Abstract
Sevoflurane is shown to be safe and effective in pediatric echocardiography. This study explores the optimum level in pediatric echocardiography. One hundred and twenty children, with an age range of 35 days–3 years, were included in this study. The children with severe cyanotic congenital heart disease or severe pneumonia, which was Grade I or II according to the American College of Physicians Guideline Grading, were excluded. All children received the anesthesia with sevoflurane. The inhalation anesthesia level decreased from 2.5 to 1.0 %, with a decrement of 0.5 %. The induction time (T0), echocardiography time (T1), and time to awakening (T2) in each child were recorded, and the changes in the blood pressure, heart rate, breath, and oxygen saturation in each child were also monitored. The Ramsay scale scoring during anesthesia and the case number of failure in echocardiography in each group were also recorded. When the level of sevoflurane inhalation was maintained at 1.0 %, the childrens’ scores were low, including 8 incompliant children, and p < 0.05 in comparison with other groups. The scores increased as the sevoflurane inhalation level increased. When the sevoflurane inhalation increased to 1.5 %, the children could sleep with stable blood pressure, and no dysphoria occurred during the echocardiography. When the sevoflurane inhalation level increased to 2.5 %, the Ramsay scores did not increase. However, the T2 significantly increased (p < 0.05). The blood pressure and heart rate in each group did not change significantly. With the premise of safety and efficacy in children, the optimum level of sevoflurane in pediatric echocardiography was 1.5–2.0 %.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Generally, a child is asked to keep still when undergoing pediatric echocardiography so that satisfactory imaging can be obtained. However, most children have poor self-control, and echocardiography can be completed only after the child is sedated. Inhalation anesthetic is a commonly used anesthesia in children. Sevoflurane is an inhaled anesthetic with high safety, short induction, and awakening time. It does not increase respiratory secretions, and has few adverse effects on hemodynamic indicators, such as heart rate, and heart rhythm. Therefore, it is safe to use in pediatric outpatient examinations. This study investigates the use inhaled sevoflurane in pediatric echocardiography. The objective was to explore the optimum level of sevoflurane in pediatric outpatient echocardiography and provide evidences for use in clinical examination.
Materials and Methods
This study was approved by Medical Ethics Committee. All legal guardians of the included children had signed the informed consent. One hundred and twenty children, who were classified as ASA scale Grade I to II, were chosen to receive pediatric echocardiography. The age range was 35 days–3 years. No child had the history of respiratory tract infection, liver and kidney diseases, psychiatry, and neuropathy. These children were assigned into 4 groups: inhalation of 1.0 % sevoflurane (1.0 % group), inhalation of 1.5 % sevoflurane (1.5 % group), inhalation of 2.0 % sevoflurane (2.0 % group), and inhalation of 2.5 % sevoflurane (2.5 % group). Table 1 presents the general information of these children.
Sedation and anesthesia and the methods
The children fasted for 2 h before the echocardiography as routine and did not receive pre-anesthesia medication. The dedicated evaporation tank for sevoflurane (Sevoflurane Drager Vapor2000; Baxter) was used during anesthesia. Furthermore, an attending anesthetist provided anesthesia to the children.
The air escape valve was opened, and the manually controlled breathing bag was emptied before anesthesia. The level of sevoflurane was set at 8 % and the oxygen flow rate at 6 L/min. The breathing bag was relaxed and allowed to be filled with sevoflurane. The child’s mouth and nose were covered with an appropriate mask as required for tidal volume measurement, until the child had no eyelash reflex (induction time), and had no body movement when his/her earlobe was pinched (as the criteria of qualification for echocardiography). The level was adjusted at 2.5, 2.0, 1.5, and 1.0 % in turn, with the oxygen flow rate at 4 L/min. The inhalation of sevoflurane was discontinued at the last item (suprasternal fossae) in the echocardiography. If the child had body movement and thus could not complete the echocardiography, the maintaining level should be adjusted to 3 % until completing the echocardiography. This was recorded as “fail to complete echocardiography” and not included in the statistical analysis of T0, T1, and T2.
Monitoring Items
The children were observed for vomiting, secretion, cough, and breath-holding during sedation. The T0, T1, and T2 were recorded. The Ramsay scale scoring was used to grade the sedation of children: (1) dysphoria; (2) compliant and still, with orientation; (3) responsive to instructions; (4) sleeping, sensitive to loud acoustic stimulus; (5) sleeping, insensitive to loud acoustic stimulus; and (6) drowsiness, no response. A score of four to five indicated ideal sedation [3]. The child’s blood pressure, heart rate, respiratory rate, and oxygen saturation were measured continuously during echocardiography. The time from sedation to qualification for echocardiography (T1), the duration of echocardiography (T2), and the time from discontinuing medication to awakening (T3) were recorded.
Statistical Analysis
All data were analyzed with SPSS19.0 statistical software. The measurement data were represented by mean ± SD (\(\overline{X}\) ± S), and tested by one-way ANOVA and Independent Samples T test; the categorical data were tested by Chi-square test. p < 0.05 indicated statistical significance.
Results
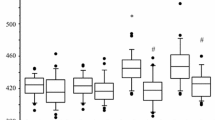
No child had cough or breath-holding during sedation. All children had little respiratory secretions and good airway tolerance. The T0, T1, and T2 in each group are presented in Table 2. No statistical differences were noted in T0 and T1 between each group. T2 was longest in 1.0 % group, and significantly prolonged in 2.5 % group.
When the inhalation level of sevoflurane was maintained at 1.0 %, the Ramsay scale score was low (Table 3), 8 children were not compliant (p < 0.05, in comparison with other groups) and required more sevoflurane to complete echocardiography. When the inhalation level of sevoflurane was maintained at 1.5 %, more children had Ramsay scale 4–5 score (p < 0.05, in comparison with 1.0 % group) and stable blood pressure, including 2 children who could not complete echocardiography. When the sevoflurane inhalation level was maintained at 2.0 %, 1 child could not complete echocardiography. When the sevoflurane inhalation level was maintained at 2.5 %, the Ramsay scale scores did not increase, and all children qualified for the echocardiography. For the children in all groups, the oxygen saturation was maintained at more than 98 %, the respiratory rate and blood pressure were not statistically different.
Discussion
The child should be relatively still in the pediatric echocardiography. However, since the child was young with poor cognition, he/she may resist and fear the irritation caused by the examination method [6]. Therefore, the anesthesia for sedation was essential for the child who was not compliant. The ideal anesthetic for outpatient sedation should be characterized by (1) stable and rapid induction, no pain or irritation; (2) sufficient sedation, amnesia, and analgesia for the examination; (3) no or minimum side effects, such as cardiovascular and respiratory inhibition; (4) rapid awakening, no complications, such as nausea and vomiting; (5) adjustable depth of anesthesia; and (6) better cost-effectiveness. Unfortunately, no anesthetic could completely satisfy these requirements to date [1].
Chloral hydrate is widely used as an anesthesia agent in pediatric outpatient examination; however, it has penetrating odor and corrosive bitterness, and children usually refused to take it or vomit after taking it. As a result, an increased or repeated dosage may be required. The coloclysis with chloral hydrate may cause resistance in children, resulting in mucosal injury and liquid medicine discharge due to crying and struggle of the children, leading to impaired sedation [2]. Therefore, it was very important to develop a safe, effective, and new outpatient sedation approach.
Sevoflurane has stable physical and chemical properties and small blood-air partition coefficient. It is characterized by rapid awakening, stable induction, and less excitation when it is used in pediatric inhalation anesthesia. Besides, it will provide stable awakening, less airway irritation and cardiovascular inhibition, and adjustable depth of anesthesia; therefore, it has unique advantages in pediatric anesthesia [4, 5]. The application of sevoflurane in pediatric outpatient sedation was less reported. This study mainly explored the optimum level of sevoflurane in pediatric echocardiography and provided evidences for the clinical use of sevoflurane in outpatient examination.
This study used the anesthesia induction with high level and large flow rate of anesthetic. Thus, the anesthesia induction may be accelerated according to the “concentration-effect” principle of the inhalation anesthetic [7]. But this method was not suitable for the children who were not compliant. The anesthetic level was decreased after the induction termination to achieve an appropriate level for echocardiography. The children had less respiratory secretions, good airway tolerance, and no cough or breath-holding during the echocardiography. This may be associated with less airway irritation and bronchial dilatation associated with the sevoflurane.
We used a series of maintaining level of 1.0, 1.5, 2.0, and 2.5 % sevoflurane in this study. The T2 was prolonged as the level of sevoflurane was increased. When the sevoflurane level was low, the scores of the children under sedation decreased, resulting in non-qualification for echocardiography. When the sevoflurane level was 1.5–2.0 %, almost all children qualified for the echocardiography and had rapid awakening. When the sevoflurane level was increased to 2.5 %, the children were sedated, but the echocardiography efficiency was decreased. Excessively high levels of sevoflurane may not only increase the incidence of adverse reactions during echocardiography, but also cause environmental pollution in the ultrasound room. Therefore, the exploration of the optimum level of sevoflurane in pediatric outpatient echocardiography is very important.
In conclusion, the inhaled sevoflurane sedation in pediatric outpatient echocardiography is characterized by rapid awakening, less effect on breath and blood circulation, and low incidence of adverse reactions. The sevoflurane at the optimum maintaining level is safe and effective to be used in pediatric outpatient echocardiography.
References
Dai, T., & Yu, T. (2011). Anesthetic Pharmacology (3rd ed., pp. 58–74). Beijing: People’s Medical Publishing House.
Li, S., Zhi, W., & Zhu, Z. (2005). The efficacy of midazolam combined with chloral hydrate in the sedation before pediatric CT. International Medicine & Health Reports, 10, 85–86.
Oto, J., Yamamoto, K., Koike, S., et al. (2011). Effect of daily sedative interruption on sleep stages of mechanically ventilated patients receiving midazolam by infusion. Anaesthesia and Intensive Care, 39, 392–400.
Ozdemir, K. I., Egilmez, H., Kaygusuz, K., Gursoy, S., & Mimaroglu, C. (2008). Open-label, prospective, randomized comparison of propofol and sevoflurane for laryngeal mask anesthesia for magnetic resonance imaging in pediatric patients. Clinical Therapeutics, 30, 175–181.
Toscano, A., Pancaro, S., Giovannoni, G., Minelli, G., Baldi, C., Guerrieri, G., et al. (2003). Sevoflurane analgesia in obstetrics: A pilot study. International Journal of Obstetric Anesthesia, 12, 79–82.
Xia, B., Liu, K., Wang, C., et al. (2010). The efficacy of oral midazolam in the pediatric dentistry. Peking University Proceedings (Medicine), 42(1), 78–81.
Yang, W., & Huang, W. (2006). The applications of sevoflurane in adult ambulatory surgery. Journal of Clinical Anesthesiology, 22, 239–240.
Funding
This study was funded by 9th High level talent Project of Jiangsu “Summit of 6 Talents” (Project No. 2012-WS-010), under Xuzhou Science and Technology Project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Conghai, F., Fengchao, Z., Chengjing, S. et al. The Optimum Level of Sevoflurane in Pediatric Echocardiography. Cell Biochem Biophys 73, 345–347 (2015). https://doi.org/10.1007/s12013-015-0602-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12013-015-0602-z