Abstract
Purpose
Optimal heparin titration during cardiopulmonary bypass (CPB) may reduce coagulation system activation and preserve hemostatic function post-CPB. Our objective was to assess if the Heparin Management System (HMS) Plus improves heparin titration, thereby leading to higher thrombin generation post-CPB compared with activated clotting time (ACT)-guided management.
Methods
We conducted a randomized controlled trial of 100 patients undergoing cardiac surgery with CPB at a single center. A total of 50 patients were randomized to conventional ACT-guided management, and 50 to the HMS Plus system. The primary outcome was change in thrombin generation post-CPB compared with baseline, as assessed by calibrated automated thrombography. Secondary outcomes included intraoperative blood loss, chest drain output up to 72 hr, and transfusions. In an exploratory analysis, we compared the quintile of patients with the highest average heparin concentration on CPB (≥ 4.0 mg⋅kg-1) with the rest of the cohort.
Results
A total of 100 patients were included in an intent-to-treat analysis. We observed no difference in post-CPB thrombin generation or secondary outcomes. However, patients in the HMS Plus group had higher average heparin concentrations while on CPB than patients in the conventional management group did (mean difference, -0.21; 95% confidence interval, -0.42 to -0.01). The quintile of patients with the highest average heparin concentration (4.0 mg⋅kg-1) had higher thrombin generation post-CPB than the rest of the cohort did.
Conclusions
The HMS Plus system did not show significant benefits in thrombin generation, bleeding outcomes, or transfusion in patients undergoing cardiac surgery with CPB. Higher average heparin concentrations on CPB were associated with higher post-CPB thrombin generation.
Study registration
www.ClinicalTrials.gov (NCT03347201); first submitted 12 October 2017.
Résumé
Objectif
Un titrage optimal de l’héparine pendant la circulation extracorporelle (CEC) peut réduire l’activation du système de coagulation et préserver la fonction hémostatique après la CEC. Notre objectif était d’évaluer si le système de gestion de l’héparine HMS Plus améliorait le titrage de l’héparine, entraînant ainsi une génération de thrombine plus élevée après la CEC par rapport à la gestion guidée par le temps de coagulation activé (ACT).
Méthode
Nous avons réalisé une étude randomisée contrôlée de 100 patients bénéficiant d’une chirurgie cardiaque sous CEC dans un seul établissement. Au total, 50 patients ont été randomisés à une gestion conventionnelle guidée par l’ACT et 50 à une gestion guidée par le système HMS Plus. Le critère d’évaluation principal était la variation de la génération de thrombine post-CEC par rapport aux valeurs de base, telles qu’évaluées par thrombographie calibrée automatisée. Les critères secondaires comprenaient les pertes sanguines peropératoires, le drainage thoracique jusqu’à 72 heures et les transfusions. Dans une analyze exploratoire, nous avons comparé le quintile de patients ayant la concentration moyenne d’héparine la plus élevée sous CEC (≥ 4,0 mg⋅kg-1) au reste de la cohorte.
Résultats
Au total, 100 patients ont été inclus dans une analyze en intention de traiter. Nous n’avons observé aucune différence dans la génération de thrombine post-CEC ou dans nos critères d’évaluation secondaires. Cependant, les patients du groupe HMS Plus présentaient des concentrations moyennes d’héparine plus élevées sous CEC que les patients du groupe de gestion conventionnelle (différence moyenne, -0,21; intervalle de confiance à 95 %, -0,42 à -0,01). Le quintile de patients ayant la concentration moyenne d’héparine la plus élevée (4,0 mg⋅kg-1) avaient une génération de thrombine post-CEC plus élevée que le reste de la cohorte.
Conclusion
Le système HMS Plus n’a pas montré d’avantages significatifs dans la génération de thrombine, les issues hémorragiques ou la transfusion chez les patients bénéficiant d’une chirurgie cardiaque sous CEC. Des concentrations moyennes d’héparine plus élevées sous CEC ont été associées à une génération de thrombine post-CEC plus élevée.
Enregistrement de l’étude
www.ClinicalTrials.gov (NCT03347201); soumis pour la première fois le 12 octobre 2017.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Coagulopathy and bleeding are common complications of cardiac surgery with cardiopulmonary bypass (CPB).1,2,3 While the causes of coagulopathy are multifactorial, impaired thrombin generation plays a central role.1 Heparin-coated CPB circuits and high levels of systemic heparin anticoagulation are used to prevent hemostatic system activation and thrombin generation during CPB.4 Nevertheless, activation of the extrinsic and intrinsic hemostatic systems on bypass circuit components can continue, resulting in consumptive coagulopathy.2
Conventional heparin management using weight-based heparin dosing and activated clotting time (ACT) monitoring has been the historical mainstream practice for suppression of thrombin generation during CPB.5 Nevertheless, there are a number of reasons to question the reliability of ACT-guided heparin management. Firstly, nonspecific prolongations of the ACT are common and may be caused by patient or CPB-related factors independent of the achieved heparin concentration.6,7 Secondly, there is poor agreement between different ACT devices, which may lead to important differences in heparin and protamine dosing.8,9 Lastly, variation in individual responses to heparin limits the effectiveness and safety of weight-based heparin dosing.10
The Heparin Management System (HMS) Plus hemostasis system (Medtronic, Inc., Minneapolis, MN, USA) was developed to address the limitations of ACT-guided heparin management. It allows for personalized anticoagulation by assessing a patient’s individual heparin dose–response curve, and uses heparin–protamine titration (HPT) to measure heparin concentration and dose protamine. Heparin concentrations assessed with HMS Plus show better correlation with plasma heparin levels11,12,13 during CPB than ACT measurements do. Additionally, the HMS Plus system may improve post-CPB protamine management.14,15,16 A technology capable of assessing thrombin generation is calibrated automated thrombography (CAT), which provides a more accurate reflection of hemostatic potential related to thrombin generation than conventional tests of hemostasis do.1,17,18,19,20
If the HMS Plus system prevents thrombin generation more effectively during CPB by personalizing heparin dosing, it may be more effective at preserving thrombin generation potential post-CPB, thereby reducing coagulopathy and transfusion, along with their associated effects on morbidity and mortality. The primary aim of this study was to determine if heparin management using the HMS Plus system improves post-CPB thrombin generation as assessed by CAT parameters. The secondary aim was to assess if HMS Plus use is associated with improvements in clinical bleeding outcomes, including blood loss and transfusion rates 24 hr after CPB. Our hypothesis was that reliably higher heparin concentrations while on CPB would improve post-CPB thrombin generation.
Methods
Study design
This was a single-center, parallel-group prospective randomized controlled trial (www.ClinicalTrials.gov; identifier NCT03347201; first submitted on 12 October 2017) of 100 patients randomized 1:1 in randomly permutated blocks to titrated heparin and protamine dosing based on HMS Plus management (intervention group), or conventional ACT-guided management (control group). Research ethics board approval was obtained from the University Health Network (Toronto, ON, Canada; REB ID 15-9761). Eligible patients were those undergoing nonemergent coronary artery bypass grafting, valve repair or replacement (with or without ascending aortic replacement), or a combination of these procedures requiring the use of CPB. Exclusions included an inability to provide informed consent, age less than 19 yr, liver dysfunction (defined as liver enzymes > two-fold higher than upper limit of normal), planned use of deep hypothermic circulatory arrest or brief circulatory arrest, highly complex cases (left ventricular device insertion or explant, heart transplant, or complex congenital repairs), pre-existing coagulopathy (international normalized ratio > 1.5, partial thromboplastin time > 45 sec, fibrinogen < 1.0 g⋅L-1, platelet count < 100 × 10-9⋅L-1), use of long-acting oral anticoagulants that had not been appropriately discontinued, preoperative use of heparin infusion, major hemoglobinopathies, thalassemia or iron storage diseases, and a previous diagnosis of heparin-induced thrombocytopenia. Results are reported according to the Consolidated Standards of Reporting Trials guidelines.21
Heparin management
INTERVENTION GROUP
In the HMS Plus group, the initial heparin bolus before CPB was determined by HMS Plus calculation to achieve a theoretic target ACT point (480 sec) on the heparin dose responsiveness (HDR) curve of each patient or to achieve a target heparin concentration of 4 mg⋅kg-1, whichever required a higher dose of heparin. The calculation was based on the HMS Plus-estimated patient plasma volume and a HDR curve generated with the HDR cartridge (304-20POR, Medtronic, Inc., Minneapolis, MN, USA) containing known heparin concentrations of 0.0, 1.7, and 2.84 U⋅mL-1 performed before skin incision. Heparin concentration was then measured by the HMS Plus HPT cartridge four minutes after the initial heparin loading dose, then at ten minutes and every 30 min after commencing CPB. Concurrently, ACTs were measured by the Hemochron™ Signature Elite system (Werfen, Bedford, MA, USA). If ACT values by the Hemochron Signature Elite system were above 480 sec, further doses of heparin were given as dictated by HMS Plus to target a heparin concentration of 4 mg⋅kg-1 until the end of CPB. If the ACT fell below 480 sec, an additional heparin bolus was given as indicated by HMS Plus or independent of HMS Plus (based on individual perfusionist judgment) if the calculated additional heparin amount was zero. The initial protamine dose was determined by HMS Plus based on the last heparin concentration on CPB. Four minutes after protamine administration, residual heparin was measured and additional protamine was given as calculated by HMS Plus until none was detected.
CONTROL GROUP
In the control group, patients underwent heparin anticoagulation using a weight-based initial dose of 400 U⋅kg-1, aiming for an ACT of > 480 sec with the Hemochron Signature Elite system as per conventional management at our institution. Heparin–protamine titration measurements for heparin concentration were performed concurrently at the same time points as selected for the HMS Plus group. Further heparin doses (5,000 to 10,000 units) were to be given only when the ACT by the Hemochron Signature Elite system fell below 480 sec. After the cessation of CPB, heparin was reversed with protamine based on the initial heparin loading dose given pre bypass, using a ratio of 1 mg of protamine for every 100 units of heparin.
Clinical management
No changes were made to usual anesthetic or surgical care. Cardiopulmonary bypass circuits comprised a Cortiva coated Fusion® integrated oxygenator, BalanceTM coated tubing, and Balance coated AffinityTM centrifugal pump (all, Medtronic, Inc., Minneapolis, MN, USA). Standard nonpulsatile CPB with moderate hypothermia aiming for a core temperature of 34–36°C was used. The CPB circuit was primed with 1,000 mL of PLASMA-LYTE A solution (Baxter Corporation, Mississauga, ON, Canada), 25 g of mannitol, and 5,000 units of heparin. Patients received tranexamic acid as per institutional practice.22 Transfusion was managed in both groups according to departmental protocol, consistent with current guidelines.23 The red blood cell transfusion trigger was generally a hemoglobin level ≤ 70 g⋅dL-1 during CPB, ≤ 80 g⋅dL-1 in the post-CPB period, and ≤ 90 g⋅dL-1 for bleeding or unstable patients. Additional blood components (plasma, platelets, cryoprecipitate, fibrinogen concentrate) were transfused as per departmental protocol.24,25
Outcome measurements
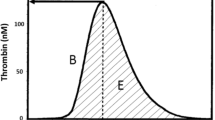
The primary outcome of interest was the difference in thrombin generation potential post-CPB compared with baseline, as assessed through CAT. Plasma samples were taken before heparinization for a baseline reading and ten minutes after reversal of heparin with protamine. All samples were obtained from preoperatively placed arterial lines discarding the first 10 mL of blood. Specimens was collected in sodium citrate tubes (0.13 M, 9 parts blood, 1 part sodium citrate) containing corn trypsin inhibitor (20 µg⋅mL-1) and centrifuged twice at 2,900 g for ten minutes at room temperature. Platelet-poor plasma was collected from the upper three quarters of the supernatant. Samples were prepared within 30 min of sampling and frozen for later batch analysis. Calibrated automated thrombography was performed as described by Hemker et al.17 with the standardization of reagents suggested by Dargaud et al.26 Calibrated automated thrombography assays were performed using a Thrombinoscope (Maastricht, The Netherlands) system based on a Fluoroskan Ascent® fluorometer (Thermo Fisher Scientific, Waltham, MA, USA). Citrated plasma samples (80 µL) were combined in wells of 96-well plates with 20 µL of trigger solution (Thrombinoscope PPP or PPP-low reagent; Stago Canada, Mississauga, ON, Canada) containing phospholipids (~4 pM) and tissue factor (TF) (~5 and ~1 pM TF, respectively).27,28,29,30 The plate was then moved to the fluorometer and 20 µL of FluCa solution added containing the fluorogenic substrate Z-Gly-Gly-Arg-AMC and CaCl2. The outcome of the thrombin generation reaction was observed by monitoring a thrombin-specific fluorogenic substrate.31
Rotational thromboelastometry (ROTEM®) was performed on the ROTEM delta instrument (Werfen, Bedford, MA, USA) using 300 μL citrated whole blood as previously described.32 Rotational thromboelastometry assays used were contact factor activation, contact factor activation with heparinase to neutralize the heparin effect, TF activation, and TF activation with platelet inhibition to assess fibrinogen status. These were performed at two time points—when the patient was rearmed to 36°C during CPB and ten minutes after the reversal of heparin with protamine following cessation of CPB. Platelet function analysis was performed with Plateletworks™ (Helena Laboratories, Beaumont, TX, USA) as per standard clinical practice in our institution as part of a blood transfusion algorithm that has been previously described.24
Secondary outcomes included intraoperative blood loss, chest drain output up to 72 hr, and transfusions. Intraoperative blood loss was recorded by subtracting inputs (irrigation volume, cell salvage anticoagulant) from losses (cell salvage volume collection, wet volume - dry volume sponges, suction canister volumes), which gave the total blood loss at the end of surgery. Postoperative blood loss for the first 24 hr was calculated from the chest drain output. Intraoperative transfusion of packed red cells, pooled platelets, plasma, cryoprecipitate, prothrombin concentrate, and fibrinogen concentrate intraoperatively and postoperatively was recorded.
Sample size
As noted in the above paragraph, our primary outcome of interest was the difference in thrombin generation post-CPB compared with baseline. Bosch et al. observed a change in mean (standard deviation [SD]) peak thrombin from 321 (63) nM pre CPB to 241 (36) nM post-CPB.33 Assuming a decrease in peak thrombin generation post-CPB of half (50%) the decrease observed in the control group in patients undergoing HMS Plus-based heparin management, to achieve a power of 0.80 with a two-sided alpha of 0.05, our approximate sample size was 50 patients per group, giving a total number of 100 patients.
Analysis
We utilized an intention-to-treat analysis approach. Continuous outcomes were compared between groups using Student’s t test for normally distributed variables and the Wilcoxon rank sum test for non-normally distributed variables. Categorical variables were compared using Fisher’s exact test for cell count values of 5 or less or the Chi square test otherwise.
We conducted additional exploratory analyses to better understand the impact of higher heparin concentrations on thrombin generation post-CPB. To better understand whether higher CPB heparin concentrations are associated with improved post-CPB thrombin generation regardless of study group, we stratified data based on quintiles of heparin concentration level maintained during CPB, with quintile 5 (the approximately 20% of patients with the highest average heparin concentrations during the first 120 min of CPB) maintaining an average heparin concentration on bypass of 4 mg⋅kg-1. We considered two-sided P values < 0.05 significant for the primary endpoint and two-sided P values < 0.001 for secondary comparisons. SAS University Edition (SAS Institute Inc., Cary, NC, USA) was used for analysis.
Results
All randomized patients were eligible for inclusion in the final analysis (Figure). The date of study initiation was 2 October 2017, with the first randomized patient sample collected on 16 October 2017. The final date of data collection for the primary endpoint was on 5 March 2019. There were no important differences in baseline characteristics between the intervention and control groups (Table 1).
In terms of the primary outcome, we observed no differences in thrombin generation parameters between the HMS Plus group and the control group. While all measures of thrombin generation showed significant changes post-CPB indicating a profound global impairment in thrombin generation (significant increases in the lag time and time to peak, with significant decreases in the endogenous thrombin potential [ETP] and peak thrombin), thrombin generation parameters post-CPB were not better in the HMS Plus group (Table 2). Similarly, we found no between-group differences with respect to other measures of hemostasis, including any ROTEM parameters (see Electronic Supplementary Material [ESM] eTable 1) or absolute platelet number or function (ESM eTable 2).
Although heparin concentrations were generally below the prespecified target threshold of 4 mg⋅kg-1, the HMS Plus group had significantly higher heparin dosing (P < 0.001), and maintained a higher average heparin concentration during CPB than the control group did (mean difference, -0.21; 95% confidence interval [CI], -0.42 to -0.01) (Table 3). Despite a significantly higher heparin level in the HMS Plus group before termination of CPB, the total protamine use and the protamine-to-heparin ratio in the HMS Plus group was lower than in the control group (Table 3), while both groups showed similar postprotamine heparin levels (Table 4).
Further analysis of heparin concentrations and ACT measurements during CPB (Table 4) showed that serial ACT measurements did not reflect the significant differences in heparin concentrations between the two groups, whose values were comparable in both groups at all time points. The discordance between ACT and heparin concentration was especially noticeable at 120 min of CPB, when the control group had a heparin concentration which was lower than the HMS Plus group by a mean difference of 1.1 mg⋅kg-1 (95% CI, -2.2 to 0.1), while the ACT values tended to be higher (Table 4).
With respect to secondary outcomes, at the time of patient arrival in the intensive care unit, both groups had significant reductions in hemoglobin level and absolute platelet count, and elevations in the prothrombin time and activated partial thromboplastin time compared with baseline, with no significant between-group differences (ESM eTable 2). There were no differences between the two groups in estimated blood loss, chest drain output up to 72 hr postoperatively (Table 2), or in transfusion of individual blood components (ESM eTable 3).
In the control group, heparin overdosing (where additional heparin was given with an ACT > 480 sec outside of the study protocol) occurred in 34% of participants ten minutes after initiation of CPB. Conversely, in the HMS Plus group, less than 6% of patients were overdosed or underdosed at any time (ESM eTable 4). In our exploratory analysis where patients were divided into quintiles of average heparin concentration achieved during the first 120 min of CPB, regardless of assigned study group, the quintile with the highest concentration consisted of 18 patients with a mean (SD) heparin concentration of 4.0 (0.3) mg⋅kg-1 (Table 5, ESM eTable 5). Examining thrombin generation parameters as measured by CAT using 5 pM of TF as a reagent, this group had significantly higher absolute ETP and peak thrombin generation, and shorter lag time and time to peak values than the remainder of the cohort did. A similar pattern was also observed under low TF conditions (1 pM), but no statistical significance was detected. We observed no differences in the estimated blood loss, chest drain output up to 72 hr postoperatively or in rates of transfusion compared with patients with lower heparin concentrations during CPB (Table 5).
Discussion
In the setting of cardiac surgery requiring CPB, maintaining a stable therapeutic heparin concentration is critical for effective inhibition of coagulation factor and thrombin consumption.34,35,36 Targeting a higher heparin concentration is advocated by several studies for its dose-related antithrombin activity35,36 and platelet inhibition during CPB.37,38 In this study, the HMS Plus group had significantly higher and more stable average heparin concentrations while on CPB. Nevertheless, our study was limited by a high rate of protocol violations in the control group (additional heparin boluses despite an ACT > 480 sec), which led to higher average heparin concentration while on CPB for the control group than our protocol would dictate. This would have minimized between-group differences in average heparin concentrations, and may partly explain why no major differences in outcomes were seen in the HMS Plus group compared with the conventional management group. Our data suggests that when used per-protocol, the HMS Plus system offers advantages over conventional ACT-guided management, particularly in relation to the stability of the average heparin concentration achieved while on CPB.
The protamine-to-heparin ratio is an important factor associated with postoperative bleeding and transfusion.39 In prior studies, a two-fold decrease in the protamine-to-heparin ratio was associated with significant improvements in platelet function.40 The majority of prior work showing favorable outcomes with HMS Plus-based management had significantly reduced protamine-to-heparin ratios, with a range of 0.6–0.7 in the HMS Plus group compared with 0.9–1.2 in the control group.13,14,41,42,43 The protamine-to-heparin ratio in our study was reduced to 0.6 in the HMS Plus group with no observed increase in bleeding or transfusion requirements. This suggests that the proper application of the HMS Plus system allows finer titration of protamine dosing, which may avoid the adverse effects associated with excessive protamine. Nevertheless, our control group protamine-to-heparin ratio of 0.7 is lower than that of the control groups in previously published studies, which may contribute to a smaller observed difference between the HMS Plus and control groups in our study. Additionally, our study was not powered to detect a difference in clinical bleeding or transfusion. Hence, while we did not observe a difference, a clinically relevant effect cannot be entirely excluded.
To better examine our hypothesis of whether higher heparin concentrations during CPB are associated with improved thrombin generation post-CPB, we conducted an exploratory analysis examining the quintile of patients (N = 18) with the highest heparin concentrations while on CPB, and compared them with the rest of the cohort. These patients had a median heparin concentration of 4.0 mg⋅kg-1 while on CPB, precisely the target heparin concentration of our original study protocol. In this group compared with the rest of the cohort, there was evidence of less impairment in thrombin generation post-CPB. This preservation of hemostatic function with higher heparin concentrations may be due to enhanced heparin antithrombin activity via antithrombin III, as well as enhanced TF pathway inhibition, which may play a larger role as CPB time is prolonged and antithrombin III is consumed.44
These results suggest that preventing thrombin generation while on CPB through more accurate heparin concentration maintenance can improve hemostasis and clinical bleeding outcomes post-CPB. Prior studies have suggested that HMS Plus reduces thrombin generation while on CPB,14,15 improves platelet preservation,14,40 and reduces blood product use.13 Nevertheless, these findings are not consistent, nor has the application of HMS Plus across studies been uniform. Individualized heparin target concentrations and dosing based on a HDR curve have potential benefits; however, inadequate anticoagulation using this approach has also been reported.45,46,47 To minimize these potential limitations, our study set a heparin target concentration of 4.0 mg⋅kg-1 when programing HMS Plus settings for heparin dose calculation. Having this particular setup, this study reported median heparin concentrations in the HMS Plus group as 3.5 mg⋅kg-1 for the majority of time points. Nevertheless, it is worth noting that subsequent heparin concentration measurements were conducted 30 min after additional heparin doses and immediately before subsequent heparin doses if required. Given the half-life of heparin, it is unsurprising that recorded measurements may have been lower than 4.0 mg⋅kg-1. In addition, the HPT cartridge used in this study has a measurement resolution of 0.5 mg⋅kg-1, with a maximum display value of 4.0 mg⋅kg-1. This may also contribute to the perceived lower than expected median heparin levels in the HMS Plus group. Despite the limitations of HMS Plus, this modified application of the HMS Plus system allowed for more reliable, improved heparin concentration management, with fewer fluctuations in heparin levels, thereby reducing the risk of inadequate anticoagulation.
Although our results indicate that the HMS Plus system may offer a better management strategy over ACT-guided management, the optimal heparin concentration to preserve thrombin function while on CPB is yet to be established. Few published studies comparing HMS Plus with conventional management have reported the heparin concentration levels maintained on CPB, and future studies establishing an evidence-based target heparin concentration range are warranted. Importantly, improvements in thrombin generation parameters and other laboratory measures of coagulation should be studied in relation to potential improvements in patient clinical outcomes.
Conclusion
Although HMS Plus-based anticoagulation management did not show significant benefits over conventional management in terms of reducing clinical bleeding, the modified use of the HMS Plus system in this study was more effective for achieving a stable heparin concentration during CPB and appropriate protamine dosing. Our results suggest higher heparin concentrations of 4 mg⋅kg-1 during CPB are associated with improved thrombin generation capacity after CPB, highlighting the potential benefits of using a targeted heparin concentration range to help preserve thrombin generation during cardiac surgical procedures.
References
Fitzgerald J, McMonnies R, Sharkey A, Gross PL, Karkouti K. Thrombin generation and bleeding in cardiac surgery: a clinical narrative review. Can J Anesth 2020; 67: 746–53.
Bartoszko J, Karkouti K. Managing the coagulopathy associated with cardiopulmonary bypass. J Thromb Haemost 2021; 19: 617–32.
De Somer F, Van Belleghem Y, Caes F, et al. Tissue factor as the main activator of the coagulation system during cardiopulmonary bypass. J Thorac Cardiovasc Surg 2002; 123: 951–8.
Höfer J, Fries D, Solomon C, Velik-Salchner C, Ausserer J. A snapshot of coagulopathy after cardiopulmonary bypass. Clin Appl Thromb Hemost 2016; 22: 505–11.
Bull BS, Huse WM, Brauer FS, Korpman RA. Heparin therapy during extracorporeal circulation. II. The use of a dose-response curve to individualize heparin and protamine dosage. J Thorac Cardiovasc Surg 1975; 69: 685–9.
Martindale SJ, Shayevitz JR, D'Errico C. The activated coagulation time: suitability for monitoring heparin effect and neutralization during pediatric cardiac surgery. J Cardiothorac Vasc Anesth 1996; 10: 458–63.
Despotis GJ, Gravlee G, Filos K, Levy J. Anticoagulation monitoring during cardiac surgery: a review of current and emerging techniques. Anesthesiology 1999; 91: 1122–51.
Thompson TZ, Kunak RL, Savage NM, Agarwal S, Chazelle J, Singh G. Intraoperative monitoring of heparin: comparison of activated coagulation time and whole blood heparin measurements by different point-of-care devices with heparin concentration by laboratory-performed plasma anti-xa assay. Lab Med 2019; 50: 348–56.
Li H, Serrick C, Rao V, Yip PM. A comparative analysis of four activated clotting time measurement devices in cardiac surgery with cardiopulmonary bypass. Perfusion 2021; 36: 610–9.
Bloemen S, Hemker HC, Al Dieri R. Large inter-individual variation of the pharmacodynamic effect of anticoagulant drugs on thrombin generation. Haematologica 2013; 98: 549–54.
Raymond PD, Ray MJ, Callen SN, Marsh NA. Heparin monitoring during cardiac surgery. Part 1: validation of whole-blood heparin concentration and activated clotting time. Perfusion 2003; 18: 269–76.
Despotis GJ, Summerfield AL, Joist JH, et al. Comparison of activated coagulation time and whole blood heparin measurements with laboratory plasma anti-Xa heparin concentration in patients having cardiac operations. J Thorac Cardiovasc Surg 1994; 108: 1076–82.
Despotis GJ, Joist JH, Hogue CW Jr, et al. The impact of heparin concentration and activated clotting time monitoring on blood conservation. A prospective, randomized evaluation in patients undergoing cardiac operation. J Thorac Cardiovasc Surg 1995; 110: 46–54.
Hofmann B, Bushnaq H, Kraus FB, et al. Immediate effects of individualized heparin and protamine management on hemostatic activation and platelet function in adult patients undergoing cardiac surgery with tranexamic acid antifibrinolytic therapy. Perfusion 2013; 28: 412–8.
Koster A, Fischer T, Praus M, et al. Hemostatic activation and inflammatory response during cardiopulmonary bypass: impact of heparin management. Anesthesiology 2002; 97: 837–41.
Koster A, Huebler S, Merkle F, et al. Heparin-level-based anticoagulation management during cardiopulmonary bypass: a pilot investigation on the effects of a half-dose aprotinin protocol on postoperative blood loss and hemostatic activation and inflammatory response. Anesth Analg 2004; 98: 285–90.
Hemker HC, Giesen P, Al Dieri R, et al. Calibrated automated thrombin generation measurement in clotting plasma. Pathophysiol Haemost Thromb 2003; 33: 4–15.
Figueiredo Duarte RC, Ferreira CN, Alves Rios DR, Dos Reis HJ, das Graças Carvalho M. Thrombin generation assays for global evaluation of the hemostatic system: perspectives and limitations. Rev Bras Hematol Hemoter 2017; 39: 259–65.
Coakley M, Hall JE, Evans C, et al. Assessment of thrombin generation measured before and after cardiopulmonary bypass surgery and its association with postoperative bleeding. J Thromb Haemost 2011; 9: 282–92.
Bosch Y, Al Dieri R, ten Cate H, et al. Preoperative thrombin generation is predictive for the risk of blood loss after cardiac surgery: a research article. J Cardiothorac Surg 2013. https://doi.org/10.1186/1749-8090-8-154.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother 2010; 1: 100–7.
Taam J, Yang QJ, Pang KS, et al. Current evidence and future directions of tranexamic acid use, efficacy, and dosing for major surgical procedures. J Cardiothorac Vasc Anesth 2020; 34: 782–90.
Raphael J, Mazer CD, Subramani S, et al. Society of Cardiovascular Anesthesiologists clinical practice improvement advisory for management of perioperative bleeding and hemostasis in cardiac surgery patients. J Cardiothorac Vasc Anesth 2019; 33: 2887–99.
Karkouti K, McCluskey SA, Callum J, et al. Evaluation of a novel transfusion algorithm employing point-of-care coagulation assays in cardiac surgery: a retrospective cohort study with interrupted time-series analysis. Anesthesiology 2015; 122: 560–70.
Raphael J, Mazer CD, Subramani S, et al. Society of Cardiovascular Anesthesiologists clinical practice improvement advisory for management of perioperative bleeding and hemostasis in cardiac surgery patients. Anesth Analg 2019; 129: 1209–21.
Dargaud Y, Luddington R, Gray E, et al. Effect of standardization and normalization on imprecision of calibrated automated thrombography: an international multicentre study. Br J Haematol 2007; 139: 303–9.
Duarte RCF, Ferreira CN, Rios DRA, Reis HJD, Carvalho MDG. Thrombin generation assays for global evaluation of the hemostatic system: perspectives and limitations. Rev Bras Hematol Hemoter 2017; 39: 259–65.
Keularts IM, Zivelin A, Seligsohn U, Hemker HC, Béguin S. The role of factor XI in thrombin generation induced by low concentrations of tissue factor. Thromb Haemost 2001; 85: 1060–5.
Brinkman HJ. Global assays and the management of oral anticoagulation. Thromb J 2015; https://doi.org/10.1186/s12959-015-0037-1.
Castoldi E, Rosing J. Thrombin generation tests. Thromb Res 2011; 127: S21–5.
Tripodi A. Thrombin generation assay and its application in the clinical laboratory. Clin Chem 2016; 62: 699–707.
Luddington RJ. Thrombelastography/thromboelastometry. Clin Lab Haematol 2005; 27: 81–90.
Bosch YP, Al Dieri R, ten Cate H, et al. Measurement of thrombin generation intra-operatively and its association with bleeding tendency after cardiac surgery. Thromb Res 2014; 133: 488–94.
Ofosu FA, Fernandez F, Gauthier D, Buchanan MR. Heparin cofactor II and other endogenous factors in the mediation of the antithrombotic and anticoagulant effects of heparin and dermatan sulfate. Semin Thromb Hemost 1985; 11: 133–7.
Gravlee GP, Haddon WS, Rothberger HK, et al. Heparin dosing and monitoring for cardiopulmonary bypass. A comparison of techniques with measurement of subclinical plasma coagulation. J Thorac Cardiovasc Surg 1990; 99: 518–27.
Hashimoto K, Yamagishi M, Sasaki T, Nakano M, Kurosawa H. Heparin and antithrombin III levels during cardiopulmonary bypass: correlation with subclinical plasma coagulation. Ann Thorac Surg 1994; 58: 799–804.
Gravlee GP, Rogers AT, Dudas LM, et al. Heparin management protocol for cardiopulmonary bypass influences postoperative heparin rebound but not bleeding. Anesthesiology 1992; 76: 393–401.
Fernandez F, N'Guyen P, Van Ryn J, Ofosu FA, Hirsh J, Buchanan MR. Hemorrhagic doses of heparin and other glycosaminoglycans induce a platelet defect. Thromb Res 1986; 43: 491–5.
Despotis GJ, Filos KS, Zoys TN, Hogue CW Jr, Spitznagel E, Lappas DG. Factors associated with excessive postoperative blood loss and hemostatic transfusion requirements: a multivariate analysis in cardiac surgical patients. Anesth Analg 1996; 82: 13–21.
Shigeta O, Kojima H, Hiramatsu Y, et al. Low-dose protamine based on heparin-protamine titration method reduces platelet dysfunction after cardiopulmonary bypass. J Thorac Cardiovasc Surg 1999; 118: 354–60.
Noui N, Zogheib E, Walczak K, et al. Anticoagulation monitoring during extracorporeal circulation with the Hepcon/HMS device. Perfusion 2012; 27: 214–20.
Despotis GJ, Joist JH, Hogue CW Jr, et al. More effective suppression of hemostatic system activation in patients undergoing cardiac surgery by heparin dosing based on heparin blood concentrations rather than ACT. Thromb Haemost 1996; 76: 902–8.
Pappalardo F, Franco A, Crescenzi G, De Simone F, Torracca L, Zangrillo A. Anticoagulation management in patients undergoing open heart surgery by activated clotting time and whole blood heparin concentration. Perfusion 2006; 21: 285–90.
Jeske W, Lormeau JC, Callas D, Iqbal O, Hoppensteadt D, Fareed J. Antithrombin III affinity dependence on the anticoagulant, antiprotease, and tissue factor pathway inhibitor actions of heparins. Semin Thromb Hemost 1995; 21: 193–200.
Gilly G, Trusheim J. Con: The Hepcon HMS should not be used instead of traditional activated clotting time to dose heparin and protamine for cardiac surgery requiring cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2016; 30: 1730–2.
Ichikawa J, Mori T, Kodaka M, Nishiyama K, Ozaki M, Komori M. Changes in heparin dose response slope during cardiac surgery: possible result in inaccuracy in predicting heparin bolus dose requirement to achieve target ACT. Perfusion 2017; 32: 474–80.
Garvin S, FitzGerald DC, Despotis G, Shekar P, Body SC. Heparin concentration-based anticoagulation for cardiac surgery fails to reliably predict heparin bolus dose requirements. Anesth Analg 2010; 111: 849–55.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453–7.
Author contributions
All authors contributed to all aspects of this manuscript, including study conception and design; acquisition, analysis, and interpretation of data; and drafting the article.
Disclosures
Keyvan Karkouti, MD, MSc has received research support, honoraria, or consultancy for speaking engagements from Octapharma, Instrumentation Laboratory/Werfen, and Bayer.
Funding statement
The original randomized controlled trial in which this observational study was nested was in part supported by Medtronic, which provided the HMS Plus Hemostasis Management System and all of the related disposables. No additional funding or support was obtained for the purposes of this nested observational study. Keyvan Karkouti, MD, MSc is in part supported by a merit award from the Department of Anesthesiology and Pain Medicine, University of Toronto, Toronto, ON, Canada. Justyna Bartoszko, MD, MSc is in part supported by a merit award from the Department of Anesthesiology and Pain Medicine, University of Toronto, Toronto, ON, Canada.
Editorial responsibility
This submission was handled by Dr. Stephan K. W. Schwarz, Editor-in-Chief, Canadian Journal of Anesthesia/Journal canadien d’anesthésie.
Author information
Authors and Affiliations
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, H., Bartoszko, J., Serrick, C. et al. Titrated versus conventional anticoagulation management for thrombin generation in cardiac surgery: a randomized controlled trial. Can J Anesth/J Can Anesth 69, 1117–1128 (2022). https://doi.org/10.1007/s12630-022-02278-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-022-02278-1