Abstract
Purpose of Review
Ductal carcinoma in situ (DCIS) of the breast is a heterogenous intraductal disease that exists within a spectrum of intraepithelial abnormalities ranging from atypia to invasive carcinoma. The vast majority of DCIS is diagnosed in asymptomatic women on screening mammography as suspicious calcifications, but can less commonly present as a palpable mass, suspicious nipple discharge, or as suspicious enhancement in high-risk women being screened with MRI. The distinction between atypia and low-grade DCIS is nuanced, and significant overlap in the imaging appearance of DCIS coupled with interobserver variability in diagnosing DCIS on pathology emphasizes the importance of collaboration between radiologist and pathologist when making a DCIS diagnosis. Under sampling or sampling error at core biopsy might lead to a diagnosis of atypia instead of DCIS or DCIS instead of invasive carcinoma, which has important management implications.
Recent Findings
Classification of DCIS continues to evolve as it relates to likelihood of recurrence; currently, nuclear grade, presence or absence of necrosis, and margin status play key roles.
Summary
While current treatment options for DCIS remain relatively aggressive and uniform for this non-lethal disease, on-going clinical trials, newer prognostic indices, and incorporation of genomics, proteomics, and radiomics aim to assist with optimizing DCIS management with the goal of decreasing overtreatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
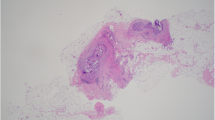
Ductal carcinoma in situ (DCIS) is a heterogenous group of intraductal proliferations that is traditionally described as a non-obligate precursor to breast cancer (Image 1). Since the advent of screening mammography, the once uncommon diagnosis now accounts for 20–25% of newly diagnosed breast cancer cases [1]. It was previously thought that approximately 40% of DCIS may not progress to invasive disease [2]. However, a more recent study, utilizing two well-established modeling groups, concluded that observational data alone is insufficient to determine the natural history of DCIS. Their model suggests that 36–99% of screen-detected DCIS will progress to invasive disease for women 50 years and older [3•].
The initial term “carcinoma in situ” was further subcategorized into “ductal” or “lobular” phenotype both of which arise from the terminal ductal lobular unit [4]. Lobular carcinoma in situ (LCIS) is classified as a non-cancerous high-risk lesion while DCIS is clinically defined as a stage 0 cancer by the National Cancer Comprehension Network (NCCN). However, DCIS lacks the ability to invade and metastasize, which is one of the six essential traits described by Hanahan and Weinberg as a “hallmark” of cancer [5]. This has led to continued controversy about DCIS and its role in breast cancer overdiagnosis and treatment.
Epidemiology of DCIS
Risk factors for DCIS are similar to those for invasive breast cancer, with age and female sex being paramount. The peak incidence occurs between the ages of 65 and 69, with DCIS being a relatively uncommon occurrence below the age of 30 [1]. There is increased risk for women with a family history of breast cancer and for women 50 years and older who are nulliparous. Rates of DCIS are lower among Hispanic, American Indian, and Alaska native women compared to those of White and Black women [1].
Histologic Description
DCIS is characterized by an intraductal proliferation of atypical cells that expands the ducts without invasion through the basement membrane or into the surrounding stroma [6]. The varying architectural patterns can be described as cribriform, micropapillary, comedo, solid, or mixed, among others [6]. Traditional classification systems utilized architectural patterns to stratify DCIS lesions. However, a significant amount of architectural heterogeneity exists, which limits histologic reproducibility and therefore the utility of these classification systems. Newer classification systems prioritize nuclear grade, the presence or absence of necrosis, and cell polarity, as histologic grade functions as a predictor of biologic behavior, and ultimately impacts treatment options [7]. The Van Nuys classification system is commonly utilized due to its simplicity. This classification system first defines a lesion as high nuclear grade (group 3) or non-high nuclear grade. The non-high-grade lesions are then further divided based on the presence of necrosis (group 2) or absence of necrosis (group 1) [8].
The Committee of the Consensus Conference on the Classification of DCIS did not endorse any single classification system but did specify which features should be included in the pathology report: nuclear grade, presence or absence of necrosis, polarization, and architectural patterns [9]. The Committee recommended the following characteristic also be included: margins, size, presence or absence of microcalcifications, and correlation of specimen radiograph with tissue sample [9]. They defined three nuclear grades—low (grade 1), intermediate (grade 2), and high (grade 3), emphasizing that lesions should be primarily stratified by this feature [9]. Low-grade nuclei are defined as monomorphic with finely dispersed chromatin, and occasional nucleoli and mitotic features [9]. High-grade nuclei are defined as markedly pleomorphic with irregular chromatin distribution, obvious mitoses, and multiple nucleoli [9]. Intermediate grade are any nuclei that do not meet grade 1 or 3 criteria [9]. Substantial comedonecrosis is usually present in high-grade DCIS; however, it is not a requirement [8]. The College of American Pathologists recognizes that nuclear grade, the presence of necrosis, and distance from margins are the most important factors in determining the likelihood of recurrence, with low-grade DCIS on average representing a more indolent disease than high-grade DCIS [1, 10•] (Image 2).
In our clinical practice, we prefer to assign grade based on the nuclear features of the neoplastic population. While low-grade DCIS is a borderline lesion on a spectrum with ADH, intermediate- and high-grade DCIS are distinct entities that are diagnosed regardless of size or extent on core biopsy. It should also be recognized that pathological characterization of the spectrum of pathologies from ADH to DCIS to invasive cancer is prone to sampling error, interobserver variability, and poor reproducibility [11]. For example, it has been estimated that 50% of DCIS lesions exhibit more than one nuclear grade [12] while another 15–20% will upgrade to invasive disease on surgical excision [13]. Furthermore, Elmore et al. demonstrated that concordance rates among pathologists are significantly lower for biopsy specimens consisting of DCIS (84%) or atypia (48%) than invasive cancers (96%) [13]. This variability highlights the importance of radiology-pathology concordance for this entity. For example, imaging findings that are very highly suspicious for DCIS, such as segmentally distributed fine-linear calcifications, would not be concordant with pathological findings of benign or high-risk pathology (e.g., atypical ductal hyperplasia), and would likely represent undersampling of the target. Similarly, an irregular-shaped mass with spiculated margins is unlikely to represent pure DCIS without invasion. In both cases, additional sampling would be imperative to ensure appropriate pathological assessment prior to finalization of management.
Mammographic Features
Mammography is the primary tool for detecting DCIS, as its most common presentation is microcalcifications. In approximately 10% of cases, DCIS can manifest as a non-calcified mass or asymmetry [8]. The detection of DCIS requires understanding of the anatomy of the terminal ductal lobular unit (TDLU), which is further described in chapter 1. The specific morphologic descriptors (as defined by the Breast Imaging-Reporting and Data Systems [BI-RADS] Atlas) of calcifications associated with DCIS, listed in increasing order of suspicion, include coarse heterogenous, amorphous, fine-pleomorphic, and fine-linear/fine-linear branching with a positive predictive value (PPV) of 70% for the latter [14]. The distribution of calcifications is equally as important with linear and segmental patterns classified as suspicious distributions. Spot magnification views are a necessity to characterize calcification morphology, distribution, and extent. Specific BI-RADS morphologies of calcifications that are commonly associated with DCIS are described in more detail below:
Coarse heterogenous: irregular shape, and larger (≥ 0.5 mm) than fine-pleomorphic with blunted ends.
Differential diagnosis: fibroadenoma, papilloma, fibrocystic change, DCIS (typically, low- to intermediate-grade) (Image 3).
Amorphous calcification: “powdered sugar” appearance.
Differential diagnosis: fibrocystic change, sclerosing adenosis, columnar cell change, or DCIS (more commonly low-grade) (Image 4).
Fine-pleomorphic and fine-linear/fine-linear branching: irregular shape with sharp or pointy ends, smaller (≤ 0.5 mm) than coarse heterogeneous.
Differential diagnosis: fibrocystic change or DCIS (more commonly high-grade) (Image 5).
Several non-BI-RADS terminologies have been reported in the literature that have been used to describe calcifications that frequently reflect DCIS. These include both “casting” and “crushed stone” features [1, 4], which have also been reported to more frequently reflect higher grade DCIS without comedonecrosis. More recently, Baker and colleagues have proposed additional calcification morphologies that may provide improved PPVs for DCIS over current BI-RADS terminologies. Among these, “teardrop,” “pill,” and “capsule” forms of calcifications were found to have an PPV of 84.9% for malignancy, most frequently (66.7%) DCIS [15]. It should be emphasized that suspicion for malignancy should not be based on morphological features alone. Even typically benign morphological features, such as “round,” could reflect DCIS when paired with a suspicious distribution, such as “linear” or “segmental.”
Finally, one in ten DCIS lesions present as a non-calcified finding. Most commonly, this will include a mass or focal asymmetry, often with relatively benign morphological features. In such cases, DCIS presenting as masses and asymmetries reflects a lower grade form. When architectural distortion is also noted with a DCIS lesion, it most commonly reflects an associated pathology such as sclerosing adenosis or a complex sclerosing lesion/radial scar [8].
Ultrasound Features
DCIS sensitivity on ultrasound is variable, ranging from 8 to 50% in the literature [16]. Ultrasound is typically most useful to evaluate mammographic findings that are not pure calcifications, although practice patterns differ, and some sites will evaluate areas of pure calcifications to assess for possible invasive components and to facilitate ultrasound-guided biopsy. The presence of a sonographically evident mass is not pathognomonic for invasive disease since DCIS can present as circumscribed or irregular masses on ultrasound (Image 6). DCIS can present as an ill-defined region of echogenic foci and dilated ducts, sometimes termed “heterogenous tissue” [17]. Another US imaging presentation of DCIS to be aware of is a mass with complex echotexture, including anechoic spaces. This type of lesion has been described as having a “pseudomicrocystic” appearance and is conjectured to be caused by distention of the lobular portion of the TDLU by DCIS [17]. Rarely, DCIS may present as a cluster of microcysts; however, in such cases, there should be associated vascularity as recent data indicates that pure clustered microcysts are benign [18]. Overall, when DCIS is visible on ultrasound and occult on mammography, it is more often lower grade [19, 20•].
MRI Features
MRI is useful in conjunction with other modalities in evaluating extent of disease. It surpasses both mammography and ultrasound in the ability to detect the presence and extent of disease [8, 21, 22]. It is the most sensitive imaging modality for detecting DCIS, particularly for high nuclear grade subtypes [23, 24]. Gadolinium-based contrast enhancement reflects increased vascularity unique or greater than background parenchymal enhancement. Non-mass enhancement (NME) is the most common MRI morphology of DCIS (Image 7). One classic presentation of DCIS is clumped NME, which represents enhancement of tumor growing within the duct giving the appearance of a “string of pearls” or “cobblestone” [25]. If DCIS involves larger ducts or expands the involved ducts, circumferential ductal enhancement becomes apparent and gives the appearance of “clustered ring” enhancement [25]. The enhancement kinetics of DCIS lesions at dynamic breast MRI vary and no kinetic pattern is pathognomonic for DCIS or closely correlates with a nuclear grade [7, 8]. Given the variability of MRI enhancement kinetics, correlation of mammographic calcifications and NME on MRI remains crucial.
Related High-risk Lesions
The current theory of progression to invasive breast cancer is a multi-step transformation from normal cells to invasive carcinoma, and within this progression lies the heterogenous class of DCIS lesions. However, there is a class of lesions that also typically present as calcifications on mammography categorized as benign but high-risk. The term “high-risk” indicates the possibility of under sampling of co-existing malignancy at core biopsy (i.e., risk of upgrade to malignancy at surgical excision) and/or association of that pathology with elevated future risk of breast cancer. Several such high-risk lesions are commonly associated with DCIS, and are discussed in more detail below:
Flat epithelial atypia (FEA) is defined as variably dilated and enlarged acini that contain a flat, intraductal epithelial proliferation comprised of atypical low-grade (monomorphic) columnar-type cells (Image 8). FEA is commonly associated with intraluminal calcifications (Image 9). FEA is at times a controversial entity with varying amounts of interobserver variability depending on training, and is on a spectrum with columnar cell change and columnar cell hyperplasia [26, 27]. A meta-analysis found that the reported rate of upgrade from FEA on biopsy to carcinoma at the time of excision ranges from 13 to 67% [28], although the recent international consensus conference on breast lesions of uncertain malignant potential reported 19.8% [22]. FEA is commonly present in association with ADH, low-grade DCIS, lobular neoplasia, invasive tubular carcinoma or lobular carcinoma, and it is thought that this upgrade to carcinoma is likely a progression of the associated proliferative component (ADH, DCIS, etc.) rather than from the FEA itself [29]. Management for FEA is evolving and requires individualized radiologic correlation [30].
Atypical ductal hyperplasia (ADH) is defined as a focal intraductal proliferation of low-grade (monomorphic) atypical epithelium with complex architecture of varying patterns (Image 10). ADH raises consideration of low-grade DCIS but falls short in extent (size) or diagnostic features of DCIS on core biopsy. This is a controversial diagnostic entity with both variation in interpretation and practice [31]. In these borderline lesions, low-grade DCIS interpreted at one institution may be interpreted as ADH at another. Often both interpretations are reasonable and the end treatment is the same: excision. Therefore, many expert breast pathologists interpret such cases as ADH so as not to over diagnose cancer at the time of biopsy. The rate of upgrade at excision is 27.6% [22].
In situ lobular neoplasia is a group of high-risk lesions that include both atypical lobular hyperplasia (ALH) and lobular carcinoma in situ (LCIS). These intraepithelial proliferations have a lobular phenotype, which is characterized by a somewhat discohesive appearance, intracytoplasmic vacuoles, and loss of E-Cadherin immunoreactivity. The distinction between ALH and LCIS is controversial, with high intra and interobserver variability, and is based on extent of involvement and distension of the TDLU. Within a TDLU, ALH is considered to fill but not distend (subjective) less than 50% of acini while LCIS distends at least 50% of the acini (Image 11). LCIS is divided into two main categories, classical and pleomorphic; however, emerging studies suggest that other clinically relevant variants such as “florid” may exist with unique prognostic profiles. Regarding indications for excisional biopsy, if on core needle biopsy there are > 4 terminal duct lobular units (TDLUs) involved by lobular neoplasia, excisional biopsy is recommended [8] (Image 12). In addition, there is consensus that surgical excision (often to clear margins) is warranted when the lobular neoplasm is pleomorphic [21] or associated with a mass on imaging. A recent meta-analysis by Shehata et al. calculated a 5.8% upgrade rate for LCIS in the setting of radiology-pathology concordance, which led the authors to propose imaging follow-up as an appropriate alternative to surgical excision [20•].
Complex sclerosing lesion and radial scars are lesions defined by a central area of sclerosis with variably complex epithelial components radiating outwards, sometimes creating a “dark star” appearance on mammography (Image 13). When larger than 1.0 cm, these lesions were historically referred to as complex sclerosing lesions; however, this distinction is generally no longer in use and the terms are used interchangeably. The radial scar/complex sclerosing lesion may be involved by epithelial proliferations ranging from usual ductal hyperplasia to sclerosing adenosis to cysts. Furthermore, involvement of the radial scar by atypical epithelial proliferations, carcinoma in situ, or invasive carcinoma can be focal and patchy and therefore not detectable until the time of excision. Diagnosing radial scar on biopsy is challenging due to the limited sampling, which may result in features that overlap with fibrocystic change or raise concern for invasive carcinoma. In particular, the central sclerosis of radial scars can lead to entrapped, angulated glands with loss of a myoepithelial layer, which may lead to overdiagnosis. Biopsy methods that allow for collection of greater tissue may aid in proper diagnosis of these lesions [32]. The rate of upgrade at excision is variable and is dependent on needle size, number of samples, and pathologist experience (Image 14).
Papillary lesions are defined by fibrovascular cores lined by myoepithelium and overlying ductal epithelium [33] (Image 15). The degree to which the epithelium is proliferative and/or atypical guides the pathologist in rendering a diagnosis. The term “papillary lesion” encompasses a diverse group of lesions (Images 16, 17). The intraductal papilloma is a proliferation of epithelium arranged along fibrovascular cores confined by a basement membrane. If on biopsy the epithelial lining has atypical cytomorphology, it raises consideration of a more worrisome process such as ADH involving a papilloma, DCIS involving a papilloma, papillary DCIS, or a form of papillary carcinoma (encapsulated or invasive). Distinguishing between these entities in the biopsy setting can be challenging and is best deferred to the time of excision. For papillary lesions diagnosed on biopsy, the rate of upgrade at excision is variable and based on associated atypia.
Implications for Management
DCIS is generally a screen-detected entity that constitutes the earliest form of breast cancer diagnosis that a patient can receive; however, it is a challenging pathology to characterize and is fraught with treatment challenges. The overarching goal of DCIS treatment is to prevent its progression to invasive disease and decrease likelihood of an ipsilateral breast tumor recurrence (IBTR). Currently, the vast majority of women diagnosed with DCIS undergo some form of surgical resection, typically to achieve disease-free margins of at least 2 mm. Surgery may be either mastectomy or wide local excision (WLE, also known as lumpectomy or partial mastectomy). When WLE is performed as part of a breast conservation treatment approach, radiation therapy and/or endocrine therapy is very often recommended. Overall, survival is excellent for DCIS; however, the rates of local recurrence vary widely between different treatments [34].
Although DCIS represents a wide spectrum of biology and prognosis, current treatment is fairly homogeneous and aggressive. Active surveillance in lieu of surgery is very rare outside of clinical trials (e.g., Comparison of Operative versus Monitoring and Endocrine Therapy [COMET] trial) [35], and radiation therapy is recommended for approximately 75% of women treated with WLE. This is because it has been shown by the Early Breast Cancer Trialists’ Collaborative Group meta-analysis of 4 randomized trials that radiation therapy after WLE reduces recurrence risk by approximately 50% (34). Endocrine therapy has also been shown to reduce the risk of both ipsilateral and contralateral breast events [34]. Nevertheless, neither adjuvant radiation therapy or endocrine therapy reduced overall mortality or improved survival (34). Several clinical models, including the Memorial Sloan Kettering Nomogram [36] and the Van Nuys Prognostic Index [37], combine clinical and pathological features to assist clinicians with adjuvant therapy decision-making. However, neither has to date been accepted widely, and it is widely recognized that the high rates of radiation therapy in the setting of DCIS likely constitutes overtreatment due to an imperfect means to stratify risk.
Newer technologies, such as Oncotype DX DCIS Score (Exact Sciences, Madison, WI) and DCISionRT (PreludeDx Laguna Hills, CA), utilize genomic information to help calculate the 10-year risk of local recurrence in a select group of patients to help guide treatment options [38, 39]. However, neither are in broad use due to cost and a lack of prospective validation in clinical trials. Risk stratification of DCIS through quantitative and radiomic MRI features also has demonstrated promise, but to date remains exploratory [40,41,42,43]. As a result, DCIS remains a heterogeneous disease with an elusive natural history. Continued research on genomic, pathomic, proteomic, and radiomic features that can further refine individual DCIS lesions’ risk is critical to improving its biological evaluation and tailoring treatment to risk.
Conclusion
DCIS and related high-risk pathology remain a diagnostic challenge from a radiologic, histologic, and clinical perspective. This disease process is most frequently diagnosed by imaging in the form of calcifications and/or non-mass enhancement, which can have significant overlap with benign entities. Interobserver variability of pathological assessment for DCIS can be high due to inherent heterogeneity of DCIS lesions, close relationship of low-grade forms with ADH, and sampling error due to image-guided approaches. Adequate tissue sampling remains paramount to provide information at the cellular level for the pathologist to interpret. Collaboration between radiology and pathology to determine concordance remains critical for appropriate management. Radiologists facing non-malignant pathologic assessment for lesions that are deemed to be highly suspicious for DCIS should recommend additional sampling, either by repeat core biopsy or surgical excision, to minimize the risk of a delayed cancer diagnosis.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Parikh U, Chhor CM, Mercado CL. Ductal carcinoma in situ: the whole truth. AJR Am J Roentgenol. 2018;210(2):246–55. Epub 2017/10/19. https://doi.org/10.2214/AJR.17.18778. PubMed PMID: 29045181.
D’Orsi CJ. Imaging for the diagnosis and management of ductal carcinoma in situ. J Natl Cancer Inst Monogr. 2010;2010(41):214–7. Epub 2010/10/20. https://doi.org/10.1093/jncimonographs/lgq037. PubMed PMID: 20956833; PMCID: PMC5161079.
• Chootipongchaivat S, van Ravesteyn NT, Li X, Huang H, Weedon-Fekjaer H, Ryser MD, Weaver DL, Burnside ES, Heckman-Stoddard BM, de Koning HJ, Lee SJ. Modeling the natural history of ductal carcinoma in situ based on population data. Breast Cancer Res. 2020;22(1):53. Epub 2020/05/29. https://doi.org/10.1186/s13058-020-01287-6. PubMed PMID: 32460821; PMCID: PMC7251719.This paper utilized two well-established population models and evaluated six possbile DCIS natural history submodels. Their results suggest that without biopsy or surgical excision the majority of screen-detected DCIS will progress to invasive breast cancer within relatively short time.
Foote FW, Stewart FW. Lobular carcinoma in situ: a rare form of mammary cancer. Am J Pathol. 1941;17(4):491–6 3. Epub 1941/07/01. https://doi.org/10.3322/canjclin.32.4.234. PubMed PMID: 19970575; PMCID: PMC1965212.
Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000;100(1):57–70. Epub 2000/01/27. https://doi.org/10.1016/s0092-8674(00)81683-9. PubMed PMID: 10647931.
Lopez-Garcia MA, Geyer FC, Lacroix-Triki M, Marchio C, Reis-Filho JS. Breast cancer precursors revisited: molecular features and progression pathways. Histopathology. 2010;57(2):171–92. Epub 2010/05/27. https://doi.org/10.1111/j.1365-2559.2010.03568.x. PubMed PMID: 20500230.
Schuh F, Biazus JV, Resetkova E, Benfica CZ, Ventura Ade F, Uchoa D, Graudenz M, Edelweiss MI. Histopathological grading of breast ductal carcinoma in situ: validation of a web-based survey through intra-observer reproducibility analysis. Diagn Pathol. 2015;10:93. Epub 2015/07/15. https://doi.org/10.1186/s13000-015-0320-2. PubMed PMID: 26159429; PMCID: PMC4702358.
Yamada T, Mori N, Watanabe M, Kimijima I, Okumoto T, Seiji K, Takahashi S. Radiologic-pathologic correlation of ductal carcinoma in situ. Radiographics. 2010;30(5):1183–98. Epub 2010/09/14. https://doi.org/10.1148/rg.305095073. PubMed PMID: 20833844.
Consensus Conference on the classification of ductal carcinoma in situ. The Consensus Conference Committee. Cancer. 1997;80(9):1798–802. Epub 1997/11/14. https://doi.org/10.1002/(sici)1097-0142(19971101)80:9<1798::aid-cncr15>3.0.co;2-0. PubMed PMID: 9351550.
• Cserni G, Sejben A. Grading ductal carcinoma in situ (DCIS) of the breast - what’s wrong with it? Pathol Oncol Res. 2020;26(2):665–71. Epub 2019/11/30. https://doi.org/10.1007/s12253-019-00760-8. PubMed PMID: 31776839; PMCID: PMC7242244. This review looks at the heterogenity of grading DCIS with a goal of emphasizing the inconsistences among current grading and classification systems. This paper impresses the importance of a uniform and universally recognized grading system so that research can further determine if low-grade DCIS lesions require the same treatment as high-grade lesions.
Schnitt SJ, Connolly JL, Tavassoli FA, Fechner RE, Kempson RL, Gelman R, Page DL. Interobserver reproducibility in the diagnosis of ductal proliferative breast lesions using standardized criteria. Am J Surg Pathol. 1992;16(12):1133–43. Epub 1992/12/01. https://doi.org/10.1097/00000478-199212000-00001. PubMed PMID: 1463092.
Miller NA, Chapman JA, Fish EB, Link MA, Fishell E, Wright B, Lickley HL, McCready DR, Hanna WM. In situ duct carcinoma of the breast: clinical and histopathologic factors and association with recurrent carcinoma. Breast J. 2001;7(5):292–302. Epub 2002/03/22. https://doi.org/10.1046/j.1524-4741.2001.99124.x. PubMed PMID: 11906438.
Elmore JG, Longton GM, Carney PA, Geller BM, Onega T, Tosteson AN, Nelson HD, Pepe MS, Allison KH, Schnitt SJ, O’Malley FP, Weaver DL. Diagnostic concordance among pathologists interpreting breast biopsy specimens. JAMA. 2015;313(11):1122–32. Epub 2015/03/18. https://doi.org/10.1001/jama.2015.1405. PubMed PMID: 25781441; PMCID: PMC4516388.
D’Orsi CJ. ACR BI-RADS atlas : breast imaging reporting and data system. Reston (VA): American College of Radiology; 2013.
Baker JA, Grimm LJ, Johnson KS. A proposal to define three new breast calcification shapes: square, sandwich, and teardrop, pill & capsule. Journal of Breast Imaging. 2019;1(3):186–91. https://doi.org/10.1093/jbi/wbz046.
Moon HJ, Kim EK, Kim MJ, Yoon JH, Park VY. Comparison of clinical and pathologic characteristics of ductal carcinoma in situ detected on mammography versus ultrasound only in asymptomatic patients. Ultrasound Med Biol. 2019;45(1):68–77. Epub 2018/10/17. https://doi.org/10.1016/j.ultrasmedbio.2018.09.003. PubMed PMID: 30322671.
Wang LC, Sullivan M, Du H, Feldman MI, Mendelson EB. US appearance of ductal carcinoma in situ. Radiographics. 2013;33(1):213–28. Epub 2013/01/17. https://doi.org/10.1148/rg.331125092. PubMed PMID: 23322838.
Goldbach AR, Tuite CM, Ross E. Clustered microcysts at breast US: outcomes and updates for appropriate nanagement recommendations. Radiology. 2020;295(1):44–51. Epub 2020/02/19. https://doi.org/10.1148/radiol.2020191505. PubMed PMID: 32068502.
Mesurolle B, El-Khoury M, Khetani K, Abdullah N, Joseph L, Kao E. Mammographically non-calcified ductal carcinoma in situ: sonographic features with pathological correlation in 35 patients. Clin Radiol. 2009;64(6):628–36. Epub 2009/05/06. https://doi.org/10.1016/j.crad.2008.12.013. PubMed PMID: 19414087.
• Shehata MN, Rahbar H, Flanagan MR, Kilgore MR, Lee CI, Ryser MD, Lowry KP. Risk for upgrade to malignancy after breast core needle biopsy diagnosis of lobular neoplasia: a systematic review and meta-analysis. J Am Coll Radiol. 2020;17(10):1207–19. Epub 2020/08/31. https://doi.org/10.1016/j.jacr.2020.07.036. PubMed PMID: 32861602. This review article looked at the risk of upgrade when classic lobular neoplasia was diagnosed on core needle biopsy. The authors concluded that the risk for upgrade to malignancy was low and suggested imaging follow-up as an alternative to surgical excision.
Foschini MP, Miglio R, Fiore R, Baldovini C, Castellano I, Callagy G, Bianchi S, Kaya H, Amendoeira I, Querzoli P, Poli F, Scatena C, Cordoba A, Pietribiasi F, Kovacs A, Faistova H, Cserni G, Quinn C. Pre-operative management of pleomorphic and florid lobular carcinoma in situ of the breast: report of a large multi-institutional series and review of the literature. Eur J Surg Oncol. 2019;45(12):2279–86. Epub 2019/07/16. https://doi.org/10.1016/j.ejso.2019.07.011. PubMed PMID: 31301938.
Rageth CJ, O’Flynn EA, Comstock C, Kurtz C, Kubik R, Madjar H, Lepori D, Kampmann G, Mundinger A, Baege A, Decker T, Hosch S, Tausch C, Delaloye JF, Morris E, Varga Z. First International Consensus Conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat. 2016;159(2):203–13. Epub 2016/08/16. https://doi.org/10.1007/s10549-016-3935-4. PubMed PMID: 27522516; PMCID: PMC5012144.
Kuhl CK, Schrading S, Bieling HB, Wardelmann E, Leutner CC, Koenig R, Kuhn W, Schild HH. MRI for diagnosis of pure ductal carcinoma in situ: a prospective observational study. Lancet. 2007;370(9586):485–92. Epub 2007/08/19. https://doi.org/10.1016/S0140-6736(07)61232-X. PubMed PMID: 17693177.
Lehman CD, Gatsonis C, Kuhl CK, Hendrick RE, Pisano ED, Hanna L, Peacock S, Smazal SF, Maki DD, Julian TB, DePeri ER, Bluemke DA, Schnall MD, Group ATI. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med. 2007;356(13):1295–303. Epub 2007/03/30. https://doi.org/10.1056/NEJMoa065447. PubMed PMID: 17392300.
Ikeda DM, Miyake KK. Breast imaging: the requisites, Third Edition2017.
Gomes DS, Porto SS, Balabram D, Gobbi H. Inter-observer variability between general pathologists and a specialist in breast pathology in the diagnosis of lobular neoplasia, columnar cell lesions, atypical ductal hyperplasia and ductal carcinoma in situ of the breast. Diagn Pathol. 2014;9:121. Epub 2014/06/21. https://doi.org/10.1186/1746-1596-9-121. PubMed PMID: 24948027; PMCID: PMC4071798.
O’Malley FP, Mohsin SK, Badve S, Bose S, Collins LC, Ennis M, Kleer CG, Pinder SE, Schnitt SJ. Interobserver reproducibility in the diagnosis of flat epithelial atypia of the breast. Mod Pathol. 2006;19(2):172–9. Epub 2006/01/21. https://doi.org/10.1038/modpathol.3800514. PubMed PMID: 16424892.
Verschuur-Maes AH, van Deurzen CH, Monninkhof EM, van Diest PJ. Columnar cell lesions on breast needle biopsies: is surgical excision necessary? A systematic review. Ann Surg. 2012;255(2):259–65. Epub 2011/10/13. https://doi.org/10.1097/SLA.0b013e318233523f. PubMed PMID: 21989373.
Said SM, Visscher DW, Nassar A, Frank RD, Vierkant RA, Frost MH, Ghosh K, Radisky DC, Hartmann LC, Degnim AC. Flat epithelial atypia and risk of breast cancer: a Mayo cohort study. Cancer. 2015;121(10):1548–55. Epub 2015/02/03. https://doi.org/10.1002/cncr.29243. PubMed PMID: 25639678; PMCID: PMC4424157.
Calhoun BC, Sobel A, White RL, Gromet M, Flippo T, Sarantou T, Livasy CA. Management of flat epithelial atypia on breast core biopsy may be individualized based on correlation with imaging studies. Mod Pathol. 2015;28(5):670–6. Epub 2014/11/22. https://doi.org/10.1038/modpathol.2014.159. PubMed PMID: 25412845.
Allison KH, Reisch LM, Carney PA, Weaver DL, Schnitt SJ, O’Malley FP, Geller BM, Elmore JG. Understanding diagnostic variability in breast pathology: lessons learned from an expert consensus review panel. Histopathology. 2014;65(2):240–51. Epub 2014/02/12. https://doi.org/10.1111/his.12387. PubMed PMID: 24511905; PMCID: PMC4506133.
Bacci J, MacGrogan G, Alran L, Labrot-Hurtevent G. Management of radial scars/complex sclerosing lesions of the breast diagnosed on vacuum-assisted large-core biopsy: is surgery always necessary? Histopathology. 2019;75(6):900–15. Epub 2019/07/10. https://doi.org/10.1111/his.13950. PubMed PMID: 31286532.
Collins LC, Schnitt SJ. Papillary lesions of the breast: selected diagnostic and management issues. Histopathology. 2008;52(1):20–9. Epub 2008/01/04. https://doi.org/10.1111/j.1365-2559.2007.02898.x. PubMed PMID: 18171414.
Barrio AV, Van Zee KJ. Controversies in the treatment of ductal carcinoma in situ. Annu Rev Med. 2017;68:197–211. Epub 2017/01/19. https://doi.org/10.1146/annurev-med-050715-104920. PubMed PMID: 28099081; PMCID: PMC5532880.
Hwang ES, Hyslop T, Lynch T, Frank E, Pinto D, Basila D, Collyar D, Bennett A, Kaplan C, Rosenberg S, Thompson A, Weiss A, Partridge A. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open. 2019;9(3):e026797. Epub 2019/03/14. https://doi.org/10.1136/bmjopen-2018-026797. PubMed PMID: 30862637; PMCID: PMC6429899.
Syed A, Eleti S, Kumar V, Ahmad A, Thomas H. Validation of Memorial Sloan Kettering Cancer Center nomogram to detect non-sentinel lymph node metastases in a United Kingdom cohort. G Chir. 2018;39(1):12–9. Epub 2018/03/20. https://doi.org/10.11138/gchir/2018.39.1.012. PubMed PMID: 29549676; PMCID: PMC5902139.
Silverstein MJ, Lagios MD, Craig PH, Waisman JR, Lewinsky BS, Colburn WJ, Poller DN. A prognostic index for ductal carcinoma in situ of the breast. Cancer. 1996;77(11):2267–74. Epub 1996/06/01. https://doi.org/10.1002/(SICI)1097-0142(19960601)77:11<2267::AID-CNCR13>3.0.CO;2-V. PubMed PMID: 8635094.
Oncotype DX DCIS score predicts recurrence. Cancer Discov. 2015;5(2):OF3. Epub 2015/02/07. https://doi.org/10.1158/2159-8290.CD-NB2014-189. PubMed PMID: 25656901.
Emdin SO, Granstrand B, Ringberg A, Sandelin K, Arnesson LG, Nordgren H, Anderson H, Garmo H, Holmberg L, Wallgren A, Swedish Breast Cancer G. SweDCIS: radiotherapy after sector resection for ductal carcinoma in situ of the breast. Results of a randomised trial in a population offered mammography screening. Acta Oncol. 2006;45(5):536–43. Epub 2006/07/26. https://doi.org/10.1080/02841860600681569. PubMed PMID: 16864166.
Chou SS, Gombos EC, Chikarmane SA, Giess CS, Jayender J. Computer-aided heterogeneity analysis in breast MR imaging assessment of ductal carcinoma in situ: correlating histologic grade and receptor status. J Magn Reson Imaging. 2017;46(6):1748–59. Epub 2017/04/04. https://doi.org/10.1002/jmri.25712. PubMed PMID: 28371110; PMCID: PMC5624816.
Kim SA, Cho N, Ryu EB, Seo M, Bae MS, Chang JM, Moon WK. Background parenchymal signal enhancement ratio at preoperative MR imaging: association with subsequent local recurrence in patients with ductal carcinoma in situ after breast conservation surgery. Radiology. 2014;270(3):699–707. Epub 2013/10/16. https://doi.org/10.1148/radiol.13130459. PubMed PMID: 24126372.
Luo J, Johnston BS, Kitsch AE, Hippe DS, Korde LA, Javid S, Lee JM, Peacock S, Lehman CD, Partridge SC, Rahbar H. Ductal carcinoma in situ: quantitative preoperative breast MR imaging features associated with recurrence after treatment. Radiology. 2017;285(3):788–97. Epub 2017/09/16. https://doi.org/10.1148/radiol.2017170587. PubMed PMID: 28914599; PMCID: PMC5708288.
Rahbar H, McDonald ES, Lee JM, Partridge SC, Lee CI. How can advanced imaging be used to mitigate potential breast cancer overdiagnosis? Acad Radiol. 2016;23(6):768–73. Epub 2016/03/28. https://doi.org/10.1016/j.acra.2016.02.008. PubMed PMID: 27017136; PMCID: PMC4867276.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Sarah Anderson, John Scheel, and Elizabeth Parker declare no conflict of interest.
Habib Rahbar has grant funding with GE Healthcare not related to this article.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Habib Rahbar is a senior author.
This article is part of the Topical Collection on Best Practice Approaches Breast Radiology-Pathology Correlation and Management.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Anderson, S., Parker, E., Rahbar, H. et al. IV Ductal Carcinoma In Situ, Including its Histologic Subtypes and Grades. Curr Breast Cancer Rep 13, 398–404 (2021). https://doi.org/10.1007/s12609-021-00439-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12609-021-00439-7