REM density.87 It is not yet known how sleep disorders and OSA affect recovery from this sleep loss, or how this sleep loss impacts risk for postoperative delirium and cognitive dysfunction. The effects of sleep disruption on POD incidence and severity have been an open question, with numerous studies reporting conflicting results. Early studies concluded that sleep disruption is not associated with delirium onset; however, these findings have been disputed by recent studies that measured sleep more rigorously in various settings (home, hospital ward, and ICU) and found associations between impaired sleep and POD.87,88 These discrepancies are likely due to challenges in accurately assessing delirium and measuring sleep, since some of the above studies did not use rigorous frequent delirium assessments or objective sleep measurements.
Fadayomi et al. recently conducted a meta-analysis of 12 independent studies that evaluated the association between pre-existing sleep disturbances and POD. They determined that patients with preoperative sleep disturbance are approximately five times more likely to experience POD than those without a known history of sleep disturbance.89 Subanalysis revealed that sleep apnea and other unspecified sleep disorders had similarly strong associations with delirium onset. Although there are clear associations between sleep disruption, OSA, and delirium, the question remains whether OSA and/or sleep disruptions (i.e., undiagnosed sleep disorders) actually increase POD risk or whether these disorders are merely more common in patients who are susceptible to delirium. In essence, are sleep disruptions merely an indicator of delirium risk, or are they involved in delirium pathophysiology?
A compelling mechanism that may link sleep disruptions to impaired postoperative cognitive function relates to the critical role of sleep in integrating and stabilizing the neural circuits responsible for learning, memory, and cognitive function. Two decades of research have revealed that sleep and wake episodes play complementary roles in synaptic homeostasis, i.e., the balance between new synapse formation and old synapse degradation.86 Briefly, during waking periods, cortical synapse formation outweighs synapse degradation, allowing for the formation and strengthening of neural circuits corresponding to learning and information processing. Conversely, during sleep, the brain undergoes a net decrease in synaptic weight as superfluous cortical circuits are pruned, thereby improving circuit specificity and signal-to-noise ratios.90 This process, collectively known as the sleep homeostasis hypothesis, is an active area of study in animal models, and these findings have correlated with findings in humans of increased electroencephalographic theta activity (marking net synaptic proliferation), increased broad-cortex excitability, and reduced intracortical inhibition after wake episodes.91 This evidence from animal models and human studies suggests that impaired synaptic homeostasis could underpin the link between sleep disruption and delirium and the negative effects of sleep disruption on cognition.
Since sleep disruption likely contributes to delirium, there has been significant interest in therapeutic strategies to improve sleep. Although some medications, such as melatonin and melatonin receptor agonists, help restore circadian rhythms none of the medications commonly used in hospital settings, such as benzodiazepines, non-benzodiazepines, and trazodone, actually promote restorative sleep. Thus, recent efforts have focused on non-pharmacologic strategies, such as sleep hygiene, to potentially reduce POD. These interventions emphasize establishing a regular sleep routine, using eye shields and ear plugs during sleep, and avoiding use of light emitting screens before bedtime. Implementation of these non-pharmacologic interventions before and after surgery can attenuate the risk for POD, but implementation barriers and adherence present current challenges.92 Promoting sleep hygiene postoperatively may mitigate the sleep disturbance that predisposes patients to POD and POCD. More studies are needed to evaluate the extent to which these approaches improve postoperative cognitive outcomes, and the extent to which they will be effective in patients with underlying sleep disorders such as OSA. Successful interventions to promote restorative sleep and prevent POD would likely incorporate testing and treatment of underlying sleep disorders including OSA.
Sympathovagal imbalance (Figure, panel F)
Obstructive sleep apnea is characterized by a state of sympathovagal imbalance in which sympathetic overactivity dominates parasympathetic activity, in part because of reduced NREM sleep where parasympathetic activity predominates.93 Sympathovagal balance is typically assessed non-invasively by measuring heart rate variability, which exhibit low and high-frequency oscillations. High-frequency oscillations result from vagal activity, i.e., parasympathetic activity, while low-frequency oscillations occur secondary to cardiac accelerator fiber activity, i.e., sympathetic activity. Sympathetic overactivation is seen in OSA patients as an increased low-frequency/high-frequency heart rate variability ratio.94 Additionally, systemic catecholamine levels are increased in OSA patients during daytime and nighttime, suggesting that sympathovagal imbalance persists even outside of sleep.95 Similar findings of sympathovagal imbalance have been observed in patients with dementia, who also exhibit a range of autonomic-related symptoms such as syncope, urinary incontinence, and constipation.96 In dementia patients, the degree of autonomic dysfunction correlates with cognitive decline, and might even play a causative role in the pathogenesis of these disorders.97 There is also evidence that sympathovagal imbalance may be associated with cognitive deficits in other diseases such as heart failure and type II diabetes.98 Since OSA patients exhibit similar sympathovagal imbalance, these studies raise the question of whether sympathovagal imbalance is associated with POD and POCD in OSA patients.
Surgery and anesthesia are associated with sympathetic overexcitation and lower sympathetic activity, and recent evidence suggests that the extent of sympathovagal imbalance is associated with POD. In one study, older non-cardiac surgery patients exhibited sympathetic overactivity postoperatively, which was thought to be due to a cortisol-mediated stress response to anesthesia and surgery.99 Another recent study found that older esophagectomy patients who developed POD had lower preoperative high-frequency heart rate oscillations, consistent with lower vagal tone.100 Further studies are needed to determine the role of sympathovagal imbalance in POD and POCD, and whether sympathovagal imbalance is associated with POD and/or POCD in OSA patients.
Disrupted brain bioenergetics (Figure, panel G)
Disruption of neuronal bioenergetic homeostasis may also be a primary mediator of cognitive dysfunction in OSA patients. Intermittent hypoxia, a hallmark of OSA, disrupts oxidative metabolism by causing cerebral oxyhemoglobin desaturations,101 which in turn generate reactive oxygen species that damage neurons and inhibit mitochondrial oxidative phosphorylation.102 Indeed, OSA patients exhibit decreased cerebral oxyhemoglobin and decreased tissue oxygenation with insufficient compensatory blood flow increases,103 and older OSA patients exhibit shifts toward anaerobic metabolism with decreased cerebral adenosine triphosphate (ATP) and elevated lactate, as measured by magnetic resonance spectroscopy (MRS).103 The application of MRS has augmented studies of bioenergetics substantially, offering real-time analysis of metabolic derangements during hypoxic events in humans, and permitting correlation between cerebral biochemical, structural, and cognitive changes. One study using MRS found decreased frontal lobe neuronal viability and increased white matter turnover in OSA patients.104 Other studies have used MRS to assess ATP, phosphocreatine, and lactate levels to understand brain bioenergetics in patients following sleep deprivation.105 One study showed that, following acute sleep deprivation, gray matter phosphocreatine increased during sleep recovery, suggesting that restorative sleep promotes brain energy homeostasis.106 Despite emerging evidence that OSA and its hallmarks of sleep deprivation and intermittent hypoxia disrupt normal bioenergetics, we do not yet fully understand the degree to which these abnormalities contribute to cognitive dysfunction in OSA patients, nor to what extent these neurometabolic changes are corrected by OSA treatment such as CPAP therapy.
Recently, evidence that correlates altered cerebral metabolism with cognitive dysfunction in patients with OSA has also been obtained via P MRS,31 which assesses the inorganic phosphate (Pi) to ATP ratio as a measure of brain energy depletion. In this study, a lower Pi/ATP ratio in the temporal lobe significantly correlated with impaired performance on psychomotor vigilance and simulated driving performance in OSA patients, suggesting that these changes may be factors that underpin cognitive disturbance.105 Nevertheless, the effects of brain metabolic changes on a comprehensive battery of cognitive tests were not measured, and warrant further investigation. The extent to which OSA-driven changes in bioenergetics predispose patients undergoing anesthesia and surgery to POCD or POD remains unknown. Several studies support this “neurometabolic hypothesis of delirium”, with animal studies showing mitochondrial impairment after anesthesia and surgery,107 and human studies showing preoperative perturbations in glutamate synthesis and lipid metabolism in the CSF of hip fracture patients with POD.108 Taken together, these studies suggest that OSA disrupts normal brain bioenergetics and that this could play an important role in the development of postoperative cognitive disorders. Further studies are needed to determine the specific bioenergetic pathways that are disrupted in OSA patients and whether they contribute to the development of POD and POCD.
Conclusion
Currently, we lack evidence for the role of OSA in postoperative neurocognitive disorders because few studies have been conducted in the perioperative setting. We identified only seven studies that have examined OSA as a potential risk factor for POD, and no studies that investigated whether OSA is associated with POCD. Nevertheless, a potential role of OSA as a risk factor for POCD and POD is plausible, given that recent studies have shown an association between OSA and cognitive impairment outside of surgery. Thus, there is a need for future studies to assess the relationship between OSA and postoperative neurocognitive disorders, as well as for randomized controlled trials of CPAP to prevent POCD and POD (Table 2). Possible mechanisms underlying increased risk for POD and/or POCD in OSA patients should also be investigated, and may represent future targets to prevent POD, POCD, or even cognitive decline beyond the perioperative period.
References
Rudolph JL, Marcantonio ER. Review articles: postoperative delirium: acute change with long-term implications. Anesth Anal 2011; 112: 1202–11.
Berger M, Nadler JW, Browndyke J, et al. Postoperative cognitive dysfunction: minding the gaps in our knowledge of a common postoperative complication in the elderly. Anesthesiol Clin 2015; 33: 517–50. https://doi.org/10.1016/j.anclin.2015.05.008
Evered L, Silbert B, Knopman DS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery–2018. Br J Anaesth 2018; 121: 1005–12. https://doi.org/10.1016/j.bja.2017.11.087
Browndyke JN, Devinney M, Mathew JP. The devil is in the details: comparison of postoperative delirium and neurocognitive dysfunction. Anesthesiology 2019; 131: 456–8. https://doi.org/10.1097/aln.0000000000002823
Baethge C, Goldbeck-Wood S, Mertens S. SANRA—a scale for the quality assessment of narrative review articles. Res Integr Peer Review 2019; 4: 5. https://doi.org/10.1186/s41073-019-0064-8
Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 2008; 5: 136–43. https://doi.org/10.1513/pats.200709-155mg
Veasey SC, Rosen IM. Obstructive sleep apnea in adults. N Engl J Med 2019; 380: 1442–9. https://doi.org/10.1056/nejmcp1816152
Pack AI, Magalang UJ, Singh B, Kuna ST, Keenan BT, Maislin G. Randomized clinical trials of cardiovascular disease in obstructive sleep apnea: understanding and overcoming bias. Sleep 2020; 44. https://doi.org/10.1093/sleep/zsaa229
Suurna MV, Krieger AC. Obstructive sleep apnea: non-positive airway pressure treatments. Clin Geriatr Med 2021; 37: 429–44. https://doi.org/10.1016/j.cger.2021.04.005
Auckley D. Perioperative complications in obstructive sleep apnea patients. Curr Sleep Med Rep 2016; 2: 87–98. https://doi.org/10.1007/s40675-016-0040-5
Seet E, Chua M, Liaw CM. High STOP-BANG questionnaire scores predict intraoperative and early postoperative adverse events. Singapore Med J 2015; 56: 212–6. https://doi.org/10.11622/smedj.2015034
Chung F, Memtsoudis SG, Ramachandran SK, et al. Society of Anesthesia and Sleep Medicine Guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg 2016; 123: 452–73. https://doi.org/10.1213/ane.0000000000001416
Kerner NA, Roose SP. Obstructive sleep apnea is linked to depression and cognitive impairment: evidence and potential mechanisms. Am J Geriatr Psychiatry 2016; 24: 496–508. https://doi.org/10.1016/j.jagp.2016.01.134
Liguori C, Maestri M, Spanetta M, et al. Sleep-disordered breathing and the risk of Alzheimer's disease. Sleep Med Rev 2021; 55: 101375. https://doi.org/10.1016/j.smrv.2020.101375
Liguori C, Mercuri NB, Izzi F, et al. Obstructive sleep apnea is associated with early but possibly modifiable alzheimer's disease biomarkers changes. Sleep 2017; 40. https://doi.org/10.1093/sleep/zsx011
André C, Rehel S, Kuhn E, et al. Association of sleep-disordered breathing with Alzheimer Disease biomarkers in community-dwelling older adults: a secondary analysis of a randomized clinical trial. JAMA Neurol 2020; 77: 716–24. https://doi.org/10.1001/jamaneurol.2020.0311
Lucey BP, Mawuenyega KG, Patterson BW, et al. Associations between β-amyloid kinetics and the β-amyloid diurnal pattern in the central nervous system. JAMA Neurol 2017; 74: 207–15. https://doi.org/10.1001/jamaneurol.2016.4202
Culebras A, Anwar S. Sleep apnea is a risk factor for stroke and vascular dementia. Curr Neurol Neurosci Rep 2018; 18: 53. https://doi.org/10.1007/s11910-018-0855-1
Macey PM, Kumar R, Woo MA, Valladares EM, Yan-Go FL, Harper RM. Brain structural changes in obstructive sleep apnea. Sleep 2008; 31: 967–77.
Lajoie AC, Lafontaine AL, Kimoff RJ, Kaminska M. Obstructive Sleep apnea in neurodegenerative disorders: current evidence in support of benefit from sleep apnea treatment. J Clin Med 2020; 9: 297. https://doi.org/10.3390/jcm9020297
Mullins AE, Kam K, Parekh A, Bubu OM, Osorio RS, Varga AW. Obstructive sleep apnea and its treatment in aging: effects on Alzheimer's disease biomarkers, cognition, brain structure and neurophysiology. Neurobiol Dis 2020; 145: 105054. https://doi.org/10.1016/j.nbd.2020.105054
Jehan S, Farag M, Zizi F, et al. Obstructive sleep apnea and stroke. Sleep Med Disord 2018; 2: 120–5.
van Harten AE, Scheeren TW, Absalom AR. A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anaesthesia. Anaesthesia 2012; 67: 280–93. https://doi.org/10.1111/j.1365-2044.2011.07008.x
Newman MF, Grocott HP, Mathew JP, et al. Report of the substudy assessing the impact of neurocognitive function on quality of life 5 years after cardiac surgery. Stroke 2001; 32: 2874–81. https://doi.org/10.1161/hs1201.099803
Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology 2008; 108: 18–30. https://doi.org/10.1097/01.anes.0000296071.19434.1e
Berger M, Burke J, Eckenhoff R, Mathew J. Alzheimer's disease, anesthesia, and surgery: a clinically focused review. J Cardiothorac Vasc Anesth 2014; 28: 1609–23. https://doi.org/10.1053/j.jvca.2014.04.014
Berger M, Terrando N, Smith SK, Browndyke JN, Newman MF, Mathew JP. Neurocognitive function after cardiac surgery: from phenotypes to mechanisms. Anesthesiology 2018; 129: 829–51. https://doi.org/10.1097/aln.0000000000002194
Gupta RM, Parvizi J, Hanssen AD, Gay PC. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc 2001; 76: 897–905. https://doi.org/10.4065/76.9.897
Flink BJ, Rivelli SK, Cox EA, et al. Obstructive sleep apnea and incidence of postoperative delirium after elective knee replacement in the nondemented elderly. Anesthesiology 2012; 116: 788–96. https://doi.org/10.1097/aln.0b013e31824b94fc
Roggenbach J, Klamann M, von Haken R, Bruckner T, Karck M, Hofer S. Sleep-disordered breathing is a risk factor for delirium after cardiac surgery: a prospective cohort study. Crit Care 2014; 18: 477. https://doi.org/10.1186/s13054-014-0477-1
Chan MT, Wang CY, Seet E, et al. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA 2019; 321: 1788–98. https://doi.org/10.1001/jama.2019.4783
Wang S, Sigua NL, Manchanda S, et al. Preoperative STOP-BANG scores and postoperative delirium and coma in thoracic surgery patients. Ann Thorac Surg 2018; 106: 966–72. https://doi.org/10.1016/j.athoracsur.2018.05.089
Strutz PK, Kronzer V, Tzeng W, et al. The relationship between obstructive sleep apnoea and postoperative delirium and pain: an observational study of a surgical cohort. Anaesthesia; 74: 1542–50. https://doi.org/10.1111/anae.14855
Wagner S, Quente J, Staedtler S, et al. A high risk of sleep apnea is associated with less postoperative cognitive dysfunction after intravenous anesthesia: results of an observational pilot study. BMC Anesthesiol 2018; 18: 139. https://doi.org/10.1186/s12871-018-0602-9
Canessa N, Castronovo V, Cappa SF, et al. Obstructive sleep apnea: brain structural changes and neurocognitive function before and after treatment. Am J Respir Crit Care Med 2011; 183: 1419–26. https://doi.org/10.1164/rccm.201005-0693oc
Nadler JW, Evans JL, Fang E, et al. A randomised trial of peri-operative positive airway pressure for postoperative delirium in patients at risk for obstructive sleep apnoea after regional anaesthesia with sedation or general anaesthesia for joint arthroplasty. Anaesthesia 2017; 72: 729–36. https://doi.org/10.1111/anae.13833
Nagappa M, Mokhlesi B, Wong J, Wong DT, Kaw R, Chung F. The effects of continuous positive airway pressure on postoperative outcomes in obstructive sleep apnea patients undergoing surgery: a systematic review and meta-analysis. Anesth Analg 2015; 120: 1013–23. https://doi.org/10.1213/ane.0000000000000634
Puri S, Panza G, Mateika JH. A comprehensive review of respiratory, autonomic and cardiovascular responses to intermittent hypoxia in humans. Exp Neurol 2021; 341: 113709. https://doi.org/10.1016/j.expneurol.2021.113709
Kim LJ, Freire C, Curado TF, Jun JC, Polotsky VY. The role of animal models in developing pharmacotherapy for obstructive sleep apnea. J Clin Med 2019; 8: 2049. https://doi.org/10.3390/jcm8122049
Sapin E, Peyron C, Roche F, et al. Chronic intermittent hypoxia induces chronic low-grade neuroinflammation in the dorsal hippocampus of mice. Sleep 2015; 38: 1537–46. https://doi.org/10.5665/sleep.5042
Gozal D, Daniel JM, Dohanich GP. Behavioral and anatomical correlates of chronic episodic hypoxia during sleep in the rat. J Neurosci 2001; 21: 2442–50. https://doi.org/10.1523/jneurosci.21-07-02442.2001
Payne RS, Goldbart A, Gozal D, Schurr A. Effect of intermittent hypoxia on long-term potentiation in rat hippocampal slices. Brain Res 2004; 1029: 195–9. https://doi.org/10.1016/j.brainres.2004.09.045
Xie X, Pan L, Ren D, Du C, Guo Y. Effects of continuous positive airway pressure therapy on systemic inflammation in obstructive sleep apnea: a meta-analysis. Sleep Med 2013; 14: 1139–50. https://doi.org/10.1016/j.sleep.2013.07.006
Baril AA, Martineau-Dussault M, Sanchez E, et al. Obstructive sleep apnea and the brain: a focus on gray and white matter structure. Curr Neurol Neurosci Rep 2021; 21: 11. https://doi.org/10.1007/s11910-021-01094-2
Morrell MJ, McRobbie DW, Quest RA, Cummin AR, Ghiassi R, Corfield DR. Changes in brain morphology associated with obstructive sleep apnea. Sleep Med 2003; 4: 451–4. https://doi.org/10.1016/s1389-9457(03)00159-x
Snyder B, Shell B, Cunningham JT, Cunningham RL. Chronic intermittent hypoxia induces oxidative stress and inflammation in brain regions associated with early-stage neurodegeneration. Physiol Rep 2017; 5: e13258. https://doi.org/10.14814/phy2.13258
Lenz KM, Nelson LH. Microglia and beyond: innate immune cells as regulators of brain development and behavioral function. Front Immunol 2018; 9: 698. https://doi.org/10.3389/fimmu.2018.00698
Nonaka S, Nakanishi H. Microglial clearance of focal apoptotic synapses. Neurosci Lett 2019; 707: 134317. https://doi.org/10.1016/j.neulet.2019.134317
Var SR, Byrd-Jacobs CA. Role of macrophages and microglia in zebrafish regeneration. Int J Mol Sci 2020; 21: 4768. https://doi.org/10.3390/ijms21134768
Shieh CH, Heinrich A, Serchov T, van Calker D, Biber K. P2X7-dependent, but differentially regulated release of IL-6, CCL2, and TNF-α in cultured mouse microglia. Glia 2014; 62: 592–607. https://doi.org/10.1002/glia.22628
Kiernan EA, Smith SM, Mitchell GS, Watters JJ. Mechanisms of microglial activation in models of inflammation and hypoxia: Implications for chronic intermittent hypoxia. J Physiol 2016; 594: 1563–77. https://doi.org/10.1113/jp271502
Gale SD, Hopkins RO. Effects of hypoxia on the brain: neuroimaging and neuropsychological findings following carbon monoxide poisoning and obstructive sleep apnea. J Int Neuropsychol Soc 2004; 10: 60–71. https://doi.org/10.1017/s1355617704101082
Fatouleh RH, Lundblad LC, Macey PM, McKenzie DK, Henderson LA, Macefield VG. Reversal of functional changes in the brain associated with obstructive sleep apnoea following 6 months of CPAP. Neuroimage Clin 2015; 7: 799–806. https://doi.org/10.1016/j.nicl.2015.02.010
Macey PM, Haris N, Kumar R, Thomas MA, Woo MA, Harper RM. Obstructive sleep apnea and cortical thickness in females and males. PLoS One 2018; 13: e0193854. https://doi.org/10.1371/journal.pone.0193854
Macey PM, Harper RM. OSA brain morphology differences: magnitude of loss approximates age-related effects. Am J Respir Crit Care Med 2005; 172: 1056–7. https://doi.org/10.1164/ajrccm.172.8.954
Park B, Palomares JA, Woo MA, et al. Disrupted functional brain network organization in patients with obstructive sleep apnea. Brain Behav 2016; 6: e00441. https://doi.org/10.1002/brb3.441
Rostanski SK, Zimmerman ME, Schupf N, et al. Sleep disordered breathing and white matter hyperintensities in community-dwelling elders. Sleep 2016; 39: 785–91. https://doi.org/10.5665/sleep.5628
Quagliarello VJ, Wispelwey B, Long WJ Jr, Scheld WM. Recombinant human interleukin-1 induces meningitis and blood-brain barrier injury in the rat. Characterization and comparison with tumor necrosis factor. J Clin Invest 1991; 87: 1360–6. https://doi.org/10.1172/jci115140
Witt KA, Mark KS, Hom S, Davis TP. Effects of hypoxia-reoxygenation on rat blood-brain barrier permeability and tight junctional protein expression. Am J Physiol Heart Circ Physiol 2003; 285: H2820–31. https://doi.org/10.1152/ajpheart.00589.2003
Schoch HJ, Fischer S, Marti HH. Hypoxia‐induced vascular endothelial growth factor expression causes vascular leakage in the brain. Brain 2002; 125: 2549–57. https://doi.org/10.1093/brain/awf257
Gómez-González B, Hurtado-Alvarado G, Esqueda-León E, Santana-Miranda R, Rojas-Zamorano J, Velázquez-Moctezuma J. REM sleep loss and recovery regulates blood-brain barrier function. Curr Neurovasc Res 2013; 10: 197–207. https://doi.org/10.2174/15672026113109990002
Khalyfa A, Gozal D, Kheirandish-Gozal L. Plasma exosomes disrupt the blood–brain barrier in children with obstructive sleep apnea and neurocognitive deficits. Am J Respir Crit Care Med 2018; 197: 1073–6. https://doi.org/10.1164/rccm.201708-1636le
Palomares JA, Tummala S, Wang DJ, et al. Water exchange across the blood-brain barrier in obstructive sleep apnea: an MRI diffusion-weighted pseudo-continuous arterial spin labeling study. J Neuroimaging 2015; 25: 900–5. https://doi.org/10.1111/jon.12288
Sweeney MD, Sagare AP, Zlokovic BV. Blood–brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol 2018; 14: 133–50. https://doi.org/10.1038/nrneurol.2017.188
He HJ, Wang Y, Le Y, et al. Surgery upregulates high mobility group box-1 and disrupts the blood–brain barrier causing cognitive dysfunction in aged rats. CNS Neurosci Ther 2012; 18: 994–1002. https://doi.org/10.1111/cns.12018
Ma L, Zhang H, Liu YZ, Yin YL, Ma YQ, Zhang SS. Ulinastatin decreases permeability of blood--brain barrier by inhibiting expression of MMP-9 and t-PA in postoperative aged rats. Int J Neurosci 2016; 126: 463–8. https://doi.org/10.3109/00207454.2015.1025394
Abrahamov D, Levran O, Naparstek S, et al. Blood–brain barrier disruption after cardiopulmonary bypass: diagnosis and correlation to cognition. Ann Thorac Surg 2017; 104: 161–9. https://doi.org/10.1016/j.athoracsur.2016.10.043
Munoz R, Duran-Cantolla J, Martínez-Vila E, et al. Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke 2006; 37: 2317–21. https://doi.org/10.1161/01.str.0000236560.15735.0f
Yaggi H, Mohsenin V. Obstructive sleep apnoea and stroke. Lancet Neurol 2004; 3: 333–42. https://doi.org/10.1016/s1474-4422(04)00766-5
Chokesuwattanaskul A, Lertjitbanjong P, Thongprayoon C, et al. Impact of obstructive sleep apnea on silent cerebral small vessel disease: a systematic review and meta-analysis. Sleep Med 2020; 68: 80–8. https://doi.org/10.1016/j.sleep.2019.11.1262
Ward SA, Storey E, Woods RL, et al. The study of neurocognitive outcomes, radiological and retinal effects of aspirin in sleep apnoea- rationale and methodology of the SNORE-ASA study. Contemp Clin Trials 2018; 64: 101–11. https://doi.org/10.1016/j.cct.2017.10.016
Vlisides P, Mashour GA. Perioperative stroke. Can J Anesth 2016; 63: 193–204. https://doi.org/10.1007/s12630-015-0494-9
Mrkobrada M, Hill MD, Chan MT, et al. Covert stroke after non-cardiac surgery: a prospective cohort study. Br J Anaesth 2016; 117: 191–7. https://doi.org/10.1093/bja/aew179
NeuroVISION Investigators. Perioperative covert stroke in patients undergoing non-cardiac surgery (NeuroVISION): a prospective cohort study. Lancet 2019; 394: 1022–9. https://doi.org/10.1016/s0140-6736(19)31795-7
Shi L, Chen SJ, Ma MY, et al. Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev 2018; 40: 4–16. https://doi.org/10.1016/j.smrv.2017.06.010
Mander BA, Winer JR, Jagust WJ, Walker MP. Sleep: a novel mechanistic pathway, biomarker, and treatment target in the pathology of Alzheimer's disease? Trends Neurosci 2016; 39: 552–66. https://doi.org/10.1016/j.tins.2016.05.002
Kim JH, Jung H, Lee Y, Sohn JH. Surgery performed under propofol anesthesia induces cognitive impairment and amyloid pathology in ApoE4 knock-in mouse model. Front Aging Neurosci 2021; 13: 658860. https://doi.org/10.3389/fnagi.2021.658860
Berger M, Browndyke JN, Cooter Wright M, et al. Postoperative changes in cognition and cerebrospinal fluid neurodegenerative disease biomarkers. Ann Clin Transl Neurol 2022; 9: 155–70. https://doi.org/10.1002/acn3.51499
Xie Z, Swain CA, Ward SA, et al. Preoperative cerebrospinal fluid β-amyloid/tau ratio and postoperative delirium. Ann Clin Transl Neurol 2014; 1: 319–28. https://doi.org/10.1002/acn3.58
Cunningham EL, McGuinness B, McAuley DF, et al. CSF beta-amyloid 1-42 concentration predicts delirium following elective arthroplasty surgery in an observational cohort study. Ann Surg 2019; 269: 1200–5. https://doi.org/10.1097/sla.0000000000002684
Witlox J, Kalisvaart KJ, de Jonghe JF, et al. Cerebrospinal fluid β-amyloid and tau are not associated with risk of delirium: a prospective cohort study in older adults with hip fracture. J Am Geriatr Soc 2011; 59: 1260–7. https://doi.org/10.1111/j.1532-5415.2011.03482.x
Fjell AM, Idland AV, Sala-Llonch R, et al. Neuroinflammation and tau interact with amyloid in predicting sleep problems in aging independently of atrophy. Cereb Cortex 2018; 28: 2775–85. https://doi.org/10.1093/cercor/bhx157
Shiota S, Inoue Y, Takekawa H, et al. Effect of continuous positive airway pressure on regional cerebral blood flow during wakefulness in obstructive sleep apnea. Sleep Breath 2014; 18: 289–95. https://doi.org/10.1007/s11325-013-0881-9
Kluger MT, Collier JM, Borotkanics R, van Schalkwyk JM, Rice DA. The effect of intra-operative hypotension on acute kidney injury, postoperative mortality and length of stay following emergency hip fracture surgery. Anaesthesia 2021; 77: 164–74. https://doi.org/10.1111/anae.15555
Brown CH, Neufeld KJ, Tian J, et al. Effect of targeting mean arterial pressure during cardiopulmonary bypass by monitoring cerebral autoregulation on postsurgical delirium among older patients: a nested randomized clinical trial. JAMA Surg 2019; 154: 819–26. https://doi.org/10.1001/jamasurg.2019.1163
Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron 2014; 81: 12–34. https://doi.org/10.1016/j.neuron.2013.12.025
Leung JM, Sands LP, Newman S, et al. Preoperative sleep disruption and postoperative delirium. J Clin Sleep Med 2015; 11: 907–13. https://doi.org/10.5664/jcsm.4944
Todd OM, Gelrich L, MacLullich AM, Driessen M, Thomas C, Kreisel SH. Sleep disruption at home as an independent risk factor for postoperative delirium. J Am Geriatr Soc 2017; 65: 949–57. https://doi.org/10.1111/jgs.14685
Fadayomi AB, Ibala R, Bilotta F, Westover MB, Akeju O. A systematic review and meta-analysis examining the impact of sleep disturbance on postoperative delirium. Crit Care Med 2018; 46: e1204–12. https://doi.org/10.1097/ccm.0000000000003400
Born J, Feld GB. Sleep to upscale, sleep to downscale: balancing homeostasis and plasticity. Neuron 2012; 75: 933–5. https://doi.org/10.1016/j.neuron.2012.09.007
Kuhn M, Wolf E, Maier JG, et al. Sleep recalibrates homeostatic and associative synaptic plasticity in the human cortex. Nat Comm 2016; 7: 12455. https://doi.org/10.1038/ncomms12455
Flannery AH, Oyler DR, Weinhouse GL. The impact of interventions to improve sleep on delirium in the ICU: a systematic review and research framework. Crit Care Med 2016; 44: 2231–40. https://doi.org/10.1097/ccm.0000000000001952
Somers VK, Dyken, ME, Mark, AL, Abboud, FM. Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med 1993; 328: 303–7. https://doi.org/10.1056/nejm199302043280502
Narkiewicz K, Montano N, Cogliati C, van de Borne PJ, Dyken ME, Somers VK. Altered cardiovascular variability in obstructive sleep apnea. Circulation 1998; 98: 1071–7. https://doi.org/10.1161/01.cir.98.11.1071
Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest 1995; 96: 1897–904. https://doi.org/10.1172/jci118235
Aharon-Peretz J, Harel T, Revach M, Ben-Haim SA. Increased sympathetic and decreased parasympathetic cardiac innervation in patients with Alzheimer's disease. Arch Neurol 1992; 49: 919–22. https://doi.org/10.1001/archneur.1992.00530330041013
Collins O, Dillon S, Finucane C, Lawlor B, Kenny RA. Parasympathetic autonomic dysfunction is common in mild cognitive impairment. Neurobiol Aging 2012; 33: 2324–33. https://doi.org/10.1016/j.neurobiolaging.2011.11.017
Auroprajna P, Naik BM, Sahoo JP, Keerthi GS, Pavanya M, Pal GK. Association of sympathovagal imbalance with cognitive impairment in type 2 diabetes in adults. Can J Diabetes 2018; 42: 44–50. https://doi.org/10.1016/j.jcjd.2017.01.008
Amar D, Fleisher M, Pantuck CB, et al. Persistent alterations of the autonomic nervous system after noncardiac surgery. Anesthesiology 1998; 89: 30–42. https://doi.org/10.1097/00000542-199807000-00008
Echizen M, Satomoto M, Miyajima M, Adachi Y, Matsushima E. Preoperative heart rate variability analysis is as a potential simple and easy measure for predicting perioperative delirium in esophageal surgery. Ann Med Surg (Lond) 2021; 70: 102856. https://doi.org/10.1016/j.amsu.2021.102856
Hayakawa T, Terashima M, Kayukawa Y, Ohta T, Okada T. Changes in cerebral oxygenation and hemodynamics during obstructive sleep apneas. Chest 1996; 109: 916–21. https://doi.org/10.1378/chest.109.4.916
Douglas RM, Ryu J, Kanaan A, et al. Neuronal death during combined intermittent hypoxia/hypercapnia is due to mitochondrial dysfunction. Am J Physiol Cell Physiol 2010; 298: C1594–602. https://doi.org/10.1152/ajpcell.00298.2009
Rae C, Bartlett DJ, Yang Q, et al. Dynamic changes in brain bioenergetics during obstructive sleep apnea. J Cereb Blood Flow Metab 2009; 29: 1421–8. https://doi.org/10.1038/jcbfm.2009.57
O'Donoghue FJ, Wellard RM, Rochford PD, et al. Magnetic resonance spectroscopy and neurocognitive dysfunction in obstructive sleep apnea before and after CPAP treatment. Sleep 2012; 35: 41–8. https://doi.org/10.5665/sleep.1582
D'Rozario AL, Bartlett DJ, Wong KK, et al. Brain bioenergetics during resting wakefulness are related to neurobehavioral deficits in severe obstructive sleep apnea: a 31P magnetic resonance spectroscopy study. Sleep 2018; 41. https://doi.org/10.1093/sleep/zsy117
Plante DT, Trksak GH, Jensen JE, et al. Gray matter-specific changes in brain bioenergetics after acute sleep deprivation: a 31P magnetic resonance spectroscopy study at 4 tesla. Sleep 2014; 37: 1919–27. https://doi.org/10.5665/sleep.4242
Lu Y, Chen L, Ye J, et al. Surgery/anesthesia disturbs mitochondrial fission/fusion dynamics in the brain of aged mice with postoperative delirium. Aging (Albany NY) 2020; 12: 844–65. https://doi.org/10.18632/aging.102659
Han Y, Zhang W, Liu J, et al. Metabolomic and lipidomic profiling of preoperative CSF in elderly hip fracture patients with postoperative delirium. Front Aging Neurosci 2020; 12: 570210. https://doi.org/10.3389/fnagi.2020.570210
Author contributions
Michael J. Devinney contributed to all aspects of this manuscript, including study conception and design, acquisition and interpretation of data, and drafting the article. Miles Berger contributed to study conception and design, interpretation of data, and drafting the article. Keith W. VanDusen, Jad M. Kfouri, and Pallavi Avasarala contributed to the acquisition and interpretation of data and drafting the article. Andrew R. Spector and Joseph P. Mathew contributed to study conception and design and drafting the article.
Acknowledgements
We thank Kathy Gage for comments on this manuscript, Leila Ledbetter for conducting the literature searches, and Stan Coffman for work on the illustrations.
Disclosures
None.
Funding statement
Dr. Devinney acknowledges support from the National Institutes of Health (R03AG067976), a Research Fellowship Grant from the Foundation for Anesthesia Education and Research, a William L. Young neuroscience research award from the Society for Neuroscience in Anesthesiology and Critical Care (SNACC), NIH T32 GM008600, and additional support from the Duke Anesthesiology Department. Dr. Berger acknowledges support from the National Institutes of Health (1K76AG057022) (to Dr. Miles Berger) and additional support from the Duke Claude D. Pepper Older American Independence Center (P30AG028716), a William L. Young neuroscience research award from the Society for Neuroscience in Anesthesiology and Critical Care (SNACC), and the Duke Anesthesiology Department. Dr. Mathew acknowledges support from the National Institutes of Health (1R01AG074185).
Editorial responsibility
This submission was handled by Dr. Alana M. Flexman, Associate Editor, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Devinney, M.J., VanDusen, K.W., Kfouri, J.M. et al. The potential link between obstructive sleep apnea and postoperative neurocognitive disorders: current knowledge and possible mechanisms. Can J Anesth/J Can Anesth 69, 1272–1287 (2022). https://doi.org/10.1007/s12630-022-02302-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02302-4