Abstract
Purpose
Desflurane has the lowest solubility of currently available volatile anesthetics and may allow for more rapid emergence and recovery compared with sevoflurane. Nevertheless, after volatile induction with sevoflurane, it has not been determined whether the use of desflurane provides faster emergence and recovery. The present study aimed to elucidate the effects of changing from sevoflurane to desflurane during the early part of anesthesia.
Methods
Fifty-two patients who were scheduled for vitreous surgery with general anesthesia were enrolled in this randomized controlled study. Anesthesia was induced with volatile induction consisting of 100% oxygen (6 L·min−1) and 5% sevoflurane. For anesthesia maintenance, patients were randomized to receive 1-2% sevoflurane or 3-6% desflurane. In the desflurane group, the anesthetic agent was changed from sevoflurane to desflurane within five minutes following endotracheal intubation. After surgery, we assessed the following endpoints: the times from discontinuing volatile anesthetics to eye opening, obeying the command to squeeze the investigator’s hand, tracheal extubation, and orientation to the patients’ full name, date, and place.
Results
Emergence and recovery were significantly faster in the desflurane group than in the sevoflurane group in times to mean (SD) eye opening [6.5 (2.9) vs 10.1(3.0) min, respectively; mean difference, 3.6 min; 95% confidence interval (CI), 1.9 to 5.3; P < 0.001], obeying commands [6.6 (2.7) vs 10.1 (3.1) min, respectively; mean difference, 3.5 min; 95% CI, 1.9 to 5.2; P < 0.001], and tracheal extubation [7.0 (2.5) vs 10.6 (3.0) min, respectively; mean difference, 3.6 min; 95% CI, 1.9 to 5.1; P < 0.001]. Similarly, the times from discontinuation of volatile anesthetics to orientation to the patients’ full name, date, and place were significantly shorter in the desflurane group compared with the sevoflurane group. There were no significant differences between groups on a 100-mm visual analogue scale assessing postoperative nausea and vomiting, eye pain, and patient satisfaction regarding anesthesia.
Conclusion
Changing the anesthetic agent from sevoflurane to desflurane after sevoflurane induction provides faster emergence and recovery compared with sevoflurane anesthesia. This study protocol was registered at http://www.umin.ac.jp/ctr/index.htm, (UMIN000009941).
Résumé
Objectif
Le desflurane est l’agent dont la solubilité est la plus faible parmi les agents anesthésiques volatils actuellement disponibles sur le marché; cette propriété pourrait favoriser un réveil et une récupération plus rapides par rapport au sévoflurane. Toutefois, après une induction volatile à base de sévoflurane, il n’a pas encore été déterminé si l’utilisation de desflurane procurait un réveil et une récupération plus rapides. L’objectif de cette étude était d’élucider les effets d’un remplacement du sévoflurane par le desflurane pendant la première partie de l’anesthésie.
Méthode
Cinquante-deux patients devant subir une vitrectomie sous anesthésie générale ont été enrôlés dans cette étude randomisée contrôlée. L’anesthésie a été initiée par une induction volatile composée de 100 % d’oxygène (6 L·min−1) et de 5 % de sévoflurane. Pour maintenir l’anesthésie, on a randomisé les patients à recevoir soit du sévoflurane à 1-2 % ou du desflurane à 3-6 %. Dans le groupe desflurane, le sévoflurane a été remplacé par du desflurane dans les cinq minutes suivant l’intubation endotrachéale. Après la chirurgie, nous avons évalué les critères suivants: les temps entre l’arrêt des agents volatils et l’ouverture des yeux, le respect de la consigne de serrer la main du chercheur, l’extubation trachéale et l’orientation jusqu’à la déclaration du nom complet du patient, de la date et du lieu.
Résultats
Le réveil et la récupération étaient significativement plus rapides dans le groupe desflurane que dans le groupe sévoflurane en matière de temps moyen (ÉT) jusqu’à ouverture des yeux [6,5 (2,9) vs 10,1(3,0) min, respectivement; différence moyenne, 3,6 min; intervalle de confiance (IC) 95 %, 1,9 à 5,3; P < 0,001], le respect d’une consigne [6,6 (2,7) vs 10,1 (3,1) min, respectivement; différence moyenne, 3,5 min; IC 95 %, 1,9 à 5,2; P < 0,001] et l’extubation trachéale [7,0 (2,5) vs 10,6 (3,0) min, respectivement; différence moyenne, 3,6 min; IC 95 %, 1,9 à 5,1; P < 0,001]. De la même façon, les temps depuis l’arrêt des anesthésiques volatils jusqu’à l’orientation jusqu’à la déclaration du nom complet du patient, de la date et du lieu étaient significativement plus courts dans le groupe desflurane que dans le groupe sévoflurane. Aucune différence significative n’a été observée entre les groupes sur une échelle visuelle analogique de 100 mm évaluant les nausées et vomissements postopératoires, la douleur oculaire et la satisfaction des patients concernant leur anesthésie.
Conclusion
Le remplacement du sévoflurane par du desflurane après une induction au sévoflurane procure un réveil et une récupération plus rapides par rapport à une anesthésie au sévoflurane. Ce protocole d’étude a été enregistré au http://www.umin.ac.jp/ctr/index.htm, (UMIN000009941).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Volatile anesthetics such as sevoflurane and desflurane are widely used for general anesthesia because of their convenience and predictable therapeutic effects.1 Maintaining anesthesia with sevoflurane in day surgery is popular because it has a relatively lower solubility than other volatile anesthetics and allows for rapid emergence and recovery.2 Additionally, sevoflurane provides smooth volatile induction due to its lack of airway irritation, and it is often used as an induction agent.3-5 Desflurane has the lowest solubility of currently available volatile anesthetics,6 which may allow for more rapid emergence and recovery than sevoflurane.7 Additionally, the use of desflurane is associated with more predictable emergence and recovery than sevoflurane.8 Nevertheless, unlike sevoflurane, the use of desflurane for volatile induction is limited because of airway irritation;9 therefore, when desflurane is employed to maintain anesthesia, it is initiated after the induction with other anesthetic agents. Although previous studies have reported faster emergence with desflurane than with sevoflurane after induction with intravenous anesthetics (e.g., propofol and thiopental),10-15 few studies have compared emergence and recovery with desflurane vs with sevoflurane after inhalational induction. It is still unknown whether desflurane provides faster emergence and recovery than sevoflurane even after volatile induction with sevoflurane.
This randomized controlled study was designed to elucidate the effects of changing from sevoflurane to desflurane following sevoflurane induction on emergence and recovery (e.g., times to eye opening, tracheal extubation, and orientation to name, date, and place). We hypothesized that changing the anesthetic agent from sevoflurane to desflurane during the early phase of anesthesia improves emergence and recovery.
Methods
This study was approved by the Kushiro Red Cross Hospital Institutional Ethical Committee on February 27, 2013. Kushiro Red Cross Hospital is a secondary care centre with 489 inpatient beds, and anesthesiologists of Asahikawa Medical University provide anesthesia for more than 2,000 operations each year.
An investigator enrolled 52 patients who were scheduled for vitreous surgery at Kushiro Red Cross Hospital. All the patients provided their written informed consent to participate in the study. The inclusion criteria were patients aged over 20 years and American Society of Anesthesiologists physical status I-III. The exclusion criteria were patient refusal, pregnancy, clinically significant disorders (e.g., cardiovascular, hepatorenal, pulmonary, or neurologic), and a history of alcohol or drug abuse within three months of surgery. Patients were randomly assigned to either the sevoflurane group or the desflurane group (allocation ratio 1:1) via a computer-generated randomization table that was accessed by an independent investigator who was not involved in data collection. The randomization result was sealed in an opaque envelope, and only the attending anesthesiologist was allowed to open the envelope in the absence of data collectors. The randomization process was stratified by sex and blocked (block size = 2).
No pre-anesthetic medication was administered to the patients. Upon their arrival at the operating room, standard monitoring devices were placed, including electrocardiography, pulse oximetry, and automated blood pressure (every five minutes). Also, each patient’s bispectral index (BIS) was monitored with an A-2000™ electroencephalogram monitor (Aspect Medical Systems, Natick, MA, USA). Volatile anesthetic concentrations were determined using an IntelliVue M1019A G5 gas module (Philips Healthcare, Andover, MA, USA).
An unblinded anesthesiologist administered the study medication to each patient after the administration of oxygen and determination of baseline values for the BIS and hemodynamic variables. Anesthesia was induced with 5% sevoflurane in oxygen (6 L·min−1), and a continuous infusion of remifentanil (0.3 μg·kg−1·min−1) was started after loss of consciousness. Rocuronium (0.6 mg·kg−1) was administered to achieve muscle relaxation before endotracheal intubation. Mechanical ventilation was controlled to maintain end-tidal carbon dioxide at 32-35 mmHg. For anesthesia maintenance, patients were randomly assigned to receive either sevoflurane 1-2% end-tidal or desflurane 3-6% end-tidal with air (1 L·min−1) and oxygen (1 L·min−1). All the patients were blinded to their group assignment. In the desflurane group, the administration of sevoflurane was discontinued, and the anesthetic was immediately changed to desflurane within five minutes after endotracheal intubation. During the procedure, the sevoflurane or desflurane anesthetic was titrated to an intraoperative BIS range of 40-50, and no attempt was made to decrease the anesthetic dosing until the discontinuation of volatile anesthetic after surgery. The continuous infusion of remifentanil (0.1 μg·kg−1·min−1) was discontinued approximately 15 min before the end of surgery. Additional rocuronium was administered as appropriate during surgery, and a residual neuromuscular block was antagonized with 2 mg·kg−1 of sugammadex after surgery.
Boluses of ephedrine 5-10 mg iv were administered to treat hypotension, defined as a > 30% decrease in systolic blood pressure from the baseline value. Bradycardia (heart rate < 50 beats·min−1) was treated with 0.5 mg of atropine if needed. Elevations in the heart rate and systolic blood pressure (> 30% of baseline values) were treated with boluses of remifentanil (1 μg·kg−1) iv.
After the neuromuscular block was reversed, administration of the volatile anesthetic was discontinued and the rate of fresh gas inflow was changed to 6 L·min−1 of oxygen (Time 0). If there were less than ten minutes from discontinuing remifentanil to the end of surgery, then volatile anesthetic administration was discontinued at least ten minutes afterwards to minimize the influence of opioids on the recovery profiles. Controlled ventilation was maintained until the patient’s first spontaneous breath or cough reflex, followed by manually assisted lung ventilation. Immediately after the attending anesthesiologist covered the gas analyzer and started a stopwatch at Time 0, the anesthesiologist summoned the second anesthesiologist (now blinded due to the covered vaporizer) into the operating room and handed over the stopwatch for assessment of emergence and recovery times. This second blinded anesthesiologist assessed the times from Time 0 to eye opening in response to verbal stimulation, obeying a command to squeeze the investigator’s hand, tracheal extubation, and orientation to the patient’s full name, date, and place. Verbal stimulation was provided by loudly calling the patient’s last name every 20 sec. The patient’s trachea was extubated upon following commands and reaching a respiratory rate of at least 8 breaths·min−1. The duration of surgery and anesthesia (from the start of induction to Time 0) was also recorded.
Upon the patients’ arrival at the ward, a blinded anesthesiologist recorded postoperative nausea and vomiting (PONV) and eye pain scores at zero, 30, and 60 min, and 24 hr on a 100-mm visual analogue scale (VAS) (0 mm = no nausea or no pain; 100 mm = worst possible nausea or worst possible pain). Patients routinely took loxoprofen (60 mg orally every 8 hr) after surgery for eye pain. At the 24-hr postoperative visit, the patients were asked a VAS satisfaction question regarding anesthesia (0 mm = least satisfied; 100 mm = most satisfied). Additionally, the patients were asked whether they had experienced awareness during the anesthesia.
On the basis of preliminary data on time to eye opening, the sample size was calculated as 21 patients per group to give an α value of 0.05 and a β value of 0.2, assuming a three-minute mean difference between the groups [estimated standard deviation (SD) of 3.3 min]. To account for dropouts, we set the total sample size of patients to undergo randomization at n = 52. Student’s t test was performed for continuous variables, and categorical data were analyzed by the Fisher’s exact test. All reported P values are two sided. Statistical analyses were performed using SPSS® version 22 (IBM, Armonk, NY, USA). Data are expressed as mean (SD) except where stated otherwise.
Results
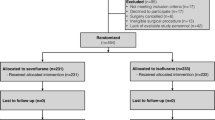
Fifty-two patients were randomized to receive either sevoflurane (n = 26) or desflurane (n = 26) for the maintenance of anesthesia. Two patients (one in each group) were excluded because of protocol violations, leading to a final n = 25 patients in each group (Fig. 1).
The two groups had comparable baseline characteristics and intraoperative data (Table 1). Adverse airway events during volatile induction, such as coughing and breath-holding, were recorded in both groups; however, they were mild and easily treated by anesthesiologists (Table 1). None of the patients had laryngospasm or arterial oxygen desaturation during volatile induction. The BIS in both groups continued to be stable at 40-50 during surgery and was similar at Time 0 (Table 1). Three patients in the sevoflurane group and two in the desflurane group needed additional intraoperative boluses of remifentanil; however, the total amount of intravenous remifentanil was similar in the two groups (Table 1).
The mean (SD) time from Time 0 to eye opening was 10.1 (3.0) min vs 6.5 (2.9) min for patients in the sevoflurane group vs the desflurane group, respectively (mean difference, 3.6 min; 95% confidence interval [CI], 1.9 to 5.3; P < 0.001), which was significantly different (Table 2). Similarly, the times from Time 0 to hand-squeezing, tracheal extubation, and orientation to the patients’ full name, date, and place were significantly shorter in the desflurane group than in the sevoflurane group (Table 2). Moreover, the SDs of the mean times to orientation to date and place were narrower in the desflurane group than in the sevoflurane group, suggesting that recovery times after desflurane anesthesia are less variable than sevoflurane (Table 2). No significant differences were observed between the groups with respect to the 100-mm VAS satisfaction question about anesthesia at the 24-hr postoperative interview. Patients in both groups were highly satisfied with their anesthetic experience (Table 2). No patients experienced awareness during anesthesia. Five patients in the sevoflurane group spontaneously complained of a postoperative unpleasant breath odour at the 24-hr postoperative interview; whereas, one patient in the desflurane group reported an unpleasant odour, which was not significantly different (P = 0.19).
Fig. 2 shows the 100-mm VAS PONV scores at 0, 30, and 60 min, and 24 hr after arrival to the ward, and there was no significant difference between the groups. The 100-mm VAS eye pain scores in the two groups were not significantly different (Fig. 3).
Discussion
In the present study, the times from discontinuation of volatile anesthetics to eye opening, hand squeezing, tracheal extubation, and orientation to the patients’ full name, date, and place were significantly shorter in the desflurane group than in the sevoflurane group. The times to orientation to the date and place were less variable in the desflurane group than in the sevoflurane group. These findings support our hypothesis that changing the anesthetic agent from sevoflurane to desflurane improves emergence and recovery from general anesthesia, even after sevoflurane induction.
Previous studies in children have reported faster emergence with desflurane than with sevoflurane after volatile induction with sevoflurane.16,17 Our results are consistent with these findings despite the fact that these previous studies differed in their use of nitrous oxide for anesthesia induction and maintenance. Nevertheless, few studies have compared anesthesia emergence times between desflurane and sevoflurane after volatile induction in adults. Furthermore, it is unknown whether changing the anesthetic agent from sevoflurane to desflurane improves the recovery profile after general anesthesia. This is most likely due to the young age of the participants in prior studies, which prevented precise measurements of recovery times.16,17 The times in our study from discontinuation of volatile anesthetics to orientation to the patients’ full name, date, and place were significantly shorter in the desflurane group than in the sevoflurane group, which suggests that changing from sevoflurane to desflurane permits faster recovery than sevoflurane anesthesia, even after sevoflurane induction. In addition, the time trend in recovery events differed between the two groups. The time intervals between tracheal extubation and orientation to the patients’ full name were similar (1 min in the sevoflurane group vs 1.3 min in the desflurane group). Nevertheless, the times between tracheal extubation and orientation to the date and place were longer in the sevoflurane group (5.4 min and 4.6 min, respectively) than in the desflurane group (2.4 min and 2.4 min, respectively). These results indicate that maintenance with sevoflurane delays orientation to the date and place after tracheal extubation compared with maintenance with desflurane. Additionally, the times to orientation to the date and place were less variable in the desflurane group, suggesting that changing from sevoflurane to desflurane provides more predictable recovery compared with sevoflurane anesthesia. Patients’ rapid and predictable recovery after desflurane anesthesia in our study is consistent with previous studies,8,18 and our findings show that volatile induction with sevoflurane does not alter the favourable pharmacological characteristics of desflurane. The rapid and predictable recovery that results from changing from sevoflurane to desflurane may improve patient turnover in the operating room and may be cost-effective.8
Previous studies have attempted to combine the advantages of different volatile anesthetics. Several studies have investigated the effects of changing from isoflurane to desflurane during the latter part of anesthesia,19-21 and Kang et al. have reported that changing from enflurane to desflurane effectively improved recovery from general anesthesia.22 Nevertheless, few studies have reported the advantages of changing from sevoflurane to desflurane. In the present study, none of the patients experienced severe adverse events during volatile induction, and changing from sevoflurane to desflurane provided fast emergence and recovery. Therefore, this technique can achieve both smooth induction and rapid recovery without pain on intravenous catheter insertion or injection of intravenous anesthetics such as propofol.
In the present study, there were no significant differences in PONV scores between the sevoflurane group and the desflurane group, which is consistent with previous studies.23,24 Eye pain scores did not differ significantly between the groups in our study, which is also in accordance with previous studies.25,26 These results suggest that there are no significant differences in the degree of PONV or postoperative pain between patients receiving sevoflurane or desflurane.
Interestingly, five patients in the sevoflurane group complained of a postoperative unpleasant breath odour at the 24-hr postoperative interview, whereas only one patient in the desflurane group reported an unpleasant odour. The odour was likely caused by sevoflurane, as all the patients who complained of this odour noticed the presence of a similar odour during volatile induction. These results can be attributed to the slower elimination kinetics of sevoflurane compared with desflurane.27,28 Although there was no significant difference between groups on the 100-mm VAS satisfaction question on anesthesia, postoperative breath odour may be unpleasant for patients.
In this changing technique from sevoflurane to desflurane, the patients’ awareness during the changing period may concern anesthesiologists. The BIS never exceeded 60 during the changing period in the desflurane group; awareness during anesthesia is unlikely when the BIS is < 60.29,30 Furthermore, none of the patients experienced awareness during anesthesia, suggesting that changing from sevoflurane to desflurane during the early part of anesthesia does not cause awareness during the changing period. The low solubility of desflurane may provide faster wash-in compared with the wash-out of sevoflurane, maintaining an adequate depth of anesthesia during the changing period.31 Nevertheless, the gas analyzer may not always indicate accurate concentrations of volatile anesthetics when more than one agent is present; therefore, the use of a BIS monitor is recommended when changing from sevoflurane to desflurane.
Our study has several limitations. First, we did not attempt to decrease the anesthetic dose until discontinuation of the volatile anesthetic after surgery. Titration of the anesthetic concentration to achieve a higher BIS (e.g., 55 or 60) towards the end of surgery may affect the times for emergence and recovery. Second, we did not administer opioids except for remifentanil, an ultra-short-acting opioid.32 Additionally, the continuous infusion of remifentanil was discontinued at least ten minutes before Time 0 to minimize its influence on emergence and recovery. The administration of longer lasting opioids, such as fentanyl and alfentanil, or remifentanil immediately before the end of surgery may affect the efficacy of the changing technique.33,34 Third, regarding the recovery from anesthesia, we assessed only the early recovery, such as the times to orientation to the patients’ full name, date, and place. Further studies of late recovery, such as the times to discharge from the hospital and full normal activity, are necessary to evaluate the long-term effects of the changing technique on the recovery profile.
In conclusion, we found that changing the anesthetic agent from sevoflurane to desflurane after volatile induction with sevoflurane provides faster emergence and recovery compared with sevoflurane anesthesia. This changing technique allows for both smooth induction and rapid recovery, achieving high patient satisfaction.
References
Aranake A, Mashour GA, Avidan MS. Minimum alveolar concentration: ongoing relevance and clinical utility. Anaesthesia 2013; 68: 512-22.
Ghatge S, Lee J, Smith I. Sevoflurane: an ideal agent for adult day-case anesthesia? Acta Anaesthesiol Scand 2003; 47: 917-31.
Bulte CS, Slikkerveer J, Kamp O, et al. General anesthesia with sevoflurane decreases myocardial blood volume and hyperemic blood flow in healthy humans. Anesth Analg 2013; 116: 767-74.
Lee JR, Kim SD, Kim CS, Yoon TG, Kim HS. Minimum alveolar concentration of sevoflurane for laryngeal mask airway removal in anesthetized children. Anesth Analg 2007; 104: 528-31.
Young CJ, Apfelbaum JL. Inhalational anesthetics: desflurane and sevoflurane. J Clin Anesth 1995; 7: 564-77.
Yasuda N, Targ AG, Eger EI 2nd. Solubility of I-653, sevoflurane, isoflurane, and halothane in human tissues. Anesth Analg 1989; 69: 370-3.
Gupta A, Stierer T, Zuckerman R, Sakima N, Parker SD, Fleisher LA. Comparison of recovery profile after ambulatory anesthesia with propofol, isoflurane, sevoflurane and desflurane: a systematic review. Anesth Analg 2004; 98: 632-41.
Jakobsson J. Desflurane: a clinical update of a third-generation inhaled anaesthetic. Acta Anaesthesiol Scand 2012; 56: 420-32.
Zwass MS, Fisher DM, Welborn LG, et al. Induction and maintenance characteristics of anesthesia with desflurane and nitrous oxide in infants and children. Anesthesiology 1992; 76: 373-8.
Mahmoud NA, Rose DJ, Laurence AS. Desflurane or sevoflurane for gynaecological day-case anaesthesia with spontaneous respiration? Anaesthesia 2001; 56: 171-4.
Strum EM, Szenohradszki J, Kaufman WA, Anthone GJ, Manz IL, Lumb PD. Emergence and recovery characteristics of desflurane versus sevoflurane in morbidly obese adult surgical patients: a prospective, randomized study. Anesth Analg 2004; 99: 1848-53.
Demirbilek S, Togal T, Cicek M, Aslan U, Sizanli E, Ersoy MO. Effects of fentanyl on the incidence of emergence agitation in children receiving desflurane or sevoflurane anaesthesia. Eur J Anaesthesiol 2004; 21: 538-42.
Magni G, Rosa IL, Melillo G, Savio A, Rosa G. A comparison between sevoflurane and desflurane anesthesia in patients undergoing craniotomy for supratentorial intracranial surgery. Anesth Analg 2009; 109: 567-71.
White PF, Tang J, Wender RH, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg 2009; 109: 387-93.
Rortgen D, Kloos J, Fries M, et al. Comparison of early cognitive function and recovery after desflurane or sevoflurane anaesthesia in the elderly: a double-blinded randomized controlled trial. Br J Anaesth 2010; 104: 167-74.
Cohen IT, Finkel JC, Hannallah RS, Hummer KA, Patel KM. The effect of fentanyl on the emergence characteristics after desflurane or sevoflurane anesthesia in children. Anesth Analg 2002; 94: 1178-81.
Sethi S, Ghai B, Ram J, Wig J. Postoperative emergence delirium in pediatric patients undergoing cataract surgery—a comparison of desflurane and sevoflurane. Paediatr Anaesth 2013; 23: 1131-7.
McKay RE, Malhotra A, Cakmakkaya OS, Hall KT, McKay WR, Apfel CC. Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth 2010; 104: 175-82.
Neumann MA, Weiskopf RB, Gong DH, Eger EI 2nd, Ionescu P. Changing from isoflurane to desflurane toward the end of anesthesia does not accelerate recovery in humans. Anesthesiology 1998; 88: 914-21.
Kang H, Cha SM, Park SG, et al. The effects of changing from isoflurane to desflurane on the recovery profile during the latter part of anesthesia. Acta Med Okayama 2010; 64: 307-16.
Gong DH, Weiskopf RB, Neumann MA, Laster MJ, Eger EI 2nd. In rats breathing from a nonrebreathing system, substitution of desflurane for isoflurane toward the end of anesthesia incompletely restores the time of recovery toward that of desflurane. Anesth Analg 1998; 86: 198-201.
Kang H, Park SG, Baek CW, et al. The effect on the recovery profile of a change from enflurane to desflurane during the latter part of anaesthesia. J Int Med Res 2008; 36: 951-63.
Chen X, Zhao M, White PF, et al. The recovery of cognitive function after general anesthesia in elderly patients: a comparison of desflurane and sevoflurane. Anesth Analg 2001; 93: 1489-94.
Saros GB, Doolke A, Anderson RE, Jakobsson JG. Desflurane vs. sevoflurane as the main inhaled anaesthetic for spontaneous breathing via a laryngeal mask for varicose vein day surgery: a prospective randomized study. Acta Anaesthesiol Scand 2006; 50: 549-52.
Vallejo MC, Sah N, Phelps AL, O’Donnell J, Romeo RC. Desflurane versus sevoflurane for laparoscopic gastroplasty in morbidly obese patients. J Clin Anesth 2007; 19: 3-8.
Fassoulaki A, Melemeni A, Paraskeva A, Siafaka I, Sarantopoulos C. Postoperative pain and analgesic requirements after anesthesia with sevoflurane, desflurane or propofol. Anesth Analg 2008; 107: 1715-9.
Bailey JM. Context-sensitive half-times and other decrement times of inhaled anesthetics. Anesth Analg 1997; 85: 681-6.
Lockwood G. Theoretical context-sensitive elimination times for inhalation anaesthetics. Br J Anaesth 2010; 104: 648-55.
Myles PS, Leslie K, McNeil J, Forbes A, Chan MT. Bispectral index monitoring to prevent awareness during anaesthesia: the B-Aware randomised controlled trial. Lancet 2004; 363: 1757-63.
Ekman A, Lindholm ML, Lennmarken C, Sandin R. Reduction in the incidence of awareness using BIS monitoring. Acta Anaesthesiol Scand 2004; 48: 20-6.
La Colla L, Albertin A, La Colla G, Mangano A. Faster wash-out and recovery for desflurane vs sevoflurane in morbidly obese patients when no premedication is used. Br J Anaesth 2007; 99: 353-8.
Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia 2007; 62: 1266-80.
Glass PS, Hardman D, Kamiyama Y, et al. Preliminary pharmacokinetics and pharmacodynamics of an ultra-short-acting opioid: remifentanil (GI87084B). Anesth Analg 1993; 77: 1031-40.
Glass PS. Remifentanil: a new opioid. J Clin Anesth 1995; 7: 558-63.
Acknowledgements
The authors thank the staff at Kushiro Red Cross Hospital for their assistance in conducting this study. We also express our thanks to Chie Asakura MD, Department of Anesthesiology and Critical Care Medicine, Asahikawa Medical University, for language revision of the manuscript.
Funding
No external funding and no competing interests declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Ikuomi Mikuni, Shuto Harada, Ryuta Yakushiji, and Hiroshi Iwasaki helped design the study. Ikuomi Mikuni, Shuto Harada, and Ryuta Yakushiji helped collect the data. Ikuomi Mikuni analyzed the data. Shuto Harada and Ryuta Yakushiji helped conduct the study. Ikuomi Mikuni and Hiroshi Iwasaki helped prepare the manuscript. All authors contributed to the final manuscript.
Rights and permissions
About this article
Cite this article
Mikuni, I., Harada, S., Yakushiji, R. et al. Effects of changing from sevoflurane to desflurane on the recovery profile after sevoflurane induction: a randomized controlled study. Can J Anesth/J Can Anesth 63, 290–297 (2016). https://doi.org/10.1007/s12630-015-0514-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0514-9